Abstract
Lung cancer long term survival still remains poor and early detection is still the best methodology to treatment. Therefore several novel approaches have been investigated for anticancer drug administration. Inhaled therapies for lung diseases are used since the ancient times. Inhaled anticancer treatment administration was firstly investigated almost 30 years ago. Since then the inclusion and exclusion criteria have been investigated in correlation with the safety and efficacy of cisplatin, 5-fluoracil, carboplatin, paclitaxel, docetaxel, 9-nitro camptothecine, gemcitabine, cetuximab, granulocyte-colony stimulating factor, interleukins and recently with bevasizumab. Along with the anticancer drug formulations administered, other aspects of this local treatment have been also investigated to improve the efficiency and safety, such as; proper nebulization system, drug formulation delivery system, setting of administration, aerosol protection measures, inhalation techniques and safety issues follow up. During the last years with the use of actigraphy wrist watches, an extended investigation of the circadian rhythm of animals and humans has been performed and new insights are included in lung cancer chemotherapy administration. The “personalized” therapy administration should not be considered only as a molecular pathway inhibition, but also as a chrono-targeted anticancer treatment.
Key Words: Chrono-modulation, non-small cell lung cancer (NSCLC), cancer
Lung cancer treatment has been individualized during the last years as targeted therapies according to the tumors genome are being used. The “pharmacogenomics” science is under development, since we have understood the importance of the regulatory function that the genome expression has on the efficiency of anticancer drugs. Nevertheless, the targeted therapies have not yet presented the effectiveness that was expected. The targeted therapies until now are designed that each drug formulation inhibits specific disrupted pathways that induce tumorigenesis. However, the neoplasia disrupts many pathways at the same time, making the effort of targeted therapy still inefficient. Therefore the administration of fundamental chemotherapy anti-cancer drugs is still very useful as they inhibit several tumorigenesis pathways and induce apoptosis on a large scale. The systemic side effects from these drugs still remain unacceptable; therefore novel treatment modalities have been explored. The concept behind local treatment is the local deposition of a chemotherapeutic agent to the target site with the highest efficiency and decreased side effects. It has been observed that the inhaled chemotherapy administration of 5-fluoracil, doxorubicin, paclitaxel, docetaxel, platinum analogues, cetuximab, 9-nitro camptothecin, interleukins, granulocyte stimulating growth factor and recently bevazisumab is effective and safe (1). However, although certain drugs demonstrated efficiency at the same time they presented pulmonary toxicity (taxanes and doxorubicin). The platinum analogues which are the cornerstone of the anticancer treatment were used with effectiveness and safety in human trials (1,2). To further improve the anticancer treatment several other aspects of the cancer patients were observed. Sleep disturbances of cancer patients are well known and have been associated with cancer status and disease response (3). Sleep disturbances until recently were evaluated with questionnaires and polysomnography. However, the circadian rhythm, the 24 h “individual” clock has been investigated and useful information have been presented regarding the regulatory influence upon the genes expression and protein production (4). It has been presented that the circadian rhythmicity regulates several cell functions relevant to lung cancer; cellular apoptosis, repair and drug metabolism. There are genes that regulate the circadian rhythm Per 1-3, Bmal-1, Rev-erba. It has been stated that the mRNA expression is depended by the cancer type and disease status (5). The circadian timing system (CTS) is based upon the function of suprachiasmatic nuclei (SCN). These nuclei are calibrated to a 24 h and in some people to 25 h based on the light-dark day cycle, sociocultural and feeding synchronization with meal times. Therefore normalization of the circadian rhythm is possible through light and meal treatment synchronization (5). The SCN generate and/or control cellular physiology like; (I) locomotor activity, (II) serum cortisol, (III) serum melatonin and (IV) body temperature. The sympathetic and parasympathetic, cytokines such as; tumor growth factor-α TNF-(α) and epidermal growth factor (EGF) are also controlled by SCN. The pharmacokinetics and pharmacodynamics are circadian dependent and data have been presented that toxicity was correlated for more than 30 drugs with circadian rhythmicity disruption (5). In addition it has been presented that the efficiency is indifferent of the route of administration and was 50% higher when administered as chrono-target therapy (6). Therefore a protocol based on chrono-target administration of inhaled chemotherapy was established to investigate and provide novel insights when combining these two treatment modalities.
Inhaled chemotherapy
Inhaled chemotherapy administration with nebulizer has been previously described. The inclusion criteria and candidates for this treatment modality have been also presented in several studies (1) (Table 1). The setting of the inhaled chemotherapy administration for now with current technology is preferred to be delivered within a high efficiency particulate air filter tent (HEPA). The patients will be given bronchodilators and inhaled corticosteroids with neduliser before the inhalation of the chemotherapy agent and after. A spirometry will also be performed prior to the chemotherapy administration. Patients in the control group will be given a platinum analog as inhalation in the morning hours where another group of patients will be given the chemotherapy according to the circadian rhythm evaluation.
Table 1. Protocol proposal (Phase I/II).
| Inclusion criteria |
| -Unresectable stage Non-Small Cell Lung Cancer (NSCLC) |
| -ATS/ERS Predicted values |
| Forced Expiratory Volume in 1 sec (FEV1) no less than ≤50% |
| Forced Vital Capacity (FVC) no less than ≤50% |
| Diffusing Capacity of the Lung for Carbon Monoxide (DLCO) no less than ≤50% |
| -Tumor diameter no larger than ≥5 cm |
| -Unpreviously treated NSCLC |
| -Saturation oxygenation upon rest ≤90% and exercise oxygene saturation ≥80% |
| -Karnofsky performance status ≥80 |
| -Adequate laboratory values in order to receive chemotherapy |
| Exclusion criteria |
| -Known collagen disease (interstitial lung disease, systematic lupus erythromatosis, rheumatoid arthritis e.t.c) |
| -Alnagesic treatment with opioids prior to treatment initiation |
| -Recent surgery |
| -Active respiratory infection |
| -Previous immunotherapy, or concurrently included in another protocol |
| -Unstable or serious concurrent medical condition (e.g., recent myocardial infarction and superior vena cava syndrome) |
| -Previous radiotherapy sessions to the thorax |
Sleep-disorder measurements
It has been previously demonstrated that in specific, lung cancer patients have additional factors that enhance their sleep disorders like exert dyspnoia. The sleep disorders are associated with disease stage and performance status; however an association between treatment modality and outcome has not been associated with changes in sleep disorders. Radiation has been found to be an independent parameter that enhances fatigue and augments sleep disorders (7). The parameters that are usually used to measure the sleep disorders in these patients are the Epworth Severity Scale (ESS), Fatigue Severity Score (FSS), Pittsburgh Sleep Quality Index (PSQI) and Medical Research Council Questionnaire (MRCQ), Karnosfky Performance Status (KPS), Attentional Function Index (AFI) and General Sleep Disturbance Scale (GSDS) (8-15). These questionaires have been previously combined with polysomnography in lung cancer patients to correlate performance status and response to treatment (3). Recently actigraphy with state of the art wrist watches are able to record digitally-integrated measure of gross motor activity that can be used to visualize rest activity patterns and quantify physical activity or sleep. Features like Integrated light sensors provide irradiance and luminous flux recordings in red, green, and blue color bands and a white light measurement in lux. It is an ideal equipment to measure the circadian rhythm. Combing all these information with several laboratory parameters like adrenaline, cortisol, adrenocorticotropic hormone, insulin, nor-adrenaline and vitamin-D we can have a complete profile of the cancer patient and his biologic internal clock. A relatively new method to measure cortisol multiple times throughout the day without the discomfort of needles is the salivatory cortisol, it is a well-established minimally invasive and efficient method.
Chrono-target administration
It has been previously presented that the efficiency of chemotherapy is associated with the proper gene expression and protein production that are included in the metabolism of the chemotherapeutic pharmaceuticals. Moreover, the toxic effects of chemotherapy are associated with the sustained circulation of the anticancer drugs independently of the drug concentration because the drugs are not metabolized due to lack of the necessary enzymes. The chrono-target therapy aims to administer the chemotherapy regimen when the biologic clock of the normal cell is at rest and therefore the normal cells are protected from the drugs cytotoxicity. On the other hand the disrupted and accelerated continuous division of cancer cells makes them vulnerable to the regimen. The respiratory tract has different transporters in different sites of the airways and more than 380 genes are expressed (1,16). The ABC family and in specific abcc2/abcc2 was observed to be modified throughout the 24-h circadian clock, the mRNA expression ranges from 3-to 6-fold and the protein from 2- to 3- fold (17). Several drugs metabolism is associated with the ABC family transporters such as; cisplatin, epirubicin, docetaxel, doxorubicin, paclitaxel, vinblastine and methotrexate as these drug effluxes involve the abcc2 transporter. Therefore, since these transporters are found locally on the respiratory tract local activation is observed. Afterwards, as it is known the drug formulation and metabolites are distributed to the blood circulation and lymphatic circulation. It has been observed that 5-flouoracil efficiency is augmented when administered at 4 AM, irrinotecan at 5 AM and oxaliplatin at 4 PM (18,19). The 5-fluoracil efficiency was associated with high intracellular dehydropyrimide (DPD) activity in normal human cells and low DNA synthesis in normal tissues. The oxaliplatin efficiency was associated with highly reduced glutathione levels and high circulating enzyme and proteins. The irrinotecan efficiency is observed with high Bcl-2 messange RNA expression and low percentage of S phase cells in normal cells. The dihydropyrimidine dehydrogenase (DPD), an enzyme that catabolizes the 5-FU and glutathione (GSH), it is a tripeptide that exists in the cytoplasm of most cells. It has been observed that the concentration of DPD is higher between midnight and 4:00 and the concentration of GSH is higher near noon. The GSH concentrations have been observed to be higher in bone marrow. The GSH concentration has been associated with reduced toxicity of oxaliplatin (4).
Regarding the granulocyte cell stimulating factor (G-CSF) it has been observed that plasma G-CSF levels are significantly lower at 7:00 am than at 7:00 pm in patients with chemotherapy induced leukopenia. The administration of G-CSF regulates the bone marrows rhythm production and granulopoiesis. There is a large debate regarding the optimal time administration of G-CSF for maximum production and there are more questions than answers. There are controversial data; however, morning administration is the best considered approach (20). Several studies presented data that tumor tissue has its own cell biology that is affected by the disease status and therapy response. Chrono-target aims to identify the rest time of normal cells and optimal circulation of specific metabolites depending of the anticancer drug administered. Parameters explored by chrono-target until now are: (I) Internal patient clock, (II) Circadian rhythm of cancer cells, and (III) daily circulation of metabolites and enzymes.
The normalization of the disrupted rhythm can be modified by a number of pharmacological and non-pharmacological methods. The innervations investigated are: (I) analgesics, (II) inhibition of tumor transcriptome with meal programming (5), (III) light treatment, (IV) melatonin, (V) modafinil, (VI) acupuncture, (VII) donepezil, (VIII) dexmethylphenidate, (IX) guarana, (X) erythropoietin, (XI) corticoid. The medical professional should seek for the previous mentioned sleep disorder solutions before investigating the circadian rhythm. The normalization of the circadian rhythm can add to the quality of life, since less behavioral disorders will be present. In addition, the chrono-target therapy would be easier applied. A tailored chrono-target treatment schedule should be followed in any case after diagnosis of the biological function of the patient, since the biologic clock of the cancer patient changes according to disease status/response.
Conclusions
Locoregional treatment modality aims to deposit anticancer treatment to the target site in order to induce apoptosis and at the same time decrease systematic adverse. Inhaled chemotherapy studies investigated whether smaller chemotherapy concentrations can be used with efficiency if deposited locally. As a result less systematic adverse effects are observed. Several delivery systems for sustained drug formulation release have been investigated, in order to have a prolonged therapeutic effect. To further augment the efficiency of anticancer therapies, additional parameters of lung cancer patients have been investigated. The sleep disturbances, circadian rhythm and tumor-biology have been well associated in many studies. Chrono-target administration of anticancer treatment according to the circadian rhythm of cancer patients has demonstrated efficiency and less systematic side effects indifferent of the high drug concentrations. This observation has been attributed to the fact that genes expression and protein production system is strongly associated with the circadian rhythm. The disrupted circadian rhythm inhibits optimal function of the gene/protein system and therefore the anticancer treatment results in low efficiency and high systematic toxicity. The toxic anticancer agents circulate for a longer period of without being deconstructed to their toxic metabolites. Moreover, several transporters that are incorporated to the efflux function of several cytotoxic agents are found in the airway system. Combining the local therapy with the normalization of the circadian rhythm (proper gene/protein) function, it can be speculated that efficiency and safety is observed. The optimal function of genes/proteins locally on the airway epithelium can enhance the antincancer drug administration and decrease chemotherapy side effects. Chrono-target administration, enhances the anticancer effects of chemotherapy, decreases the side effects and improves the quality of life by reducing the sleep disturbances of lung cancer patients.
Future perspective
The circadian rhythm is a powerful biological and behavioral modulator. Sleep disturbances in lung cancer patients disrupt the “internal clock” and therefore the disease progression is accelerated. Moreover, local therapies have demonstrated efficiency in many cancer types. The local microenvironment is also modified by the circadian rhythm (gene/protein system-function). It has been presented before that in many cancer types and indifferent of the disease status (initial/progressed) the chrono-target administration is an effective treatment modality to enhance anticancer effect. Lung cancer treatment during the last years is exploring the molecular pathways of the disease to “individualize” the treatment of these patients according to their genome (pharmacogenomics of tumor biology). Although a complex mode of administration, the chrono-target modality has much to offer additionally to the quality of life of the patient by reducing the side effects of the toxic chemotherapeutic agents and by eliminating sleep disorders. (Figure 1)
Figure 1.
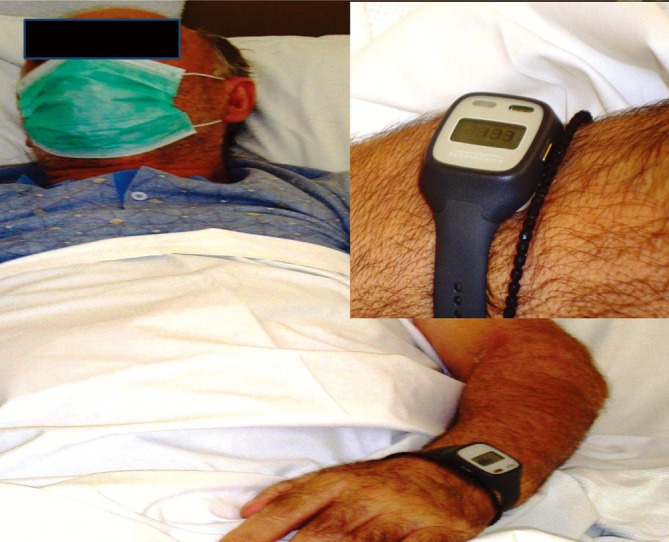
Photo by George Kalamaras (a lung cancer patient receiving before chemotherapy treatment). Actiwatch spectrum (Philips, Respironics) purchased by “Athromed Company” for Paul Zarogoulidis.
Executive summary
-Novel locoregional therapies are underway as a mode of administration to provide high efficiency by local administration of the drug formulation and to avoid unnecessary systemic side effects.
-Lung cancer patients have more severe sleep disorders than other cancer patients. The sleep disorders are correlated with disease burden and therefore their circadian rhythm is disrupted.
-Several pharmacological and non-pharmacological treatment modalities can be used to normalize the circadian rhythm of these patients.
-The tumor has its own biologic rhythm and all the biological growth parameters are accelerated by the disruptive circadian rhythm of the lung cancer patient.
-Chrono-target local therapy normalizes the “internal clock” and induces apoptosis. At the same time when the circadian rhythm is normalized the anticancer treatment is more effective with less systemic side effects.
Acknowledgements
Dr. Paul Zarogoulidis would like to thank the president of “Athromed Company” Mr. Stefanos Gogos for his help in acquiring the actiwatch spectrum wrist watches from Philips, Respironics.
Disclosure: The authors declare no conflict of interest.
References
- 1.Zarogoulidis P, Chatzaki E, Porpodis K, et al. Inhaled chemotherapy in lung cancer: future concept of nanomedicine. Int J Nanomedicine 2012;7:1551-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zarogoulidis P, Eleftheriadou E, Sapardanis I, et al. Feasibility and effectiveness of inhaled carboplatin in NSCLC patients. Invest New Drugs 2012;30:1628-40. [DOI] [PubMed] [Google Scholar]
- 3.Zarogoulidis P, Steiropoulos P, Perantoni E, et al. Subjective sleep quality in lung cancer patients before and after chemotherapy. Thoracic Cancer 2012. [Epud ahead of print]. [DOI] [PubMed] [Google Scholar]
- 4.Lévi F, Altinok A, Clairambault J, et al. Implications of circadian clocks for the rhythmic delivery of cancer therapeutics. Philos Transact A Math Phys Eng Sci 2008;366:3575-98. [DOI] [PubMed] [Google Scholar]
- 5.Li XM, Delaunay F, Dulong S, et al. Cancer inhibition through circadian reprogramming of tumor transcriptome with meal timing. Cancer Res 2010;70:3351-60. [DOI] [PubMed] [Google Scholar]
- 6.Lévi F, Focan C, Karaboué A, et al. Implications of circadian clocks for the rhythmic delivery of cancer therapeutics. Adv Drug Deliv Rev 2007;59:1015-35. [DOI] [PubMed] [Google Scholar]
- 7.Miaskowski C, Lee K, Dunn L, et al. Sleep-wake circadian activity rhythm parameters and fatigue in oncology patients before the initiation of radiation therapy. Cancer Nurs 2011;34:255-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buysse DJ, Reynolds CF, 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193-213. [DOI] [PubMed] [Google Scholar]
- 9.Craver LF. The nitrogen mustards; clinical use. Radiology 1948;50:486-93. [DOI] [PubMed] [Google Scholar]
- 10.Lee KA. Self-reported sleep disturbances in employed women. Sleep 1992;15:493-8. [DOI] [PubMed] [Google Scholar]
- 11.Lee KA, Hicks G, Nino-Murcia G. Validity and reliability of a scale to assess fatigue. Psychiatry Res 1991;36:291-8. [DOI] [PubMed] [Google Scholar]
- 12.Cimprich B.Attentional fatigue following breast cancer surgery. Res Nurs Health 1992;15:199-207. [DOI] [PubMed] [Google Scholar]
- 13.Tsara V, Serasli E, Amfilochiou A, et al. Greek version of the Epworth Sleepiness Scale. Sleep Breath 2004;8:91-5. [DOI] [PubMed] [Google Scholar]
- 14.Katsarou Z, Bostantjopoulou S, Hatzizisi O, et al. Immune factors or depression? Fatigue correlates in Parkinson's disease. Rev Neurol 2007;45:725-8. [PubMed] [Google Scholar]
- 15.Stenton C.The MRC breathlessness scale. Occup Med (Lond) 2008;58:226-7. [DOI] [PubMed] [Google Scholar]
- 16.Leclerc J, Courcot-Ngoubo Ngangue E, Cauffiez C, et al. Xenobiotic metabolism and disposition in human lung: transcript profiling in non-tumoral and tumoral tissues. Biochimie 2011;93:1012-27. [DOI] [PubMed] [Google Scholar]
- 17.Okyar A, Piccolo E, Ahowesso C, et al. Strain- and sex-dependent circadian changes in abcc2 transporter expression: implications for irinotecan chronotolerance in mouse ileum. PLoS One 2011;6:e20393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bouchahda M, Adam R, Giacchetti S, et al. Rescue chemotherapy using multidrug chronomodulated hepatic arterial infusion for patients with heavily pretreated metastatic colorectal cancer. Cancer 2009;115:4990-9. [DOI] [PubMed] [Google Scholar]
- 19.Innominato PF, Focan C, Gorlia T, et al. Circadian rhythm in rest and activity: a biological correlate of quality of life and a predictor of survival in patients with metastatic colorectal cancer. Cancer Res 2009;69:4700-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sato S, Kigawa J, Irie T, et al. Timing of G-CSF administration based on the circadian rhythm in patients with ovarian cancer. Am J Clin Oncol 2002;25:289-90. [DOI] [PubMed] [Google Scholar]


