Abstract
Since the 1995 report of the prospective randomized trial of lobectomy versus sublobar resection for stage I non-small cell lung cancer (NSCLC) performed by the the Lung Cancer Study Group, lobectomy remains the standard of care for the surgical management of stage I NSCLC. Sublobar resection has been typically used for high-risk patients who are operative candidates but for whom a lobectomy is contraindicated. Recent advances in imaging and staging modalities and improved spatial resolution of computed tomography (CT) scan have refined the presentation and diagnosis of early-stage NSCLC. The detection of small tumors and ground-glass opacity (GGO) appearance associated with a favorable histology have led to the increased use of sublobar resection in many institutes to include good-risk patients. There is an increasing body of evidence that sublobar resection may achieve oncological outcomes similar to those with lobectomy in early-stage NSCLC, especially that 2 cm or less in size. However, whether or not sublobar resection constitutes adequate treatment for small-sized lung cancer or for the radiographic “early” lung cancer such as a GGO-dominant lesion is still being prospectively investigated. Sublobar resection will be expected to play an important role as a primary treatment option for patients with small stage IA NSCLC, based on an anatomical functional advantage over lobectomy as well as comparable prognostic outcomes between sublobar resection and lobectomy.
Keywords: Non-small cell lung cancer (NSCLC), sublobar resection, prognosis, early-stage lung cancer, surgery
Introduction
In 1995, the Lung Cancer Study Group (LCSG) reported the only randomized trial that compared lobectomy to sublobar resection for the treatment of stage IA non-small cell lung cancer (NSCLC) (1,2). They found an increased risk for locoregional recurrence, a reduced 5-year survival rate, and no statistical evidence for the preservation of pulmonary function, and thereby disproved the speculation that sublobar resection had an outcome that was comparable to that of lobectomy, and reinforced the need for lobectomy in early-stage patients. Thus, sublobar resection was considered to be a “compromise” operation for high-risk patients who were not candidates for lobectomy because of advanced age, severely impaired pulmonary function, or other comorbidity (3-7).
Although lobectomy remains the standard of care for patients with stage IA NSCLC, recent advances in clinical imaging/staging modalities and the increased identification of smaller tumors by computed tomography (CT) screening have led to a resurgence of interest in sublobar resection for these tumors (8-13). Several recent studies have demonstrated comparable recurrence and survival rates for lobectomy and sublobar resection, even in good-risk patients with small stage I lung cancer (14-18). In addition, due to improvements in CT resolution, a ground-glass opacity (GGO) appearance on thin-section CT (TSCT) has been reported to be associated with a favorable histology such as non- or minimally-invasive adenocarcinoma in lung cancer (19-21). These GGO lesions are also likely to be amenable to sublobar resection.
If sublobar resection is equivalent to lobectomy with respect to their oncological results for the surgical treatment of lung cancer, the potential benefits of sublobar resection include the preservation of vital lung tissue and a chance for a second resection with a subsequent primary tumor. Thus, sublobar resection plays an important role in the surgical treatment of patients with NSCLC who are diagnosed at an early stage.
This article reviews the current status of sublobar resection for early-stage NSCLC, with particular attention to issues such as tumor size, type of sublobar resection (segmentectomy versus wedge resection), surgical margin, radiology-pathology correlation, and pulmonary function.
History
In the early half of the 20th century, pneumonectomy was considered the only appropriate treatment for primary lung cancer. However, due to the unacceptably high mortality rate associated with pneumonectomy at that time, lobectomy evolved as the treatment of choice for resectable lung cancers. As a further extension of the anatomic approach to lung resection, thoracic surgeons began to explore the use of segmentectomy for early-stage lung cancer in high-risk patients (22-26). Subsequently, many studies reported that segmentectomy was useful as a compromise operation in selected, high-risk patients (3,27,28), since Jensik and colleagues first described its use for lung cancer resection in 1973 (22). Several of these studies advocated sublobar resection (wedge resection or segmentectomy) as an appropriate treatment for patients with early-stage lung cancer (3,27).
Due to speculation about the prospect of sublobar resection for early-stage NSCLC, the Lung Cancer Study Group (LCSG) conducted a prospective, randomized trial that compared lobectomy to sublobar resection for the treatment of clinical T1N0 NSCLC, and the results were published in 1995 (1). This trial demonstrated a 3-fold increase in local recurrence and a decrease in overall survival after sublobar resection. Consequently, the need for formal lobectomy in early-stage NSCLC was reinforced. Since this publication, many studies have retrospectively supported these results; i.e., lobectomy offers an overall and disease-free survival advantage (Table 1) (1,15,29-43).
Table 1. Survival data in studies that compared sublobar resection to lobectomy for patients with NSCLC.
| Author [year] | Study design | No. of Patients | Stage | Compromised vs. intentional | Type of sublobar resection | Mortality (%) |
5-YSR |
Local rec. rate |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lobectomy | Sublobar resection | Lobectomy (%) | Sublobar resection (%) | P | Lobectomy (%) | Sublobar resection (%) | P | ||||||||
| LCSG [1995] | Pros.; phase III | 247 | IA | Intentional | Wedge: 40; Seg.: 82 | 1.6 | 0.8 | 69 | 60 | 0.08 | 6.4 | 17 | 0.079 | ||
| Koike [2003] | Pros.; non-randomized | 233 | IA (≤2 cm) | Intentional | Wedge: 14; Seg.: 60 | 0 | 0 | 90.1 | 89.1 | NS | 1.3 | 2.7 | NS | ||
| Campione [2004] | Retro. | 120 | IA | Compromised | Seg.: 21 | 3 | 9.5 | 65 | 62 | NS | 2 | 19 | – | ||
| Keenan [2004] | Retro. | 201 | I | Compromised | Seg.: 54 | 4.8 | 5.6 | 67 (4-YSR) | 62 (4-YSR) | NS | 7.5 | 11.1 | NS | ||
| Martin-Ucar [2005] | Retro.; propensity matched study | 34 | I | N/R | Seg.: 17 | 5.8 | 5.8 | 64 | 70 | NS | 2 | 0 | NS | ||
| El-Sherif [2006] | Retro. | 784 | I | Compromised | Wedge: 122; Seg.: 85 | – | – | 54 | 40 | 0.0038 | 4.2 | 7.2 | 0.0204 | ||
| Chang [2007] | Retro.; SEER database | 10,761 | IA | N/R | Sublobar: 2,234 | – | – | 61.4 | 44.0 | <0.0001 | – | – | – | ||
| Iwasaki [2007] | Retro. | 86 | <2 cm | Mixed | Seg.: 31 | 0 | 0 | 73 | 70 | NS | 3.6 | 3.2 | NS | ||
| Kraev [2007] | Retro. | 289 | I | Compromised | Wedge: 74 | – | – | 5.8 years (MST) | 4.1 years (MST) | NS | – | – | – | ||
| Sienel [2007] | Retro. | 199 | IA | Compromised | Seg.: 49 | – | – | 83 | 67 | 0.01 | 5 | 16 | 0.005 | ||
| Kilic [2009] | Retro. | 184 (age >75) | I | Compromised | Seg.: 78 | 4.7 | 1.3 | 47 | 46 | NS | 4 | 6 | NS | ||
| Billmeier [2011] | Retro. | 679 | I-II | Mixed | Wedge: 120; Seg.: 35 | 1.9 | 7.1 | 57 | 49 | NS | – | – | – | ||
| Wolf [2011] | Retro. | 238 | ≤2 cm | Compromised | Wedge: 130; Seg.: 24 | 4 | 0. | 80 | 59 | 0.0027 | 8 | 16 | NS | ||
| Varlotto [2013] | Retro. | 411 | I | Compromised | Wedge: 79; Seg.: 14 | – | – | 64.5 | 54.5 | NS | 24.6 | 39.5 | NS | ||
| Altorki [2014] | Retro. | 347 | IA | Compromised | Wedge: 37; Seg.: 16 | 1 | 0 | 86 | 85 | NS | – | – | – | ||
| Okada [2014] | Retro. | 634 | IA | Mixed | Seg.: 155 | 0 | 94.1 (3-YSR) | 95.7 (3-YSR) | NS | 3.5 | 1.9 | – | |||
| Tsutani [2014] | Retro. | 239 | IA (>50% GGO) | N/R | Wedge: 93; Seg.: 56 | 0 | 0 | 97.6 | Wedge: 98.7; Seg.: 98.2 | NS | 0 | 0 | – | ||
NSCLC, non-small cell lung cancer; 5-YSR, 5-year survival rate; LCSG, Lung Cancer Study Group; Pros., prospective study; Seg., segmentectomy; Retro., retrospective study; NS, not significant; N/R, not reported; SEER, Surveillance, Epidemiology, and End Results; MST, median survival time; GGO, ground-glass opacity.
However, the 1995 LCSG study (1) received several major criticisms: (I) a high percentage of patients in the sublobar group underwent wedge resection other than anatomic segmentectomy; (II) routine chest CT examination was not required either preoperatively or for postoperative surveillance; (III) the difference in the prognosis between sublobar and lobar resections was relatively small; (IV) the analysis regarding the preservation of postoperative pulmonary function was inadequate between sublobar and lobar resections, and so on (16,44). In addition, recent advances in imaging and staging modalities and the detection of smaller tumors by TSCT scan have rekindled interest in sublobar resection for early-stage NSCLC. Thus, single-institutional retrospective investigations have demonstrated that sublobar resection is equivalent to lobectomy in patients with early-stage NSCLC and especially for smaller tumors (2 cm or less in diameter) (14,15,45,46). Currently, two prospective, randomized, multi-institutional phase III trials are being conducted by the Cancer and Leukemia Group B (CALGB 140503) and the Japan Clinical Oncology Group (JCOG 0802) (47). Additionally, according to the correlation between TSCT findings and the pathology of lung cancer, lung nodules with a GGO appearance on TSCT have been considered to be “early” lung adenocarcinoma (6,48). Whether or not sublobar resection constitutes adequate treatment for small peripheral cancer in general or for tumors in which the preoperative radiographic features suggest an “early” adenocarcinoma is still being investigated.
Tumor size
It is well known that tumor size is a recognized prognostic variable in NSCLC (49). Over the past decade, many studies have demonstrated improved survival and local control for patients with T1N0 tumors of 2 cm or smaller compared with larger tumors (11,30,50), although the LCSG trial (1) showed no survival advantage based on tumor size. Data from the recent lung cancer staging project headed by the International Association for the Study of Lung Cancer (IASLC) also found an improvement in survival for stage IA tumors less than 2 cm in diameter compared with those 2 to 3 cm in size and led to the reclassification of T1 tumors in the revised staging system (51,52). In this revision, tumors that measure 2 cm or less are considered to be T1a and those of 2 to 3 cm are T1b (52). The appropriateness of sublobar resection for small lung tumors, especially those 2 cm or less in size, has recently been addressed by many researchers. Table 2 summarizes the results of sublobar resection for NSCLC ≤2 cm (14-17,34,36,39,45,53-56). There is a growing body of evidence that sublobar resection may achieve oncological outcomes similar to those with lobectomy in this setting of smaller tumors. Patients with NSCLC of 2 cm or smaller may represent a population in whom sublobar resection should be considered.
Table 2. Evidence for survival after sublobar resection for cT1N0M0 NSCLC of 2 cm or less in size.
| Author [year] | No. of patients | Intentional vs. compromised | Mode of sublobar resection | 5-YSR (%) | Local rec. rate (%) |
|---|---|---|---|---|---|
| Kodama [1997] | 46 (<3 cm in size) | Intentional | Seg. | 93.0 | 8.7 |
| Okada [2001] | 70 | Intentional | Extended seg.* | 87.3 | 0 |
| Koike [2003] | 74 | Intentional | Wedge: 14; Seg.: 60 | 89.1 | 2.7 |
| Fernando [2005] | 124 | Compromised | Wedge: 52; Seg.: 73 | 55.8 mo; (MST) | 17.5 |
| Okada [2006] | 260 | Intentional | Wedge: 30; Seg.: 230 | 89.6 | 4.9 |
| Iwasaki [2007] | 31 | Mixed | Seg. | 69.7 | 3.2 |
| Sienel [2007] | 32 | Compromised | Seg. | 68 | 12 |
| Schuchert [2007] | 182 (IA/IB) | N/R | Seg. | 82 | 7.7 |
| Bando [2009] | 68 | Mixed | Seg. | 86.0 | – |
| Watanabe [2009] | 38 | Intentional | Seg. | 74.5 | 0 |
| Wolf [2011] | 154 | Compromised | Wedge: 130; Seg.: 24 | 59 | 16 |
| Donahue [2012] | 40 | Mixed | Seg. | 68.8%, DFS | 5 |
NSCLC, non-small cell lung cancer; 5-YSR, 5-year survival rate; Seg., segmentectomy; MST, median survival time; N/R, not reported; DFS, disease-free survival. *, Extended segmentectomy is defined as resection of both the affected segment and adjacent subsegments plus the exploration of mediastinal and hilar lymph nodes by intraoperative frozen sectioning.
Type of sublobar resection (segmentectomy versus wedge resection)
The most common operative approaches for sublobar resection are wedge resection and segmentectomy. Wedge resection consists of the removal of a lung tumor with a surrounding margin of normal lung tissue, and is not an anatomical resection. On the other hand, segmentectomy is an anatomical resection that usually includes one or more pulmonary parenchymal segments with the dissection of intraparenchymal and hilar lymph nodes. Segmentectomy theoretically has the advantages of a wider resection, reduced technical limitations for achieving adequate margins (57), and the more extensive resection of draining lymphatics including intersegmental planes that are commonly considered to be a source of residual cancer cells (58). Many reports have suggested that nonanatomic wedge resection is inferior to anatomic segmentectomy as an oncologic approach (9,59). Actually, these reports found a significant increase in local recurrence and a decrease in survival after wedge resection compared with segmentectomy for especially stage I NSCLC (Table 3) (50,60-63). The superiority of segmentectomy with regard to the parenchymal margin has been documented in prior studies (57,61). For example, a study from the University of Pittsburgh retrospectively reviewed 81 patients who were treated with sublobar resection. Among the patients with wedge resection, only 39% had a margin greater than 1 cm, compared with 73% of those with segmentectomy (61). Consequently, the incidence of local recurrence was significantly higher in the wedge resection group. A prospective study by Kent et al. reached a similar result that wedge resection had a significantly smaller surgical margin than segmentectomy for non-small lung cancer (57). The inadequate surgical margins in wedge resection would result in a higher incidence of local recurrence (64). Sawabata et al. (65) and Shuchert et al. (54) identified a margin distance of greater than 2 cm or greater than the maximal tumor diameter as favorable indicators of decreased local recurrence after lung resection.
Table 3. Outcome after wedge resection and segmentectomy for NSCLC.
| Author [year] | No. of patients | Stage | Compromised vs. intentional | Resection type | 5-YSR |
Local rec. rate (%) |
|||
|---|---|---|---|---|---|---|---|---|---|
| Wedge | Seg. | Wedge | Seg. | ||||||
| Miller [2002] | 25 | ≤1 cm | Compromised | Wedge: 13; Seg.: 12 | 27% | 57% | 30.8 | 8.3 | |
| Okada [2005] | 158 | IA (≤2 cm) | Mixed | Wedge: 35; Seg.: 123 | 85.7% | 96.7% | N/R | N/R | |
| El-Sherif [2007] | 81 | I | Compromised | Wedge: 55; Seg.: 26 | N/R | N/R | 14.5 | 3.8 | |
| Sienel [2008] | 87 | IA | Compromised | Wedge: 31; Seg.: 56 | 48%; cancer-related | 71%; cancer-related | 55 | 16 | |
| Koike [2014] | 328 | IA | Mixed | Wedge: 112; Seg.: 216 | 68.0%; disease-specific | 91.3%; disease-specific | 34 | 6.3 | |
NSCLC, non-small cell lung cancer; 5-YSR, 5-year survival rate; Seg., segmentectomy; N/R, not reported.
With respect to radiologic findings, based on the advent of high-resolution CT or TSCT, the radiology-pathology correlation has been studied (19,21,66), and the radiologic appearance of the various histologic subtypes in lung cancer, especially adenocarcinoma, has been described in detail (67). It has been shown that the lesions with GGO are more likely to be “early” adenocarcinomas such as adenocarcinoma in situ (AIS), or minimally invasive adenocarcinoma (MIA). Recent studies demonstrated that patients with GGO-dominant lung adenocarcinoma (consolidation/tumor ratio ≤0.5 on TSCT scan; Figure 1) of clinical stage I have an excellent prognosis (19,68). These tumors might be curatively treated with sublobar resection such as wedge resection or segmentectomy.
Figure 1.
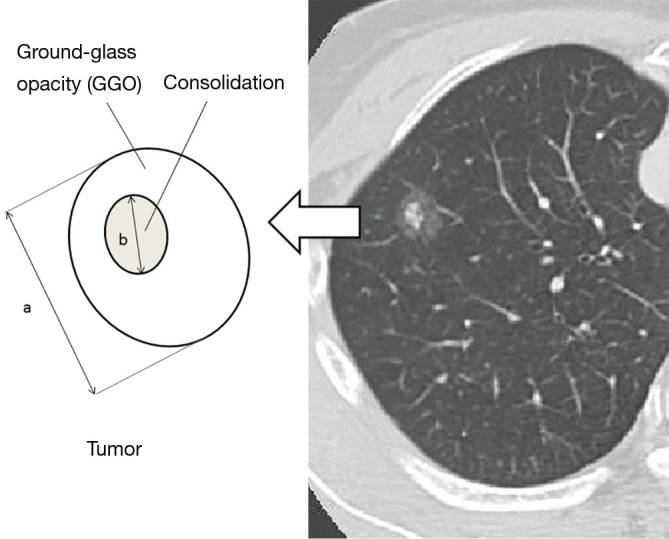
Calculation of the consolidation/tumor ratio to define radiologic noninvasive lung cancer on thin-section computed tomography. The maximum diameter of consolidation (b) is divided by the maximum tumor diameter (a) to give the consolidation/tumor ratio.
Intentional sublobar resection
Lobectomy has been the standard of care for early-stage NSCLC since the 1995 report from the LCSG (1). Many studies have retrospectively supported this result, and have indicated that lobectomy carries an overall and disease-free survival advantage when compared to sublobar resection (32,33,36,69). Consequently, sublobar resection has typically been used for high-risk, but still operable, patients with lung cancer. However, recent improvements in the detection of small peripheral tumors and GGOs associated with a favorable histology have led to the increased use of sublobar resection in many centers to include patients with an adequate physiologic reserve.
GGO is defined as a hazy increased attenuation with the preservation of bronchial and vascular margins on TSCT (70). It has been proposed that lung cancer with dominant GGO (consolidation/tumor ratio 0.5 or less) within the lesion is more likely to be an early form of adenocarcinoma such as AIS or MIA (19,21). In particular, some GGOs are accompanied by a solid part (consolidation), and it has been demonstrated that a consolidation represents the portion of invasive growth, i.e., the consolidation/tumor ratio is thought to predict pathologic early adenocarcinoma (21). On the basis of these observations, the Japan Clinical Oncology Group (JCOG) 0201 study (48), a multi-institutional prospective study, was planned to establish radiologic criteria for predicting pathologic early (noninvasive) adenocarcinoma. Based on the results of this study, radiologic noninvasive lung adenocarcinoma could be defined as an adenocarcinoma ≤2.0 cm (cT1a) with a consolidation/tumor (C/T) ratio of 0.25 or less. Subsequently, Asamura and colleagues (68) reevaluated the radiology-pathology correlation in the JCOG 0201 study in terms of the prognosis. The radiologic criteria of a C/T ratio of 0.5 or less in cT1a-b (≤3.0 cm) as well as 0.25 or less in cT1a (≤2.0 cm) could be used to define a homogeneous group of patients with an excellent prognosis after surgery. These criteria can be used to select patients with early lung adenocarcinoma in whom a sublobar resection such as wedge resection or segmentectomy would be safely indicated. Clinical phase II trials to determine the appropriateness of intentional sublobar resection for “early” adenocarcinoma with these radiologic criteria have been conducted (JCOG 0804 and JCOG 1211).
On the other hand, for radiologic invasive lung cancer (cT1aN0M0) with a tumor diameter of 2.0 cm or less and a C/T ratio greater than 0.5, a prospective, randomized phase III study (JCOG0802/WJOG4607L) that compares lobectomy and segmentectomy in a noninferiority setting is ongoing (47). The primary and main secondary end-points are overall survival and postoperative pulmonary function, relapse-free survival, and proportion of local recurrence. This study began in August 2009 in Japan and a total of 1,100 patients will be accrued. Intraoperatively, the distance from the surgical resected margin to the tumor edge and lymph node must be evaluated. When lymph node metastasis is present or the resected margin is not cancer-free, the surgical procedure must be converted to a lobectomy. All randomized patients will be followed for at least five years. In North America, a similar trial entitled CALGB 140503 is also underway, in which the prognosis and preservation of pulmonary function are being compared in lobectomy and sublobar resection (segmentectomy or wedge resection) in a noninferiority study setting.
Postoperative pulmonary function
If we wish to advocate sublobar resection for early-stage lung cancer, it must offer some clinically significant advantage in comparison to lobectomy. The preservation of pulmonary function is one such meaningful advantage. Theoretically, sublobar resection such as segmentectomy has an anatomically functional advantage over lobectomy, since some segments of lung parenchyma that would otherwise be removed by lobectomy can be preserved. However, it is unclear whether the functional advantage of segmentectomy is as great as its anatomic advantage over lobectomy. In the 1995 LCSG trial (1), a preservation of pulmonary function was demonstrated for patients who underwent sublobar resection compared with lobectomy at 6 months after surgery, but not at 8 or 12 months. However, this may have been due to the loss of follow-up pulmonary function tests for many patients at this longer interval evaluation. Nevertheless, the increasing body of evidence of comparable prognostic outcomes between lobectomy and sublobar resection for small tumors has prompted surgeons to more exhaustively investigate their impact on postoperative pulmonary function (17,30,71). Takizawa and colleagues (72) retrospectively studied pre- and post-operative pulmonary function [forced expiratory volume in 1 second (FEV1.0) and forced vital capacity (FVC)] in 40 segmentectomy patients and 40 paired lobectomy patients, who were matched with respect to the estimated propensity score. The significant benefit in FEV1.0, but not that in FVC, as a percentage of the preoperative value, observed two weeks postoperatively in the group of patients who had undergone segmentectomy (segmentectomy group 73.0% versus lobectomy group 66.6%, P=0.03) was maintained at 12 months (segmentectomy group 93.0% versus lobectomy group 87.3%, P=0.03). Harada and colleagues (73) analyzed pulmonary function tests preoperatively and at 2 and 6 months after segmentectomy in 38 patients and after lobectomy in 45 patients, where both groups could tolerate a lobectomy and had clinical T1N0M0 NSCLC ≤2 cm. In the segmentectomy group, the postoperative reductions in FVC and FEV1.0 were significantly smaller than those in the lobectomy group. On the other hand, a recent report by Deng and colleagues (74) failed to find a significant difference in the effect on pulmonary function after segmentectomy or lobectomy. Since these results were mainly derived from retrospective studies, the preservation of postoperative pulmonary function with sublobar resection should be confirmed in a prospective study based on adequate postoperative follow-up pulmonary function data.
Conclusions
The number of patients who present with small tumors continues to increase due to the prevalence of CT screening. This should lead to a notable increase in the detection of tumors smaller than those included in the LCSG trial (1), which was conducted in the 1980s and based on the detection of lung cancer by plain chest radiography. Additionally, a recent report from the National Lung Screening trial demonstrated that CT screening for lung cancer reduced relative lung cancer mortality compared with screening by chest radiography (75). Sublobar resection will be expected to play an important role as a primary treatment option for patients with small stage IA NSCLC, especially if 2 cm or less in size, who can tolerate a lobectomy. However, care should be taken in promoting widespread indications for intentional segmentectomy in good-risk patients with a small tumor until the results of ongoing prospective, randomized clinical trials, such as JCOG0802/WJOG4607L and CALGB140503, are available (47). If these trials demonstrate that lobectomy and sublobar resection have similar curative effects and that sublobar resection offers better pulmonary functional preservation, sublobar resection should take the place of a lobectomy as the standard of care for patients with early-stage NSCLC.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22; discussion 622-3. [DOI] [PubMed] [Google Scholar]
- 2.Lederle FA. Lobectomy versus limited resection in T1 N0 lung cancer. Ann Thorac Surg 1996;62:1249-50. [DOI] [PubMed] [Google Scholar]
- 3.Pastorino U, Valente M, Bedini V, et al. Limited resection for stage I lung Cancer. Eur J Surg Oncol 1991;17:42-6. [PubMed] [Google Scholar]
- 4.Date H, Ando A, Shimizu N.The value of limited resection for “clinical” stage I peripheral non-small cell lung cancer in poor-risk patients: comparison of limited resection and lobectomy by a computer-assisted matched study. Tumori 1994;80:422-6. [DOI] [PubMed] [Google Scholar]
- 5.Mery CM, Pappas AN, Bueno R, et al. Similar long-term survival of elderly patients with non-small cell lung cancer treated with lobectomy or wedge resection within the surveillance, epidemiology, and end results database. Chest 2005;128:237-45. [DOI] [PubMed] [Google Scholar]
- 6.Griffin JP, Eastridge CE, Tolley EA. Wedge resection for non-small cell lung cancer in patients with pulmonary insufficiency: prospective ten-year survival. J Thorac Oncol 20061:960-4. [PubMed] [Google Scholar]
- 7.LoCicero J 3rd. Surgical treatment of non-small-cell lung cancer: In: Shields TW, LoCicero J, Reed CE, Feins RH, eds. General thoracic surgery. 7th ed. Philadelphia: Lippincott Williams and Wilkins, 2009:1387-425. [Google Scholar]
- 8.Rami-Porta R, Tsuboi M.Sublobar resection for lung cancer. Eur Respir J 2009;33:426-35. [DOI] [PubMed] [Google Scholar]
- 9.Blasberg JD, Pass HI, Donington JS. Sublobar resection. A movement from the Lung Cancer Study Group. J Thorac Oncol 2010;5:1583-93. [DOI] [PubMed] [Google Scholar]
- 10.Schuchert MJ, Abbas G, Pennathur A, et al. Sublobar resection for early-stage lung cancer. Semin Thorac Cardiovasc Surg 2010;22:22-31. [DOI] [PubMed] [Google Scholar]
- 11.Narsule CK, Ebright MI, Fernando HC. Sublobar versus lobar resection. Current status. Cancer J 2011;17:23-7. [DOI] [PubMed] [Google Scholar]
- 12.Donington JS. Current readings: sublobar resection for non-small-cell lung cancer. Semin Thorac Cardiovasc Surg 2013;25:22-9. [DOI] [PubMed] [Google Scholar]
- 13.Cao C, Gupta S, Chandrakumar D, et al. Meta-analysis of intentional sublobar resections versus lobectomy for early stage non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:134-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kodama K, Doi O, Higashiyama M, et al. Intentional limited resection for selected patients with T1 N0 M0 non-small-cell lung cancer: a single-institution study. J Thorac Cardiovasc Surg 1997;114:347-53. [DOI] [PubMed] [Google Scholar]
- 15.Koike T, Yamato Y, Yoshiya K, et al. Intentional limited pulmonary resection for peripheral T1 N0 M0 small-sized lung cancer. J Thorac Cardiovasc Surg 2003;125:924-8. [DOI] [PubMed] [Google Scholar]
- 16.Okada M, Koike T, Higashiyama M, et al. Radical sublobar resection for small-sized non-small cell lung cancer: a multicenter study. J Thorac Cardiovasc Surg 2006;132:769-75. [DOI] [PubMed] [Google Scholar]
- 17.Watanabe A, Ohori S, Nakashima S, et al. Feasibility of video-assisted thoracoscopic surgery segmentectomy for selected peripheral lung carcinomas. Eur J Cardiothorac Surg 2009;35:775-80. [DOI] [PubMed] [Google Scholar]
- 18.Dembitzer FR, Flores RM, Parides MK, et al. Impact of Histological Subtyping on Outcome in Lobar versus Sublobar Resections for Lung Cancer: A Pilot Study. Chest 2014. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 19.Suzuki K, Asamura H, Kusumoto M, et al. “Early” peripheral lung cancer: prognostic significance of ground glass opacity on thin-section computed tomographic scan. Ann Thorac Surg 2002;74:1635-9. [DOI] [PubMed] [Google Scholar]
- 20.Sakurai H, Dobashi Y, Mizutani E, et al. Bronchioloalveolar carcinoma of the lung 3 centimeters or less in diameter: a prognostic assessment. Ann Thorac Surg 2004;78:1728-33. [DOI] [PubMed] [Google Scholar]
- 21.Asamura H.Minimally invasive approach to early, peripheral adenocarcinoma with ground-glass opacity appearance. Ann Thorac Surg 2008;85:S701-4. [DOI] [PubMed] [Google Scholar]
- 22.Jensik RJ, Faber LP, Milloy FJ, et al. Segmental resection for lung cancer. A fifteen-year experience. J Thorac Cardiovasc Surg 1973;66:563-72. [PubMed] [Google Scholar]
- 23.Bennett WF, Smith RA. Segmental resection for bronchogenic carcinoma: a surgical alternative for the compromised patients. Ann Thorac Surg 1979;27:169-72. [DOI] [PubMed] [Google Scholar]
- 24.Hoffmann TH, Ransdell HT. Comparison of lobectomy and wedge resection for carcinoma of the lung. J Thorac Cardiovasc Surg 1980;79:211-7. [PubMed] [Google Scholar]
- 25.Errett LE, Wilson J, Chiu RC, et al. Wedge resection as an alternative procedure for peripheral bronchogenic carcinoma in poor-risk patients. J Thorac Cardiovasc Surg 1985;90:656-61. [PubMed] [Google Scholar]
- 26.Miller JI, Hatcher CR. Limited resection of bronchogenic carcinoma in the patient with marked impairment of pulmonary function. Ann Thorac Surg 1987;44:340-3. [DOI] [PubMed] [Google Scholar]
- 27.Read RC, Yoder G, Schaeffer RC. Survival after conservative resection for T1 N0 M0 non-small cell lung cancer. Ann Thorac Surg 1990;49:391-8; discussion 399-400. [DOI] [PubMed] [Google Scholar]
- 28.Warren WH, Faber LP. Segmentectomy versus lobectomy in patients with stage I pulmonary carcinoma. Five-year survival and patterns of intrathoracic recurrence. J Thorac Cardiovasc Surg 1994;107:1087-93; discussion 1093-4. [PubMed] [Google Scholar]
- 29.Campione A, Ligabue T, Luzzi L, et al. Comparison between segmentectomy and larger resection of stage IA non-small cell lung carcinoma. J Cardiovasc Surg (Torino) 2004;45:67-70. [PubMed] [Google Scholar]
- 30.Keenan RJ, Landreneau RJ, Maley RH, et al. Segmental resection spares pulmonary function in patients with stage I lung cancer. Ann Thorac Surg 2004;78:228-33. [DOI] [PubMed] [Google Scholar]
- 31.Martin-Ucar AE, Nakas A, Pilling JE, et al. A case-matched study of anatomical segmentectomy versus lobectomy for stage I lung cancer in high-risk patients. Eur J Cardiothorac Surg 2005;27:675-9. [DOI] [PubMed] [Google Scholar]
- 32.El-Sherif A, Gooding WE, Santos R, et al. Outcomes of sublobar resection versus lobectomy for stage I non-small cell lung cancer: a 13-year analysis. Ann Thorac Surg 2006;82:408-15; discussion 415-6. [DOI] [PubMed] [Google Scholar]
- 33.Chang MY, Mentzer SJ, Colson YL, et al. Factors predicting poor survival after resection of stage IA non-small cell lung cancer. J Thorac Cardiovasc Surg 2007;134:850-6. [DOI] [PubMed] [Google Scholar]
- 34.Iwasaki A, Hamanaka W, Hamada T, et al. Comparison between a case-matched analysis of left upper lobe trisegmentectomy and left upper lobectomy for small size lung cancer located in the upper division. Thorac Cardiovasc Surg 2007;55:454-7. [DOI] [PubMed] [Google Scholar]
- 35.Kraev A, Rassias D, Vetto J, et al. Wedge resection vs lobectomy. 10-year survival in stage I primary lung cancer. Chest 2007;131:136-40. [DOI] [PubMed] [Google Scholar]
- 36.Sienel W, Stremmel C, Kirschbaum A, et al. Frequency of local recurrence following segmentectomy of stage IA non-small cell lung cancer is influenced by segment localisation and width of resection margins--implications for patient selection for segmentectomy. Eur J Cardiothorac Surg 2007;31:522-7; discussion 527-8. [DOI] [PubMed] [Google Scholar]
- 37.Kilic A, Schuchert MJ, Pettiford BL, et al. Anatomic segmentectomy for stage I non-small cell lung cancer in the elderly. Ann Thorac Surg 2009;87:1662-6; discussion 1667-8. [DOI] [PubMed]
- 38.Billmeier SE, Ayanian JZ, Zaslavsky AM, et al. Predictors and outcomes of limited resection for early-stage non-small cell lung cancer. J Natl Cancer Inst 2011;103:1621-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wolf AS, Richards WG, Jaklitsch MT, et al. Lobectomy versus sublobar resection for small (2 cm or less) non-small cell lung cancers. Ann Thorac Surg 2011;92:1819-23; discussion 1824-5. [DOI] [PubMed]
- 40.Varlotto JM, Medford-Davis LN, Recht A, et al. Identification of stage I non-small cell lung cancer patients at high risk for local recurrence following sublobar resection. Chest 2013;143:1365-77. [DOI] [PubMed] [Google Scholar]
- 41.Altorki NK, Yip R, Hanaoka T, et al. Sublobar resection is equivalent to lobectomy for clinical stage 1A lung cancer in solid nodules. J Thorac Cardiovasc Surg 2014;147:754-62; Discussion 762-4. [DOI] [PubMed] [Google Scholar]
- 42.Okada M, Mimae T, Tsutani Y, et al. Segmentectomy versus lobectomy for clinical stage IA lung adenocarcinoma. Ann Cardiothorac Surg 2014;3:153-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tsutani Y, Miyata Y, Nakayama H, et al. Appropriate sublobar resection choice for ground glass opacity-dominant clinical stage IA lung adenocarcinoma. Wedge resection or segmentectomy. Chest 2014;145:66-71. [DOI] [PubMed] [Google Scholar]
- 44.Villamizar N, Swanson SJ. Lobectomy vs. segmentectomy for NSCLC (T < 2 cm). Ann Cardiothorac Surg 2014;3:160-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Okada M, Yoshikawa K, Hatta T, et al. Is segmentectomy with lymph node assessment an alternative to lobectomy for non-small cell lung cancer of 2 cm or smaller? Ann Thorac Surg 2001;71:956-60; discussion 961. [DOI] [PubMed] [Google Scholar]
- 46.Wisnivesky JP, Henschke CI, Swanson S, et al. Limited resection for the treatment of patients with stage IA lung cancer. Ann Surg 2010;251:550-4. [DOI] [PubMed] [Google Scholar]
- 47.Nakamura K, Saji H, Nakajima R, et al. A phase III randomized tial of lobectomy versus limited resection for small-sized peripheral non-small cell lung cancer (JCOG0802/WJOG4607L). Jpn J Clin Oncol 2010;40:271-4. [DOI] [PubMed] [Google Scholar]
- 48.Suzuki K, Koike T, Asakawa T, et al. A prospective radiological study of thin-section computed tomography to predict pathological noninvasiveness in peripheral clinical IA lung cancer (Japan Clinical Oncology Group 0201). J Thorac Oncol 2011;6:751-6. [DOI] [PubMed] [Google Scholar]
- 49.Port JL, Kent MS, Korst RJ, et al. Tumor size predicts survival within stage IA non-small cell lung cancer. Chest 2003;124:1828-33. [DOI] [PubMed] [Google Scholar]
- 50.Okada M, Nishio W, Sakamoto T, et al. Effect of tumor size on prognosis in patients with non-small cell lung cancer: the role of segmentectomy as a type of lesser resection. J Thorac Cardiovasc Surg 2005;129:87-93. [DOI] [PubMed] [Google Scholar]
- 51.Rami-Porta R, Ball D, Clowly J, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the T descriptors in the forthcoming (seventh) edition of the TNM classification for lung cancer. J Thorac Oncol 2007;2:593-602. [DOI] [PubMed] [Google Scholar]
- 52.International Union Against Cancer. Lung and pleural tumours. In: Sobin LH, Gospodarowicz M, eds. TNM Classification of Malignant Tumours, 7th Ed. New York, NY: Wiley-Blackwell, 2009:138-46. [Google Scholar]
- 53.Fernando HC, Santos RS, Benfield JR, et al. Lobar and sublobar resection with and without brachytherapy for small stage IA non-small cell lung Cancer. J Thorac Cardiovasc Surg 2005;129:261-7. [DOI] [PubMed] [Google Scholar]
- 54.Schuchert MJ, Pettiford BL, Keeley S, et al. Anatomic segmentectomy in the treatment of stage I non-small cell lung cancer. Ann Thorac Surg 2007;84:926-32; discussion 932-3. [DOI] [PubMed] [Google Scholar]
- 55.Bando T, Miyahara R, Sakai H, et al. A follow-up report on a new method of segmental resection for small-sized early lung cancer. Lung Cancer 2009;63:58-62. [DOI] [PubMed] [Google Scholar]
- 56.Donahue JM, Morse CR, Wigle DA, et al. Oncologic efficacy of anatomic segmentectomy in stage IA lung cancer patients with T1a tumors. Ann Thorac Surg 2012;93:381-7; discussion 387-8. [DOI] [PubMed] [Google Scholar]
- 57.Kent M, Landreneau R, Mandrekar S, et al. Segmentectomy versus wedge resection for non-small cell lung cancer in high-risk operable patients. Ann Thorac Surg 2013;96:1747-54; discussion 1754-5. [DOI] [PubMed]
- 58.Ramsay BH, Mass B. The anatomic guide to the intersegmental plane. Surgery 1949;25:533-8. [PubMed] [Google Scholar]
- 59.Smith CB, Swanson SJ, Mhango G, et al. Survial after segmentectomy and wedge resection in stage I non-small-cell lung cancer. J Thorac Oncol 2013;8:73-8. [DOI] [PubMed] [Google Scholar]
- 60.Miller DL, Rowland CM, Deschamps C, et al. Surgical treatment of non-small cell lung cancer 1 cm or less in diameter. Ann Thorac Surg 2002;73:1545-50; discussion 1550-1. [DOI] [PubMed] [Google Scholar]
- 61.El-Sherif A, Fernando HC, Santos R, et al. Margin and local recurrence after sublobar resection of non-small cell lung cancer. Ann Surg Oncol 2007;14:2400-5. [DOI] [PubMed] [Google Scholar]
- 62.Sienel W, Dango S, Kirschbaum A, et al. Sublobar resections in stage IA non-small cell lung cancer: segmentectomies result in significantly better cancer-related survival than wedge resections. Eur J Cardiothorac Surg 2008;33:728-34. [DOI] [PubMed] [Google Scholar]
- 63.Koike T, Koike T, Yoshiya K, et al. Risk factor analysis of locoregional recurrence after sublobar resection in patients with clinical stage IA non-small cell lung cancer. J Thorac Cardiovasc Surg 2013;146:372-8. [DOI] [PubMed] [Google Scholar]
- 64.Feizi I, Sokouti M, Golzari SE, et al. Determination of safe margin in the surgical pathologic specimens of non-small cell carcinoma of the lung. Pneumologia 2013;62:16-8. [PubMed] [Google Scholar]
- 65.Sawabata N, Ohta M, Matsumura A, et al. Optimal distance of malignant negative margin in excision of nonsmall cell lung cancer: a multicenter prospective study. Ann Thorac Surg 2004;77:415-20. [DOI] [PubMed] [Google Scholar]
- 66.Zwirewich CV, Vedal S, Miller RR, et al. Solitary pulmonary nodule: high-resolution CT and radiologic-pathologic correlation. Radiology 1991;179:469-76. [DOI] [PubMed] [Google Scholar]
- 67.Suzuki K, Kusumoto M, Watanabe S, et al. Radiologic classification of small adenocarcinoma of the lung: radiologic-pathologic correlation and its prognostic impact. Ann Thorac Surg 2006;81:413-9. [DOI] [PubMed] [Google Scholar]
- 68.Asamura H, Hishida T, Suzuki K, et al. Radiographically determined noninvasive adenocarcinoma of the lung: survival outcomes of Japan Clinical Oncology Group 0201. J Thorac Cardiovasc Surg 2013;146:24-30. [DOI] [PubMed] [Google Scholar]
- 69.Landreneau RJ, Sugarbaker DJ, Mack MJ, et al. Wedge resection versus lobectomy for stage I (T1 N0 M0) non-small-cell lung cancer. J Thorac Cardiovasc Surg 1997;113:691-8; discussion 698-700. [DOI] [PubMed] [Google Scholar]
- 70.Collins J, Stern EJ. Ground-glass opacity at CT: the ABCs. AJR Am J Roentgenol 1997;169:355-67. [DOI] [PubMed] [Google Scholar]
- 71.Yoshimoto K, Nomori H, Mori T, et al. Postoperative change in pulmonary function of the ipsilateral preserved lung after segmentectomy versus lobectomy. Eur J Cardiothorac Surg 2010;37:36-9. [DOI] [PubMed] [Google Scholar]
- 72.Takizawa T, Haga M, Yagi M, et al. Pulmonary function after segmentectomy for small peripheral carcinoma of the lung. J Thorac Cardiovasc Surg 1999;118:536-41. [DOI] [PubMed] [Google Scholar]
- 73.Harada H, Okada M, Sakamoto T, et al. Functional advantage after radical segmentectomy versus lobectomy for lung cancer. Ann Thorac Surg 2005;80:2041-5. [DOI] [PubMed] [Google Scholar]
- 74.Deng B, Cassivi SD, de Andrade M, et al. Clinical outcomes and changes in lung function after segmentectomy versus lobectomy for lung cancer cases. J Thorac Cardiovasc Surg 2014. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.National Lung Screening Trial Research Team , Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [DOI] [PMC free article] [PubMed] [Google Scholar]


