Abstract
Introduction
There is only limited data on the influence of the admission time (normal business hours versus nighttime and weekends) on procedural timings, revascularization efficacy, and outcome after mechanical thrombectomy. We investigated whether the admission time has an impact on the above-mentioned factors.
Methods
Our neurointerventional database was screened for all mechanical thrombectomies in anterior circulation acute ischemic stroke between 07/13 and 06/14. Outcome measures were procedural timings and clinical and demographic data; we compared patients who were admitted at normal business hours (Monday to Friday 8:00–18:00) to those admitted at night or at the weekend.
Results
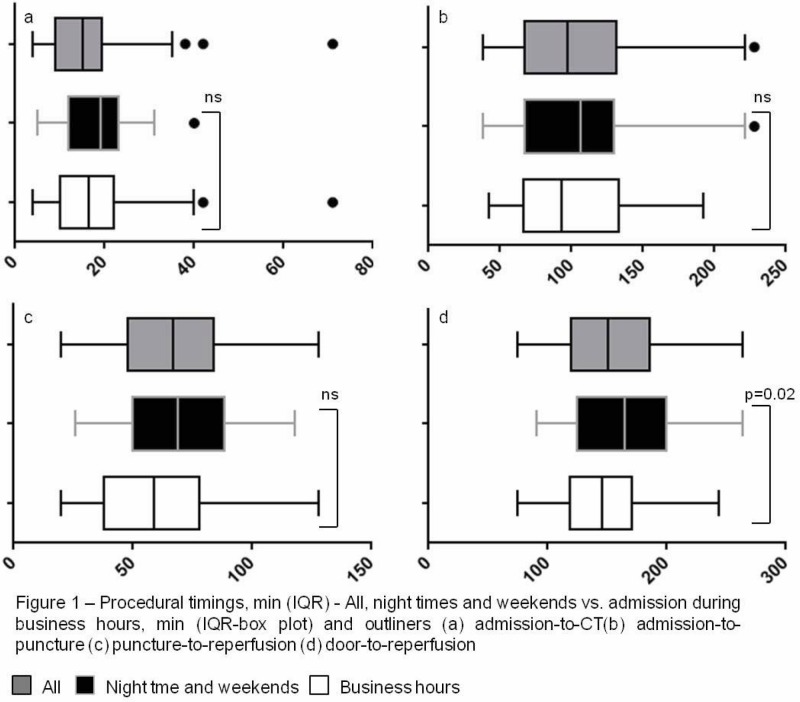
98 patients were identified. Of them, 52 (53%) were admitted during normal business hours, the remainder at night or at weekend. There was no statistically significant difference between the groups regarding the time from symptom-onset to admission, baseline National Institutes of Health Stroke Scale (NIHSS) or IVT-rate. There was a significant difference between groups for door-to-reperfusion timing, favoring patients admitted during normal business hours (146 versus 165 min, p = 0.02). Door-to-groin-puncture and groin-puncture-to-reperfusion time did not differ significantly. The rate of successful revascularizations (mTICI ≥ 2b) and the rate of favorable clinical outcome at discharge (mRS ≤ 2) did not differ between groups (77% versus 78% and 37% versus 35%, respectively).
Conclusions
There was a statistically significant prolongation of door-to-reperfusion timings for patients admitted during nighttime and weekends; it went along neither with a lower rate of successful revascularizations nor with a lower rate of favorable outcome in our series.
Abbreviations
- AF
atrial fibrillation
- AIS
acute ischemic stroke
- CTA
computed tomography angiography
- DM
diabetes mellitus
- ENT
embolization to new territory
- EVT
endovascular therapy
- HLP
hyperlipoproteinemia
- HTN
hypertension
- IQR
inter-quartile range
- IVT
intravenous thrombolysis
- mRS
modified Rankin Scale
- MT
mechanical thrombectomy
- NIHSS
National Institutes of Health Stroke Scale
- n.s.
not significant
- sICH
symptomatic intracranial hemorrhage
Introduction
IVT has been the standard of care in AIS within 4.5 h after symptom onset for almost 10 years.1 In recent times, a vast number of large case series and registries have investigated the efficacy and clinical outcome after MT in AIS and procedural recommendations have been derived from these studies. 2–12 Detailed recommendations for MT do not yet exist, as the body of evidence is still evolving; IVT guidelines though recommend a door-to-needle time of <60 min based on the finding that early recanalization is associated with an improved outcome.5 Additionally, the door-to-needle time represents an important parameter for the evaluation of the quality of service for stroke centers; a prolonged door-to-needle time results in a higher in-hospital mortality rate. 13 The efficacy of IVT is limited in cases with underlying large artery occlusions.14 Therefore, endovascular approaches have been developed and improved significantly over time regarding revascularization efficacy and clinical outcome with stent-retriever-based MT becoming an established therapeutic option in AIS.15 The impact of door-to-groin-puncture or door to reperfusion timings on the clinical outcome has become more and more evident.16 Consequently, the brain attack coalition proposed a door-to-groin-puncture time of ≤2 h as a benchmark for MT.17 Recently published results from the rapid reperfusion registry confirmed the clinically important role of the door-to-groin-puncture time in terms of functional outcome after AIS.18 In another publication by the same investigators, a delay of the image-to-groin-puncture time resulted in a reduced probability of a favorable outcome .19 In view of a broad variety of local and national conditions, there are to date no consensus recommendations on the periprocedural timings of MT. An important issue in this context is that MT requires dedicated technical and human resources, including the immediate availability of an angiosuite, the technical staff to support it, anesthesia whenever necessary and a trained neurointerventionalist. These complex prerequisites might affect the delicate workflow especially during nighttime and on weekends. A recently published study by Almekhlafi et al. investigated the influence of the admission time on procedural timings and found prolonged imaging to groin-puncture and imaging to reperfusion times at nighttime and on weekends.20 The role of potential time delays at nighttime and on weekends becomes even more relevant if we take into account that a prolonged endovascular procedure is significantly associated with a higher rate of complications and a higher rate of unfavorable outcome.16,21
We investigated the procedural timings of a one-year period at our stroke center (>100 MT procedures per year) with a special interest in the influence of the admission time (nighttime and weekends versus normal business hours) on the procedural timings, the procedural complication-rate, the revascularization rates, and the early clinical outcome at discharge.
Methods
We searched our longitudinal neurointerventional database for all patients with anterior circulation AIS who received MT from July 2013 to June 2014 and conducted a retrospective analysis; according to institutional guidelines, no ethics committee approval was required for this observational study. Inclusion criteria for MT were: 1) CTA-proven large artery occlusion, 2) treatment within 8 h of symptom-onset, and 3) a baseline NIHSS≥5 or aphasia. Exclusion criteria for MT were evidence of sICH (defined according to ECASS III Criteria22), infarction of more than one third of the MCA territory on native brain CT-scan or no evidence of salvageable brain parenchyma (penumbra concept of AIS) as depicted by Perfusion-CT.23,24 No other inclusion or exclusion criteria were applied. IVT was administered independently from MT in all eligible patients according to national neurological guidelines.
Baseline clinical evaluation
NIHSS on admission and discharge as well as mRS were assessed by a consultant neurologist. The treating physician assessed cardiovascular risk factors (AF, HTN, HLP, and DM).
Endovascular therapy and image evaluation
All procedures were carried out under general anesthesia. The endovascular procedure was performed as described previously.25 In brief: A large guide catheter (Penumbra 088 MAX, Penumbra Inc., Alameda, CA) was placed into the internal carotid artery followed by an intermediate aspiration catheter (Penumbra 5MAX or 5MAX ACE), which was advanced to the level of the clot over a microcatheter and a microguidewire. Then, the microguidewire and microcatheter were navigated across the clot and the microguidewire exchanged for a Penumbra Separator 3D. The microcatheter was withdrawn and the stent-retriever pulled back into the intermediate catheter under continuous aspiration.
A board certified interventional neuroradiologist evaluated all angiographic imaging blinded to all demographic and clinical data. A favorable revascularization result was defined as mTICI≥2b and ENT as any embolic event in a vascular territory other than the primary target downstream territory according to the recent recommendations of the cerebral angiographic revascularization group .26
Procedural timings evaluation
Procedural timings were defined as follows: Admission time was the point of time, when the patient data was entered into the electronic data management system. This is consistently among the first things to be done upon admission. Image time was defined to be the point of time of completion of the native brain CT scan. Groin-puncture-to-reperfusion time was defined as the time from groin puncture to the final angiogram. Stroke onset was defined to be the last time the patient was seen well.
Variables and statistical analysis
Nighttime was defined as the time-interval between 18:00 and 8:00 o’clock. Weekend was defined as the interval between Friday, 18:00 o'clock and Monday morning, 08:00 o'clock. The remainder was business hours. Patients were then assigned to the nighttime and weekend and the business hours subgroups according to the above-mentioned criteria. Continuous variables were compared using the Mann–Whitney U-test and categorical variables using Fisher’s exact test (two-tailed); a p-value of ≤0.05 was considered to be statistically significant. Variables in the different procedural timings were summarized as median (IQR) and “Tukey” box plots were created. All statistical analyses and graph plotting were carried out using GraphPad Prism Version 6.01 (GraphPad Software Inc., La Jolla, CA).
Results
Demographics
We identified 98 patients who received MT for AIS between July 2013 and June 2014. The median age was 73 (IQR: 41-91), 49% were male. 76/98 (78%) received IVT. The patients presented with a median NIHSS score of 15 (IQR: 12-17) after a median of 118min (IQR: 50-179) from symptom onset. We observed a difference between groups in the median age: patients admitted at nighttime or weekends were significantly younger (median: 70 vs. 75; p=0.02). Cardiovascular risk factors (AF, HTN, HLP and DM) did not differ (Table 1).
Table 1. Baseline characteristics of the patients.
| Characteristics | All (N=98) | Nighttime and Weekends (N=46) | Business Hours (N=52) | p-Value |
|---|---|---|---|---|
| Age, Median (range) | 73 (41–94) | 70 (46–86) | 75 (41–94) | 0.02 |
| Male Sex, n/N (%) | 48/98 (49%) | 24/46 (52%) | 24/52 (46%) | 0.7 |
| IVT, n/N (%) | 76/98 (78%) | 35/46 (76%) | 41/52 (79%) | 0.8 |
| Baseline NIHSS, Median (IQR) | 15 (12–17) | 15 (13–17) | 15 (12–18) | 0.9 |
| Symptom-onset-to-admission time, median (IQR) | 118 (50–179) | 134 (46–188) | 115 (54–172) | 0.6 |
| AF, n/N (%) | 50/98 (51%) | 23/46 (50%) | 27/52 (52%) | 1.0 |
| HTN, n/N (%) | 76/98 (78%) | 36/46 (78%) | 42/52 (81%) | 0.8 |
| HLP, n/N (%) | 40/98 (41%) | 15/46 (33%) | 25/52 (48%) | 0.7 |
| DM, n/N(%) | 13/98 (13%) | 9/46 (20%) | 4/52 (8%) | 0.1 |
Timings
The symptom-onset-to admission time was longer in the group of patients who had been admitted during nighttime and on weekends with a median of 135 versus 115 min in the group of patients, who had been admitted during normal business hours without reaching statistical significance (p=0.6). The door-to -image time was also shorter in the business hours group, but not significantly (15 versus 19 min; p=0.2). This was also true for the differences in the door-to-groin-puncture interval (93 min for business hours versus. 106 min during nighttime and weekends), as well as for the groin-puncture-to-reperfusion interval (59 versus 65 min). Both the time intervals did not differ significantly between subgroups (Table 2).
Table 2. Outcome characteristics of the patients.
| Characteristics | All (n=98) | Nighttime and Weekends (n=46) | Business Hours (n=52) | p-Value |
|---|---|---|---|---|
| Door to imaging, min (IQR) | 17 (10–22) | 19 (12–23) | 15 (9–20) | 0.2 |
| Door to groin-puncture, min (IQR) | 97 (67–131) | 106 (67–130) | 93 (67–133) | 0.8 |
| Groin-puncture to reperfusion, min (IQR) | 67 (48–84) | 69 (50–89) | 59 (38–78) | 0.2 |
| Door to reperfusion, min (IQR) | 151 (120–186) | 165 (125–200) | 146 (118–170) | 0.02 |
| Symptom-Onset to Reperfusion, min (IQR) | 264 (217–323) | 301 (231–363) | 247 (204–285) | 0.01 |
| mTICI≥2b | 77/98 (79%) | 36/46 (78%) | 41/52 (79%) | 1.0 |
| mRS 0-2 at Discharge, n/N (%) | 35/98 (36%) | 16/46 (35%) | 19/52 (37%) | 1.0 |
| NIHSS at Discharge, Median (IQR) | 7 (3–12) | 5 (3–8) | 7 (3–14) | 0.2 |
| sICH, n/N (%) | 6/98 (6%) | 3/46 (7%) | 3/52 (6%) | 1.0 |
| ENT, n/N (%) | 3/98 (3%) | 3/46 (7%) | 1/52 (2%) | 0.3 |
| Mortality (in-hospital), n/N (%) | 22/98 (22%) | 11/46 (24%) | 11/52 (21%) | 0.8 |
Overall, 67% of the patients had a door-to-groin-puncture time of 2 h or less (64% of patients during nighttime and weekends and 70% of patients during normal business hours). None of these differences were significant, but the addition of delays during the in-hospital treatment amounted to a statistically significant prolongation of the door to reperfusion (165versus 146 min) time-interval in the nighttime and weekends subgroup; this reached statistical significance (p=0.02). Symptom-onset-to-reperfusion time increased also significantly (301 versus. 247 min) outside of business hours, but dominantly due to external delays during transportation. The median symptom onset to admission (=door) interval was 35 min longer outside of business hours; all relevant timings are displayed and summarized in Figure 1 and Table 2.
Figure 1.
MT during nighttime and on weekends was not associated with poorer revascularization results: a mTICI≥2b result was achieved in 79% of cases during business hours and in 78% during nighttime and weekends, respectively. There was no statistically significant difference regarding the early clinical outcome at discharge with 35% favorable outcome for those treated during unpropitious times versus 37% in the business hours group (p=1). This was also true for the rate of in-hospital mortality with 24% versus 21% and the rates of sICH and ENT (Table 2).
Discussion
Several factors contribute to the outcome after MT in AIS. Age, a high baseline NIHSS, a prolonged time from symptom-onset to reperfusion, a prolonged revascularization procedure, and an unfavorable revascularization result have been shown to predict unfavorable outcome after AIS treated by endovascular means.6,15,27–29 Not all of these variables can be fully influenced by the treating physicians at the stroke center; this is certainly not the case for all stroke-related internal organizational processes within the hospital, e.g., time from admission to imaging or from door to groin-puncture. These in-hospital delays contribute to the overall time from symptom-onset to reperfusion and thereby influence dramatically the outcome after MT in AIS.27, 30 It has been shown that stroke-relevant timings can be significantly reduced by means of a meticulous organization and preparation, e.g., down to a median of 20 minutes for the door to needle interval in IVT.31 This is not an exemption or national phenomenon; by implementing the organizational principles, these results can be transferred and successfully established transnationally.32
A less well-studied factor that might influence these periprocedural timings is the time of admission of the individual patient. A recently published study by Almekhlafi et al. found significant delays of the imaging to groin-puncture and the imaging-to-reperfusion times whenever patients were admitted during nighttime or on weekends compared with normal business hours. The differences did not amount to reach significance pertaining to the overall door to reperfusion interval in their study.20 This was not the case in our data, where the increased in-hospital delays during nighttime (i.e., imaging-to-reperfusion interval 146 versus 111 min in Almekhlafi et al.) led to a statistically significant difference in door-to-reperfusion time. This difference resulted as much from a prolonged door to groin-puncture time as from a prolonged groin-puncture-to-reperfusion time; it shows that suboptimal operating principles of all involved departments account for a time loss during nighttime and weekends. Like in Almekhlafi et al., the observed delays did not translate into a statistically significant difference in the rate of good functional outcome on discharge. We have to keep in mind though, that this finding might be biased by the statistically significant difference in the median age with more younger patients admitted during nighttime and weekends in our cohort; higher age is a predictor of worse outcome.28
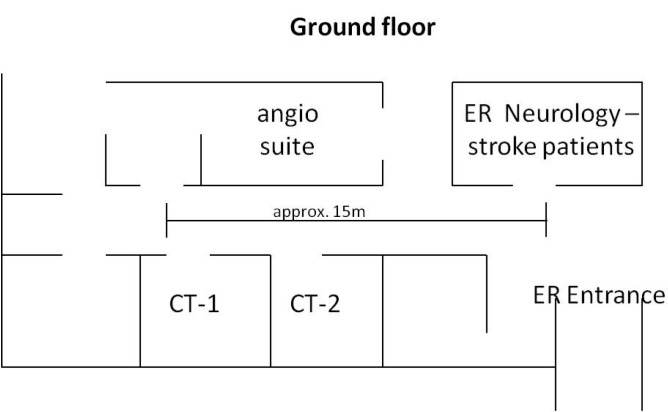
The rapid reperfusion registry collaborators reported a median of 112 min (IQR: 68-171) for door-to-groin-puncture time. In this context, they observed also substantial differences between the participating centers, which stresses the importance of the local organization for a reduction of periprocedural timings. Interestingly, Gupta et al. found procedural timings to be significantly shorter in high-volume centers.33 An architectonical setup favoring short ways between emergency room, imaging site, and angio-suite should naturally help in reducing in-hospital delays; this was the case in the current study, where all rooms were in close vicinity of the angio suite (Figure 2).
Figure 2.
Nevertheless, we found the door-to-reperfusion time and consecutively the symptom-onset-to-reperfusion time to be significantly longer, when the patients were admitted during nighttime and on weekends indicating that even slight delays in each sector accumulate to a significant delay until reperfusion is finally established. Although we could not demonstrate an association with an unfavorable outcome, we think that this finding should not act as an excuse for a lack of consistency outside of business hours. Further research should therefore focus on a consistent time metric for endovascular stroke centers which should secondarily find its way into transnational guidelines for MT in AIS. We also recommend that each neurointerventional department should monitor its performance closely and restructure its processes whenever performance drops.
There are several limitations in our study that should be considered seriously. The first is its retrospective, single-center design and the small number of cases. In addition, our conclusions are limited by the missing 90-day follow up and the self-reported revascularization rates. The reader should also consider that our stroke center is located in a densely populated area, potentially allowing shorter times from symptom-onset to admission compared with more remote areas.
Conclusion
Significant in-hospital delays of periprocedural timings do happen during nighttime and weekends. Although they might not translate immediately into a lower rate of successful revascularizations or favorable outcome, they have to be taken seriously and have to be addressed by proper organizational means. Future studies are mandatory to develop metrics and guidelines for periprocedural timings in endovascular stroke therapy.
References
- Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N. Engl. J. Med. 2008;359(13):1317–29. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- Behme D, Kowoll A, Mpotsaris A, et al. Multicenter clinical experience in over 125 patients with the Penumbra Separator 3D for mechanical thrombectomy in acute ischemic stroke. J. Neurointerv. Surg. 2014 doi: 10.1136/neurintsurg-2014-011446. [DOI] [PubMed] [Google Scholar]
- Dorn F, Stehle S, Lockau H, Zimmer C, Liebig T. Endovascular treatment of acute intracerebral artery occlusions with the solitaire stent: single-centre experience with 108 recanalization procedures. Cerebrovasc. Dis. 2012;34(1):70–7. doi: 10.1159/000338903. [DOI] [PubMed] [Google Scholar]
- Hussain SI, Zaidat OO, Fitzsimmons B-FM. The Penumbra system for mechanical thrombectomy in endovascular acute ischemic stroke therapy. Neurology. 2012;79(13 Suppl 1):S135–41. doi: 10.1212/WNL.0b013e31826958a8. [DOI] [PubMed] [Google Scholar]
- Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- Menon BK, Almekhlafi MA, Pereira VM, et al. Optimal workflow and process-based performance measures for endovascular therapy in acute ischemic stroke: analysis of the Solitaire FR thrombectomy for acute revascularization study. Stroke. 2014;45(7):2024–9. doi: 10.1161/STROKEAHA.114.005050. [DOI] [PubMed] [Google Scholar]
- Nogueira RG, Lutsep HL, Gupta R, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet. 2012;380(9849):1231–40. doi: 10.1016/S0140-6736(12)61299-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saver JL, Jahan R, Levy EI, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012;380(9849):1241–9. doi: 10.1016/S0140-6736(12)61384-1. [DOI] [PubMed] [Google Scholar]
- Singer OC, Haring H-P, Trenkler J, et al. Periprocedural aspects in mechanical recanalization for acute stroke: data from the ENDOSTROKE registry. Neuroradiology. 2013;55(9):1143–51. doi: 10.1007/s00234-013-1219-9. [DOI] [PubMed] [Google Scholar]
- Smith WS, Sung G, Saver J, et al. Mechanical thrombectomy for acute ischemic stroke: final results of the Multi MERCI trial. Stroke. 2008;39(4):1205–12. doi: 10.1161/STROKEAHA.107.497115. [DOI] [PubMed] [Google Scholar]
- Zaidat OO, Castonguay AC, Gupta R, et al. North American Solitaire Stent Retriever Acute Stroke registry: post-marketing revascularization and clinical outcome results. J. Neurointerv. Surg. 2014;6(8):584–8. doi: 10.1136/neurintsurg-2013-010895. [DOI] [PubMed] [Google Scholar]
- The Interventional Management of Stroke (IMS) II Study. Stroke. 2007;38(7):2127–35. doi: 10.1161/STROKEAHA.107.483131. [DOI] [PubMed] [Google Scholar]
- Reeves MJ, Smith E, Fonarow G, Hernandez A, Pan W, Schwamm LH. Off-hour admission and in-hospital stroke case fatality in the get with the guidelines-stroke program. Stroke. 2009;40(2):569–76. doi: 10.1161/STROKEAHA.108.519355. [DOI] [PubMed] [Google Scholar]
- Bhatia R, Hill MD, Shobha N, et al. Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke: real-world experience and a call for action. Stroke. 2010;41(10):2254–8. doi: 10.1161/STROKEAHA.110.592535. [DOI] [PubMed] [Google Scholar]
- Hinman JD, Rao NM, Yallapragada A, et al. Drip, Ship, and Grip, then Slice and Dice: Comprehensive Stroke Center Management of Cervical and Intracranial Emboli. Front. Neurol. 2013;4:104. doi: 10.3389/fneur.2013.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiotta AM, Vargas J, Turner R, Chaudry MI, Battenhouse H, Turk AS. The golden hour of stroke intervention: effect of thrombectomy procedural time in acute ischemic stroke on outcome. J. Neurointerv. Surg. 2014;6(7):511–6. doi: 10.1136/neurintsurg-2013-010726. [DOI] [PubMed] [Google Scholar]
- Alberts MJ, Latchaw RE, Jagoda A, et al. Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke. 2011;42(9):2651–65. doi: 10.1161/STROKEAHA.111.615336. [DOI] [PubMed] [Google Scholar]
- Sun C-HJ, Ribo M, Goyal M, et al. Door-to-puncture: a practical metric for capturing and enhancing system processes associated with endovascular stroke care, preliminary results from the rapid reperfusion registry. [Nov 11;2014 ];J. Am. Heart Assoc. 2014 3(2):e000859. doi: 10.1161/JAHA.114.000859. Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4187502&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun C-HJ, Nogueira RG, Glenn BA, et al. “Picture to puncture”: a novel time metric to enhance outcomes in patients transferred for endovascular reperfusion in acute ischemic stroke. Circulation. 2013;127(10):1139–48. doi: 10.1161/CIRCULATIONAHA.112.000506. [DOI] [PubMed] [Google Scholar]
- Almekhlafi MA, Hockley A, Desai JA, et al. Overcoming the evening/weekend effects on time delays and outcomes of endovascular stroke therapy: the Calgary Stroke Program experience. J. Neurointerv. Surg. 2014;6(10):729–32. doi: 10.1136/neurintsurg-2013-011000. [DOI] [PubMed] [Google Scholar]
- Behme D, Gondecki L, Fiethen S, Kowoll A, Mpotsaris A, Weber W. Complications of mechanical thrombectomy for acute ischemic stroke-a retrospective single-center study of 176 consecutive cases. Neuroradiology . 2014;56(6):467–76. doi: 10.1007/s00234-014-1352-0. [DOI] [PubMed] [Google Scholar]
- Bluhmki E, Chamorro A, Dávalos A, et al. Stroke treatment with alteplase given 3.0-4.5 h after onset of acute ischaemic stroke (ECASS III): additional outcomes and subgroup analysis of a randomised controlled trial. Lancet. Neurol. 2009;8(12):1095–102. doi: 10.1016/S1474-4422(09)70264-9. [DOI] [PubMed] [Google Scholar]
- Wintermark M, Sanelli PC, Albers GW, et al. Imaging recommendations for acute stroke and transient ischemic attack patients: A joint statement by the American Society of Neuroradiology, the American College of Radiology, and the Society of NeuroInterventional Surgery. AJNR. Am. J. Neuroradiol. 34(11):E117–27. doi: 10.3174/ajnr.A3690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J-T, Yoon W, Park M-S, et al. Early outcome of combined thrombolysis based on the mismatch on perfusion CT. Cerebrovasc. Dis. 2009;28(3):259–65. doi: 10.1159/000228256. [DOI] [PubMed] [Google Scholar]
- Mpotsaris A, Bussmeyer M, Weber W. Mechanical thrombectomy with the penumbra 3D separator and lesional aspiration: technical feasibility and clinical outcome. Clin. Neuroradiol. 2014;24(3):245–50. doi: 10.1007/s00062-013-0242-x. [DOI] [PubMed] [Google Scholar]
- Zaidat OO, Yoo AJ, Khatri P, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013;44(9):2650–63. doi: 10.1161/STROKEAHA.113.001972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal M, Almekhlafi MA, Fan L, et al. Evaluation of interval times from onset to reperfusion in patients undergoing endovascular therapy in the Interventional Management of Stroke III trial. Circulation. 2014;130(3):265–72. doi: 10.1161/CIRCULATIONAHA.113.007826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer OC, Haring H-P, Trenkler J, et al. Age dependency of successful recanalization in anterior circulation stroke: the ENDOSTROKE study. Cerebrovasc. Dis . 2013;36(5-6):437–45. doi: 10.1159/000356213. [DOI] [PubMed] [Google Scholar]
- Soize S, Barbe C, Kadziolka K, Estrade L, Serre I, Pierot L. Predictive factors of outcome and hemorrhage after acute ischemic stroke treated by mechanical thrombectomy with a stent-retriever. Neuroradiology. 2013;55(8):977–87. doi: 10.1007/s00234-013-1191-4. [DOI] [PubMed] [Google Scholar]
- Manning NW, Campbell BC V, Oxley TJ, Chapot R. Acute ischemic stroke: time, penumbra, and reperfusion. Stroke. 2014;45(2):640–4. doi: 10.1161/STROKEAHA.113.003798. [DOI] [PubMed] [Google Scholar]
- Meretoja A, Strbian D, Mustanoja S, Tatlisumak T, Lindsberg PJ, Kaste M. Reducing in-hospital delay to 20 minutes in stroke thrombolysis. Neurology. 2012;79(4):306–13. doi: 10.1212/WNL.0b013e31825d6011. [DOI] [PubMed] [Google Scholar]
- Meretoja A, Weir L, Ugalde M, et al. Helsinki model cut stroke thrombolysis delays to 25 minutes in Melbourne in only 4 months. Neurology. 2013;81(12):1071–6. doi: 10.1212/WNL.0b013e3182a4a4d2. [DOI] [PubMed] [Google Scholar]
- Gupta R, Horev A, Nguyen T, et al. Higher volume endovascular stroke centers have faster times to treatment, higher reperfusion rates and higher rates of good clinical outcomes. J. Neurointerv. Surg. 2013;5(4):294–7. doi: 10.1136/neurintsurg-2011-010245. [DOI] [PubMed] [Google Scholar]