TO THE EDITOR: During the period from early June to mid-September 2014, the epidemic of Ebola virus disease (EVD) in Guinea, Liberia, and Sierra Leone grew exponentially, with national doubling times of between 16 and 30 days.1 On the basis of case reports through mid-September, and assuming no change in the trajectory of the epidemic, we predicted a cumulative total of 21,000 cases in these three countries by November 2.1 In fact, the epidemic did change course in September: the increase in case incidence appears to have halted in Guinea and Sierra Leone and has reversed in Liberia (Fig. 1). Now, 1 year after the first case was reported in December 2013,2 we report updated epidemiologic findings for the three countries that have been most affected, using data recorded through December 14.
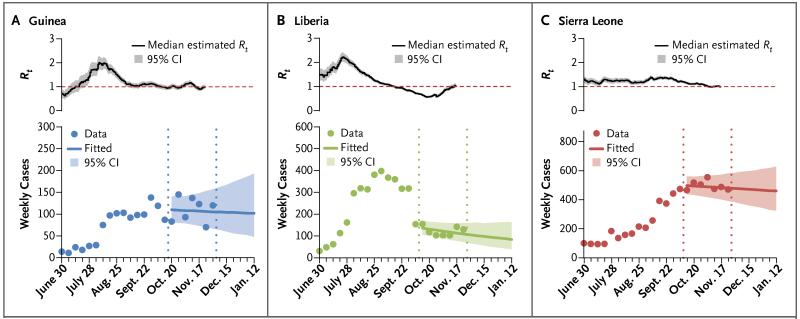
Figure 1. Case Reproduction Numbers and Weekly Incidence in Guinea, Liberia, and Sierra Leone.
Shown are the estimated case reproduction number (Rt) over time (upper panels) and the observed and projected weekly incidence (lower panels) of confirmed and probable cases of Ebola virus disease (EVD), according to the date of symptom onset, from the week beginning June 30, 2014, until the week beginning January 12, 2015, on the basis of data reported through December 7 for Guinea and November 30 for Liberia and Sierra Leone. The projections shown in the lower panels were generated from Rt estimates derived from data on case incidence (daily situation reports) for the 7 weeks through December 7 for Guinea and November 30 for Liberia and Sierra Leone (the time period delineated by the vertical dotted lines).
In the 4 weeks preceding December 14, the number of confirmed or probable cases of EVD ranged from 77 to 154 per week in Guinea, 73 to 138 in Liberia, and 327 to 537 in Sierra Leone. By December 14, a total of 18,625 confirmed, probable, or suspected EVD cases had been reported in eight affected countries (the three mentioned above, plus Mali, Nigeria, Senegal, Spain, and the United States), with 6971 recorded deaths.2 The true burden of illness and death is certainly higher, but the changes in epidemic trends between August and December are clear (Fig. 1).
National summary statistics do not tell the whole story, however; within the affected countries, the geographic distribution of cases has shifted markedly (Fig. S3 and S7 in the Supplementary Appendix, available with the full text of this letter at NEJM.org). In Gueckedou, Guinea, where the epidemic began, the incidence of EVD has decreased from an average of 11 confirmed or probable cases per week between March and September to 2 cases per week since the beginning of October, whereas the incidence has increased sharply in the neighboring districts of Kerouane, Macenta, and N’zerekore. Districts at the epicenter in eastern Sierra Leone (Kailahun and Kenema) and northern Liberia (Lofa) reported an average of 120 cases per week during July and August but only 2 per week since the beginning of November. EVD has been persistently active in Conakry, the capital of Guinea, since March and highly active in all three national capitals since June. During the period of peak incidence between August 11 and October 5, Monrovia, Liberia, averaged close to 200 confirmed or probable cases per week. In Sierra Leone, the center of activity had moved from the east to the west of the country by October; by the second week of December, the rise in case incidence had slowed in Freetown, but the case incidence may still not have peaked (Freetown is shown as part of Western Area in Fig. S6 and S10 in the Supplementary Appendix).
Guided by targets for patient isolation and safe burial practices set by United Nations Mission for Ebola Emergency Response, control measures have been stepped up since October 1.3 By December 14, the total number of beds (>2000) in Ebola treatment centers far exceeded the number of patients reported each week, though there were substantial gaps in treatment capacity in some areas of all three countries — in western Sierra Leone (Freetown and Western Area), in the southeastern forest area and some northern districts of Guinea (Kerouane, N’zerekore, and Siguiri), and in western Liberia (Grand Cape Mount). The capacity to carry out safe burials has more than doubled since October 1; approximately 200 burial teams were covering all but a small number of districts by December 14. And yet, knowing that many deaths are still unreported, and with continuing resistance to safe burial practices in some areas, deaths from EVD still pose a considerable hazard.
With the changes in the incidence of EVD and with the scale-up of case isolation and safe burial measures, there have been concomitant changes in key epidemiologic parameters. The case reproduction numbers (Rt) for all three countries, averaged across all districts, have now fallen to values close to 1 (Fig. 1, and Fig. S24 in the Supplementary Appendix). The precise reasons for these changes are still being investigated. However, in a comparison of periods before and after October 1, the average time from symptom onset to hospitalization decreased from 5.3 days to 4.3 days, which indicates a reduction in opportunities for transmission in communities (Table 1, and Tables S7 and S8 in the Supplementary Appendix). Further quantitative analysis is expected to support strong anecdotal evidence that comprehensive measures to interrupt transmission, including careful case finding and contact tracing, have had an effect — for instance, in eastern Sierra Leone (Kenema) and northern Liberia (Lofa).
Table 1. Characteristics Associated with Confirmed or Probable Ebola Virus Disease in Guinea, Liberia, and Sierra Leone*.
| Characteristic | December 2013 to November 25, 2014 | No. of Patients with Data | December 2013 to September 30, 2014 | No. of Patients with Data | October 1 to November 25, 2014† | No. of Patients with Data | P Value‡ |
|---|---|---|---|---|---|---|---|
| Incubation period — days | |||||||
| Observed single-day exposures — median (IQR)§ | 9 (5–13) | 1798 | 8 (5–13) | 1285 | 10 (5–15) | 513 | |
| Fitted single-day exposures — mean (95% CI)¶ | 10.3 (9.9–10.7) | 1798 | 9.7 (9.2–10.1) | 1285 | 11.8 (11–12.7) | 513 | <0.001 |
| Serial interval — days∥ | |||||||
| Observed data (IQR) | 13 (8–18) | 305 | 12.5 (8–17) | 206 | 14 (8–20) | 99 | |
| Fitted data, gamma distribution (95% CI) | 14.2 (13.1–15.3) | 305 | 13.2 (12.1–14.5) | 206 | 16.1 (14.1–18.4) | 99 | 0.01 |
| Interval from symptom onset, fitted data — mean days (95% CI) | |||||||
| To hospitalization | 5.0 (4.9–5.1) | 4499 | 5.3 (5.1–5.5) | 3038 | 4.3 (4.1–4.5) | 1461 | <0.001 |
| To hospital discharge | 15.1 (14.6–15.6) | 1335 | 15.3 (14.7–15.8) | 1085 | 14.4 (13.5–15.4) | 250 | 0.06 |
| To death | 8.2 (7.9–8.4) | 2741 | 8.8 (8.5–9.1) | 2094 | 6.2 (5.8–6.6) | 647 | <0.001 |
| Interval from hospitalization, fitted data — mean days (95% CI) | |||||||
| To discharge | 11.2 (10.8–11.7) | 1004 | 11.4 (10.9–11.9) | 813 | 10.6 (9.7–11.5) | 191 | 0.07 |
| To death | 4.3 (4.1–4.5) | 1167 | 4.4 (4.2–4.7) | 930 | 3.8 (3.4–4.3) | 237 | 0.01 |
| Mean duration of hospital stay — days** | 9.27 | 9.45 | 8.48 | ||||
| Case fatality rate — rate (95% Cl)†† | |||||||
| All patients | 70.4 (69.2–71.6) | 67.8 (66.4–69.2) | 76.5 (74.2–78.7) | 0.01 | |||
| All hospitalized patients | 60.7 (59.2–62.3) | 60 (58.3–61.7) | 63.7 (60.2–67.1) | 0.39 | |||
| According to sex | |||||||
| Male | 71.6 (69.9–73.2) | 69.4 (67.4–71.4) | 76.6 (73.2–79.7) | 0.16 | |||
| Female | 68.9 (67.1–70.6) | 66.0 (63.9–68.0) | 75.7 (72.3–78.8) | 0.05 | |||
| According to age group | |||||||
| <15 yr | 68.7 (65.6–71.6) | 64.5 (60.8–68.1) | 75.9 (70.2–80.8) | 0.18 | |||
| 15–44 yr | 66.7 (65.0–68.3) | 64.3 (62.4–66.2) | 72.7 (69.3–75.9) | 0.07 | |||
| ≥45 yr | 79.4 (77.1–81.5) | 77.5 (74.7–80.0) | 83.2 (79.0–86.8) | 0.47 | |||
| According to occupation | |||||||
| Health care worker | 66.8 (61.9–71.3) | 67.3 (62.1–72.1) | 61.5 (48.0–73.5) | 0.80 | |||
| Non–health care worker | 70.6 (69.4–71.9) | 67.8 (66.3–69.3) | 77.1 (74.7–79.3) | 0.01 |
CI denotes confidence interval, and IQR interquartile range.
October 1, 2014, marked the initiation of the United Nations Mission for Ebola Emergency Response.
The P values are for the comparisons between the period from December 2013 to September 30, 2014, and the period from October 1, 2014, to November 25, 2014.
Contacts on day 0 (the day of symptom onset) were excluded.
Gamma distributions were fitted to confirmed and probable cases. Contacts on day 0 (the day of symptom onset) were excluded.
Serial interval is defined as the interval between the onset of disease in an index case patient and the onset of disease in a person infected by that index case patient. The numbers here refer to the numbers of epidemiologically linked pairs in which the person infected by the index case patient reported only one direct contact.
The duration reported here is the weighted average of the observed means of the distributions of durations from hospitalization to discharge and hospitalization to death.
The late-stage case fatality rate (October 1 to November 25, 2014) may be an overestimate, since there are likely to be more discharges than deaths yet to be recorded for patients with disease onset during this time period, because the mean time from hospitalization to death is shorter than the mean time from hospitalization to discharge (see the Supplementary Appendix).
The uneven success of EVD control measures to date, in the face of shifting geographic patterns of transmission, illustrates the continuing threat posed by the Ebola virus 1 year after the start of the epidemic. A total of 625 confirmed or probable cases were reported from Guinea, Liberia, and Sierra Leone in the first week of December, a number similar to the average for the preceding 10 weeks (667), but these cases are now spread over a wider geographic area. The worst fears of persistent exponential growth beyond September were not realized; nevertheless, Ebola still presents a huge challenge as we move into the second year of the epidemic in West Africa.
Supplementary Material
Acknowledgments
Supported by the Medical Research Council, the Bill and Melinda Gates Foundation, the Models of Infectious Disease Agent Study of the National Institute of General Medical Sciences (National Institutes of Health), the Health Protection Research Units of the National Institute for Health Research, European Union PREDEMICS consortium, Wellcome Trust, Fogarty International Center, and World Health Organization.
Footnotes
A list of authors (members of the WHO Ebola Response Team who contributed to this letter, in alphabetic order) is available with the full text of this letter at NEJM.org.
An animated map with timeline is available at NEJM.org
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
References
- 1.WHO Ebola Response Team Ebola virus disease in West Africa — the first 9 months of the epidemic and forward projections. N Engl J Med. 2014;371:1481–95. doi: 10.1056/NEJMoa1411100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ebola response roadmap — situation report. World Health Organization; Geneva: http://www.who.int/csr/disease/ebola/situation-reports/en/ [Google Scholar]
- 3.UN Mission for Ebola Emergency Response (UNMEER) External situation report. http://www.un.org/ebolaresponse/index.shtml#&panel1-1. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.