Abstract
In this study, we have analyzed both administrative and clinical data from our hospital during 2002 to 2012 to evaluate the influence of government medical policies on reducing abandonment treatment in pediatric patients with acute lymphoblastic leukemia. Two policies funding for the catastrophic diseases and the new rural cooperative medical care system (NRCMS) were initiated in 2005 and 2011, respectively. About 1151 children diagnosed with acute lymphoblastic leukemia were enrolled in our study during this period and 316 cases abandoned treatment. Statistical differences in sex, age, number of children in the family, and family financial status were observed. Of most importance, the medical insurance coverage was critical for reducing abandonment treatment. However, 92 cases abandoning treatment after relapse did not show significant difference either in medical insurance coverage or in duration from first complete remission. In conclusion, financial crisis was the main reason for abandoning treatment. Government-funded health care expenditure programs reduced families’ economic burden and thereby reduced the abandonment rate with resultant increased overall survival.
Key Words: acute lymphoblastic leukemia (ALL), childhood, abandonment, medical care system, low and middle income countries (LMIC)
Acute lymphoblastic leukemia (ALL) is one of the common malignancies of childhood. In developed countries, the 5-year event-free survival (EFS) of pediatric ALL has reached 83% and overall survival (OS) is nearly up to 90%.1 However, 5-year EFS rate in low and middle income countries has been reported to be <35%.2 The resultant survival gap has been attributed to delayed presentation, greater treatment-related mortality, and a higher rate of relapse.3–5 Another important yet often overlooked cause is abandonment of therapy, the failure to start or complete potentially curative therapy.6 In China, although 5-year EFS and OS of children with ALL has improved greatly, abandonment rate (AR) still accounts for a large percentage of deaths.7,8
Suzhou is a city with above GDP per capita in China. In 2005, Suzhou government instituted funds for protection against catastrophic diseases expenditure (PACDE), including childhood cancer. In 2011, Chinese government instituted funds for protection against ALL of low and intermediate risk in children living in the countryside. Although the authors found several recent reports describing abandonment of ALL treatment in China, we found limited data regarding the impact of government assistance on AR. Therefore, we retrospectively analyzed the AR by dividing the time period into 2002 to 2005, 2005 to 2010, and 2011 to 2012, so as to evaluate the impact of medical policies on the abandoned treatment.
MATERIALS AND METHODS
We collected and retrospectively analyzed information on 1151 patients diagnosed with ALL at the Children’s Hospital of Soochow University from 2002 to 2012, which included general data (name, sex, age, home address, and telephone number), medical payment, final diagnosis, MICM (morphology, immunology, cytogenetics, and molecular biology) test results, treatment response, the stage, and reason for abandonment. In addition, we surveyed parents of inpatients by phone and noted their current living condition and treatment after hospital discharge, especially aiming at those with abandoned treatment.
Treatment abandonment is defined as failure to start or complete curative treatment (except in situations when such treatment is contraindicated for medical reasons, eg, if the patient is critically ill).9 Treatment abandonment after recurrence is defined as failure to continue treatment or just receiving palliative cure after recurrence. Lost to follow-up is defined as losing contact because of change of telephone number or address.
Patients were classified into urban, town, and rural population according to their addresses. On the basis of 5 administrative levels in China, including state, provincial, prefectural, county, and township level, people living in provincial or prefectural city who do not live on agriculture are considered as urban population. People living in county or town who do not mainly live on agriculture are classified into town population, and people living in countryside who mainly live on agriculture are viewed as rural population. PACDE was carried out on Suzhou children since 2005. New rural cooperative medical system (NRCMS) was carried out in some parts of rural areas since 2011. The family annual income is relatively lower for rural people, generally highest for urban people, and intermediate for town people.
Statistics
Frequency distributions, median, mean, and SDs were assessed for each variable. SPSS 18.0 version was employed for data analysis. ARs were compared using the χ2 test. P<0.05 was considered statistically significant.
RESULTS
General Information
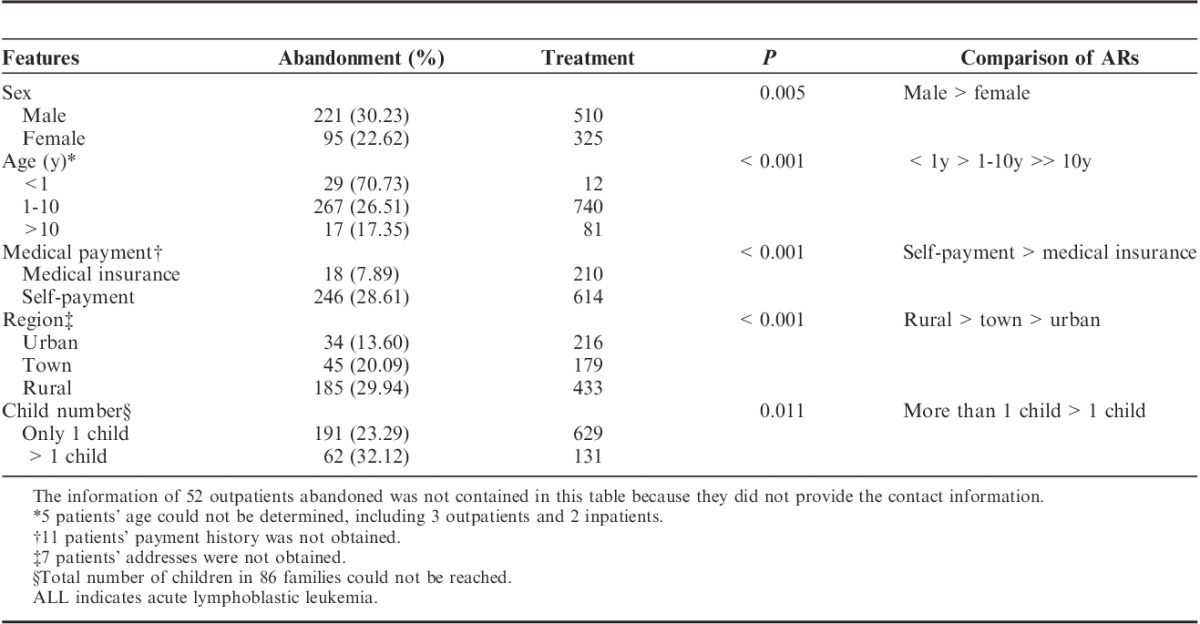
According to the policies carried out, the time period studied was divided into 3 phases: year 2002 to 2004, 2005 to 2010, and 2011 to 2012. The numbers of diagnosed patients were 258, 511, and 382 for each phase. Of the 1151 ALL diagnosed cases, 731 cases were boys and 420 cases were girls (boy:girl=1.74:1). The median age was 4.85 years ranging from 1 month to 16 years. Fifty-two cases abandoned as outpatients and 7 cases of inpatients were excluded in further analysis of abandonment reasons as unknown address. The number of inpatients from urban, town, and rural area were 250, 224, and 618, respectively. Families bearing 1 child accounted for 820 cases and 193 for >1 child. Of the 1099 ALL inpatients, 114 cases were Suzhou citizen and 90 cases benefited from the project of PACDE since 2005, and 132 cases as rural population benefited from the NRCMS during 2011 and 2012. Patients covered by these 2 health insurance programs usually paid 500 to 2000 RMB, roughly equal to monthly salary of people working in Suzhou city, for each course of chemotherapy and their economic burdens were largely reduced. Others had to pay the full cost of the treatment in the hospital and could be partially imbursed (<50% of the hospital fee) from the local government within 2 to 12 months after being discharged. The interruption of financial support somehow caused difficulty for the family to continue the following course of chemotherapy on time. We found 316 cases of abandoned treatment after diagnosis and 92 cases abandoning treatment after recurrence. Furthermore information is provided in Table 1.
TABLE 1.
Demography and Features of ALL Patients Abandoning Therapy
Patients Abandoning Treatment
A total of 316 patients were found to abandon treatment from 2002 to 2012, of which, 52 cases abandoned at their diagnosis of ALL, and only 264 cases were hospitalized (Fig. 1). A total of 178 patients abandoned after starting the chemotherapy <7 days, 61 cases abandoned after completing induction remission therapy, 14 cases abandoned on consolidation therapy, and 11 cases abandoned on intensification therapy. A total of 105 cases suffered a severe complication such as fatal infection or bleeding before abandonment. A significant difference in AR was found among those with various factors: boy>girl, children below 1 year>children above 1 year, self-paid>medical insurance covered, rural>town>urban, family with more than 1 child>family with only single child. Furthermore, the AR of patients in Suzhou from 2002 to 2005 was much higher than that from 2006 to 2012 (8/16 vs. 15/75, P=0.05) (Fig. 2). As a rapidly developed city, the population of Suzhou increased strikingly since 2006 by attracting more people nationwide. Most notably, as NRCMS covered all the rural districts of Suzhou during recent years, AR of patients residing in the countryside in 2011 and 2012 remarkably reduced compared with the AR from 2002 to 2010 (4/128 vs. 70/81, P<0.001) (Fig. 3).
FIGURE 1.
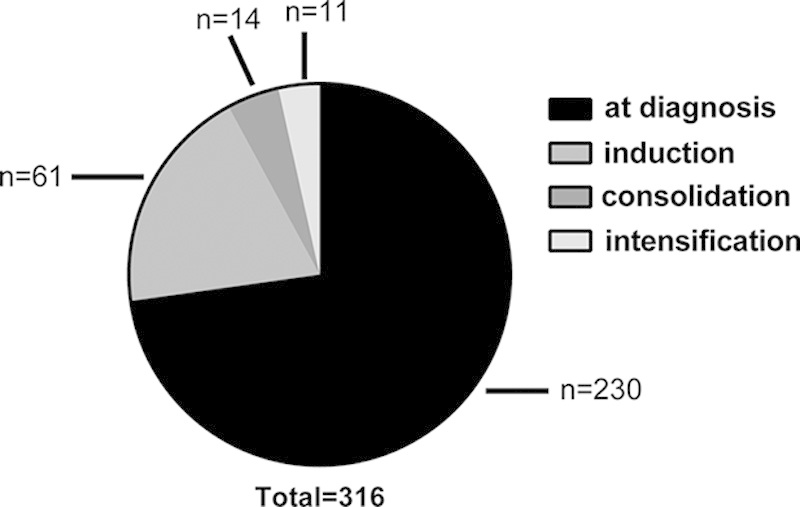
The number of abandonment for the newly diagnosed pediatric ALL at different stage of chemotherapy. A total of 230 cases of abandonment at diagnosis included 2 parts: one part was 52 outpatients and another part was 178 inpatients who abandoned within 1 week after starting induction remission therapy.
FIGURE 2.
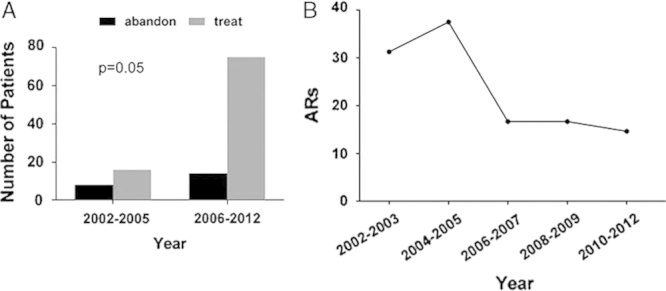
Comparison of the number of patients and ARs before and after PACDE funding in Suzhou City. The first period from 2002 to 2005 was the duration before the project was carried out. The second period from 2006 to 2012 was the time after the project. The ratio of completing treatment to abandonment in the second period is much higher than that in first period (A, P=0.05). ARs decreased rapidly since 2006 and kept a stable level about 15% since then (B) coinciding with the new policy.
FIGURE 3.
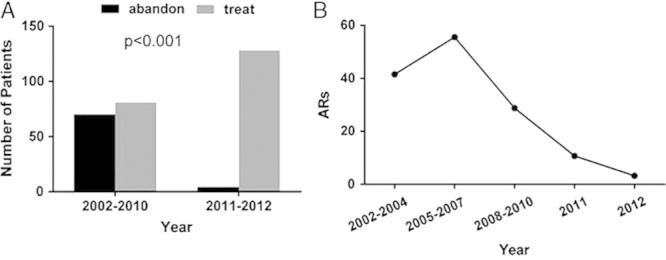
Comparison of the number of patients and ARs in remote areas before and after NRCMS (the new rural cooperative medical care system) began. The first period from 2002 to 2010 was the duration before NRCMS was carried out in rural regions. The second period from 2011 to 2012 was the time after NRCMS was carried out. The ratio of completing treatment to abandonment in the second period is much higher than that in first period, which reached a significant difference (A, P<0.001). ARs decreased steadily since 2006 and reached a very lower level of 5% in 2012 (B).
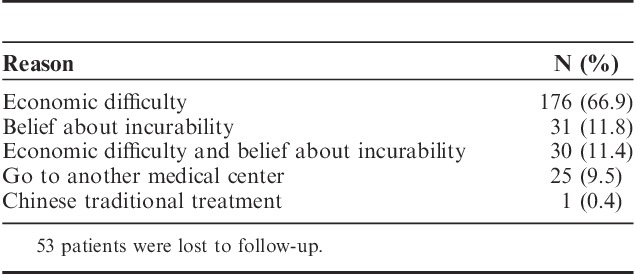
From the telephone survey information collected from 263 patients, we determined that financial difficulty involved was the primary reason for abandonment (206/263, 78.3%) (Table 2).
TABLE 2.
Reasons for Abandoning Treatment (Interviewed, n=263)
Patients Abandoning Treatment After Recurrence
A total of 92 patients abandoned treatment after recurrence who accounted for 41.26% of all the relapsed patients in our hospital from 2002 to 2012. To analyze the relevant factors influencing the AR, we evaluated the effect of relapse site, sex, medical insurance, and duration of first remission. Our data revealed that abandoned patients with bone marrow relapse accounted for 62 cases, testicular relapse 10, CNS relapse 11, and combined relapse 9. The ratio of abandoned male to female was 1.71 (58/34), which was similar to the ratio of patients receiving treatment (1.91, 86/45). Relapse patients abandoned who were covered by medical insurance accounted for 35.48% (11/31) and self-paid accounted for 42.19% (81/192). No significant difference could be found between them. The number of relapse patients at very early stage, early stage, and late stage was 109, 42, and 35, respectively, and abandoned patients were 47 (43.11%), 17 (40.48%), and 11 (31.43%) correspondingly. No statistic differences were calculated among them.
DISCUSSION
Treatment abandonment is one of the most important reasons for the short survival of patients with ALL in developing countries.10 It is important to determine what factors contribute to abandonment. Analyzing 316 cases of treatment abandonment, we found that children below 1 year of age represent the highest percentage (P<0.001). As the infant leukemia has a relatively unfavorable prognosis,11 and the parents are always informed with the poor prognosis, further more, most infants with leukemia are not covered by medical insurance which cause the desperate parents to abandon the treatment. Therefore, more researches on infant leukemia are urgently needed and the medical care system emphasizing on infants should decrease infants’ AR.
The AR of patients from rural areas is remarkably higher than that from urban and town regions (P<0.001). In China, parents from rural areas usually have a relatively lower income and poorer educational background. Furthermore, they also regard leukemia as an incurable and high expense bearing disease. From our statistical analysis, we found that AR is also higher in the self-paid patients and families with >1 child. ALL relapse is an index of unfavorable prognosis.12 The recurrence rate was 20.2% (223/1099) and the AR was 41.3% (92/223) in our hospital from 2002 to 2012. Although the AR of self-paid relapsed patients is higher than those covered by medical insurance, there is no statistical difference among them. From these information gathered we determined that financial burden is the major factor in treatment abandonment. We believe that revision and improvement of the policy of China’s medical care system, enhancement of the awareness of the inevitable ALL relapse, and more close communication and mutual understanding between doctors and parents to impart medical knowledge are necessarily important for reducing AR and improving OS of ALL.
Patients with ALL, especially those from undeveloped regions, can greatly benefit from the new policy, which is demonstrated in our statistical data (Table 1). Since 2006, AR in Suzhou has dramatically dropped to only 4 children from the countryside in 2011 and 2012. As Ribeiro13 pointed out that every cancer child could receive corresponding treatment of higher quality by expanding government’s medical care support, within the time period studied, we can see a clear picture demonstrating the decrease in the AR after the incorporation of new policies. Therefore, we conclude that the improvement of our medical care system can relieve economical burden, reduce AR, and improve OS of patients with ALL to a great extent.
In summary, financial crisis was the main reason for abandoning treatment in pediatric ALL patients. Government-funded health care expenditure programs reduced families’ economic burden and thereby reduced the AR with resultant increased OS.
Footnotes
Supported by the grants from Jiangsu Province’s Clinical Medical Science and Technology Projects (Grant No. BL2013014), National Natural Science Foundation of China (No. 81100371 and No. 81370627), Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD), and National clinical key subject construction project.
The authors declare no conflict of interest.
REFERENCES
- 1.Pui CH, Evans WE. Treatment of acute lymphoblastic leukemia. N Engl J Med. 2006;354:166–178. [DOI] [PubMed] [Google Scholar]
- 2.Metzger ML, Howard SC, Fu LC, et al. Outcome of childhood acute lymphoblastic leukaemia in resource-poor countries. Lancet. 2003;362:706–708. [DOI] [PubMed] [Google Scholar]
- 3.Eden T, Pui CH, Schrappe M, et al. All children have a right to full access to treatment for cancer. Lancet. 2004;364:1121–1122. [DOI] [PubMed] [Google Scholar]
- 4.Luo XQ, Ke ZY, Huang LB, et al. High-risk childhood acute lymphoblastic leukemia in China: factors influencing the treatment and outcome. Pediatr Blood Cancer. 2009;52:191–195. [DOI] [PubMed] [Google Scholar]
- 5.Gupta S, Yeh S, Martiniuk A, et al. The magnitude and predictors of abandonment of therapy in paediatric acute leukaemia in middle-income countries: a systematic review and meta-analysis. Eur J Cancer. 2013;49:2555–2564. [DOI] [PubMed] [Google Scholar]
- 6.Howard SC, Marinoni M, Castillo L, et al. Improving outcomes for children with cancer in low-income countries in Latin America: a report on the recent meetings of the Monza International School of Pediatric Hematology/Oncology (MISHPO)—part I. Pediatr Blood Cancer. 2007;48:364–369. [DOI] [PubMed] [Google Scholar]
- 7.Tang Y, Xu X, Song H, et al. Long-term outcome of childhood acute lymphoblastic leukemia treated in China. Pediatr Blood Cancer. 2008;51:380–386. [DOI] [PubMed] [Google Scholar]
- 8.Wang YR, Jin RM, Xu JW, et al. A report about treatment refusal and abandonment in children with acute lymphoblastic leukemia in China, 1997-2007. Leuk Res. 2011;35:1628–1631. [DOI] [PubMed] [Google Scholar]
- 9.Mostert S, Arora RS, Arreola M, et al. Abandonment of treatment for childhood cancer: position statement of a SIOP PODC Working Group. Lancet Oncol. 2011;12:719–720. [DOI] [PubMed] [Google Scholar]
- 10.Arora RS, Pizer B, Eden T. Understanding refusal and abandonment in the treatment of childhood cancer. Indian Pediatr. 2010;47:1005–1010. [DOI] [PubMed] [Google Scholar]
- 11.Pieters R, Schrappe M, De Lorenzo P, et al. A treatment protocol for infants younger than 1 year with acute lymphoblastic leukaemia (Interfant-99): an observational study and a multicentre randomised trial. Lancet. 2007;370:240–250. [DOI] [PubMed] [Google Scholar]
- 12.Marjerrison S, Antillon F, Fu L, et al. Outcome of children treated for relapsed acute lymphoblastic leukemia in Central America. Cancer. 2013;119:1277–1283. [DOI] [PubMed] [Google Scholar]
- 13.Ribeiro RC. Impact of the Mexican government’s system of social protection for health, or Seguro Popular, on pediatric oncology outcomes. Pediatr Blood Cancer. 2013;60:171–172. [DOI] [PMC free article] [PubMed] [Google Scholar]


