Abstract
Background
Hepato-pancreatico-biliary (HPB) fellowship training has risen in popularity in recent years and hence large numbers of graduating fellows enter the workforce each year. Studies have proposed that the increase in HPB-trained surgeons will outgrow demand in the USA. This study shows that the need for HPB-trained surgeons refers not to the meeting of demand in terms of case volume, but to improving patient access to care.
Methods
The National Inpatient Sample (NIS) database for the years 2005–2011 was queried for CPT codes relating to pancreatic, liver and biliary surgical cases. These numbered 6627 in 2005 and increased to 8515 in 2011. Cases were then mapped to corresponding states. The number of procedures in an individual state was divided by the total number of procedures to give a ratio for each state. A similar ratio was calculated for the population of each state to the national population. These ratios were combined to give a ratio by state of observed to expected HPB surgical cases.
Results
Of the 46 states that participate in the NIS, only 18 achieved ratios of observed to expected cases of >1. In the remaining 28 states, the number of procedures was lower than that expected according to each state's population.
Conclusions
The majority of the USA is underserved in terms of HPB surgery. Given the growing number of HPB-trained physicians entering the job market, this sector should focus on bringing understanding and management of complex disease to areas of the country that are currently in need.
Introduction
A recent survey of graduating senior residents showed that over 80% of respondents were pursuing fellowship training.1,2 The most common reason cited was inadequate training during residency for advanced procedures. This is particularly true for complex abdominal procedures such as pancreaticoduodenectomy and liver resection, which are performed infrequently by residents and hence have resulted in the emergence and evolution of Hepato-pancreatico-biliary (HPB) fellowships.3 A study conducted in 2006 found that a majority of graduating residents perform only one major hepatic resection, distal pancreatectomy and pancreaticoduodenectomy during their general surgery residency training.4 This has led to a rise in the number of applicants to fellowship training in HPB surgery. Although there is no board certification for HPB surgical training, fellowships exist in surgical oncology, abdominal transplant surgery and HPB surgery to prepare surgeons for challenging clinical problems and operative procedures.
A growing concern among HPB surgery leaders refers to the lack of HPB-centric positions for graduates of HPB fellowship programmes.5 This need is not specific to HPB surgery: a recent study by Decker et al. showed that only 34% of general surgery positions require fellowship training.6 Another study by Scarborough et al., published in 2008, projected that current training in HPB surgery will lead to a surplus of trainees in the job market.5 The authors predicted that the current training paradigm will outnumber the estimated number of HPB procedures performed by 2020. They concluded that increased standardization of HPB training to decrease the number of fellows would prevent a surplus of HPB-trained surgeons in the future.
The purpose of this study is to show that although demand for HPB-specific positions is not increasing, need for HPB-trained surgeons exists across the country. Various studies have shown discrepancies in access to surgical care across the country and among socioeconomic groups.7,8 Other studies have shown that patients prefer to receive treatment closer to home, rather than being required to travel, even with the knowledge that outcomes may be better at more distant hospitals.9 These factors are likely to combine to show why the majority of pancreatic resections still occur in low-volume centres, despite data showing that outcomes are comparatively better at high-volume centres. This study proposes to identify discrepancies in HPB surgical case volumes across the country and to show where the need for HPB-trained surgeons exists.
Materials and methods
The Nationwide Inpatient Sample (NIS) was utilized for the years 2005–2011. The NIS is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP). The NIS is the largest all-payer inpatient health care database in the USA, yielding national estimates of hospital inpatient stays. Unweighted, it contains data for approximately eight million hospital discharges each year. Weighted, it estimates roughly 40 million hospitalizations.10 It contains all discharge data from more than 1000 short-term and non-federal hospitals each year, which approximates a 20% stratified sample of US community hospitals. The most recent (2011) file contains a sampling frame that comprises approximately 97% of hospital discharges. Data are available for hospital identifiers (city listing or state) and International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes. The file has been validated for accuracy in capturing discharge data by an independent party.10 The NIS does not contain information that identifies specific patients and therefore institutional review board approval was not required for this study.
For the purposes of this study, ICD-9 procedure codes were pulled for selected procedures relating to surgery involving the pancreas, liver or biliary tract. Table 1 lists the specific procedure codes analysed. Data were associated with the location of the hospital at which the procedure was performed. These associations were then tabulated for the entire state in order not to identify specific cities or cases. Seven states do not list hospital locations by city, but do so by state alone. Four states, Alabama, Alaska, Idaho and Delaware, do not participate in the NIS. Procedure occurrences were then mapped to geographic locations on a map of the USA by the latitude and longitude of the centre of an individual state, and in relationship to the population of that city determined by the 2011 Census11 to ascertain the density of procedures per index population.
Table 1.
HPB procedures (ICD-9-CM codes) analysed in the current study
| Pancreas procedures |
| Other partial pancreatectomy (52.59) |
| Total pancreatectomy (52.6) |
| Proximal pancreatectomy (52.51) |
| Distal pancreatectomy (52.52) |
| Radical subtotal pancreatectomy/Whipple (52.53) |
| Internal drainage of pancreatic cyst (52.4) |
| Anastomosis of pancreas including intestine (52.96) |
| Liver procedures |
| Partial hepatectomy (50.22) |
| Hepatic lobectomy (50.3) |
| Other destruction of liver lesion (50.29) |
| Biliary procedures |
| Anastomosis of gallbladder or bile duct (51.3) |
| Local excision/destruction of lesion/tissue of bile ducts and sphincter of Oddi (51.6) |
| Excision of cystic duct remnant (51.61) |
| Other excision of common duct (51.63) |
| Excision of ampulla of Vater (with re-implantation of common duct) (51.62) |
| Choledochoenterostomy (51.36) |
| Pancreatic sphincteroplasty (51.83) |
| Choledochoplasty (51.72) |
| Revision of anastomosis of biliary tract (51.94) |
To evaluate the need for procedures in a given state's population, observed-to-expected (O–E) ratios were calculated. To obtain these ratios, a ratio was first calculated for a procedure in a given state. This was calculated by dividing the number of procedures performed in that state by the total number of procedures performed across the country. Next, a similar calculation was performed using population data for that state obtained in the 2011 US Census. This gave the proportion of each state's population to the total US population. The populations of Alabama, Alaska, Idaho and Delaware were subtracted from the total population.
The ratio of each state's procedures to the US total was then divided by each state's population ratio to give the O–E ratio of procedures performed. If a state had 15% of the US population, the expected proportion of procedures would also be 15%, giving a ratio of 1. Any state with a lower number of procedures performed would have a ratio of <1 and those with a higher number of procedures would have a ratio of >1. A state with a ratio of <1 would then be performing a lower than expected number of HPB procedures for its given population.
Results
The NIS dataset showed the number of procedures under the identified ICD-9 codes amounted to 6627 in 2005 and increased over time to 8515 in 2011. The rise in the number of procedures reflects the greater number of hospitals sampled each year by the NIS. Total numbers for each year are listed in Fig. 1. Data were separated according to state and the mean number of procedures was calculated over the study period. The mean was then mapped to the corresponding geographic location on a map of the USA. The log of each mean was taken to ensure a whole number, which was necessary for mapping. Figure 2 shows the mean numbers of procedures performed per state during 2005–2011. States that are shaded in green (Alabama, Delaware, Idaho) did not participate in the NIS data sample and were not included in the mapping. The darker colours indicate greater numbers of procedures were performed per year. The map shows that, as predicted, larger and more populated states such as California and Texas perform greater numbers of procedures per year than do smaller states, such as Maine and Wyoming.
Figure 1.
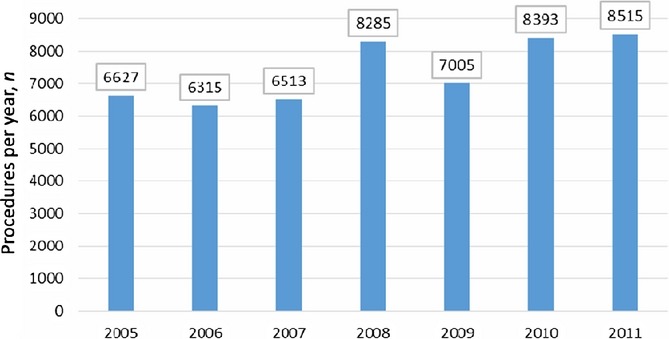
Numbers of HPB procedures listed in the National Inpatient Sample database as performed in the USA each year during 2005–2011
Figure 2.
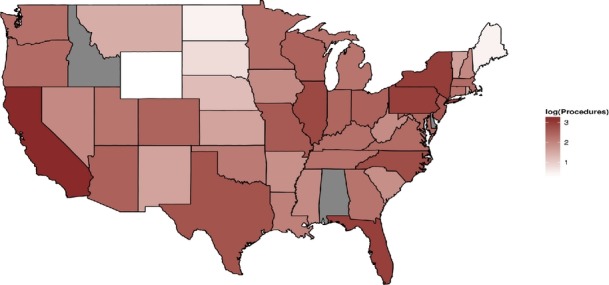
Mean number of HPB procedures performed per year in each state during 2005–2011. Darker shades indicate higher numbers of procedures
The O–E ratio of each state was calculated for all states participating in the NIS. These values were then mapped to geographic data as shown in Fig. 3. States in darker red have an O–E ratio of >1; those shown in white have an O–E ratio of 1, and those marked in blue have a ratio of <1.
Figure 3.
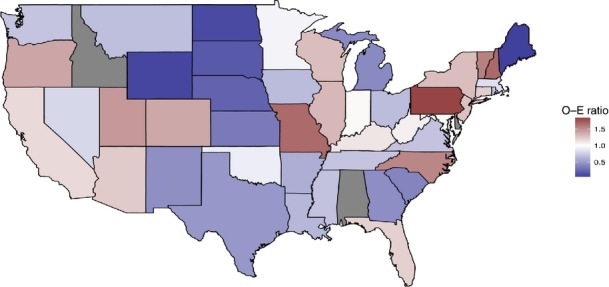
Ratio of observed-to-expected numbers of HPB procedures performed in each state during 2005–2011. A ratio of 1 implies that the number of procedures performed is proportional to that state's population
Only 18 states had ratios of >1. The remaining 28 states had ratios of ≤1. States such as Ohio and Texas had higher mean numbers of procedures (Fig. 1), but their populations resulted in O–E ratios of 0.66 and 0.48, respectively. Table 2 lists the O–E ratios of each state over the study period.
Table 2.
Ratios of observed-to-expected (O–E) numbers of HPB procedures performed in each state during 2005–2011a
| States with an O–E ratio of <1 | States with an O–E ratio of >1 | ||
|---|---|---|---|
| State | O–E ratio | State | O–E ratio |
| Maine | 0.05 | Indiana | 1.02 |
| Wyoming | 0.08 | Maryland | 1.04 |
| North Dakota | 0.10 | West Virginia | 1.07 |
| South Dakota | 0.17 | Kentucky | 1.12 |
| Nebraska | 0.22 | California | 1.17 |
| Kansas | 0.33 | Florida | 1.21 |
| South Carolina | 0.38 | Connecticut | 1.22 |
| Michigan | 0.41 | Arizona | 1.24 |
| Georgia | 0.43 | New Jersey | 1.28 |
| New Mexico | 0.44 | Wisconsin | 1.29 |
| Texas | 0.48 | New York | 1.30 |
| Hawaii | 0.50 | Illinois | 1.33 |
| Arkansas | 0.59 | Colorado | 1.40 |
| Louisiana | 0.64 | Oregon | 1.40 |
| Iowa | 0.66 | Utah | 1.46 |
| Ohio | 0.66 | North Carolina | 1.54 |
| Montana | 0.67 | Vermont | 1.57 |
| Rhode Island | 0.68 | Missouri | 1.66 |
| Mississippi | 0.69 | New Hampshire | 1.67 |
| Virginia | 0.69 | Pennsylvania | 1.83 |
| Washington | 0.70 | ||
| Tennessee | 0.71 | ||
| Nevada | 0.80 | ||
| Massachusetts | 0.84 | ||
| Oklahoma | 0.91 | ||
| Minnesota | 0.94 | ||
A ratio of 1 indicates that the number of procedures carried out is proportional to that state's population.
Discussion
These data demonstrate that higher numbers of procedures are performed in states with larger populations, such as California and Texas. However, when data for numbers of procedures are compared with population data, it becomes clear that the majority of the USA is under-represented with regard to HPB surgical procedures performed, with an O–E ratio of <1. Although this may reflect sampling error inherent in the NIS database, which does not pick up all HPB procedures performed, the finding that various areas show a lack of procedures across the years lends credibility to the suggestion that the volume of HPB procedures expected is not being performed or that these patients are travelling to other geographic locations for their care. Although many studies have shown that the regionalization of care improves outcomes, the reality is that the majority of patients do not want to or cannot travel for their care.12
In 1999, Birkmeyer et al. published data showing mortality rates after major surgery of 3.6% at high-volume centres and 16.8% at low-volume centres.13 This has led to a nationwide push towards the regionalization of care in larger hospitals. Other countries, such as Germany and Norway, have created a true regionalization of care in select centres, but no such system has been achieved in the USA. Many studies have shown that patients, even with the knowledge that a closer, smaller hospital has a higher mortality rate for a given procedure, will still choose the local centre over a more distant high-volume institution. Colavita et al. found that almost 40% of HPB surgery procedures performed during 2005–2009 were carried out in low-volume or medium-volume centres, which they defined as those conducting 28 or fewer resections per year.14 This contrasts with the method used by Birkmeyer et al., who defined a high-volume centre as one performing more than 12 procedures per year.13 These data indicate that a large proportion of the US population does not receive care in high-volume centres.
It is reasonable to postulate that the greatest need in the USA is to improve outcomes at low-volume centres rather than to presume that patients will travel to high-volume centres. This may also increase the rate of resection in patients with early-stage disease that warrants definitive surgical treatment which may not be offered currently at closer low-volume centres. A recent study from Australia shows similar rates of morbidity and mortality in pancreaticoduodenectomy performed at a low-volume centre in comparison with the same procedure performed at high-volume centres.15 The outcomes seen in this study were attributed to the presence of a specialized HPB surgery department with amenities similar to those at a high-volume centre. This included surgeons with HPB surgery fellowship training, along with other departments such as those of gastroenterology, radiology and oncology that are well equipped to deliver care to these patients. This suggests that HPB fellowship-trained surgeons are required in low- or intermediate-volume centres to improve outcomes. The training of graduates of these programmes should centre on the multidisciplinary care of HPB patients, rather than on the technical aspects of complex abdominal operations.
A distance bias refers to the fact that patients who can travel long distances for care often achieve better outcomes.12 This may contribute to the better outcomes reported by high-volume in comparison with low-volume centres. Patients who are able to travel to high-volume centres are often healthier and have better access to health care than others. This leads to better access to definitive surgical and medical treatment, which results in the better outcomes observed. The path to better outcomes should start with improvements of the standardization and care pathways at low-volume centres in order to ensure that all centres can meet the standards of a high-volume facility.
Each year, close to 100 fellows graduate from a training in HPB surgery through the surgical oncology, HPB fellowship and abdominal transplant pathways. However, positions at high-volume centres are limited and these fellows are faced with the reality of the job market. A recent study conducted in 2013 found that only 30% of general surgery job postings required fellowship training.6 This shows that the majority of need in the USA is for broad-based general surgery. As over 80% of graduating residents pursue fellowship training after general surgery residency,2 fellows should be aware that in reality the majority of their practice may not be limited to the area of their subspecialty training.
Wider strategy should encourage graduating HPB surgery fellows to bring the substantial breadth of their training and the systems processes learned in fellowship to populations that are identified as being underserved, while also serving the general surgical needs of the community. The multidisciplinary care team approach and practice-building aspect of an HPB surgery programme should represent important components of all HPB fellowship training. Greater standardization is needed to ensure that graduates of training pathways are educated and gain experience in learning treatment pathways and all aspects of multidisciplinary care. In addition, the importance of developing the provision of gastroenterology, medical and radiation oncology, and interventional radiology expertise at low-volume centres in order to ensure a team-based approach to the care of complex HPB patients, who cannot be managed by the surgeon alone, should be emphasized. The current focus on outcomes transparency highlights the need to improve care in low-volume centres through a systems approach, rather than reducing opportunities for surgical resection based on reimbursement considerations.
Conclusions
Within the USA, many states perform high volumes of HPB surgery each year, yet the majority of the US population is underserved for this subset of surgical procedures. Training in HPB surgery should be encouraged to meet the demands of the population and to bring better outcomes to smaller and underserved populations. As resident training case numbers in HPB surgery are not increasing, fellowship training must bring the technical skills and systems-building processes required to the majority of the US population.
Conflicts of interest
None declared.
References
- Borman KR, Vick LR, Biester TW, Mitchell ME. Changing demographics of residents choosing fellowships: longterm data from the American Board of Surgery. J Am Coll Surg. 2008;206:782–788. doi: 10.1016/j.jamcollsurg.2007.12.012. ; discussion 788–789. [DOI] [PubMed] [Google Scholar]
- Stitzenberg KB, Sheldon GF. Progressive specialization within general surgery: adding to the complexity of workforce planning. J Am Coll Surg. 2005;201:925–932. doi: 10.1016/j.jamcollsurg.2005.06.253. [DOI] [PubMed] [Google Scholar]
- Rassadi R, Dickerman RM, Dunn EL, Tarnasky PR, Linder JD, Mejia A, et al. Hepatopancreaticobiliary (HPB) surgery: what is the right fellowship for the right training? J Surg Educ. 2008;65:186–190. doi: 10.1016/j.jsurg.2007.11.012. [DOI] [PubMed] [Google Scholar]
- Helling TS, Khandelwal A. The challenges of resident training in complex hepatic, pancreatic, and biliary procedures. J Gastrointest Surg. 2008;12:153–158. doi: 10.1007/s11605-007-0378-6. [DOI] [PubMed] [Google Scholar]
- Scarborough JE, Pietrobon R, Bennett KM, Clary BM, Kuo PC, Tyler DS, et al. Workforce projections for hepato-pancreato-biliary surgery. J Am Coll Surg. 2008;206:678–684. doi: 10.1016/j.jamcollsurg.2007.11.016. [DOI] [PubMed] [Google Scholar]
- Decker MR, Bronson NW, Greenberg CC, Dolan JP, Kent KC, Hunter JG. The general surgery job market: analysis of current demand for general surgeons and their specialized skills. J Am Coll Surg. 2013;217:1133–1139. doi: 10.1016/j.jamcollsurg.2013.07.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang DC, Zhang Y, Mukherjee D, Wolfgang CL, Schulick RD, Cameron JL, et al. Variations in referral patterns to high-volume centres for pancreatic cancer. J Am Coll Surg. 2009;209:720–726. doi: 10.1016/j.jamcollsurg.2009.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riall TS, Eschbach KA, Townsend CM, Jr, Nealon WH, Freeman JL, Goodwin JS. Trends and disparities in regionalization of pancreatic resection. J Gastrointest Surg. 2007;11:1242–1251. doi: 10.1007/s11605-007-0245-5. ; discussion 1251–1252. [DOI] [PubMed] [Google Scholar]
- Birkmeyer JD, Siewers AE, Marth NJ, Goodman DC. Regionalization of high-risk surgery and implications for patient travel times. JAMA. 2003;290:2703–2708. doi: 10.1001/jama.290.20.2703. [DOI] [PubMed] [Google Scholar]
- Dunderdale J, McAuliffe JC, McNeal SF, Bryant SM, Yancey BD, Flowers G, et al. Should pancreatectomy with islet cell autotransplantation in patients with chronic alcoholic pancreatitis be abandoned? J Am Coll Surg. 2013;216:591–596. doi: 10.1016/j.jamcollsurg.2012.12.043. ; discussion 596–598. [DOI] [PubMed] [Google Scholar]
- US Census Bureau. Incorporated Places and Minor Civil Divisions. Datasets: subcounty resident population estimates: April 1, 2010 to July 1, 2012. Available at http://www.census.gov/popest/data/cities/totals/2012/SUB-EST2012.html (last accessed 15 January 2014)
- Etzioni DA, Fowl RJ, Wasif N, Donohue JH, Cima RR. Distance bias and surgical outcomes. Med Care. 2013;51:238–244. doi: 10.1097/MLR.0b013e318270bbfa. [DOI] [PubMed] [Google Scholar]
- Birkmeyer JD, Finlayson SR, Tosteson AN, Sharp SM, Warshaw AL, Fisher ES. Effect of hospital volume on in-hospital mortality with pancreaticoduodenectomy. Surgery. 1999;125:250–256. [PubMed] [Google Scholar]
- Colavita PD, Tsirline VB, Belyansky I, Swan RZ, Walters AL, Lincourt AE, et al. Regionalization and outcomes of hepato-pancreato-biliary cancer surgery in USA. J Gastrointest Surg. 2014;18:532–541. doi: 10.1007/s11605-014-2454-z. [DOI] [PubMed] [Google Scholar]
- Kanhere H, Satyadas T, Maddern GJ. Surgical outcomes following pancreatic resection at a low-volume community hospital. Do all patients need to be sent to a regional cancer centre? Am J Surg. 2010;199:866–867. doi: 10.1016/j.amjsurg.2009.09.030. [DOI] [PubMed] [Google Scholar]


