Abstract
Background
There are controversial data regarding infarct-related artery only (IRA-PCI) revascularisation versus multivessel revascularisation (MV-PCI) in ST-elevation myocardial infarction (STEMI) patients with multivessel disease undergoing primary percutaneous coronary intervention (PCI). We performed a meta-analysis comparing outcome in same stage MV-PCI versus IRA-PCI in STEMI patients with multivessel disease.
Methods
Systematic searches of studies comparing MV-PCI with IRA-PCI in the MEDLINE and the Cochrane Database of systematic reviews were conducted. A meta-analysis was performed of all available studies. Primary outcome was all-cause mortality. Secondary endpoints were re-infarction, revascularisation, bleeding and major adverse cardiac events (MACE).
Results
A total of 15 studies were identified with a total number of 35,975 patients. Mortality rate was significantly higher in the MV-PCI group compared with the IRA-PCI group, odds ratio (OR): 1.64 (1.46–1.85). Both the incidence of re-infarction and re-PCI were significantly lower in the MV-PCI group compared with the IRA-PCI group: OR 0.54 (0.34–0.88) and OR 0.67 (0.48–0.93), respectively. Bleeding complications occurred more often in the MV-PCI group as compared with the IRA-PCI group: OR 1.24 (1.08–1.42). Rates of MACE were comparable between the two groups.
Conclusions
MV-PCI during the index of primary PCI in STEMI patients is associated with a higher mortality rate, a higher risk of bleeding complications, but lower risk of re-intervention and re-infarction and comparable rates of MACE.
Keywords: STEMI, Multivessel diseases, Multivessel PCI, Infarct-related artery
Background
About half of the patients presenting with ST-elevation myocardial infarction (STEMI) have multivessel disease. Compared with STEMI patients with single-vessel disease, STEMI patients with multivessel disease have a worse prognosis [1–3].
The current guidelines recommend intervention in the infarct-related artery only during primary percutaneous coronary intervention (PCI) except in haemodynamically unstable patients [4]; this is mainly due to the fact that evidence supporting immediate (preventive) intervention in the non-infarct-related artery is a matter of debate.
There are controversial data regarding infarct-related artery only revascularisation (IRA-PCI) versus multivessel revascularisation (MV-PCI) in STEMI patients with multivessel disease [5–19].
Previously, other meta-analyses assessed MV-PCI versus IRA-PCI; however, in those meta-analysis, MV-PCI was defined as same stage PCI as well as staged PCI days after the primary PCI. Furthermore, the results of the most recent trials were not included [20–23].
We performed a meta-analysis comparing outcome in MV-PCI versus IRA-PCI during the index of primary PCI in STEMI patients with multivessel disease.
Methods
Literature review
The literature search was performed from Cochrane Library, EMBASE and MEDLINE, from January 2014 to December 2014. The terms “ST-elevation myocardial infarction”, “coronary angioplasty”, “percutaneous coronary intervention”, “multi-vessel”, “non-culprit”, “culprit coronary revascularisation”, “complete revascularisation”, “myocardial infarction” and their variations were used as keywords. The search was limited to records in humans and English language articles.
Study selection
Two reviewers independently screened all citations for eligibility. Both randomised controlled trials (RCTs) and cohort studies comparing multivessel versus culprit-only PCI in patients with STEMI and multivessel coronary artery disease treated with primary PCI were included. Studies enrolling patients with other than STEMI or comparing alternative revascularisation strategies were excluded. Full-text citations and abstracts were selected and independently screened for eligibility in the meta-analysis. The unpublished Complete Versus culprit-Lesion only PRimary PCI Trial (CVLPRIT) was also included because of its importance for this meta-analysis [20]. Quality of abstracted studies was assessed using the Cochrane Collaboration’s tool for assessing risk of bias [24].
Information on study design, inclusion and exclusion criteria, number of patients and clinical outcome was extracted by two investigators. Disagreements were resolved by consensus. Finally, all co-authors had full access to all study data and take responsibility for the integrity of the data and the accuracy of the data analysis.
Definitions
MV-PCI was defined as PCI of the infarct-related artery (IRA) and non-IRA performed during the index primary PCI procedure for STEMI. IRA-PCI is defined as the PCI of the IRA only during the index primary PCI procedure. Major adverse cardiac event (MACE) was defined as the composite of death, re-infarction and revascularisation. Bleeding included both minor and major bleeding.
Endpoints/data abstraction
The primary clinical endpoint was all-cause mortality. Secondary endpoints were re-infarction, revascularisation, bleeding and MACE.
Statistical analysis
Continuous data were expressed as mean ± standard deviation and dichotomous data as absolute values and percentages. Mantel–Haenszel model was used to construct random effects summary odds ratios (ORs) and risk differences. All analyses were performed using Review Manager (RevMan, Version 5.0, The Nordic Cochrane Centre, The Cochrane Collaboration 2008) and SAS 9.3, (SAS Institute, Cary, NC). p-Value < 0.05 was considered statistically significant.
Results
The search yielded 15 studies [5–19]: 5 RCTs and 10 cohort studies. The characteristics of the included studies are shown in Table 1. A total of 35,975 patients comprised the study population including 1134 (3.2 %) patients from RCTs. MV-PCI was performed in 5109 (12.2 %) patients, and 30,939 (85.8 %) patients underwent IRA-PCI.
Table 1.
Study characteristics
| Study | Design | Subjects | Inclusion criteria | Exclusion criteria | Primary endpoint | Mean length follow-up |
|---|---|---|---|---|---|---|
| Cavender | Cohort study | 28,936 | STEMI with CAD of > 1 major artery | LM, staged PCI (multiple PCIs before hospital discharge), thrombolytic | In-hospital mortality | In-hospital |
| Corpus | Cohort study | 532 | STEMI with > 70 % stenosis of ≥ 2 arteries | PCI of graft or after angioplasty, LM, planned staged revascularisation | MACE | 12 months |
| Di Mario | Randomised | 69 | STEMI with MVD and 1–3 lesions in non-culprit artery technically amenable to revascularisation by stent | Lesion in vein and arterial grafts, prior angioplasty, thrombolytic, cardiogenic shock, LM | Repeat revascularisation | 12 months |
| Dziewierz | Cohort study | 777 | STEMI with MVD 2–3 lesions in non-culprit artery | CABG | All-cause mortality | 12 months |
| Hannan | Cohort study | 1006 | STEMI with MVD | LM disease, prior thrombolysis, prior CABG, cardiogenic shock, missing EF | All-cause mortality | 42 months |
| Khattab | Cohort study | 73 | STEMI with > 70 % stenosis of ≥ 2 coronary arteries or major branches | Non-IRA diameter < 2.5 mm, LM disease, previous MI | MACE | 12 months |
| Kornowski | Cohort study | 668 | STEMI with MVD | TIMI flow < 3 in non-IRA | MACE | 12 months |
| Ochala | Randomised | 92 | STEMI with > 70 % stenosis of ≥ 2 coronary arteries, successful PCI of IRA | Cardiogenic shock, LM disease, pervious CABG, renal insufficiency, severe valvular disease | Improvement in LVEF | 6 months |
| Politi | Randomised | 214 | STEMI with > 70 % stenosis of ≥ 2 coronary arteries or major branches | Cardiogenic shock, LM > 50 %, pervious CABG, severe valvular heart disease or unsuccessful procedure | MACE | 30 months |
| Qarawani | Cohort study | 120 | STEMI with > 70 % multivessel narrowing | Cardiogenic shock, LM disease | Clinical outcome | 12 months |
| Roe | Cohort study | 129 | STEMI with ≥ 50 % stenosis of ≥ 1 non-culprit artery in addition to culprit IRA | PCI of branch vessels of IRA, LM disease | MACE (death, re-MI, and revascularisation) | 6 months |
| Toma | Cohort study | 2201 | STEMI with > 70 % stenosis of > 1 major epicardial artery and/or a non-IRA requiring intervention | PCI on LM, second intervention in the culprit artery | MACE (death, CHF, shock) | 3 months |
| Varani | Cohort study | 399 | STEMI with > 70 % stenosis of ≥ 2 epicardial arteries or major branches | Occlusion after prior angioplasty, cardiogenic shock, pulmonary oedema | Death and repeat revascularisation | 1 month |
| Wald | Randomised | 465 | STEMI with ≥ 50 % stenosis of ≥ 1 non-IRA in addition to IRA | Cardiogenic shock, LM > 50 %, pervious CABG | MACE | 23 months |
| Gershlick | Randomised | 294 | STEMI with > 70 % stenosis of ≥ 2 epicardial arteries or major branches (> 2 mm) | Cardiogenic shock, previous MI, pervious CABG, chronic kidney disease, CTO | MACE | 12 months |
CABG coronary artery bypass graft, CAD coronary artery disease, CHF congestive heart failure, CTO chronic total occlusion, IRA infarct-related artery, LM left main artery, LVEF left ventricular ejection fraction, MACE major adverse cardiac events, MI myocardial infarction, MVD multivessel disease, PCI percutaneous coronary intervention, STEMI ST-elevation myocardial infarction, TIMI thrombolysis in myocardial infarction
Patient characteristics
Table 2 shows the baseline characteristics of the study population. The vast majority of the studies excluded patients with cardiogenic shock and in two trials cardiogenic shock was not reported.
Table 2.
Baseline characteristics
| Age | Male (%) | Diabetes (%) | Anterior MI (%) | Cardiogenic shock (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study | MV-PCI | IRA-PCI | MV-PCI | IRA-PCI | MV-PCI | IRA-PCI | MV-PCI | IRA-PCI | MV-PCI | IRA-PCI |
| Cavender | 60 | 62 | 71.5 | 72.1 | 24.7 | 23.4 | NR | NR | 13.8 | 10.3 |
| Corpus | 64 | 63 | 70 | 70 | 19 | 17 | NR | NR | 3.3 | 3.4 |
| Di Mario | 64 | 65 | 88.2 | 84.6 | 11.5 | 41.5 | 51.9 | 58.8 | Excluded | Excluded |
| Dziewier | 68 | 68 | 72.2 | 72.2 | NR | NR | NR | NR | Not reported | Not reported |
| Hannan | NR | NR | 77.5 | 75.5 | 23.7 | 21.4 | NR | NR | Excluded | Excluded |
| Khattab | 69 | 65 | 75 | 78 | 7 | 16 | 57 | 54 | 3.6 | 4.4 |
| Kornowski | 62 | 63.5 | 80.9 | 79.6 | 15.3 | 18.1 | 40.6 | 35.1 | Not reported | Not reported |
| Ochala | 65 | 67 | 72.9 | 75 | 31 | 34 | 45.8 | 45.4 | Excluded | Excluded |
| Politi | 65 | 65 | 76.9 | 77.8 | 14 | 21 | 48 | 43 | Excluded | Excluded |
| Qarawani | 66 | 67 | 62 | 61 | 13 | 16 | 51 | 52 | Excluded | Excluded |
| Roe | 64 | 63 | 77.2 | 65.8 | 37 | 29 | 46 | 41 | 28 | 28 |
| Toma | 64 | 64 | 74 | 73 | 12 | 20 | 56 | 48 | 3 | 3 |
| Varani | 69 | 67 | 68.7 | 67 | NR | NR | 49 | 34 | Excluded | Excluded |
| Wald | 62 | 62 | 76 | 81 | 35 | 48 | 29 | 39 | Excluded | Excluded |
| Gershlick | 65 | 65 | 85 | 77 | 12.9 | 14.3 | 36 | 35.6 | Excluded | Excluded |
IRA-PCI infarct-related artery only revascularisation, MI myocardial infarction, MV-PCI multivessel revascularisation, NR not reported
Clinical outcomes
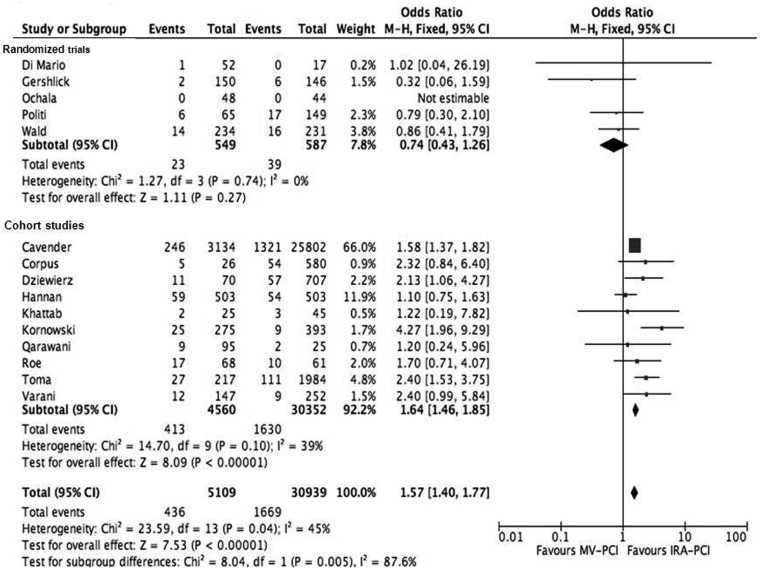
The primary endpoint, all-cause mortality, was significantly higher in the MV-PCI (8.5 %) compared with the IRA-PCI (5.4 %) group (OR 1.57, 95 % CI 1.40–1.76, p < 0.001) (Fig. 1). However, analysis limited to the five RCTs only showed no significant difference in mortality rate between MV-PCI and IRA-PCI (OR 0.74, 95 % CI 0.43–1.26, p = 0.27).
Fig. 1.
Forest plot of all-cause mortality
Secondary endpoints
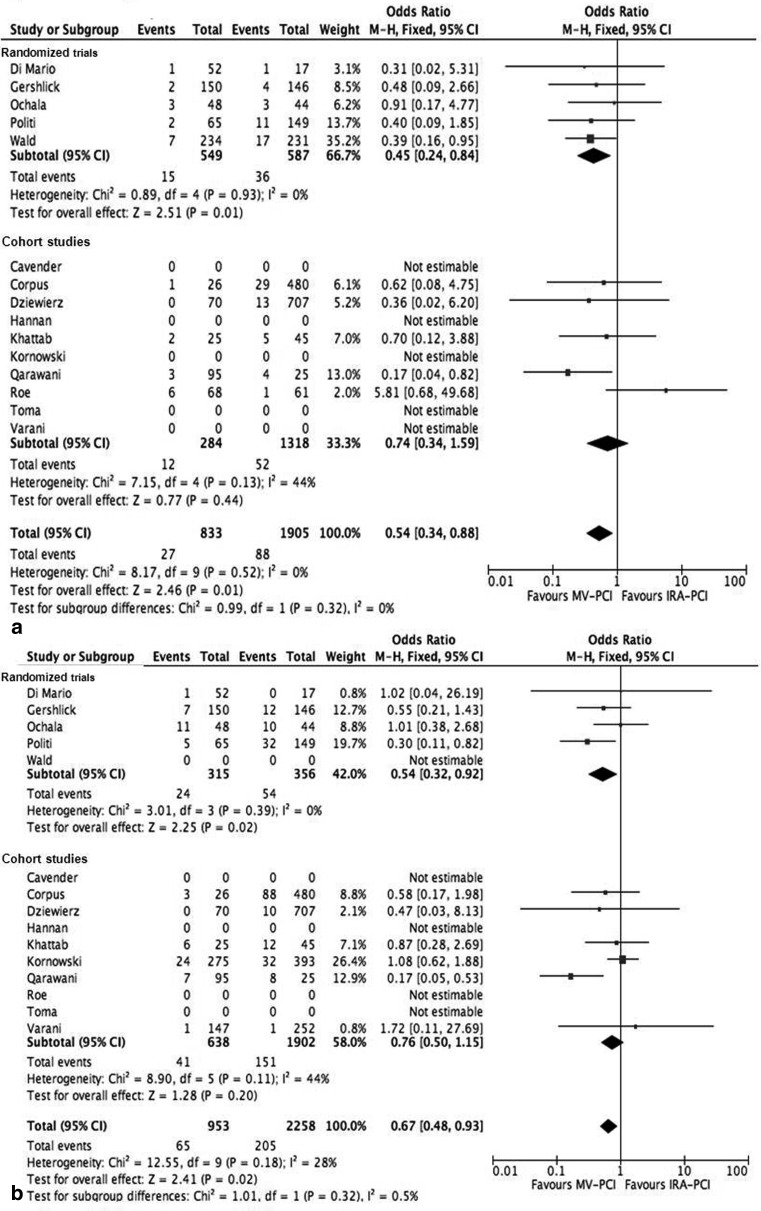
Rates of re-infarction (OR 0.54, 95 % CI 0.34–0.88, p = 0.01) and revascularisation (OR 0.67, 95 % CI 0.48–0.93, p = 0.002) were lower in the MV-PCI group. This was found for both randomised and cohort trials (Fig. 2a and b).
Fig. 2.
a Forest plot of re-infarction. b Forest plot of re-percutaneous coronary intervention
Bleeding complications (major and minor) occurred more often in the MV-PCI group: 6.2 versus 5.1 %, (OR 1.24, 95 % CI 1.08–1.42, p = 0.002) and this was mainly found in the cohort studies (Fig. 3).
Fig. 3.
Forest plot of bleeding (major and minor)
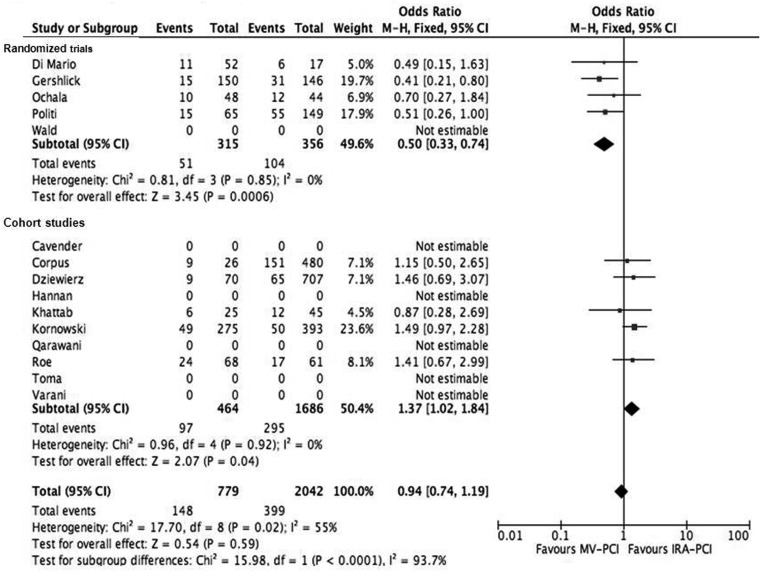
MACE was comparable between the two groups: 19 versus 19.5 % (OR 0.94, 95 % CI 0.74–1.19, p = 0.59). In the RCT trials, MACE was significantly lower in patients undergoing MV-PCI compared with the IRA-PCI group (Fig. 4).
Fig. 4.
Forest plot of major adverse cardiac events (death, re-infarction and re-percutaneous coronary intervention)
Discussion
In this large scale meta-analysis, we found that PCI of the IRA and non-IRA performed during the index primary PCI procedure for STEMI, compared with IRA-only PCI, is associated with a higher mortality rate and more bleeding complications, but less re-infarction and revascularisation. Rates of MACE were comparable between the two groups. However, there was a clear difference in outcome between the randomised trials and cohort studies. In the cohort studies, mortality and bleeding complications were significantly higher in the MV-PCI group; however, these were not significantly different in the randomised trials between the MV-PCI group versus IRA-PCI group (Figs. 1 and 4).
Approximately 40–65 % of patients with STEMI have multivessel disease with increased risk of morbidity and mortality compared with single-vessel disease [1–3]. The underlying mechanism for this adverse prognosis may be plaque instability, impaired myocardial perfusion and contractility, arrhythmia and death.
The potential advantages of MV-PCI during the index primary PCI may prevent recurrent ischaemia and infarction by decreasing total ischaemia and improvement in myocardial function [25, 26]. Plaque instability may not be limited to the IRA but may involve other territories in the coronary vasculature. Moreover, complete revascularisation has been associated with improved long-term clinical outcome in patients with stable coronary artery disease. Finally, patients and clinicians may be more comfortable with complete revascularisation rather than medical therapy for angiographically significant residual coronary stenosis, especially if they are associated with a large territory of myocardial jeopardy [27–30].
However, multivessel PCI also has disadvantages. In the acute phase of STEMI, intervention of a non-culprit lesion may result in unnecessary haemodynamic compromise during PCI with balloon inflations or vessel-related complications (dissection, no-reflow) at a time when the patient has regional myocardial compromise. Given the extended duration of the intervention, increased contrast load and additional adverse peri-procedural outcomes may occur. Another important concern is poor assessment of lesion severity in non-culprit artery [22]. Hanratty et al. [30] demonstrated that 21 % of the non-culprit lesions are overestimated at time of AMI, and this may affect unnecessary revascularisation and inappropriate decision making. The severity of the non-culprit artery was judged visually and PCI of the non-IRA was not ischaemia guided in any of the studies included in this meta-analysis.
There is only one randomised study in which revascularisations on the non-IRA was guided by fractional flow reserve (FFR). FFR of the non-IRA was performed 7.5 days after primary PCI, and they found functional stenosis severity of non-culprit lesions is frequently overestimated and invasive strategy for non-culprit lesions did not lead to an increase in ejection fraction or a reduction in MACE [31].
Prior meta-analyses in this area have reported varying results due to differences in study design, comparison of different groups and different analytical methods [20–23]. Vlaar et al. [20] found that the strategy of staged PCI resulted in lower short- and long-term mortality compared with MV-PCI or IRA-PCI. Bangalore et al. [21] found that MV-PCI compared with IRA-PCI resulted in similar long-term mortality but a lower long-term rate of MACE. A recent meta-analysis showed that MV-PCI compared with IRA-PCI resulted in worse outcomes in cohort studies, but not in the randomised clinical trials [22]. This is in line with our findings.
Furthermore, Bainey et al. [23] found that staged multivessel PCI was superior to multivessel PCI during the index procedure.
The difference in outcome between the IRA-only and MV-PCI group may not only be due to revascularisation, differences in baseline may also play an important role. Patients in the MV-PCI group have a higher baseline risk evidenced by a higher proportion of anterior myocardial infarction and more cardiogenic shock.
Based on the current evidence, we think that in the acute phase of STEMI, revascularisation should be limited to the IRA only, except in patients with haemodynamic instability, as recommended by the current guidelines [4]. Staged and ischaemia-driven revascularisation of non-culprit lesions may be the treatment strategy for STEMI patients with multivessel disease. Further studies are needed to confirm this. The current ongoing COMPLETE and COMPARE ACUTE trials are studying these issues.
Limitations
This meta-analysis was not performed on individual patient data. Caution should be exercised in the interpretation of the results, given the potential clinical heterogeneity among trials, due to varying patient populations and potential treatment bias. No information was available with regard to extent of coronary disease, use of drug-eluting stents, duration of dual antiplatelet therapy and access site. The short follow-up period of some studies is another important limitation. Furthermore, only a minority of the patients (14.2 %) undergo MV-PCI during the index procedure, so it is hard to draw definitive conclusions based on this meta-analysis.
In addition, no information was available regarding referral method, ambulance versus referring via non-PCI centres, factors that may affect total ischaemic time [32].
Finally, although the STEMI and non-STEMI are not uniquely related to different pathophysiological mechanisms [33], our results cannot be applied to non-STEMI patients with multivessel disease.
Conclusion
Multivessel PCI during the index of primary PCI in STEMI patients is associated with a higher mortality and more bleeding, but a lower risk of re-intervention and re-infarction. Additional large-scale randomised trials are needed to guide the therapy and the timing for these patient subsets.
Funding
None.
Conflict of interest
None.
References
- 1.van der Schaaf RJ, Timmer JR, Ottervanger JP. Long-term impact of multivessel disease on cause-specific mortality after ST elevation myocardial infarction treated with reperfusion therapy. Heart. 2006;92:1760–3. doi: 10.1136/hrt.2005.086058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muller DW, Topol EJ, Ellis SG. Multivessel coronary artery disease: a key predictor of short-term prognosis after reperfusion therapy for acute myocardial infarction. Thrombolysis and Angioplasty in Myocardial Infarction (TAMI) Study Group. Am Heart J. 1991;121:1042–9. doi: 10.1016/0002-8703(91)90661-Z. [DOI] [PubMed] [Google Scholar]
- 3.Sorajja P, Gersh BJ, Cox DA. Impact of multivessel disease on reperfusion success and clinical outcomes in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Eur Heart J. 2007;28:1709–16. doi: 10.1093/eurheartj/ehm184. [DOI] [PubMed] [Google Scholar]
- 4.The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC) ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33:2569–619. doi: 10.1093/eurheartj/ehs215. [DOI] [PubMed] [Google Scholar]
- 5.Cavender MA, Milford-Beland S, Roe MT. Prevalence, predictors, and in-hospital outcomes of non-infarct artery intervention during primary percutaneous coronary intervention for ST-segment elevation myocardial infarction (from the National Cardiovascular Data Registry) Am J Cardiol. 2009;104:507–13. doi: 10.1016/j.amjcard.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 6.Corpus RA, House JA, Marso SP. Multivessel percutaneous coronary intervention in patients with multivessel disease and acute myocardial infarction. Am Heart J. 2004;148:493–500. doi: 10.1016/j.ahj.2004.03.051. [DOI] [PubMed] [Google Scholar]
- 7.Di Mario C, Mara S, Flavio A. Single vs multivessel treatment during primary angioplasty: results of the multicentre randomised HEpacoat for cuLPrit or multivessel stenting for Acute Myocardial Infarction (HELP AMI) Study. Int J Cardiovasc Intervent. 2004;6:128–33. doi: 10.1080/14628840310030441. [DOI] [PubMed] [Google Scholar]
- 8.Dziewierz A, Siudak Z, Rakowski T. Impact of multivessel coronary artery disease and noninfarct-related artery revascularization on outcome of patients with ST-elevation myocardial infarction transferred for primary percutaneous coronary intervention (from the EUROTRANSFER Registry) Am J Cardiol. 2010;106:342–7. doi: 10.1016/j.amjcard.2010.03.029. [DOI] [PubMed] [Google Scholar]
- 9.Hannan EL, Samadashvili Z, Walford G. Culprit vessel percutaneous coronary intervention versus multivessel and staged percutaneous coronary intervention for ST-segment elevation myocardial infarction patients with multivessel disease. JACC Cardiovasc Interv. 2010;3:22–31. doi: 10.1016/j.jcin.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 10.Khattab AA, Abdel-Wahab M, Rother C. Multi-vessel stenting during primary percutaneous coronary intervention for acute myocardial infarction. A single-center experience. Clin Res Cardiol. 2008;97:32–8. doi: 10.1007/s00392-007-0570-4. [DOI] [PubMed] [Google Scholar]
- 11.Kornowski R, Mehran R, Dangas G. Prognostic impact of staged versus “one-time” multivessel percutaneous intervention in acute myocardial infarction: analysis from the HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infarction) trial. J Am Coll Cardiol. 2011;58:704–11. doi: 10.1016/j.jacc.2011.02.071. [DOI] [PubMed] [Google Scholar]
- 12.Ochala A, Smolka GA, Wojakowski W. The function of the left ventricle after complete multivessel one-stage percutaneous coronary intervention in patients with acute myocardial infarction. J Invasive Cardiol. 2004;16:699–702. [PubMed] [Google Scholar]
- 13.Politi L, Sgura F, Rossi R. A randomised trial of target-vessel versus multi-vessel revascularisation in ST-elevation myocardial infarction: major adverse cardiac events during long-term follow-up. Heart. 2010;96:662–7. doi: 10.1136/hrt.2009.177162. [DOI] [PubMed] [Google Scholar]
- 14.Qarawani D, Nahir M, Abboud M. Culprit only versus complete coronary revascularization during primary PCI. Int J Cardiol. 2008;123:288–92. doi: 10.1016/j.ijcard.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 15.Roe MT, Cura FA, Joski PS. Initial experience with multivessel percutaneous coronary intervention during mechanical reperfusion for acute myocardial infarction. Am J Cardiol. 2001;88:170–3. doi: 10.1016/S0002-9149(01)01615-0. [DOI] [PubMed] [Google Scholar]
- 16.Toma M, Buller CE, Westerhout CM. Non-culprit coronary artery percutaneous coronary intervention during acute ST-segment elevation myocardial infarction: insights from the APEX-AMI trial. Eur Heart J. 2010;31:1701–7. doi: 10.1093/eurheartj/ehq129. [DOI] [PubMed] [Google Scholar]
- 17.Varani E, Balducelli M, Aquilina M. Single or multivessel percutaneous coronary intervention in ST-elevation myocardial infarction patients. Catheter Cardiovasc Interv. 2008;72:927–33. doi: 10.1002/ccd.21722. [DOI] [PubMed] [Google Scholar]
- 18.Wald DS, Morris JK, Wald NJ. PRAMI Investigators. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med. 2013;369:1115–23. doi: 10.1056/NEJMoa1305520. [DOI] [PubMed] [Google Scholar]
- 19.The Complete Versus culprit-Lesion only PRimary PCI Trial (CVLPRIT). http://www.escardio.org/about/press/esc-congress-2014/press-conferences/Documents/gershlick.pdf (Hotline Session, ESC 1 sep. 2014).
- 20.Vlaar PJ, Mahmoud KD, Holmes DR., Jr. Culprit vessel only versus multivessel and staged percutaneous coronary intervention for multivessel disease in patients presenting with ST-segment elevation myocardial infarction: a pairwise and network meta-analysis. J Am Coll Cardiol. 2011;58:692–703. doi: 10.1016/j.jacc.2011.03.046. [DOI] [PubMed] [Google Scholar]
- 21.Bangalore S, Kumar S, Poddar KL. Meta-analysis of multivessel coronary artery revascularization versus culprit-only revascularization in patients with ST-segment elevation myocardial infarction and multivessel disease. Am J Cardiol. 2011;107:1300–10. doi: 10.1016/j.amjcard.2010.12.039. [DOI] [PubMed] [Google Scholar]
- 22.Bagai A, Thavendiranathan P, Sharieff W, Al Lawati HA, Cheema AN. Non-infarct-related artery revascularization during primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review and meta-analysis. Am Heart J. 2013;166:684–693. doi: 10.1016/j.ahj.2013.07.027. [DOI] [PubMed] [Google Scholar]
- 23.Bainey KR, Mehta SR, Lai T, Welsh RC. Complete vs culprit-only revascularization for patients with multivessel disease undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review and meta-analysis. Am Heart J. 2014;167:1–14. doi: 10.1016/j.ahj.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 24.Higgins JP. Cochrane handbook for systematic reviews of interventions. West Sussex: Wiley; 2008. [Google Scholar]
- 25.Asakura M, Ueda Y, Yamaguchi O. Extensive development of vulnerable plaques as a pan-coronary process in patients with myocardial infarction: an angioscopic study. J Am Coll Cardiol. 2001;37:1284–8. doi: 10.1016/S0735-1097(01)01135-4. [DOI] [PubMed] [Google Scholar]
- 26.Goldstein JA, Demetriou D, Grines CL. Multiple complex coronary plaques in patients with acute myocardial infarction. N Engl J Med. 2000;343:915–22. doi: 10.1056/NEJM200009283431303. [DOI] [PubMed] [Google Scholar]
- 27.Bell MR, Gersh BJ, Schaff HV. Effect of completeness of revascularization on long-term outcome of patients with three-vessel disease undergoing coronary artery bypass surgery. A report from the Coronary Artery Surgery Study (CASS) Registry. Circulation. 1992;86:446–57. doi: 10.1161/01.CIR.86.2.446. [DOI] [PubMed] [Google Scholar]
- 28.Jones EL, Weintraub WS. The importance of completeness of revascularization during long-term follow-up after coronary artery operations. J Thorac Cardiovasc Surg. 1996;112:227–37. doi: 10.1016/S0022-5223(96)70243-X. [DOI] [PubMed] [Google Scholar]
- 29.Wu C, Dyer AM, King SB., III Impact of incomplete revascularization on long-term mortality after coronary stenting. Circ Cardiovasc Interv. 2011;4:413–21. doi: 10.1161/CIRCINTERVENTIONS.111.963058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hanratty CG, Koyama Y, Rasmussen HH. Exaggeration of nonculprit stenosis severity during acute myocardial infarction: implications for immediate multivessel revascularization. J Am Coll Cardiol. 2002;40:911–6. doi: 10.1016/S0735-1097(02)02049-1. [DOI] [PubMed] [Google Scholar]
- 31.Dambrink JH, Debrauwere JP, van AW. Non-culprit lesions detected during primary PCI: treat invasively or follow the guidelines? Eurointervention. 2010;5:968–75. doi: 10.4244/EIJV5I8A162. [DOI] [PubMed] [Google Scholar]
- 32.Postma S, Dambrink JH, de Boer MJ. The influence of residential distance on time to treatment in ST-elevation myocardial infarction patients. Neth Heart J. 2014;22:513–9. doi: 10.1007/s12471-014-0599-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.IJkema BB, Bonnier JJ, Schoors D, Schalij MJ, Swenne CA. Role of the ECG in initial acute coronary syndrome triage: primary PCI regardless presence of ST elevation or of non-ST elevation. Neth Heart J. 2014;22:484–90. doi: 10.1007/s12471-014-0598-9. [DOI] [PMC free article] [PubMed] [Google Scholar]