Abstract
A 43-year-old man suffering from Klebsiella liver abscess and bacteraemia presented with left eye visual disturbance a few days after admission. His visual acuity was 6/6. There was a whitish subretinal mass located at the temporal periphery without vitritis. His visual acuity dropped to 6/120 with marked vitritis 1 day later and a diagnosis of a subretinal abscess was made. The vitreous cultures were negative. Response was suboptimal with intravitreal antibiotics, and retinotomy, vitrectomy, antibiotic irrigation and silicone oil tamponade were required. His vision gradually improved to 6/60 with silicone oil in situ. This case illustrates the rare presentation of a subretinal abscess in endogenous endophthalmitis with no initial associated vitritis, and the importance of maintaining a high level of suspicion despite good visual acuity on presentation in cases with relevant history. Early detection and intervention, and close monitoring may salvage the patient's vision in such cases.
Background
Endogenous endophthalmitis is the haematogenous spread of organism to the eye by crossing the blood-retina barrier. Gram-negative bacterial endophthalmitis is more common in Asia and Klebsiella pneumoniae is emerging as a popular culprit.1 2 Diabetes mellitus, intravenous drug addiction, indwelling catheters and malignancy are common risk factors.3 4 Liver abscess is a common cause of systemic infection.5 The presenting visual acuity is usually poor, such as hand movement or worse, especially if the disease is bacterial in origin.3 Endogenous endophthalmitis patients tend to have a poor visual prognosis despite early and aggressive treatment, and there is no formal guideline for screening or treatment specific to endogenous endophthalmitis, though guidelines on postoperative endophthalmitis may shed some light on its management.6 7 The Endophthalmitis Vitrectomy Study and the recent European Society of Cataract & Refractive Surgeons guidelines focused on postoperative endophthalmitis.6 7 Their results may not be totally applicable, as the spectrum of causative organism and pathogenesis differs significantly.8 Subretinal abscesses were more commonly related to Nocardia systemic infection.9 K. pneumoniae-related endogenous endophthalmitis presenting with a subretinal abscess is rare and none of the reported cases have described good visual acuity on presentation.9 10
Case presentation
A 43-year-old man with diabetes mellitus presented with fever, right lower quadrant abdominal pain and night sweats for 1 week. He was admitted to our medical ward for work up and started on intravenous piperacillin and tazobactam. Blood results showed raised white cell count 10.9×109/L, alkaline phosphatase 190 IU/L, alanine transaminase 103/L and bilirubin 40 μmol/L. Bedside ultrasound of the abdomen on the same day showed a heterogeneous liver lesion suspected to be a liver abscess. There was also fatty liver but no biliary tract dilation. CT of the abdomen carried out the next day confirmed the diagnosis of a liver abscess of 6×7.3×5.7 cm in the posterior segment, so ultrasound-guided drainage was performed. C reactive protein and white cell count dropped. The patient was switched to intravenous amoxicillin and clavulanate, after 3 days of piperacillin and tazobactam, as the blood culture results came back positive for K. pneumoniae sensitive to amoxicillin and clavulanate. However, on the same day, the patient began to have intermittent fever again and presented with a left eye visual disturbance, which he described as a veil over his eye with a mild foreign body sensation. There was no subjective drop in visual acuity.
On examination with a hand-held Snellen chart, both eyes had a visual acuity of 6/6. There was mild injection of the left eye and the pupil took longer to dilate compared with the right eye. With a portable slit lamp, anterior chamber cells could not be seen and there was no hypopyon. On fundus examination of the left eye, there was a three-disc diameter subretinal whitish mass with clear margin, overlying retinal haemorrhage and surrounding ghost vessels at the 9 o'clock region, not involving the macula. The vitreous was clear and the right eye was unremarkable. In view of good visual acuity and no vitritis, vitreous tap was not performed (figure 1).
Figure 1.
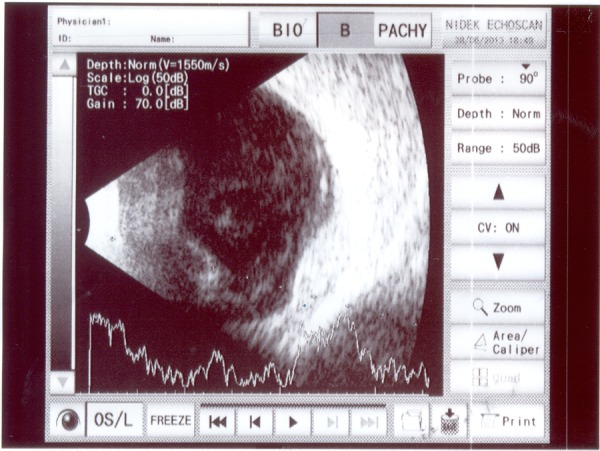
B-scan of the subretinal mass on day 2. Retina was flat and vitritis was not dense. Day 1 fundus photos are not available as the patient was bedbound.
Treatment
On the next day the patient's left eye vision had dropped to 6/120 with significant vitritis noticed. Vitreous tap and intravitreal amikacin 0.4 mg and ceftazidime 2 mg were injected in view of his Klebsiella infection. His general condition was suboptimal as well, with increased collection at the paracolic gutter and right-sided basal pleural effusion, requiring 4 L O2/min. He was switched to intravenous ceftriazone with oral ciprofloxacin in view of his eye condition. The vitreous (0.1 mL aspirated) culture was negative for bacteria and fungus.
The patient's visual acuity dropped to hand movement with increasing vitritis 5 days after the intravitreal antibiotics, so pars plana vitrectomy, retinotomy of the abscess for biopsy with silicone oil tamponade and endolaser was carried out. Intravitreal vancomycin 1 mg and ceftazidime 2 mg was given (figure 2). Intraoperatively, a chalky white powder-like substance was drained from the mass (figure 3), which confirmed that the mass was subretinal and not in the choroid. There was, however, insufficient tissue for histology and the vitreous tap yielded a negative culture once again. Owing to his septic condition, the patient could not lie prone and subretinal fluid extended inferiorly from the retinotimised abscess. On postoperative day 4 he was finally well enough for posturing and the retina was reattached.
Figure 2.
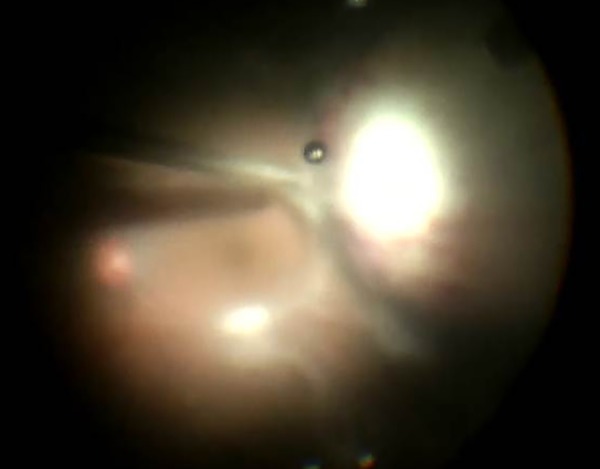
Intraoperative view of the whitish subretinal mass with overlying dilated retinal vessels. Macula was spared.
Figure 3.
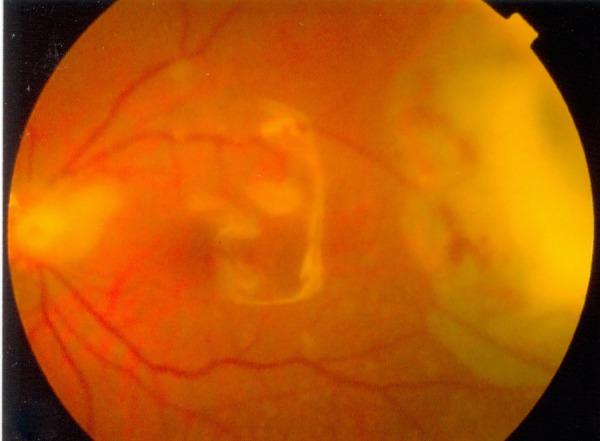
Fundus photo at 10 days after first pars plana vitrectomy. Retina was flat with silicone oil. The subretinal abscess remained.
Outcome and follow-up
The patient's visual acuity gradually improved to 6/24 at 3 months. The subretinal abscess and vitritis resolved gradually, leaving an atrophic area of the chorioretina (figure 4). However, inferior retinal detachment was noted and the patient was reoperated with encircling band, pars plana vitrectomy, retinotomy, endolaser, cryotherapy, silicone oil tamponade as well as phacoemulsification and intraocular lens insertion. The retina reattached successfully with a visual acuity of 6/60 at 3 months after the second surgery.
Figure 4.
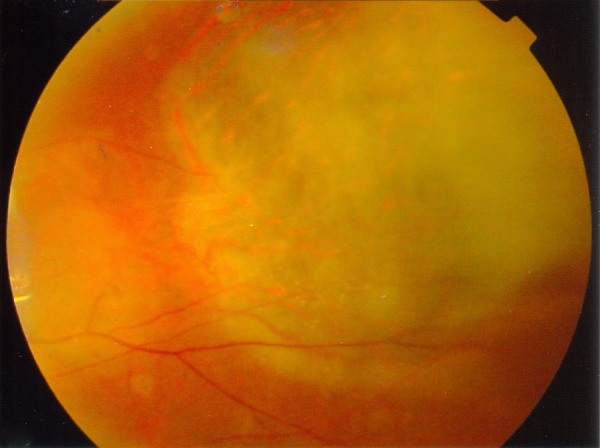
Fundus photo at 2 months after endophthalmitis. Area of chorioretinal atrophy seen where the subretinal abscess had been.
Discussion
Endogenous endophthalmitis usually presents late with poor visual acuity and prognosis. Bacterial endogenous endophthalmitis presenting with a visual acuity of 6/6 has not been reported so far.9–18
Since most endophthalmitis cases present late, there may already be florid signs of corneal oedema, conjunctival chemosis, hypopyon, fibrin and anterior chamber cells. The fundal view is often obscured in these cases and ultrasound B-scan is needed to assess the posterior pole. It is not surprising to see dense vitreous echogenicity and multiple loculations in the B-scan. One would not anticipate a subretinal abscess with vitritis at the early stage of the disease, as the infection usually spreads haematogeously to the choroid first. Looking back at the progress of our case, the sole presentation with a subretinal abscess is rare but may be a mid-stage sign before full blown endophthalmitis with vitritis. Our case illustrates the fast progression of the endophthalmitis from a simple subretinal mass on presentation to severe vitritis within 24 h. This subretinal abscess stage may therefore be often missed, especially when the subretinal abscess spares the macula and vision is maintained, as in our patient. Examination was made difficult as our patient was too ill and bedbound. In retrospect, low-grade vitritis might have already been present on the first day, given the patient's symptom of feeling a veil over his eye, and a pupil that was slow to dilate, which might have prompted our ophthalmologist for treatment on day 1. Therefore, physicians or ophthalmologists should maintain a high level of suspicion of endophthalmitis in patients with poorly controlled sepsis, subjective visual blurring, ocular signs such as conjunctival injection, sluggish pupil dilation and anterior chamber or anterior vitreous inflammation.
Subretinal abscess is difficult to manage. Since these patients may already be on systemic antibiotics and, in addition, the bacterial load may still be contained in the subretinal abscess, a negative vitreous tap is not surprising9 12–14 16–18 and should not be the reason to delay treatment. In other words, penetration of intravitreal antibiotics to the subretinal layer may also be limited as most systemic antibiotics do not cross the blood-retinal barrier. As a result, most reported subretinal abscess cases eventually required surgical intervention due to poorly controlled ocular infection.9–12 14–16 Yet, the risk of retinal detachment after drainage of a subretinal abscess is high,9 14 15 18 especially when the effect of silicone oil tamponade is reduced while the abscess resolves and the vitreous cavity volume expands. The dose of intravitreal antibiotics may also have to be adjusted postoperatively. The ESCRS guidelines suggested reducing the dose of intravitreal antibiotics up to 50% for a vitrectomised eye.7 19 For eyes with silicone oil or gas, a reduction of 1/4–1/10 of the standard dose may be considered.7 19
As illustrated by this case, despite good vision and the concern about antibiotics toxicity, the fast progression of endophthalmitis calls for early intervention. Early pars plana vitrectomy and drainage should be considered. Abscess fluid can be sent for culture as well as pathology, which may aid the diagnosis.16 Posturing with tamponade agent immediately postoperatively is essential if the patient is physically fit. In our literature review, after the initial operation, none of the cases required further intravitreal antibiotics, so the postulated dosage issue after injection of tamponade agent may not be as intimidating. Instead, if intravitreal antibiotics is to be administered intraoperatively, standard concentration should be used prior to air-fluid exchange and subsequent oil or gas tamponade. In view of the high risk of retinal detachment, the use of encircling band or scleral buckle can be considered to aid the reattachment of the necrotic retina.
Learning points.
Normal visual acuity does not exclude endogenous endophthalmitis.
Vitreous tap culture result may be negative as the bacterial load may not be in the vitreous.
Retinal detachment is a common complication after drainage of a subretinal abscess.
Acknowledgments
The authors would like to acknowledge Dr Vesta Chan who was involved in the management of this patient.
Footnotes
Contributors: GDJ-YS is the first author of the manuscript and was also involved in the treatment of the patient. EC-FL and AY both helped in editing the manuscript. EC-FL was also involved in the treatment of the patient.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Jackson TL, Eykyn SJ, Graham EM et al. Endogenous bacterial endophthalmitis: a 17-year prospective series and review of 267 reported cases. Surv Ophthalmol 2003;48:403–23. 10.1016/S0039-6257(03)00054-7 [DOI] [PubMed] [Google Scholar]
- 2.Kashani AH, Eliott D. The emergence of Klebsiella pneumoniae endogenous endophthalmitis in the USA: basic and clinical advances. J Ophthal Inflamm Infect 2013;3:28 10.1186/1869-5760-3-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Okada AA, Johnson RP, Liles WC et al. Endogenous bacterial endophthalmitis. Report of a ten-year retrospective study. Ophthalmology 1994;101:832–8. 10.1016/S0161-6420(13)31255-X [DOI] [PubMed] [Google Scholar]
- 4.Connell PP, O'Neill EC, Fabinyi D et al. Endogenous endophthalmitis: 10-year experience at a tertiary referral centre. Eye 2011;25:66–72. 10.1038/eye.2010.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee S, Um T, Joe SG et al. Changes in the clinical features and prognostic factors of endogenous endophthalmitis: fifteen years of clinical experience in Korea. Retina 2012;32:977–84. 10.1097/IAE.0b013e318228e312 [DOI] [PubMed] [Google Scholar]
- 6.Endophthalmitis Vitrectomy Study Group. Results of the Endophthalmitis Vitrectomy Study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol 1995;113:1479–96. 10.1001/archopht.1995.01100120009001 [DOI] [PubMed] [Google Scholar]
- 7.Barry P, Cordovés L, Gardner S. ESCRS Guidelines for prevention and treatment of endopthalmitis following cataract surgery: Data, dilemmas and conclusions. http://www.escrs.org/endophthalmitis/default.asp (access date 19 May 2014).
- 8.Kernt M, Kampik A. Endophthalmitis: pathogenesis, clinical presentation, management, and perspectives. Clin Ophthalmol 2010;4:121–35. 10.2147/OPTH.S6461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harris EW, D'Amico DJ, Bhisitkul R et al. Bacterial subretinal abscess: a case report and review of the literature. Am J Ophthalmol 2000;129:778–85. 10.1016/S0002-9394(00)00355-X [DOI] [PubMed] [Google Scholar]
- 10.Yarng SS, Hsieh CL, Chen TL. Vitrectomy for endogenous Klebsiella pneumoniae endophthalmitis with massive subretinal abscess. Ophthalmic Surg Lasers 1997;28:147–50. [PubMed] [Google Scholar]
- 11.Dodds EM, Echandi LV, Puente SI et al. Subretinal abscess due to Nocardia farcinica resistant to trimethoprim- sulfamethoxazole in a patient with systemic lupus erythematosus. Ocul Immunol Inflamm 2006;14:249–51. 10.1080/09273940600760514 [DOI] [PubMed] [Google Scholar]
- 12.Halperin LS, Roseman RL. Successful treatment of a subretinal abscess in an intravenous drug abuser. Arch Ophthalmol 1988;106:1651–2. 10.1001/archopht.1988.01060140823011 [DOI] [PubMed] [Google Scholar]
- 13.Jones NP. Disseminated Nocardia infection with subretinal abscess. Eye 2010;24:187–8. 10.1038/eye.2009.69 [DOI] [PubMed] [Google Scholar]
- 14.Kaburaki T, Takamoto M, Araki F et al. Endogenous Candida albicans infection causing subretinal abscess. Int Ophthalmol 2010;30:203–6. 10.1007/s10792-009-9304-0 [DOI] [PubMed] [Google Scholar]
- 15.Ng EW, Zimmer-Galler IE, Green WR. Endogenous Nocardia asteroides endophthalmitis. Arch Ophthalmol 2002;120:210–13. [PubMed] [Google Scholar]
- 16.Rimpel NR, Cunningham ET, Howes EL et al. Viridans group Streptococcus subretinal abscess. Br J Ophthalmol 1999;83:373 10.1136/bjo.83.3.373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trigui A, Laabidi H, Khairallah M et al. Retinal abscess: case report of an uncommon evolution. Int Ophthalmol 2011;31:327–31. 10.1007/s10792-011-9454-8 [DOI] [PubMed] [Google Scholar]
- 18.Webber SK, Andrews RA, Gillie RF et al. Subretinal Pseudomonas abscess after lung transplantation. Br J Ophthalmol 1995;79:861–6. 10.1136/bjo.79.9.861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Foster RE, Rubsamen PE, Joondeph BC et al. Concurrent endophthalmitis and retinal detachment. Ophthalmology 1994;101:490–8. 10.1016/S0161-6420(94)31308-X [DOI] [PubMed] [Google Scholar]


