Abstract
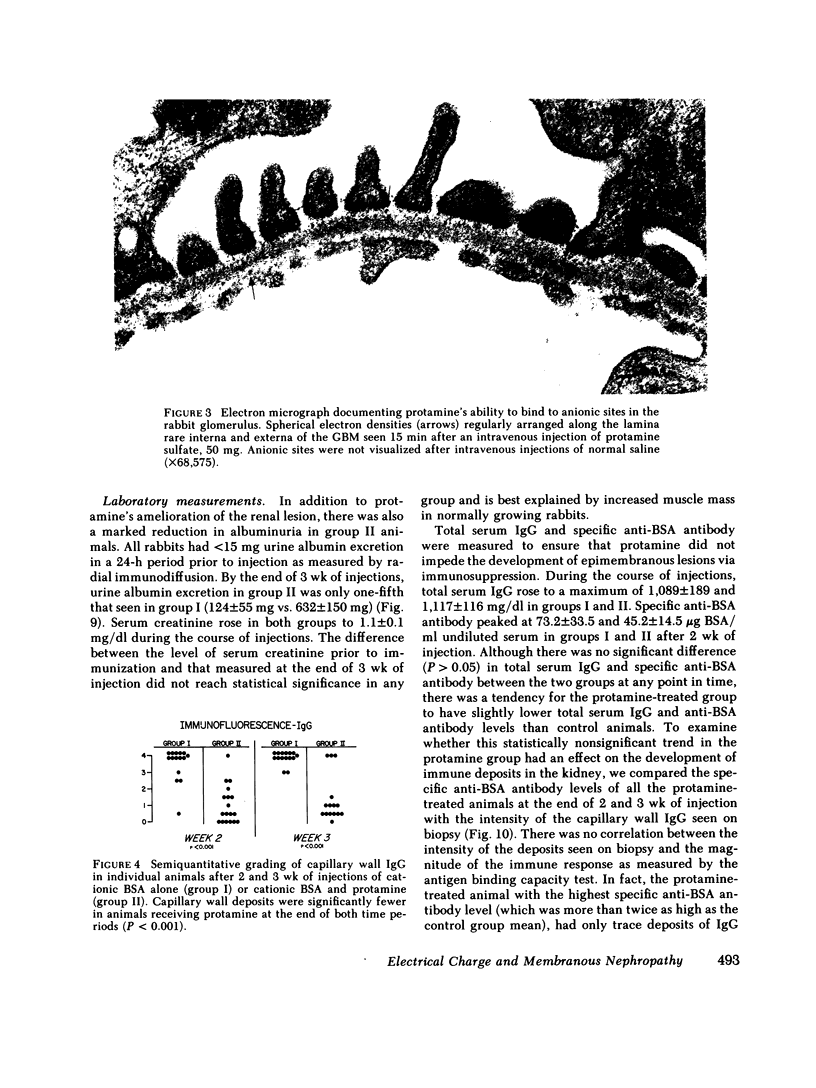
Intravenous cationic bovine serum albumin (BSA, pI > 9.5) induces membranous nephropathy in immunized rabbits. In this study, unimmunized rabbits received intravenous injections of cationic (n = 3) or native (n = 3) or native (n = 3) BSA, followed by ex vivo isolated left renal perfusions with sheep anti-BSA antibody. Capillary wall deposits of IgG and C3 were seen exclusively in the group receiving cationic BSA, confirming an in situ pathogenesis for cationic, BSA-induced membranous nephropathy, and demonstrating the importance of a cationic antigen for its production. We then explored whether membranous nephropathy in this model is prevented by the concomitant injection of protamine sulfate, a filterable, relatively non-immunogenic polycation. An in vitro study demonstrated that protamine sulfate incubated with glomerular basement membrane (GBM) decreased the subsequent binding of radiolabeled cationic BSA (P < 0.05). In vivo, protamine sulfate was shown to bind to anionic sites in the glomerular capillary wall after intravenous injection.
Groups of rabbits received 3 wk of daily intravenous injections of cationic BSA alone (n = 15) or cationic BSA and protamine (n = 18). After 2 wk of injection of cationic BSA alone, typical membranous nephropathy developed. Granular deposits of IgG and C3 were present along the GBM associated with subepithelial dense deposits, foot process effacement, and marked albuminuria. Protamine significantly reduced or prevented the formation of deposits (P < 0.001) and in6 of 18 protamine-treated animals, existing deposits decreased or disappeared between 2 and 3 wk of injection. Albuminuria was significantly reduced in protamine-treated animals with a mean of 124±55 mg/24 h compared to 632±150 mg/24 h in the control group receiving cationic BSA alone. No significant differences between the groups were noted in serum lev9lsof IgG, C3, anti-BSA antibody, or circulating immune complex size. Studies in additional animals (n = 5) given radiolabeled cationic BSA showed that protamine did not alter the clearance of cationic BSA from serum.
Control experiments showed that protamine's beneficial effects were not related to its weak anticoagulant property or toits theoretical ability to deplete tissue histamine. The administration of heparin (n = 6) or diphenhydramine (n = 6) had no effect on the development of the epimembranous lesion compared to the group receiving cationic BSA alone. In addition, homogenized whole kidney histamine content was not significantly different in the group receiving cationic BSA alone compared to the group receiving cationic BSA and protamine.
This work shows that a cationic BSA-induced glomerular lesion can be produced by a renal perfusion technique involving in situ complex formation and that this process requires a cationic antigen for its development. We believe that the demonstrated beneficial effects of protamine are due to its ability to bind to glomerular anionic sites, and that this electrostatic interaction results in inhibition for the further binding of the cationic antigen, thereby limiting the severity of glomerulonephritis in this model.
Full text
PDF











Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Batsford S. R., Takamiya M., Vogt A. A model of in situ immune complex glomerulonephritis in the rat employing cationized ferritin. Clin Nephrol. 1980 Nov;14(5):211–216. [PubMed] [Google Scholar]
- Border W. A., Ward H. J., Kamil E. S., Cohen A. H. Induction of membranous nephropathy in rabbits by administration of an exogenous cationic antigen. J Clin Invest. 1982 Feb;69(2):451–461. doi: 10.1172/JCI110469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Border W. A., Wilson C. B., Dixon F. J. Failure of heparin to affect two types of experimental glomerulonephritis in rabbits. Kidney Int. 1975 Sep;8(3):140–148. doi: 10.1038/ki.1975.93. [DOI] [PubMed] [Google Scholar]
- Caulfield J. P., Farquhar M. G. Distribution of annionic sites in glomerular basement membranes: their possible role in filtration and attachment. Proc Natl Acad Sci U S A. 1976 May;73(5):1646–1650. doi: 10.1073/pnas.73.5.1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochrane C. G., Hawkins D. Studies on circulating immune complexes. 3. Factors governing the ability of circulating complexes to localize in blood vessels. J Exp Med. 1968 Jan 1;127(1):137–154. doi: 10.1084/jem.127.1.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couser W. G., Salant D. J. In situ immune complex formation and glomerular injury. Kidney Int. 1980 Jan;17(1):1–13. doi: 10.1038/ki.1980.1. [DOI] [PubMed] [Google Scholar]
- Couser W. G., Steinmuller D. R., Stilmant M. M., Salant D. J., Lowenstein L. M. Experimental glomerulonephritis in the isolated perfused rat kidney. J Clin Invest. 1978 Dec;62(6):1275–1287. doi: 10.1172/JCI109248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DIXON F. J., FELDMAN J. D., VAZQUEZ J. J. Experimental glomerulonephritis. The pathogenesis of a laboratory model resembling the spectrum of human glomerulonephritis. J Exp Med. 1961 May 1;113:899–920. doi: 10.1084/jem.113.5.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EGERTON W. S., ROBINSON C. L. The anti-heparin, anticoagulant and hypotensive properties of hexadimethrine and protamine. Lancet. 1961 Sep 16;2(7203):635–637. doi: 10.1016/s0140-6736(61)90311-7. [DOI] [PubMed] [Google Scholar]
- Fleuren G., Grond J., Hoedemaeker P. J. In situ formation of subepithelial glomerular immune complexes in passive serum sickness. Kidney Int. 1980 May;17(5):631–637. doi: 10.1038/ki.1980.74. [DOI] [PubMed] [Google Scholar]
- Ford P. M. The effect of manipulation of reticuloendothelial system activity on glomerular deposition of aggregated protein and immune complexes in two different strains of mice. Br J Exp Pathol. 1975 Dec;56(6):523–529. [PMC free article] [PubMed] [Google Scholar]
- Germuth F. G., Jr, Rodriguez E., Lorelle C. A., Trump E. I., Milano L. L., Wise O. Passive immune complex glomerulonephritis in mice: models for various lesions found in human disease. II. Low avidity complexes and diffuse proliferative glomerulonephritis with subepithelial deposits. Lab Invest. 1979 Oct;41(4):366–371. [PubMed] [Google Scholar]
- Germuth F. G., Jr, Senterfit L. B., Pollack A. D. Immune complex disease. I. Experimental acute and chronic glomerulonephritis. Johns Hopkins Med J. 1967 Apr;120(4):225–251. [PubMed] [Google Scholar]
- Golbus S. M., Wilson C. B. Experimental glomerulonephritis induced by in situ formation of immune complexes in glomerular capillary wall. Kidney Int. 1979 Aug;16(2):148–157. doi: 10.1038/ki.1979.116. [DOI] [PubMed] [Google Scholar]
- Hebert L. A., Allhiser C. L., Koethe S. M. Some hemodynamic determinants of immune complex trapping by the kidney. Kidney Int. 1978 Nov;14(5):452–465. doi: 10.1038/ki.1978.150. [DOI] [PubMed] [Google Scholar]
- Hoffsten P. E., Swerdlin A., Bartell M., Hill C. L., Venverloh J., Brotherson K., Klahr S. Reticuloendothelial and mesangial function in murine immune complex glomerulonephritis. Kidney Int. 1979 Feb;15(2):144–159. doi: 10.1038/ki.1979.20. [DOI] [PubMed] [Google Scholar]
- Hoyer J. R., Mauer S. M., Michael A. F. Unilateral renal disease in the rat. I. Clinical, morphologic, and glomerular mesangial functional features of the experimental model produced by renal perfusion with aminonucleoside. J Lab Clin Med. 1975 May;85(5):756–768. [PubMed] [Google Scholar]
- Kanwar Y. S., Farquhar M. G. Anionic sites in the glomerular basement membrane. In vivo and in vitro localization to the laminae rarae by cationic probes. J Cell Biol. 1979 Apr;81(1):137–153. doi: 10.1083/jcb.81.1.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley V. E., Cavallo T. Glomerular permeability: transfer of native ferritin in glomeruli with decreased anionic sites. Lab Invest. 1978 Dec;39(6):547–553. [PubMed] [Google Scholar]
- Kniker W. T., Cochrane C. G. The localization of circulating immune complexes in experimental serum sickness. The role of vasoactive amines and hydrodynamic forces. J Exp Med. 1968 Jan 1;127(1):119–136. doi: 10.1084/jem.127.1.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kniker W. T., Cochrane C. G. The localization of circulating immune complexes in experimental serum sickness. The role of vasoactive amines and hydrodynamic forces. J Exp Med. 1968 Jan 1;127(1):119–136. doi: 10.1084/jem.127.1.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maack T. Physiological evaluation of the isolated perfused rat kidney. Am J Physiol. 1980 Feb;238(2):F71–F78. doi: 10.1152/ajprenal.1980.238.2.F71. [DOI] [PubMed] [Google Scholar]
- Mancini G., Carbonara A. O., Heremans J. F. Immunochemical quantitation of antigens by single radial immunodiffusion. Immunochemistry. 1965 Sep;2(3):235–254. doi: 10.1016/0019-2791(65)90004-2. [DOI] [PubMed] [Google Scholar]
- Mohos S. C., Skoza L. Variations in the sialic acid concentration of glomerular basement membrane preparations obtained by ultrasonic treatment. J Cell Biol. 1970 May;45(2):450–455. doi: 10.1083/jcb.45.2.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SHORE P. A., BURKHALTER A., COHN V. H., Jr A method for the fluorometric assay of histamine in tissues. J Pharmacol Exp Ther. 1959 Nov;127:182–186. [PubMed] [Google Scholar]
- Schurer J. W., Kalicharan D., Hoedemaeker P. J., Molenaar I. The use of polyethyleneimine for demonstration of anionic sites in basement membranes and collagen fibrils. J Histochem Cytochem. 1978 Aug;26(8):688–689. doi: 10.1177/26.8.690407. [DOI] [PubMed] [Google Scholar]
- Seiler M. W., Rennke H. G., Venkatachalam M. A., Cotran R. S. Pathogenesis of polycation-induced alterations ("fusion") of glomerular epithelium. Lab Invest. 1977 Jan;36(1):48–61. [PubMed] [Google Scholar]
- Seiler M. W., Venkatachalam M. A., Cotran R. S. Glomerular epithelium: structural alterations induced by polycations. Science. 1975 Aug 1;189(4200):390–393. doi: 10.1126/science.1145209. [DOI] [PubMed] [Google Scholar]
- Sharon Z., Schwartz M. M., Pauli B. U., Lewis E. J. Kinetics of glomerular visceral epithelial cell phagocytosis. Kidney Int. 1978 Nov;14(5):526–529. doi: 10.1038/ki.1978.158. [DOI] [PubMed] [Google Scholar]
- Spiro R. G. Studies on the renal glomerular basement membrane. Preparation and chemical composition. J Biol Chem. 1967 Apr 25;242(8):1915–1922. [PubMed] [Google Scholar]
- Van Damme B. J., Fleuren G. J., Bakker W. W., Vernier R. L., Hoedemaeker P. J. Experimental glomerulonephritis in the rat induced by antibodies directed against tubular antigens. V. Fixed glomerular antigens in the pathogenesis of heterologous immune complex glomerulonephritis. Lab Invest. 1978 Apr;38(4):502–510. [PubMed] [Google Scholar]
- Wilson C. B., Dixon F. J. Quantitation of acute and chronic serum sickness in the rabbit. J Exp Med. 1971 Sep 1;134(3 Pt 2):7s–8s. [PubMed] [Google Scholar]













