Abstract
Undescended parathyroid adenomas are rare, representing 0.08% of all parathyroid adenomas; however, they make up 7% of the underlying cause of failed cervical exploration in patients with persistent primary hyperparathyroidism. A 43-year-old woman with no significant medical or family history presented with fatigue and was diagnosed with primary hyperparathyroidism; however, preoperative imaging including sestamibi scan and ultrasound was unable to identify the hyperfunctioning gland. She underwent a neck exploration and hemithyroidectomy and partial parathyroidectomy with failure of resolution of her disease. Subsequent work up including a CT of the neck demonstrated a 1.9 cm mass adjacent to the left submandibular gland. This was removed with postoperative normalisation of the patient's serum calcium and parathyroid hormone levels.
Background
Ectopic parathyroid adenomas are not unusual, occurring in approximately 16% of initial operations for primary hyperparathyroidism.1 Embryology provides an explanation for the common locations of ectopic parathyroid glands. The third brachial pouch descends to form the inferior parathyroids and the thymus, and the superior parathyroids develop from the fourth pouch. Descent of the inferior parathyroids beyond the level of the inferior pole of the thyroid gland accounts for ectopic glands found near the thymus and in the mediastinum; by the same mechanism, undescended parathyroid glands are thought to result from arrested descent of the third brachial pouch.2 The most common location for ectopic parathyroid adenomas is the thymus, followed by retro-oesophageal, intrathyroidal, mediastinal and carotid sheath; undescended adenomas, described by Fraker et al3 as those located at or above the carotid bifurcation, are the least common, representing 2–7% of parathyroid adenomas found in ectopic locations.1 4 The most common cause of persistent primary hyperparathyroidism following neck exploration is a missed adenoma, most commonly located in the tracheal oesophageal groove.5 Despite their rarity, making up only 0.08% of all parathyroid adenomas, undescended adenomas make up 7% of the underlying cause for failed cervical exploration in patients with primary hyperparathyroidism.6
Case presentation
A 43-year-old woman initially presented to an outside facility for evaluation of myalgias and fatigue. She was otherwise healthy with no significant medical history or family history, including any findings concerning Multiple Endocrine Neoplasia. Her workup was significant for primary hyperparathyroidism, with serum calcium of 11.6 (normal range 8.5–10.2 mg/dL) and parathyroid hormone (PTH) of 213 (normal 10–55 pg/mL). As part of her preoperative workup she underwent a sestamibi scan as well as an ultrasound of the neck, neither of which were able to localise the hyperfunctioning gland. She underwent a neck exploration at an outside facility, where a right intrathyroidal gland and two left parathyroid glands were identified; a right hemithyroidectomy for removal of one and a half of the left parathyroids was performed. Pathological evaluation of this specimen revealed two and a half normal parathyroid glands and a 3 mm papillary microcarcinoma (follicular variant) in the thyroid gland. The patient continued to be symptomatic with elevated PTH and calcium levels consistent with persistent primary hyperparathyroidism, and she was referred to this institution for further evaluation and management.
Investigations
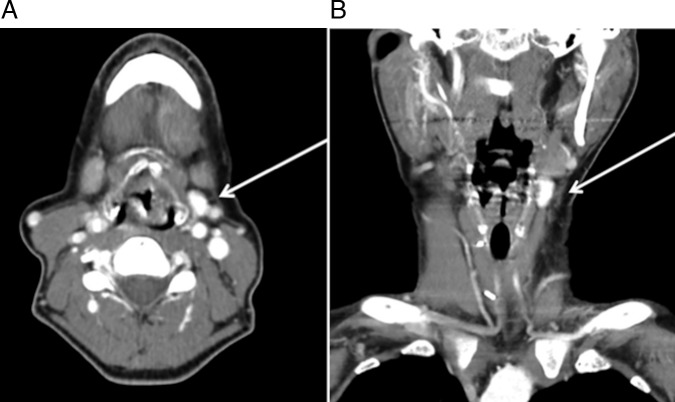
Repeat sestamibi scan was again negative for a hyperfunctioning gland, and the patient's laboratory workup demonstrated serum calcium of 11.6 and PTH of 261. On physical examination she had a well-healed scar at the site of her prior surgery and no masses were noted. In an attempt to identify the location of the adenoma, a CT scan of the neck was obtained, which demonstrated a 1.9 cm enhancing nodule in the left neck posterior to the submandibular gland (figure 1).
Figure 1.
CT of the neck with contrast obtained after first neck exploration, on which a 1.9 cm hyperintensity was noted near the left submandibular gland (arrow), (A) transverse and (B) coronal.
Treatment
Excision of the lesion found on the CT scan was planned, and intraoperative ultrasound was initially used to identify the area with the nodule and to plan the incision. Dissection along the site identified revealed a 2 cm lesion appearing consistent with a parathyroid adenoma located immediately deep to the platysma, approximately at the level of the carotid bifurcation (figure 2A–C). Pre-incision PTH was measured at 365, 10 min following excision at 150, and on discharge the following day the patient's PTH was 9, with serum calcium of 8.1. She was discharged on calcitriol and calcium carbonate supplementation.
Figure 2.
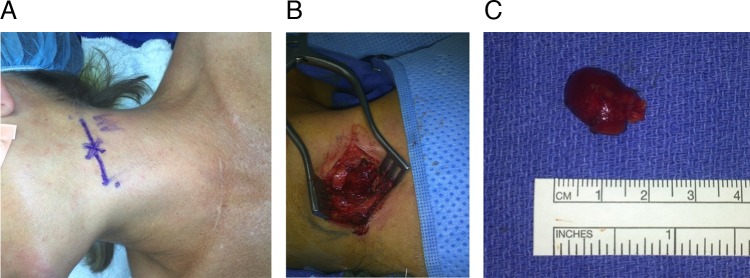
(A) Planned incision following localisation of mass with ultrasound. (B) Dissection demonstrating 2 cm mass immediately deep to the platysma (patient's head is to the left in the image). (C) Specimen following removal, 1.9×1.2×1.0 cm and weighing 1.01 g; pathology was consistent with a hypercellular parathyroid adenoma.
Outcome and follow-up
On postoperative day 3, the patient presented to the emergency department with symptoms of hypocalcaemia including malaise and paresthesias of the feet and hands; her PTH was 8, serum calcium 8.0 and serum magnesium level 2.0. On physical examination, Chvostek's and Trousseau's signs were negative, and the patient's calcitriol and calcium supplementation doses were increased with resolution of her symptoms. Her postoperative course was otherwise uneventful, and she has remained without evidence of hyperparathyroidism, with serum PTH of 12 and calcium 8.5 at 1-month postoperative follow-up.
Discussion
Other reports of undescended adenomas include intraneural adenomas as well as adenomas located in other high pharyngeal spaces. In a case series of eight patients, Chan et al7 describe four adenomas located within the vagus nerve near the carotid bifurcation and the rest located at various locations in the pharynx, including the posterior pharyngeal wall and pterygopalatine fossa. Nguyen et al8 describe a parathyroid adenoma located within the hypoglossal nerve and found with selective venous sampling, and Pawlik et al9 describe two cases of adenomas found within the vagus nerve. While intraneural adenomas are often located in a similar region as undescended parathyroid adenomas, embryological aetiology of the two is thought to differ. As originally illustrated by Gilmour,10 the third branchial pouch contacts the ectodermal structures from which the vagus and hypoglossal nerves arise, and thus may give rise to additional parathyroid glands embedded in these nerves. It should also be noted that in the majority of these cases, as with the one presented in this report, patients had typically undergone one, if not several, previous neck explorations before the adenoma was identified and removed.
Several authors have developed solutions to address non-diagnostic imaging and failed initial neck exploration. Although invasive, selective venous sampling of the internal jugular vein has been used to successfully localise undescended adenomas both preoperatively and intraoperatively in the case of negative imaging.3 11 Other options include angiography, with a blush demonstrating the hypervascular adenoma.12 However, non-invasive studies should always be considered first, as CT and ultrasound can locate potentially 50% of undescended adenomas provided that imaging extends to the level of the mandible.3 Fine-needle aspiration may be performed on lesions located with ultrasound or other non-invasive means with PTH levels of the aspirate measured to confirm the diagnosis of an undescended adenoma.12 In addition, several studies have examined ways to utilise current parathyroid imaging techniques to improve preoperative adenoma localisation, especially in cases of ectopic or ‘hidden’ adenomas. In a study involving re-examining preoperative sestamibi scans following removal of an undescended parathyroid adenoma, Axelrod et al13 noted asymmetry between the submandibular glands corresponding to the side and location of the adenoma; all scans had been read as non-diagnostic preoperatively. Nagar et al14 compared thyroid lobe length between ultrasound and sestamibi scans in patients with sestamibi scan initially read as non-diagnostic but with successful removal of an adenoma on neck exploration; they found that a discordance in thyroid lobe length between the nuclear medicine scan and ultrasound predicted a ‘hidden’ adenoma on the side with a longer lobe seen on sestamibi, with sensitivity of 93.8% and specificity of 85.2%. In this case, no special studies beyond CT scan and ultrasound were used to identify the adenoma, and the finding of discordance in a submandibular location is consistent with other literature describing imaging findings suggestive of undescended adenomas.
Another interesting feature of this case is the incidental finding of papillary microcarcinoma in the initial hemithyroidectomy specimen. The coexistence of non-medullary thyroid cancer and primary hyperparathyroidism has been approximated at 2.4–3.7% in patients undergoing parathyroidectomy.15 Ryan et al16 examined the incidence of coincident thyroid pathology with parathyroid adenoma in a study of 135 patients undergoing parathyroidectomy; 29% had resection of thyroid along with parathyroid tissue, with co-incidental malignant disease noted in 5 (14%) of those patients; however, only 1 of the 5 patients had suspected thyroid malignancy prior to the operation.
Our patient also experienced symptomatic hypocalcaemia following removal of the adenoma, likely attributable to the initial removal of 2.5 normal parathyroid glands as well as suppression of her remaining gland function by the adenoma. One study examining predictors of postoperative hypocalcaemia found that PTH levels less than 15 pg/mL at 8 h postoperatively had a high risk of developing hypocalcaemia with 75% of patients with PTH <15 developing symptoms; preoperative 1,25-dihydroxy vitamin D levels were not predictive.17 This patient's postoperative PTH of 9 and thus increased risk for hypocalcaemia is consistent with these findings.
Learning points.
Undescended parathyroid adenomas remain an important consideration in patients with persistent primary hyperparathyroidism following neck exploration as well as those with initial ‘non-diagnostic’ imaging.
In these cases, invasive and non-invasive techniques are available to localise the hyperfunctioning gland.
Careful examination of imaging studies with particular attention paid to the submandibular region may offer clues for preoperative planning, thus minimising the use of invasive diagnostic techniques and allowing for simplification and avoidance of extensive dissection in the previous operative field in the case of re-operation.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Phitayakorn R, McHenry CR. Incidence and location of ectopic abnormal parathyroid glands. Am J Surg 2006;191:418–23. 10.1016/j.amjsurg.2005.10.049 [DOI] [PubMed] [Google Scholar]
- 2.Edis AJ, Purnell DC, van Heerden JA. The undescended “parathymus”. An occasional cause of failed neck exploration for hyperparathyroidism. Ann Surg 1979;190:64–8. 10.1097/00000658-197907000-00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fraker DL, Doppman JL, Shawker TH et al. Undescended parathyroid adenoma: an important etiology for failed operations for primary hyperparathyroidism. World J Surg 1990;14:342–8. 10.1007/BF01658522 [DOI] [PubMed] [Google Scholar]
- 4.Lee JC, Mazeh H, Serpell J et al. Adenomas of cervical maldescended parathyroid glands: pearls and pitfalls. ANZ J Surg . Published Online First: 10 Dec 2012. doi:10.1111/ans.12017. [DOI] [PubMed] [Google Scholar]
- 5.Fraker DL. Update on the management of parathyroid tumors. Curr Opin Oncol 2000;12:41–8. 10.1097/00001622-200001000-00007 [DOI] [PubMed] [Google Scholar]
- 6.Billingsley KG, Fraker DL, Doppman JL et al. Localization and operative management of undescended parathyroid adenomas in patients with persistent primary hyperparathyroidism. Surgery 1994;116:982–9; discussion 989–90. [PubMed] [Google Scholar]
- 7.Chan TJ, Libutti SK, McCart JA et al. Persistent primary hyperparathyroidism caused by adenomas identified in pharyngeal or adjacent structures. World J Surg 2003;27:675–9. 10.1007/s00268-003-6812-3 [DOI] [PubMed] [Google Scholar]
- 8.Nguyen J, Abemayor E, Yeh MW. Undescended parathyroid adenoma arising within the hypoglossal nerve. Arch Otolaryngol Head Neck Surg 2011;137:709–11. 10.1001/archoto.2011.90 [DOI] [PubMed] [Google Scholar]
- 9.Pawlik TM, Richards M, Giordano TJ et al. Identification and management of intravagal parathyroid adenoma. World J Surg 2001;25:419–23. 10.1007/s002680020067 [DOI] [PubMed] [Google Scholar]
- 10.Gilmour J. The embryology of the parathyroid glands, the thymus and certain associated rudiments. J Pathol Bacteriol 1937;45:507–22. 10.1002/path.1700450304 [DOI] [Google Scholar]
- 11.Lee LS, Canter RJ, Fraker DL. Intraoperative jugular venous sampling aids detection of an undescended parathyroid adenoma. World J Surg 2006;30:620–3. 10.1007/s00268-005-0238-z [DOI] [PubMed] [Google Scholar]
- 12.Jaskowiak N, Norton JA, Alexander HR et al. A prospective trial evaluating a standard approach to reoperation for missed parathyroid adenoma. Ann Surg 1996;224:308–20; discussion 320–1 10.1097/00000658-199609000-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Axelrod D, Sisson JC, Cho K et al. Appearance of ectopic undescended inferior parathyroid adenomas on technetium Tc 99 m sestamibi scintigraphy: a lesson from reoperative parathyroidectomy. Arch Surg 2003;138:1214–18. 10.1001/archsurg.138.11.1214 [DOI] [PubMed] [Google Scholar]
- 14.Nagar S, Walker DD, Embia O et al. A novel technique to improve the diagnostic yield of negative sestamibi scans. Surgery 2014;156:584–90. 10.1016/j.surg.2014.05.020 [DOI] [PubMed] [Google Scholar]
- 15.Leitha T, Staudenherz A. Concomitant hyperparathyroidism and nonmedullary thyroid cancer, with a review of the literature. Clin Nucl Med 2003;28:113–17. [DOI] [PubMed] [Google Scholar]
- 16.Ryan S, Courtney D, Timon C. Co-existent thyroid disease in patients treated for primary hyperparathyroidism: implications for clinical management. Eur Arch Otorhinolaryngol 2014:1–5. [DOI] [PubMed] [Google Scholar]
- 17.Chia SH, Weisman RA, Tieu D et al. Prospective study of perioperative factors predicting hypocalcemia after thyroid and parathyroid surgery. Arch Otolaryngol Head Neck Surg 2006;132:41–5. 10.1001/archotol.132.1.41 [DOI] [PubMed] [Google Scholar]