Abstract
We present an impressive case of a pregnant woman presenting with severe right flank pains. A rare rupture of the right renal pelvis turned out to be the cause of her problems. Renal pelvis rupture in pregnancy is difficult to diagnose. It is easily confused with other more prevalent diagnoses, like hydronephrosis, ureteral distension, renal calculus and pyelonephritis. Ultrasonography is not always conclusive. Pyelography seems to be a good diagnostic tool, this case shows that MRI is another option. Renal pelvis rupture can be effectively treated with the insertion of a JJ-stent.
Background
While urinary tract complications like hydronephrosis are common or even physiological in pregnancy, they rarely progress to a rupture of the renal collecting system. It can be caused distinctively by pregnancy and can be hard to diagnose, because of its rarity and because it mimics other more prevalent diagnoses. Renal pelvis rupture can have negative outcomes in case the delay in the diagnostic process takes too much time. In addition, symptoms can be very severe, so delay can cause unnecessary despair to the patient.
We describe an impressive case of renal pelvis rupture and we will give an overview of previous reports on this subject.
Case presentation
A 27-year-old G2 P1 of Caucasian origin was admitted at 341/7 weeks gestation with frequent premature contractions and extreme right flank pain. Symptoms started that same day with colicky flank pain and shortly she developed contractions. In addition she was reporting of nausea and vomiting. She felt normal fetal movements and there was no history of vaginal blood loss or amniotic fluid loss. She also had no clear history of dysuria, frequency or haematuria, nor constipation.
Our patient was in stable hemodynamic status and she was looking despairingly painful. She did not have fever or chills. She was seated straight up in bed, but she did not present typical restlessness. There were no peritoneal signs and the womb relaxed normally in between contractions, but there was an extreme tenderness in the costovertebral angle on the right side. Vaginal examination showed a cervical dilation of 2 cm.
Investigations
Cardiotocography showed no apparent fetal distress.
Urinalysis showed no haematuria and no leucocyturia. Blood tests showed a white cell count of 15.800×106/L, a C reactive protein of 13 mg/L, kidney function showed no abnormalities. Ultrasonography revealed a slight bilateral dilation of the upper urinary tract fitting her pregnancy, it did not reveal any kidney or gallbladder stones. The appendix was not seen.
The next day C reactive protein increased to 44 mg/L and MRI revealed the source of despair: extravasation of urine around the right renal collecting system was seen, suggesting a rupture of the right renal pelvis. No other pathology was seen (figure 1).
Figure 1.
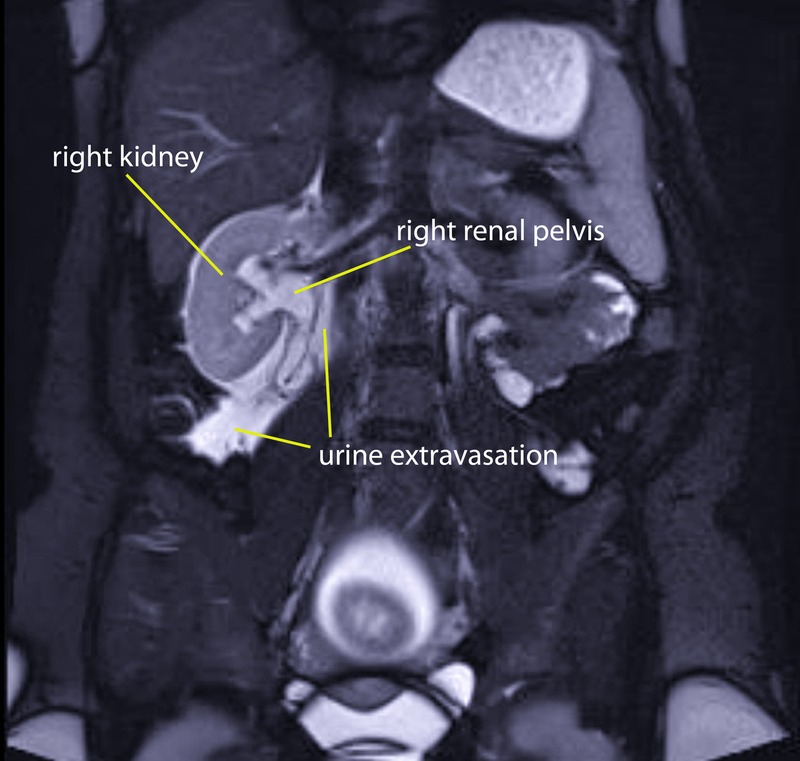
MRI showing right renal pelvis rupture.
Differential diagnosis
A pregnant woman with colicky pains was suspected to have a complication of urinary tract obstruction during pregnancy. Hydronephrosis, ureteral distension, renal calculus and pyelonephritis are the most likely, common diagnoses. The patient did not respond to the usual symptomatic treatment for colicky pains and urinalysis and ultrasonography did not show any signs of urological problems. Therefore the attention shifted to surgical problems like cholecystolithiasis, cholecystitis and appendicitis. Especially because infection parameters tended to increase, an inflammation became more likely.
Additional imaging was performed to prove this hypothesis, but instead it showed a rare right renal pelvis rupture and proved the first suspicion of a urinary tract complication during pregnancy. Since it is a rare thing, renal pelvis rupture was not explicitly in the differential diagnosis.
Treatment
At admission, before the MRI was performed, we started treating her symptoms. Intravenous butylscopolamine and paracetamol did not have satisfactory results, pethidine was able to decrease the pain for just a short term.
When the diagnosis was clear a JJ-stent was inserted. After the insertion, symptoms immediately decreased and by the next day our patient was free of symptoms, she was not depending on pain medication anymore. At 343/7 weeks gestation she was discharged from the hospital.
Outcome and follow-up
Labour was induced at 375/7 weeks gestation because of pre-eclampsia; that same day she delivered spontaneously of a healthy baby girl with a good start (Apgar of 9 over 10, umbilical artery pH of 7.28, a base excess of −4) and a birth weight of 2538 g (ref. 1, p.9). The JJ-stent was removed 8 weeks postpartum under antibiotic prophylaxis with nitrofurantoin. There were no residual symptoms after 6 months of follow-up.
Discussion
Urinary tract problems are common during pregnancy.2 The urinary tract is subject to anatomical and physiological changes. Obstruction and stasis of urine, caused by these changes, result in a higher relative risk for pyelonephritis during pregnancy and in hydronephrosis and distension above the pelvic brim in 90% of all pregnant women.3 4 Hydronephrosis during pregnancy becomes symptomatic in less than 3% of cases.5
Unlike the frequent appearance of hydronephrosis, a rupture of the urinary tract is an extremely rare complication of pregnancy which can occur in all stages of pregnancy.2 6–9 Urinary tract rupture can be divided in parenchyma rupture and renal pelvis rupture. Parenchyma ruptures can be caused by urological tumours, such as hamartomas, abscesses or trauma.3 Whereas renal pelvis ruptures are usually due to higher pressure inside the renal pelvis, because of pregnancy or renal calculus, leading to spontaneous rupture in the absence of underlying pathology.3 7 To the best of our best knowledge, since the first case description in 1947 by Campbell,10 only 32 cases of urinary tract rupture during pregnancy have been reported in the past.3 6 8 In 15 of these cases no other cause than pregnancy was detected, we added the 16th. Urinary tract rupture during pregnancy is a worrisome condition, because the symptoms can become very critical,6 especially when underlying causes are present. Urinary tract rupture is easily confused with other common urological and surgical diagnoses in pregnancy,2 as our case demonstrates as well. In combination with an infection complications of urinary tract rupture can be very severe, it may cause a perinephric abscess and the need for nephrectomy.2 7
In this case there were difficulties setting up the diagnosis. Although renal pelvis rupture is rare, it presented in a typical way compared to other reported cases. The most usual location is right-sided; only three cases of left-sided renal pelvis rupture were described.6 8 11 Though haematuria seems likely, commonly patients renal pelvis ruptures do not present with haematuria, in comparison with renal parenchyma ruptures.8 Only 3 of 16 cases of renal pelvis rupture showed haematuria (table 1).6 10 12 Therefore the absence of haematuria in our case is in accordance with the literature.
Table 1.
Review of previous spontaneous renal pelvis rupture cases during pregnancy
| Publication | Age, parity, gestation | Side | Symptoms | Haematuria | Ultrasonography | Pyelography | Other investigations | Treatment | Obstetric follow-up | Comments | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Campbell10 | 37 years, G3P2, 34 weeks | Right | 2 months existing flank mass | Yes | – | – | – | Right nephrectomy | Spontaneous stillbirth first day after nephrectomy | – |
| 2 | Cohen14 | 35 years, G8P7, 26 weeks | Right | Flank pain, upper right abdominal pain, history of urinary tract infections in pregnancy | No, but anaemia | – | Distended ureter and renal pelvis, urine extravasation | – | Right nephrectomy | Vaginal delivery at term | – |
| 3 | Aaro and Kelalis12 | 31 years, G8P7, pp1d | Right | Flank pain, progressive palpable mass | Yes | – | Pyelonephrosis, urine extravasation | – | Right nephrectomy | – | Onset of symptoms after delivery |
| 4 | Middleton, 1982 | 26 years, G3P2, 18 weeks | Right | Intermittent flank pain | No | – | Urine extravasation | – | Right nephrostomy | Vaginal delivery at term | – |
| 5 | Maresca and Koucky16 | 34 years, G6P5, 18 weeks | Right | Flank pain, vomiting, lower right abdominal pain with peritoneal signs | No | Hydronephrosis, urinoma | Urine extravasation | – | Right ureteral catheterisation after diagnostic laparotomy | Vaginal delivery at term | – |
| 6 | Kramer17 | 18 years, G1P0, 30 weeks | Right | Flank pain, vomiting, urinary frequency | No | Hydronephrosis, urinoma | Urine extravasation | – | Left lateral decubitus position | Vaginal delivery at term | – |
| 7 | Meyers et al2 | 18 years, G1P0, 27 weeks | Right | Flank pain, lower right abdominal pain | No | Hydronephrosis, urinoma | – | – | Right JJ stent | Vaginal delivery at 28 weeks | – |
| 8 | De Wilde, 1988 | 27 years, G3P2, 32 weeks | Right | Flank pain | No | Urine extravasation | – | – | Right ureteral catheterisation | Vaginal delivery at term | – |
| 9 | Oesterling et al18 | 36 years, G1P0, 20 weeks | Right | Flank pain, vomiting | No | Hydronephrosis, urinoma | Urine extravasation | – | Right ureteral catheterisation | Vaginal delivery at term | – |
| 10 | Van Winter et al9 | 20 years, G1P0, 34 weeks | Right | Flank pain, nausea, lower right abdominal pain with peritoneal signs | No | Hydronephrosis | Urine extravasation | – | Right JJ stent | Vaginal delivery at term | – |
| 11 | Chelli, 1994 | 24 years, G4P1, 28 weeks | Left | Flank pain, symptoms of urinary tract infection | No | Urine extravasation | – | CT: renal pelvis rupture with urine extravasation | Right nephrostomy | Vaginal delivery at term | – |
| 12 | Satoh et al7, 2002 | 34 years, G2P0, 20 weeks | Right | Flank pain | No | Hydronephrosis, urinoma | Urine extravasation | – | Right JJ stent | Caesarean section at term | – |
| 13 | Sidra et al19 | 28 years, G1P0, 34 weeks | Right | Flank pain | No | Hydronephrosis, hydroureter | – | – | Epidural analgesia during labor. Postpartum right nephrostomy | Vaginal delivery at 34 weeks | Patient delivered before placement of nephrostomy |
| 14 | Lo et al11 | 33 years, G1P0, 32 weeks | Left | Flank pain, lower abdominal pain | No | (performed after delivery) Hydronephrosis bilateral, hydro-ureter | – | CT performed after delivery: urine extravasation | Left nephrostomy | Caesarean section at 32 weeks | Renal pelvis rupture diagnosed after delivery |
| 15 | Matsubara et al6 | 38 years, G1P0, 34 weeks | Left | Left back pain | Yes | Bilateral hydronephrosis. | Urine extravasation | – | Left JJ stent | Caesarean section at 34 weeks | Patient anxious for continuing pregnancy and demanded caesarean section |
| 16 | Present case | 27 years, G2P1, 34 weeks | Right | Flank pain | No | Slightly distended ureter | – | MRI: urine extravasation | Right JJ stent | Vaginal delivery at term | Induction of labour because of pre-eclampsia |
Ultrasonography is considered to be the examination of choice by Wolff et al3 since this can differentiate physiological dilatation of the urinary tract from pathological dilatation in pregnancy.13 In our case, besides a slight dilatation, there were no clear signs of renal pelvis rupture. In only one previous case the same negative ultrasound result occurred.9 This negative result diverged our attention from a urinary tract problem to possible surgical problems. That is why pyelography was not considered in our case. Unfortunately, because in most previous cases it was performed and it turned out to be conclusive for the diagnosis (table 1).6 7 9 12 14–18 It might therefore be advisable to perform pyelography when the suspicion for a urinary tract problem is high, especially after a negative ultrasound result.
Instead of pyelography an MRI was performed, which was preferred above CT to protect the fetus from radiation. Though performed for other purposes, it clearly showed rupture of the renal collecting system.
Nowadays, treatment of renal pelvis rupture is easily done with JJ-stenting.10 12 14 JJ-stenting immediately resolves symptoms. The main problem is not the treatment, but the diagnosis is the main problem of this complication of pregnancy: like in our case, some previous cases show a delay in the diagnostic process as well. In one patient labour progressed quickly and the patient delivered through emergency caesarean section because of fetal distress before the diagnosis was set up,11 another patient delivered premature.19 One patient even underwent a diagnostic laparotomy on suspicion of appendicitis before she was treated for renal pelvis rupture.16
Concluding, renal pelvis rupture is an important diagnosis to have in mind when a pregnant patient presents with severe symptoms suggesting a urinary tract problem, it is important to shorten delay in setting up the diagnosis in order to start adequate treatment early. Severe complications, negative pregnancy outcomes and unnecessary despair to the patient can be prevented by early recognition and diagnosis of renal pelvis rupture.
Learning points.
Renal pelvis rupture is a rare, but impressive complication of pregnancy, which can occur spontaneously during all stages of pregnancy and which should be considered in pregnant patients with severe symptoms suggesting a urological problem.
Renal pelvis rupture can be diagnosed by ultrasonography, but this may be difficult. In case of negative ultrasound results, further diagnostic imaging like a pyelography is advisable to perform in patients with severe symptoms of urinary tract obstruction. This case has shown that MRI can be a helpful tool to set up this diagnosis without exposing the fetus to radiation.
Renal pelvis rupture can be effectively treated by the insertion of a JJ-stent, which can stay in place during the remaining weeks of pregnancy and does not necessarily need induction of labour, nor caesarean section.
Patient's perspective.
Thinking back to this period I become emotional again. I remember the intense pain and the uncertainty I felt as well as the fear for a premature delivery. I remember how desperately I was begging for painkillers. I have never felt so helpless. Owing to the combination with the emotional rollercoaster, caused by the pregnancy hormones, every minute seemed to last an hour during these days. How bizarre is it that the huge amount of despair this misery causes, so quick and painless is its intervention? The treatment immediately solved my problems. Since the efficient treatment as well as the emotional impact of these days to the following weeks of my pregnancy (ie, the sleepless nights while worrying about my baby and fearing the possible harm all medication could have on her), it is important that this diagnosis can be set up early in order to solve the problem quickly.
Footnotes
Contributors: FB was the doctor treating the patient mentioned in the manuscript. Initiated by JM—the corresponding author—FB started writing the first draft of this case report with support of HB and JM. HB provided expertise in writing a scientific manuscript for refinement and provided the reference list. The draft was reviewed by and adjusted by all authors. All authors had a substantial contribution to the manuscript and approved the final manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Visser GH, Eilers PH, Elferink-Stinkens PM et al. New Dutch reference curves for birthweight by gestational age. Early Hum Dev 2009;85:737–44. 10.1016/j.earlhumdev.2009.09.008 [DOI] [PubMed] [Google Scholar]
- 2.Meyers SJ, Lee RV, Munschauer RW. Dilatation and nontraumatic rupture of the urinary tract during pregnancy: a review. Obstet Gynecol 1985;66:809–15. [PubMed] [Google Scholar]
- 3.Wolff JM, Jung PK, Adam G et al. Non-traumatic rupture of the urinary tract during pregnancy. Br J Urol 1995;76:645–8. 10.1111/j.1464-410X.1995.tb07795.x [DOI] [PubMed] [Google Scholar]
- 4.Fiadjoe P, Kannan K, Rane A. Maternal urological problems in pregnancy. Eur J Obstet Gynecol Reprod Biol 2010;152:13–17. 10.1016/j.ejogrb.2010.04.013 [DOI] [PubMed] [Google Scholar]
- 5.Rasmussen PE, Nielsen FR. Hydronephrosis during pregnancy: a literature survey. Eur J Obstet Gynecol Reprod Biol 1988;27:249–59. 10.1016/0028-2243(88)90130-X [DOI] [PubMed] [Google Scholar]
- 6.Matsubara S, Morita T, Saito Y et al. Non-traumatic rupture of the left upper urinary tract during pregnancy without discernable underlying disorders. Arch Gynecol Obstet 2010;282:111–13. 10.1007/s00404-009-1342-3 [DOI] [PubMed] [Google Scholar]
- 7.Satoh S, Okuma A, Fujita Y et al. Spontaneous rupture of the renal pelvis during pregnancy: a case report and review of the literature. Am J Perinatol 2002;19:189–95. 10.1055/s-2002-28489 [DOI] [PubMed] [Google Scholar]
- 8.Chelli H, Bitri M, Mazlout N et al. [Spontaneous rupture of the upper urinary tract in a pregnant woman. Value of ultrasonography and computed tomography in the diagnosis and treatment] Rupture spontanee de la voie excretrice urinaire superieure chez une femme enceinte. Apport de l'echographie et de la tomodensitometrie dans le diagnostic et le traitement. J Gynecol Obstet Biol Reprod (Paris) 1997;26:734–9. [PubMed] [Google Scholar]
- 9.Van Winter JT, Ogburn PL Jr, Engen DE et al. Spontaneous renal rupture during pregnancy. Mayo Clin Proc 1991;66:179–82. 10.1016/S0025-6196(12)60490-X [DOI] [PubMed] [Google Scholar]
- 10.Campbell IC. A case of spontaneous extra- and intra-peritoneal rupture of a hydronephrosis in pregnancy. J Obstet Gynaecol Br Emp 1947;54:853 10.1111/j.1471-0528.1947.tb10774.x [DOI] [PubMed] [Google Scholar]
- 11.Lo KL, Ng CF, Wong WS. Spontaneous rupture of the left renal collecting system during pregnancy. Hong Kong Med J 2007;13:396–8. [PubMed] [Google Scholar]
- 12.Aaro LA, Kelalis PP. Spontaneous rupture of the kidney associated with pregnancy. Am J Obstet Gynecol 1971;111:270–3. [DOI] [PubMed] [Google Scholar]
- 13.MacNeily AE, Goldenberg SL, Allen GJ et al. Sonographic visualization of the ureter in pregnancy. J Urol 1991;146:298–301. [DOI] [PubMed] [Google Scholar]
- 14.Cohen SG, Pearlman CK. Spontaneous rupture of the kidney in pregnancy. J Urol 1968;100:365–9. [DOI] [PubMed] [Google Scholar]
- 15.Middleton AW Jr, Middleton GW, Dean LK. Spontaneous renal rupture in pregnancy. Urology 1980;15:60–3. 10.1016/0090-4295(80)90543-9 [DOI] [PubMed] [Google Scholar]
- 16.Maresca L, Koucky CJ. Spontaneous rupture of the renal pelvis during pregnancy presenting as acute abdomen. Obstet Gynecol 1981;58:745–7. [PubMed] [Google Scholar]
- 17.Kramer RL. Urinoma in Pregnancy. Obstet Gynecol 1983;62(3 Suppl):26s–8s. [PubMed] [Google Scholar]
- 18.Oesterling JE, Besinger RE, Brendler CB. Spontaneous rupture of the renal collecting system during pregnancy: successful management with a temporary ureteral catheter. J Urol 1988;140:588–90. [DOI] [PubMed] [Google Scholar]
- 19.Sidra LM, Keriakos R, Shayeb AG et al. Rupture renal pelvicalyceal system during pregnancy. J Obstet Gynaecol 2005;25:61–3. 10.1080/01443610400025671 [DOI] [PubMed] [Google Scholar]


