Abstract
A 29-year-old woman noticed a tender mass in her right breast. The patient was seen by her gynaecologist and was prescribed antibiotics for 10 days for mastitis. Subsequently, she underwent a core biopsy of this mass and the pathology showed granulomatous mastitis. Cultures from the biopsy sample were negative for fungus and tuberculosis. The patient's clinical symptoms initially appeared to improve with antibiotic treatment, but were complicated by the formation of an abscess, which was drained in clinic. The patient was referred to rheumatology in anticipation of steroid or methotrexate therapy, and was placed again on antibiotic treatment to which she responded adequately.
Background
Idiopathic granulomatous mastitis (GM) is a rare, benign breast disease characterised by presentation clinically similar to breast carcinoma. It usually affects women of childbearing age. The diagnosis is confirmed by characteristic histology showing multinucleated giant cells and the formation of non-caseating granulomas. Although the precise cause of this inflammatory condition has not been established, the disease has been linked to prior oral contraceptive use, a history of pregnancy and breastfeeding. The treatment of this disease still remains controversial. Antibiotics, surgical interventions and corticosteroid therapy have been used. We are presenting a case of idiopathic GM that initially responded to antibiotic treatment but was later complicated by an abscess. The patient was then referred to rheumatology where she was treated with further antibiotics and had an adequate response. Surgical intervention should be avoided, if feasible, given the autoimmune nature of this disease process and the high rate of surgical complications, including recurrence and mammary fistulas. Accurate diagnosis is essential as patients are concerned about the possibility of malignancy.
Case presentation
A 29-year-old woman first noticed a tender mass in her right breast in July 2014 while in Amarillo, Texas. She had two pregnancies in 2005 and 2008, and neither child was breastfed. She has a history of oral contraceptive use for 2 years before her first born. She has no family history of breast cancer. She consulted her gynaecologist about a week and a half after discovering the mass. She said it was initially the size of a grapefruit, with bruising and erythaema. She denied any trauma to the breast.
Investigations
A mammogram was performed, which found an 8 cm bulging, hard mass centred at 3 o'clock in the right breast (figure 1). There was flattening of the nipple areolar complex and mild retraction of the nipple. No palpable adenopathy was detected in the right axilla.
Figure 1.
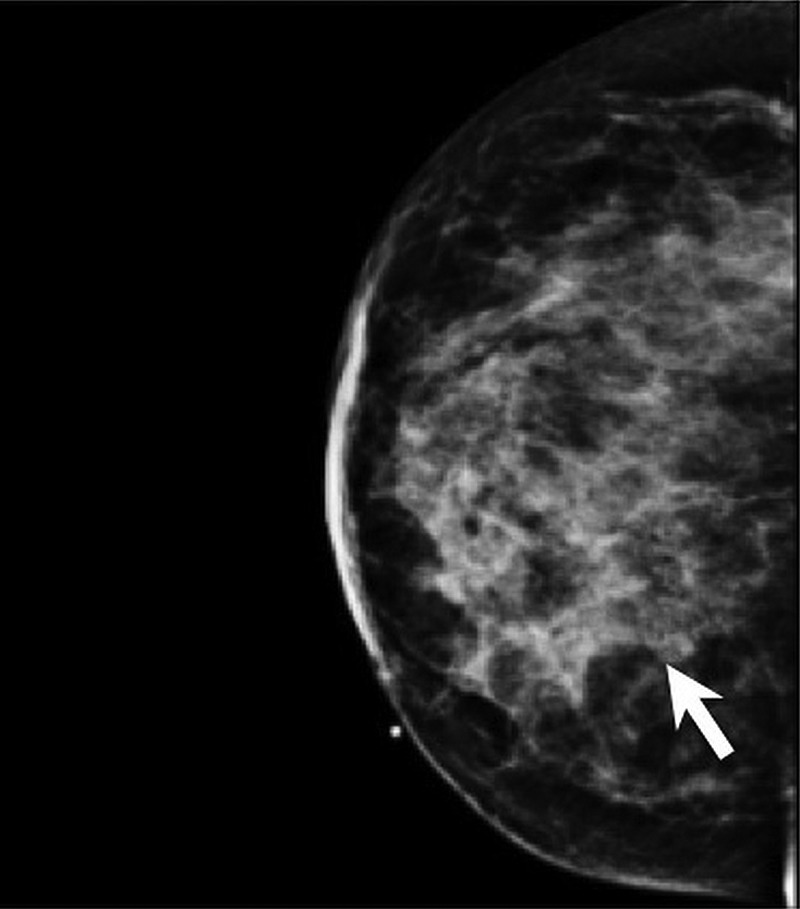
Mammogram right cranio caudal view of right breast with an 8 cm hard mass centred at 3 o’clock in the right breast.
At that point, the differential diagnoses included non-puerperal mastitis and inflammatory carcinoma, so an ultrasound-guided core needle biopsy was recommended. Since infection was on the differential diagnosis, the patient was placed on 1 tablet of sulfamethoxazole/trimethoprim twice a day for 14 days. The ultrasound-guided biopsy was performed and showed that the mass was 7 cm from the nipple (figure 2). Pathology showed benign process correlating with florid acute, chronic and granulomatous mastitis (figure 3).
Figure 2.
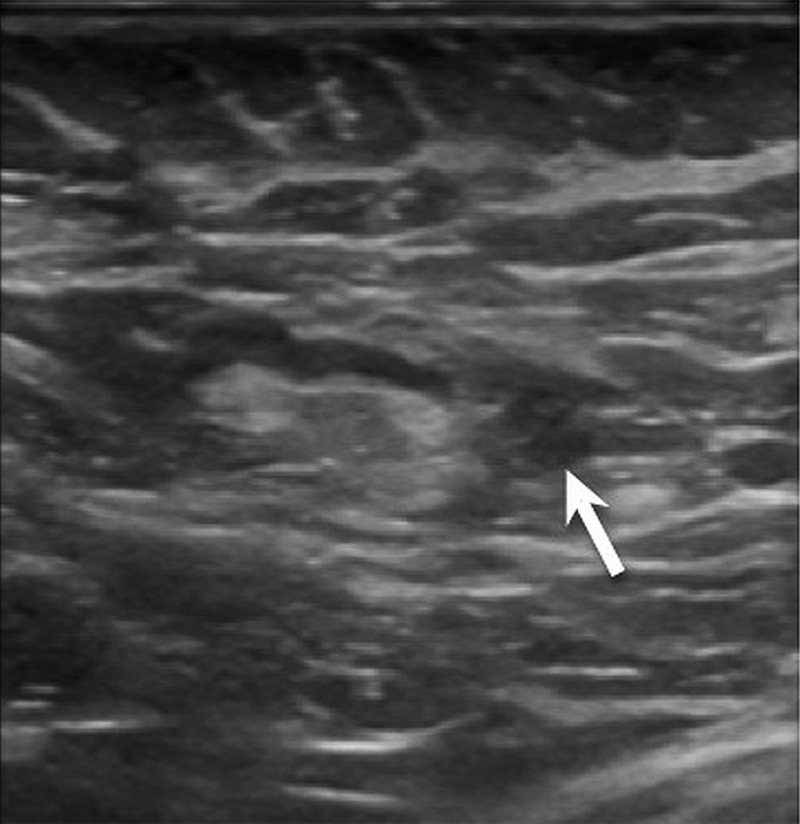
US-guided biopsy of right breast with finding of a mass 7 cm from the nipple.
Figure 3.
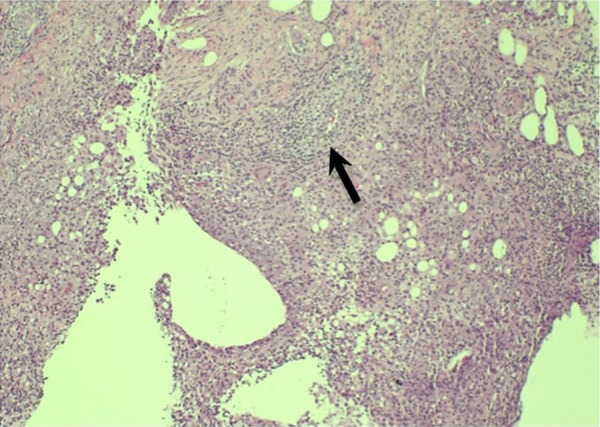
Pathology report of right breast specimen correlating with florid acute, chronic and granulomatous mastitis.
Acid-fast bacillus stain and Grocott-Gomori's methenamine silver stain were negative for mycobacterial and fungal organisms. There was no evidence of atypical hyperplasia or malignancy. Therefore, a diagnosis of idiopathic GM was established.
Differential diagnosis
Idiopathic GM is a diagnosis of exclusion, so it was imperative to rule out other possibilities to guide proper treatment. Since GM has been known to mimic breast carcinoma, it was essential to rule out cancer to prevent unnecessary aggressive treatment of a benign condition. Through the various investigations conducted as well as the patient's clinical presentation, we were able to rule out inflammatory breast carcinoma, tuberculosis, fungal disease and Wegener's granulomatosis. Pathology report of the biopsy specimen further confirmed our suspicion of idiopathic GM.
Treatment
The patient was later referred to our clinic for surgical consultation and management. In our clinic, the patient presented with positive erythaema at the biopsy site and slight warmth of the right breast. There was also positive induration of the medial aspect of the right breast measuring at 5×5 cm (figure 4). The patient noted that pain, swelling and the overall size of the mass was decreasing after the onset of sulfamethoxazole/trimethoprim use. She was counselled to complete the course of sulfamethoxazole/trimethoprim and return to our clinic in 2 weeks for follow-up.
Figure 4.

Image of right breast with erythaema and induration.
At her follow-up appointment, the patient presented with an abscess in the right breast in the area of concern. She stated that this began after she completed her antibiotic course. A small incision was made to help drain the abscess. The patient was then referred to a rheumatologist in anticipation of steroid or immunosuppressant treatment. The rheumatologist started the patient on a course of minocycline to inhibit metalloproteinase enzymes for inflammation and ranitidine for H1 and H2 blockade. On laboratory testing, the patient had elevated erythrocyte sedimentation rate, borderline anaemia, positive antinuclear antibody and positive HLA-B27, which suggested an autoimmune component.
The patient returned to our clinic, where she began treatment with amoxicillin/clavulanic acid due to a new area of ulceration near the right areola. The rheumatologist also referred the patient to an infectious disease physician due to concern over persistent infectious process. This needed to resolve before beginning any immunosuppressive therapy. The patient was instructed to continue the course of amoxicillin/clavulanic acid for 2 months, with which she improved.
Outcome and follow-up
Since steroid therapy has been shown to be effective in the treatment of idiopathic GM, the rheumatologist plans to initiate therapy with steroids and methotrexate, if necessary, in the future. At 4 months postinitial presentation of symptoms, conservative management was found effective in the treatment of this patient. This circumvented the need for surgical intervention. Close follow-up will be maintained to ensure full resolution and to monitor for recurrence.
Discussion
Idiopathic GM is an uncommon inflammatory breast disease. It was first described by Kessler and Wolloch1 in 1972, and continues to be a perplexing condition. Cases of GM are challenging because they mimic breast carcinoma and also because they are among a wide range of differential diagnoses including Mycobacterium infection, Wegener's granulomatosis, parasitic infection, fungal infections, sarcoidosis, polyarteritis nodosa and foreign body reaction.2 Radiological and cytological findings alone are not sufficient to establish a diagnosis of GM, because the remaining differentials must be excluded to do so.3 Histopathological examination with the presence of epithelioid and multinucleated giant cell granulomas with microabscesses suggests the diagnosis of GM.4 The aetiology and treatment are still challenging aspects of this benign, yet locally aggressive condition. It has been associated with a history of pregnancy, breast-feeding, childbearing age and Hispanic ethnicity.2 5 There is still considerable controversy over definitive treatment of GM. Treatment options include medical management with antibiotics, steroid therapy and immunosuppressive agents, as well as more invasive approaches such as surgical excision and abscess drainage.6 Much of the recent literature has found corticosteroid therapy to be an effective means of GM resolution with a smaller chance of recurrence.3 5–7 There are others who still support surgical excision as primary treatment with the use of steroids to limit the size of the lesion.8 A recent study of 24 patients in New York found that medical management was most effective, with an 80% response rate to prednisone and methotrexate, and a comparable recurrence rate of 50% to previous reports.2
Learning points.
Idiopathic granulomatous mastitis continues to be a rare breast disease with unclear aetiology and treatment guidelines. It should be suspected in women of childbearing age with a history of pregnancy and lactation, who present with a non-malignant breast mass.
An aetiological workup with negative results of the differential must be carried out before a diagnosis of idiopathic granulomatous mastitis can be established.
While treatment remains controversial, recent literature supports the efficacy of conservative management with steroid and immunosuppressive therapy, leaving surgical excision for complicated, refractory cases.
As response to treatment varies among individual patients and the recurrence rate remains high, close follow-up should be maintained.
Footnotes
Contributors: MM acquired the data, wrote the first draft of the manuscript and made revisions based on input and guidance from coauthors. PS and SM conducted the analyses and interpretation of data, and made revisions to the manuscript draft. All authors read and approved the final manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kessler E, Wolloch Y. Granulomatous mastitis: a lesion clinically simulating carcinoma. Am J Clin Pathol 1972;58:642–6. [DOI] [PubMed] [Google Scholar]
- 2.Joseph K, Luu X, Mor A. Granulomatous mastitis: a New York public hospital experience. Ann Surg Oncol 2014;21:4159–63. 10.1245/s10434-014-3895-z [DOI] [PubMed] [Google Scholar]
- 3.Ayeva-Derman M, Perrotin F, Lefrancq T et al. Idiopathic granulomatous mastitis. Review of literature illustrated by 4 cases. J Gynecol Obstet Biol Reprod (Paris) 1999;28:800–7. [PubMed] [Google Scholar]
- 4.Lai E, Chan W, Ma T et al. The role of conservative treatment in idiopathic granulomatous mastitis. Breast J 2005;11:454–6. 10.1111/j.1075-122X.2005.00127.x [DOI] [PubMed] [Google Scholar]
- 5.Pandey TS, Mackinnon JC, Bressler L et al. Idiopathic granulomatous mastitis—a prospective study of 49 women and treatment outcomes with steroid therapy. Breast J 2014;20:258–66. 10.1111/tbj.12263 [DOI] [PubMed] [Google Scholar]
- 6.Mizrakli T, Velidedeoglu M, Yemisen M et al. Corticosteroid treatment in the management of idiopathic granulomatous mastitis to avoid unnecessary surgery. Surg Today Published Online First: 4 July 2014. doi:10.1007/s00595-014-0966-5 10.1007/s00595-014-0966-5 [DOI] [PubMed] [Google Scholar]
- 7.Salehi M, Salehi H, Moafi M et al. Comparison of the effect of surgical and medical therapy for the treatment of idiopathic granulomatous mastitis. J Res Med Sci 2014;19(Suppl 1):S5–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Atak T, Sagiroglu J, Eren T et al. Strategies to treat idiopathic granulomatous mastitis: retrospective analysis of 40 patients. Breast Dis 2015;35:19–24. 10.3233/BD-140373 [DOI] [PubMed] [Google Scholar]


