Abstract
While the most recognised complication after joint surgery is septic arthritis, other forms of joint pathology may occur. We present a case of postoperative polyarthritis with high inflammatory markers, which responded to a course of prednisolone. The occurrence of high IgM cardiolipin antibodies that normalised with treatment suggests that this condition is a form of transient autoimmunity.
Background
Postoperative inflammation polyarthritis is an uncommon complication of surgery. In many ways it mimics presentation of rheumatoid arthritis but is acute, seronegative and responds rapidly with a short course of steroids. The pathogenesis of this condition is unknown but may represent loss of immune tolerance to self-antigens in joint tissues. There is so far no autoantibody associated with this diagnosis suggested in the literature.
Case presentation
A 63-year-old man developed symmetrical acute polyarthritis affecting the small joints of the fingers of both hands, feet, ankles, knees, wrists and elbows, 10 days after right shoulder manipulation under arthroscopy (MUA), capsular release and decompression for interval adhesive capsulitis.
He reported severe early morning stiffness lasting 3 h and there was florid synovitis of small joints in the hands and feet, wrists, elbows, knees and ankles. He could barely stand up or walk and was very restricted in activities of daily living.
Three years prior, he had an uneventful left shoulder MUA decompression of left shoulder, release of anterior capsule and repair of an intra-articular supraspinatus tear. There was no recent history of infection or trauma and no history of psoriasis, iritis or inflammatory bowel disease. The patient did not have any significant history apart from a radical prostatectomy for carcinoma of the prostate. There is no family history of rheumatological conditions.
Investigations
Laboratory investigations at presentation are shown on table 1. Abnormal results are highlighted in bold.
Table 1.
Laboratory investigations at presentation
| Laboratory test | Presentation | Normal ranges |
|---|---|---|
| General haematology | ||
| Haemoglobulin | 12.2 | 13–18 g/dL |
| White cell count | 5.5×109 | 4–11×109/L |
| Platelet count | 148×109 | 150–400×109/L |
| ESR | 112 | 1–14 mm/h |
| Coagulation | ||
| Prothrombin time | 10.3 | 8.9–12 s |
| PTR/INR | 1.0 | 0.9–1.1 |
| APTT | 22 | 21–31 s |
| APTT ratio | 0.9 | 0.8–1.2 |
| Thrombin time | 0.9 | 12–17 s |
| Thrombin time ratio | 1.1 | 0.8–1.2 |
| DRVVT ratio | 1.05 | 0.74–1.1 |
| Lupus anticoagulant | Not detected | |
| Biochemistry | ||
| Sodium serum | 133 | 136–145 mmol/L |
| Potassium serum | 4.4 | 3.6–5.0 mmol/L |
| Urea | 6.4 | 2.0–7.8 mmol/L |
| Creatinine | 78 | 75–122 µmol/l |
| Estimated GFR | 87 | mL/min |
| Total bilirubin serum | 8 | 2–22 µmol/L |
| Alanine aminotransferase | 106 | 10–40 IU/L |
| Aspartate aminotransferase | 50 | 10–40 IU/L |
| γ-Glutamyl transferase | 89 | 8–78 μ/L |
| Alkaline transferase | 51 | 30–130 IU/L |
| Total protein | 67 | 64–83 g/L |
| Albumin | 33 | 35–50 g/L |
| C reactive protein | 142 | 2–7 mg/L |
| Uric acid | 0.306 | 0.21–0.42 mmol/L |
| Ferritin | 649 | 10–160 µg/L |
| Calcium | 2.26 | mmol/L |
| Adjusted calcium | 2.20 | 2.2–2.6 mmol/L |
| Inorganic phosphate | 1.07 | 0.8–1.5 mmol/L |
| Endocrinology | ||
| Free T4 serum | 18.6 | 10–24.5 |
| TSH | 1.44 | 1.44 mIU/L |
| Specialist proteins | ||
| Immunoglobulin G | 10.5 | 5.5–16.5 g/L |
| Immunoglobulin A | 3.37 | 0.8–4 g/L |
| Immunoglobulin M | 1.27 | 0.4–2 g/L |
| Rheumatoid factor | 15 | 0–20 IU/mL |
| Autoimmune serology | ||
| ANA | Negative | |
| IgG ANCA | Negative | |
| Cardiolipin IgG | 6.4 | 0–10 IU/mL |
| Cardiolipin IgM | 132 | 0–10 IU/mL |
| Anti-B2 glycoprotein IgG | 2.5 | 0–10 IU/mL |
| Anti-B2 glycoprotein IgM | 2.5 | 0–10 IU/mL |
| CCP antibody | 1.6 | 0–10 IU/mL |
ANA, antinuclear antibody; ANCA, antineutrophil cytoplasmic autoantibody; APTT, activated partial thromboplastin time; CCP, cyclic citrullinated peptides; DRVVT, dilute Russell's viper venom time; ESR, erythrocyte sedimentation rate; eGFR, estimated-glomerular filtration rate; INR, international normalised ratio; PTR, prothrombin time; TSH, thyroid-stimulating hormone.
Radiology of the hands and wrists did not show any abnormality.
Differential diagnosis
Although this patient has a condition that resembles rheumatoid arthritis (RA), the duration of the polyarthritis lasted less than 2 weeks, which precludes the diagnosis of RA. The rheumatoid factor and anticyclic citrullinated antibody were both within normal range.
Another inflammatory condition that can present with raised erythrocyte sedimentation rate (ESR) in this patient's age group is polymyalgia rheumatism (PMR). However, the pattern of involvement in this patient was peripheral rather than proximal. Therefore, his condition is not consistent with PMR.
The differential diagnoses for acute polyarthritis are wide and include infection-associated arthritis, reactive arthritis, Still's disease, systemic lupus erythematosus and rheumatoid arthritis. In our case, there is no evidence of infection or systemic features of a connective tissue disease.
Raised ferritin is seen in hereditary haemachromatosis; however, this is unlikely in our patient, who is already in his sixth decade of age and does not have skin pigmentation, diabetes, impotence, cardiac or liver disease. There is also no evidence of iron overload; the patient had normal serum iron and transferrin levels. The elevated ferritin was an acute phase reaction and normalised when repeated.
Lastly, in relation to the raised IgM cardiolipin antibodies, the patient had no previous history of thrombosis or other features for the diagnosis of antiphospholipid syndrome.
Treatment
After assessment, the patient was started on prednisolone 30 mg and hydroxychloroquine 200 mg twice a day.
Outcome and follow-up
The patient's joint stiffness and pain largely disappeared within 1 day of receiving the prednisolone and treatment was tapered. The prednisolone was stopped after 6 months, and the hydroxychloroquine was reduced to 200 mg a day a year after onset. The improvement of his symptoms was mirrored by a steep drop in the IgM cardiolipin antibody, and inflammatory markers CRP and ESR (see figure 1) returning to normal. Ferritin levels normalised at 236 with normal iron and transferrin levels making it unlikely that this patient has haemachromatosis.
Figure 1.
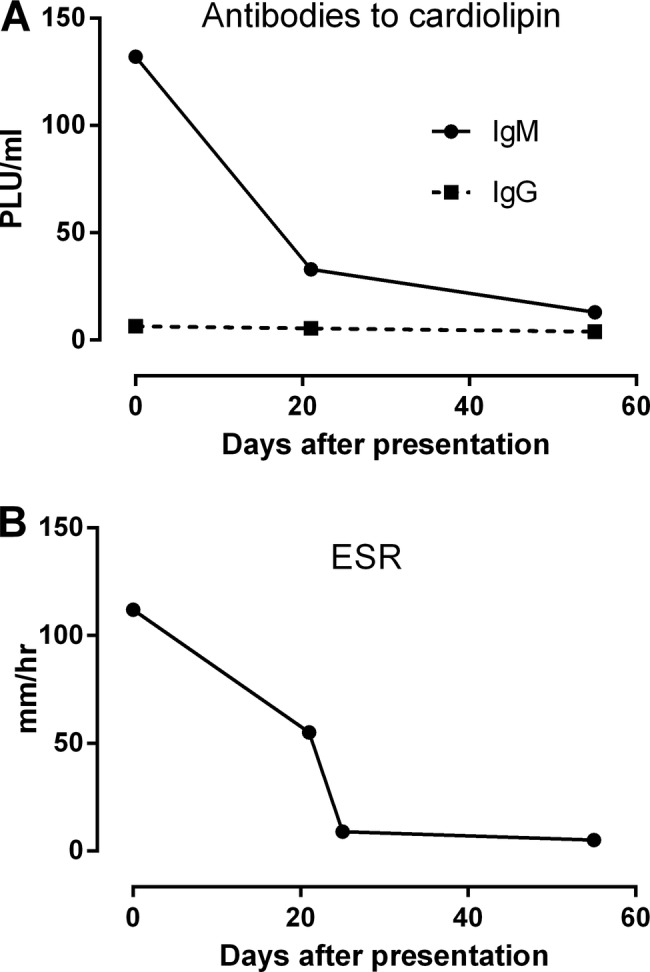
(A) Reduction of high erythrocyte sedimentation rate (ESR) at presentation with prednisolone and hydroxychloroquine given at day 0. (B) Reduction of high IgM cardiolipin antibodies at presentation correlate with reduction of ESR with prednisolone and hydroxychloroquine given at day 0.
The patient has been followed up now for 2 years with no relapse of arthritis. He is currently still on hydroxychloroquine 200 mg once a day and is on six-monthly follow-up.
Discussion
The strong temporal association implicates the joint surgery as a cause for the polyarthritis. One surgical procedure reported to cause polyarthritis is intestinal bypass surgery for morbid obesity.1 The pathogenesis was postulated to occur from the exposure of gut bacteria antigens systemically resulting in immune complexes, which activate the classical as well as alternate complement system, resulting in the polyarthritis.2 However, routine joint repair surgery is usually aseptic, which contrasts starkly with intestinal bypass surgery. In this case, neo-self-antigens are more likely to be the trigger in activating the immune system. The patient had previous joint surgery that may have sensitised his immune system resulting in polyarthritis during the next joint surgery.
Antibodies to cardiolipin can occur acutely in a wide variety of conditions including infection,3 cancer,4 acute myocardial infarction5 and organ transplant,6 but these conditions were not reported to occur with polyarthritis. In one study, 95% of patients receiving knee or hip replacement developed a new lupus anticoagulant, however, it is unusual to develop antibodies to cardiolipin (2%).7 We report an unusual case of polyarthritis after shoulder surgery associated with high levels of IgM cardiolipin antibody, which, when treated with immunosuppression, resulted in rapid improvement and reduction of the IgM cardiolipin antibody. It is unknown if the IgM cardiolipin antibody is an epiphenomenon or if it directly causes the polyarthritis.
Learning points.
Although it is important to exclude rheumatoid arthritis in a patient with symmetrical polyarthritis, other causes of acute inflammatory arthritis should be considered.
Acute inflammatory arthritis can be successfully treated with prednisolone and hydroxychloroquine.
It is important to recognise postoperative inflammatory arthritis, and IgM cardiolipin antibodies may be associated with this condition.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Shagrin JW, Frame B, Duncan H. Polyarthritis in obese patients with intestinal bypass. Ann Intern Med 1971;75:377–80. 10.7326/0003-4819-75-3-377 [DOI] [PubMed] [Google Scholar]
- 2.Wands JR, LaMont JT, Mann E et al. Arthritis associated with intestinal-bypass procedure for morbid obesity. Complement activation and characterization of circulating cryoproteins. N Engl J Med 1976;294:121–4. 10.1056/NEJM197601152940301 [DOI] [PubMed] [Google Scholar]
- 3.Avcin T, Toplak N. Antiphospholipid antibodies in response to infection. Curr Rheumatol Rep 2007;9:212–18. 10.1007/s11926-007-0034-x [DOI] [PubMed] [Google Scholar]
- 4.Battistelli S, Stefanoni M, Petrioli R et al. Antiphospholipid antibodies and acute-phase response in non-metastatic colorectal cancer patients. Int J Biol Markers 2008;23:31–5. [PubMed] [Google Scholar]
- 5.Gunupati S, Chava VK, Krishna BP. Effect of phase I periodontal therapy on anti-cardiolipin antibodies in patients with acute myocardial infarction associated with chronic periodontitis. J Periodontol 2011;82:1657–64. 10.1902/jop.2011.110002 [DOI] [PubMed] [Google Scholar]
- 6.Furmańczyk-Zawiska A, Bączkowska T, Sadowska A et al. Antiphospholipid antibodies in renal allograft recipients. Transplant Proc 2013;45:1655–60. 10.1016/j.transproceed.2013.02.043 [DOI] [PubMed] [Google Scholar]
- 7.Simpson M, Sanfelippo MJ, Onitilo AA et al. Anti-phospholipid antibodies in patients undergoing total joint replacement surgery. Thrombosis 2012;2012:142615–0. 10.1155/2012/142615 [DOI] [PMC free article] [PubMed] [Google Scholar]


