Abstract
Fragile X syndrome, an X-linked dominant disorder with reduced penetrance, is associated with intellectual and emotional disabilities ranging from learning problems to mental retardation, and mood instability to autism. It is most often caused by the transcriptional silencing of the FMR1 gene, due to an expansion of a CGG repeat found in the 5′-untranslated region. The FMR1 gene product, FMRP, is a selective RNA-binding protein that negatively regulates local protein synthesis in neuronal dendrites. In its absence, the transcripts normally regulated by FMRP are over translated. The resulting over abundance of certain proteins results in reduced synaptic strength due to AMPA receptor trafficking abnormalities that lead, at least in part, to the fragile X phenotype.
Keywords: Fragile X syndrome, FMR1, permutation, full mutation, autism
Introduction
Fragile X syndrome (FXS) is the most common inherited cause of mental retardation with approximately 1 in 4000 males affected.1 In the vast majority of cases, this X-linked disorder is caused by expansions of a CGG repeat in the 5′-untranslated (UTR) region of the FMR1 gene that arises due to the meiotic instability of certain alleles of this repeat tract. FXS causing alleles, or full mutations, contain 200 or more copies of the repeat that are hypermethylated and transcriptionally silenced. The unstable alleles that give rise to full mutations are called premutations and are associated with phenotypes distinct from FXS. The mutational mechanism, combined with the location of this gene on the X chromosome, leads to remarkable inheritance patterns in which the relevant alleles are passed from intellectually normal men through their unaffected daughters and then to affected sons.2
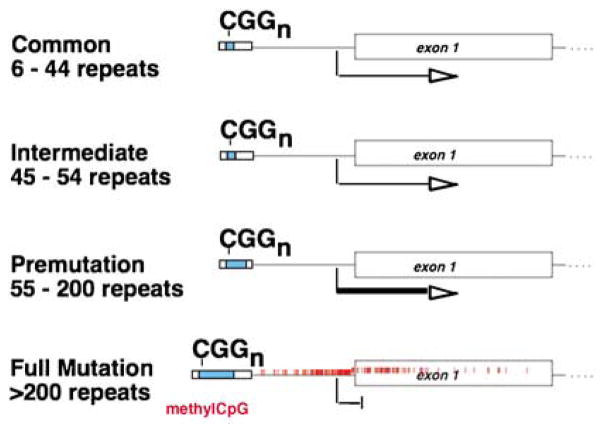
FXS may be suspected in both sexes, and includes a variable clinical phenotype. Individuals with FXS may present with anything from learning problems and a normal IQ to severe mental retardation and autistic behaviors. Physical features have been described but are often nonspecific. Thus, diagnosis is made based upon the detection of alterations to FMR1 (Figure 1).
Figure 1.
Four allelic classes of the FMR1 gene in humans. For each allele, the size of the CGG repeat in the 5′-UTR of FMR1 is indicated in blue at the left of the gene schematic. The level of transcription is indicated by the width of the arrow beneath each allele class. Increased transcription is associated with premutation alleles, whereas full mutations are hypermethylated, as indicated by the red hashmarks, and transcriptionally silent. Despite the ACMG definition, the smallest premutation allele known to expand to the full mutation in a single generation had 59 repeats.
Clinical overview
The physical characteristics of FXS are fairly subtle, and the first clinical indication is often delayed developmental milestones, such as mild motor delays and/or language delays.3 Autistic-like behaviors such as hand flapping, poor eye contact, and hand biting may be noted.
The average IQ in adult men with the completely methylated full mutation is approximately 40.4 Less-affected males typically have incomplete methylation, resulting in an incomplete activation of FMR1, and they may even have an IQ in the borderline or low normal range. In general, for FXS, cognitive deficits include problems with working and short-term memory, executive function, and mathematic and visuospatial abilities.5 Because the disorder is X-linked, females are generally much more mildly affected than males, particularly in terms of cognitive functioning, but they tend to have higher risk for emotional problems compared to the general population.6 Females with the full mutation usually have normal or borderline IQ, and most will have associated learning disabilities and/or emotional problems.7
Individuals with FXS usually do not have significant medical issues. Recurrent otitis media and recurrent sinusitis are common during childhood.8 Joint laxity with hyperextensibility finger joints and pes planus (flat feet) may be present and usually improve with age.9 Gastroesophageal reflux disease occurs in a third of young infants with FXS, and may present with irritability or recurrent emesis.9 Seizures and EEG findings consistent with epilepsy are another common feature of FXS during childhood, with an incidence between 13 and 18% in boys and 5% in girls.10
The majority of individuals with the premutation have normal intelligence, but males are prone to have attentional problems, executive dysfunction, social deficits, and obsessive-compulsive behavior.11 Approximately 20% of women who carry an FMR1 premutation have premature ovarian failure (POF), which is the premature cessation of menses before the age of 40.12 A subgroup of men with a premutation develop neurologic deficits beyond age 50.13 Although many of these individuals would have been given a diagnosis of parkinsonism in the past, a distinct tremor/ataxia syndrome due to premutations in FMR1 has been recently recognized. The fragile X-associated tremor/ataxia syndrome (FXTAS) causes intentional tremors, balance problems, frequent falls, neuropathy, autonomic dysfunction, cognitive decline, and dementia, which may progressively worsen over time.14
Behavioral aspects
The behavioral phenotype may be helpful in suggesting the diagnosis of FXS. Autistic-like features are common in individuals with FXS and include hand flapping, hand biting, gaze avoidance, tactile defensiveness, and hyperarousal to sensory stimuli.15,16 These features – along with impaired social skills, such as socio-emotional reciprocity – are expressed with varying degrees in children with FXS and may be indicative of a concurrent diagnosis of autism spectrum disorder or autistic-like behavior.17 Anxiety and mood disorders, hyperactivity, impulsivity, and aggressive behavior can also be present.18
The emotional and behavioral characteristics in females with FXS are usually variable. Females with the full mutation are prone to social anxiety, shyness, social avoidance, withdrawal, language deficits, mood lability, and depression.6 Furthermore, females with the premutation have also been described to have social anxiety.19
Physical features
Physical features include macroorchidism that is apparent just prior to puberty20 and those related to a connective tissue dysplasia, which include a long, narrow face, prominent ears, joint hypermobility, and flat feet.21 The facial characteristics (Figure 2) can be subtle and may become more apparent with increasing age.
Figure 2.
Facial features of fragile X syndrome. As illustrated by the photographs of four children with FXS, the facies associated with this syndrome are subtle. They can include a long, thin face, and prominent ears that often project away from the head, and a prominent forehead.
Neuroanatomy
At autopsy, no gross abnormalities are observed in the brains of individuals with FXS.22 In males with FXTAS, MRI findings include global brain atrophy and white matter abnormalities, including involvement of the middle cerebellar peduncles.23
A key neurological feature of individuals with FXS is that, in certain areas of the brain, their neurons have immature and dense dendritic spines.24 The spines are the site at which the majority of excitatory synapses occur, and, although it is not known whether they are a cause or an effect, similar abnormalities have been associated with other forms of mental retardation.25 It is believed that these differences represent a defect in dendritic spine development and maturation.24
Molecular and genetic basis of the disease
In 1991, the gene responsible for FXS, FMR1, was identified.26 Fragile X was the first known example of a trinucleotide repeat disorder (Figure 1).
There are four allelic classes for the CGG-repeat tract in the 5′-UTR of FMR1. The repeat sizes for each group are not well defined, and this complicates genetic counseling. In the general population, the repeat tract contains up to 40 repeats, with 30 being the most common (normal or common alleles).27 Next are the intermediate alleles, which range from 41 to 54 repeats and which usually are not associated with instability of the repeat tract.
Full mutations, which cause FXS, have over 200 copies of the repeat.27,28 Hypermethylation of this expanded repeat tract and the upstream CpG island silences FMR1 expression.29
Full mutations arise from the allele class known as premutations, which range in size from approximately 55–200 repeats and are meiotically unstable.27,28 Premutations are unmethylated, transcriptionally active, and produce FMRP, although possibly in lower quantities than normal.30 These alleles can expand in small amounts to yield a slightly larger premutation allele, or they can expand massively into the full mutation range. Expansion to the full mutation occurs only in females because the full mutation cannot be maintained during spermatogenesis.31
The expanded repeat may be unstable and exhibits somatic heterogeneity in affected individuals, called mosaics. Mosaicism may be both in terms of repeat length as well as methylation status (methylation mosaics). Affected males with methylation mosaicism have, on average, higher IQ scores than those with fully methylated alleles, presumably because they express some FMRP.32
Although FMR1 premutation carriers are not affected by FXS, they are at risk for the additional phenotypes of POF and FXTAS, as mentioned previously. In contrast to the lack of FMR1 transcription associated with FXS, the premutation-associated diseases are caused by a toxic RNA effect caused by an excess of FMR1 transcription and/or repeat-containing mRNA.33 With FXTAS, this toxic effect is associated with the presence of intranuclear inclusions in the neurons and astrocytes of affected brains.33
Fragile X mental retardation protein
FMRP binds to specific mRNAs and has an important role in the regulation of protein synthesis at a local level in the dendrites of neurons. The finding of abnormally long and immature dendritic spines in the brains of people with FXS and the importance of these spines in synaptic transmission, synaptic plasticity, learning, and memory suggest that understanding the function of FMRP at the synapse could be the key to understanding the development of FXS syndrome.
A proposed role for FMRP at the synapse is that it is a negative regulator of protein synthesis stimulated by group 1 metabotropic glutamate receptor (mGluR) activation.34 FXS, then, is at least partially a result of exaggerated responses to mGluR stimulation. In particular, one of the primary defects associated with the absence of FMRP appears to be excessive AMPA receptor internalization in response to mGluR signaling.35 These alterations to AMPA receptor trafficking effect persistent changes in synaptic activity. This disease model is supported by the fact that treatment with the mGluR antagonist 2-methyl-6-phenylethynyl-pyridine rescues the defect in AMPA receptor trafficking in cultured FMRP-deficient neurons,35 as well as some of the defects associated with the lack of FMRP in Drosophila and mouse models lacking FMRP function.36,37 In addition, Fmr1-deficient mice that express 50% of the normal level of mGluR5 are rescued for several phenotypes, including changes to the density of dendritic spines, susceptibility to audiogenic seizures, and altered plasticity in the visual cortex.38
Diagnostic approaches
A checklist of phenotypic criteria has been established in order to identify individuals with undiagnosed developmental delay who would be appropriate candidates for FXS molecular testing3 (Table 1). These checklists, of which several had been devised prior to that of Maes, may increase the diagnostic yield slightly, but because children may not have apparent physical features, it is accepted practice to order fragile X testing in all children with developmental delay, mental retardation, or autism,39 although this may have a diagnostic yield of only approximately 1–2%.40 The presence in the proband’s family of movement disorders, learning disabilities, mental retardation, or primary ovarian insufficiency should increase suspicion of the presence of FMR1 mutations in the family.41 A suggested targeted family history questionnaire can be found in Table 2.
Table 1.
Phenotypic screening checklist (after Maes et al3)
The following checklist was proposed by Maes et al3 to be used in men of any age who have developmental delays of unknown cause. Each of the items in the checklist is to be answered by a ‘yes’ or ‘no’. Referral is recommended by a score of at least 17, and a score of 26 or higher indicates that referral is necessary. It is important to recognize that FXS is not uniform or distinctive in its presentation. The items in the checklist may not be recognizable in early childhood and may emerge over time. Indeed, other factors (eg family history) must be considered in suspecting the diagnosis.
|
Abbreviation: FXS, fragile X syndrome.
Table 2.
Suggested targeted family questionnaire for Fragile X Syndrome (after McConkie-Rosell et al42)
This questionnaire is appropriate for use in cases of suspected FXS, families with a confirmed diagnosis, and at-risk or known carriers. The history and age of onset should be noted for each relevant family member.
|
Abbreviation: FXS, fragile X syndrome.
The testing procedure encompasses two complementary analyses. PCR with primers flanking the repeat is used to determine the number of CGG repeats in the FMR1 5′-UTR, and a Southern blot of genomic DNA is used to determine the methylation status and to gauge the size of full mutations, which are often resistant to PCR amplification. 18 The combination of Southern blot and PCR for the detection of fragile X-associated mutations has a sensitivity of 99%. The remaining 1% of mutations include missense mutations and full or partial deletions of FMR1.39 There is a deficit of reported missense mutations of FMR1 due to the over reliance on CGG-repeat testing. Thus, in any individual presenting with a clinical suspicion of FXS but with normal CGG-repeat lengths, sequencing of FMR1, which also uncovers deletions in males, should be considered. Fragile X testing of an individual with isolated cognitive impairment should be done in conjunction with cytogenetic evaluation because constitutional chromosomal abnormalities are as common, if not more common, than FXS in this population.39
The same testing approach can also be used to identify premutation carriers. Prenatal diagnosis for full mutations can be performed on either chorionic villus or amniocentesis samples and has proven to be highly reliable.43
Management
Genetic counseling
If a positive FXS test is discovered, the proband and family should be referred for genetic counseling and cascade testing of family members at risk of carrying a full mutation or premutation.41 Premutation carriers should be counseled regarding their risks of passing a full mutation onto their children, and they should also be counseled of their own risks of POF and/or FXTAS. When planning cascade testing in an affected family, particular attention should be considered for family members with mental retardation, learning disabilities, autism, or social and behavioral disorders; female relatives with infertility or premature menopause; and those with tremor, ataxia, or other neurological and psychiatric problems.
Genetic counseling becomes difficult when FMR1 alleles in the ~45–54 repeat range are identified. This is a ‘gray zone’ because unstable alleles of this size have been reported in families but the expansion is unlikely. Premutations are most often clinically reported when the repeat tract is 55 repeats or greater, although the smallest repeat known to expand to a full mutation in a single generation was 59 repeats. The American College of Medical Genetics provides guidelines for fragile X testing at http://www.acmg.net/Pages/ACMG_Activities/stds-2002/fx.htm.
Treatment and care
Current approaches to therapy for FXS are all symptom based, and few controlled trials have been performed to determine their effectiveness.44 Psychopharmacologic intervention should be combined with other supportive strategies, including speech therapy, sensory integration occupational therapy, individualized educational plans, and tailored behavioral interventions to maximize functioning.
In boys with FXS, the most frequently used medications are stimulants.44 These medications are targeted to symptoms of hyperactivity, impulsivity, and distractability and can be quite helpful in these areas.44 Despite being the most common medication in FXS, the efficacy of these drugs and their side effects vary for each individual. The response rate to stimulants may be relatively lowered in adult men with FXS because of their increased anxiety and decreased activity level.44
Some researchers believe that many of the behavioral problems observed in individuals with FXS are secondary to problems with hyperarousal to sensory stimuli.18 Although it can be difficult to implement, structuring the environment of the affected individual such that they are comfortable with their surroundings is one approach to alleviating this issue.18 Another approach is the use of α2-adrenergic agonists, which are thought to dampen the response to sensory input to the brain and show good efficacy in treating some of these behaviors in boys with FXS.44
Selective serotonin reuptake inhibitors (SSRIs) are quite commonly used to treat mood disorder, anxiety, and obsessive-compulsive behaviors associated with FXS. They are effective, particularly in alleviating social anxiety, tantrums, and aggression.44 Individuals treated with SSRIs should be monitored for restlessness, mood changes, hyperactivity, and disinhibited behavior including aggression.44
Atypical antipsychotics have been used to treat self-injury, aggressive behaviors, and autism. Parental reports of improvement in mood stabilization, attention, and academic performance have been noted with the atypical antipsychotic aripiprazole, which should be used at low doses to avoid the agitation that can be induced by higher doses.45 Adverse events associated with antipsychotics include weight gain (although not with aripiprazole), sedation, nausea, constipation, diabetes, and tardive dyskinesia. In individuals with rapid weight gain, monitoring for diabetes and metabolic syndrome must be considered.
As mentioned previously, the phenotype in FXS is caused by excessive mGluR5 signaling, thus drugs targeting mGluR5 may be an effective treatment for FXS.34 Several mGluR5 anatagonists are presently in pharmaceutical development for an array of targeted clinical symptoms, such as anxiety disorder, Parkinson’s Disease, and substance abuse.46 In addition, a recent placebo-controlled clinical trial of the AMPA receptor positive modulator (Ampakine) CX 516 indicates no significant improvements in memory, language, attention/executive function, behavior, and cognitive functioning in subjects with FXS, but suggest improvement in subjects cotreated with antipsychotics compared with those on placebo.47 Similar to other studies, it is possible that CX516 is a low potency agent and the dosing may have been inadequate for therapeutic effect. Future clinical trials involving mGluR5 antagonists and AMPA receptor signaling may potentially provide a targeted treatment of FXS in alleviating the core psychiatric and neurologic symptoms.
Environmental variables may influence an individual’s development of adaptive behaviors, cognitive abilities, and behavioral symptoms.48 For instance, children with FXS residing in a higher quality home environment displayed fewer autistic behaviors, better adaptive behavior, and higher IQ level. Some of the characteristics of the home environment that may be a factor in these effects are parenting ability, parental expectations of child behavior, organization of the home, emotional climate, and enrichments in the home.48 Further studies in this area may lead to the development of nonpharmaceutical therapies that can help improve the outcomes of individuals with FXS. At present, there are virtually no studies on the effectiveness of specific behavioral interventions in FXS despite our knowledge regarding their distinct behavioral phenotypes.
Conclusions
Although current therapies for FXS are aimed at symptom management, it is hoped that future molecular therapies, whether they are aimed at mGluR5, the AMPA receptor, or other molecular targets, will be directed at preventing the development of some of the symptoms of FXS. This may be a challenge because neurological evidence of FXS on a cellular level can be seen very early postnatally.49 Early diagnosis will be key to making these therapies more effective, and there are efforts to implement newborn or infant screening for FXS. In a survey of parents of children with FXS during the 1990s, a significant delay was found between the time they first became concerned about the child’s development (median age: 12 months) and the time they received a diagnosis of FXS (median age: 26 months).50 Thus, clinicians should address parental concern and consider the diagnosis of FXS in any infant or toddler with developmental delays.
In brief.
Fragile X syndrome is a common inherited form of mental retardation that can be associated with features of autism.
The physical features of fragile X syndrome are subtle and may not be obvious.
The vast majority of cases of fragile X syndrome are caused by the expansion to over 200 copies of a CGG repeat in the 5′-untranslated region of FMR1 that shuts off transcription of the gene.
Genetic testing for this repeat expansion is diagnostic for this syndrome, and testing is appropriate in all children with developmental delay, mental retardation or autism.
Fragile X syndrome is inherited from individuals, usually females, who typically carry an unstable premutation allele of the CGG-repeat tract in FMR1.
Premutation carriers are themselves at risk of premature ovarian failure and the fragile X-associated tremor/ataxia syndrome.
References
- 1.Crawford DC, Acuna JM, Sherman SL. FMR1 and the fragile X syndrome: human genome epidemiology review. Genet Med. 2001;3:359–371. doi: 10.1097/00125817-200109000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sherman SL, Jacobs PA, Morton NE, et al. Further segregation analysis of the fragile X syndrome with special reference to transmitting males. Hum Genet. 1985;69:289–299. doi: 10.1007/BF00291644. [DOI] [PubMed] [Google Scholar]
- 3.Maes B, Fryns JP, Ghesquiere P, Borghgraef M. Phenotypic checklist to screen for fragile X syndrome in people with mental retardation. Ment Retard. 2000;38:207–215. doi: 10.1352/0047-6765(2000)038<0207:PCTSFF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Merenstein SA, Sobesky WE, Taylor AK, Riddle JE, Tran HX, Hagerman RJ. Molecular-clinical correlations in males with an expanded FMR1 mutation. Am J Med Genet. 1996;64:388–394. doi: 10.1002/(SICI)1096-8628(19960809)64:2<388::AID-AJMG31>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 5.Kemper MB, Hagerman RJ, Altshul-Stark D. Cognitive profiles of boys with the fragile X syndrome. Am J Med Genet. 1988;30:191–200. doi: 10.1002/ajmg.1320300118. [DOI] [PubMed] [Google Scholar]
- 6.Freund LS, Reiss AL, Abrams MT. Psychiatric disorders associated with fragile X in the young female. Pediatrics. 1993;91:321–329. [PubMed] [Google Scholar]
- 7.de Vries BB, Wiegers AM, Smits AP, et al. Mental status of females with an FMR1 gene full mutation. Am J Hum Genet. 1996;58:1025–1032. [PMC free article] [PubMed] [Google Scholar]
- 8.Hagerman RJ, Altshul-Stark D, McBogg P. Recurrent otitis media in the fragile X syndrome. Am J Dis Child (1960) 1987;141:184–187. doi: 10.1001/archpedi.1987.04460020074031. [DOI] [PubMed] [Google Scholar]
- 9.Hagerman RJ. Medical follow-up and pharmacotherapy. In: Hagerman RJ, Hagerman PJ, editors. Fragile X Syndrome: Diagnosis, Treatment and Research. 3. Baltimore: The Johns Hopkins University Press; 2002. pp. 287–338. [Google Scholar]
- 10.Musumeci SA, Hagerman RJ, Ferri R, et al. Epilepsy and EEG findings in males with fragile X syndrome. Epilepsia. 1999;40:1092–1099. doi: 10.1111/j.1528-1157.1999.tb00824.x. [DOI] [PubMed] [Google Scholar]
- 11.Farzin F, Perry H, Hessl D, et al. Autism spectrum disorders and attention-deficit/hyperactivity disorder in boys with the fragile X premutation. J Dev Behav Pediatr. 2006;27:S137–S144. doi: 10.1097/00004703-200604002-00012. [DOI] [PubMed] [Google Scholar]
- 12.Allingham-Hawkins DJ, Babul-Hirji R, Chitayat D, et al. Fragile X premutation is a significant risk factor for premature ovarian failure: the International Collaborative POF in Fragile X study – preliminary data. Am J Med Genet. 1999;83:322–325. [PMC free article] [PubMed] [Google Scholar]
- 13.Jacquemont S, Hagerman RJ, Leehey MA, et al. Penetrance of the fragile X-associated tremor/ataxia syndrome in a premutation carrier population. JAMA. 2004;291:460–469. doi: 10.1001/jama.291.4.460. [DOI] [PubMed] [Google Scholar]
- 14.Willemsen R, Mientjes E, Oostra BA. FXTAS: a progressive neurologic syndrome associated with Fragile X premutation. Curr Neurol Neurosci Rep. 2005;5:405–410. doi: 10.1007/s11910-005-0065-5. [DOI] [PubMed] [Google Scholar]
- 15.Hagerman RJ, Jackson AW, III, Levitas A, Rimland B, Braden M. An analysis of autism in fifty males with the fragile X syndrome. Am J Med Genet. 1986;23:359–374. doi: 10.1002/ajmg.1320230128. [DOI] [PubMed] [Google Scholar]
- 16.Brown WT, Jenkins EC, Cohen IL, et al. Fragile X and autism: a multicenter survey. Am J Med Genet. 1986;23:341–352. doi: 10.1002/ajmg.1320230126. [DOI] [PubMed] [Google Scholar]
- 17.Kaufmann WE, Cortell R, Kau AS, et al. Autism spectrum disorder in fragile X syndrome: communication, social interaction, and specific behaviors. Am J Med Genet. 2004;129:225–234. doi: 10.1002/ajmg.a.30229. [DOI] [PubMed] [Google Scholar]
- 18.Tsiouris JA, Brown WT. Neuropsychiatric symptoms of fragile X syndrome: pathophysiology and pharmacotherapy. CNS Drugs. 2004;18:687–703. doi: 10.2165/00023210-200418110-00001. [DOI] [PubMed] [Google Scholar]
- 19.Franke P, Leboyer M, Gansicke M, et al. Genotype – phenotype relationship in female carriers of the premutation and full mutation of FMR-1. Psychiatry Res. 1998;80:113–127. doi: 10.1016/s0165-1781(98)00055-9. [DOI] [PubMed] [Google Scholar]
- 20.Lachiewicz AM, Dawson DV. Do young boys with fragile X syndrome have macroorchidism? Pediatrics. 1994;93:992–995. [PubMed] [Google Scholar]
- 21.Hagerman RJ, Van Housen K, Smith AC, McGavran L. Consideration of connective tissue dysfunction in the fragile X syndrome. Am J Med Genet. 1984;17:111–121. doi: 10.1002/ajmg.1320170106. [DOI] [PubMed] [Google Scholar]
- 22.Hinton VJ, Brown WT, Wisniewski K, Rudelli RD. Analysis of neocortex in three males with the fragile X syndrome. Am J Med Genet. 1991;41:289–294. doi: 10.1002/ajmg.1320410306. [DOI] [PubMed] [Google Scholar]
- 23.Jacquemont S, Hagerman RJ, Leehey M, et al. Fragile X premutation tremor/ataxia syndrome: molecular, clinical, and neuroimaging correlates. Am J Hum Genet. 2003;72:869–878. doi: 10.1086/374321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Irwin SA, Patel B, Idupulapati M, et al. Abnormal dendritic spine characteristics in the temporal and visual cortices of patients with fragile-X syndrome: a quantitative examination. Am J Med Genet. 2001;98:161–167. doi: 10.1002/1096-8628(20010115)98:2<161::aid-ajmg1025>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 25.Kaufmann WE, Moser HW. Dendritic anomalies in disorders associated with mental retardation. Cereb Cortex. 2000;10:981–991. doi: 10.1093/cercor/10.10.981. [DOI] [PubMed] [Google Scholar]
- 26.Verkerk AJ, Pieretti M, Sutcliffe JS, et al. Identification of a gene (FMR-1) containing a CGG repeat coincident with a breakpoint cluster region exhibiting length variation in fragile X syndrome. Cell. 1991;65:905–914. doi: 10.1016/0092-8674(91)90397-h. [DOI] [PubMed] [Google Scholar]
- 27.Snow K, Doud LK, Hagerman R, Pergolizzi RG, Erster SH, Thibodeau SN. Analysis of a CGG sequence at the FMR-1 locus in fragile X families and in the general population. Am J Hum Genet. 1993;53:1217–1228. [PMC free article] [PubMed] [Google Scholar]
- 28.Fu YH, Kuhl DP, Pizzuti A, et al. Variation of the CGG repeat at the fragile X site results in genetic instability: resolution of the Sherman paradox. Cell. 1991;67:1047–1058. doi: 10.1016/0092-8674(91)90283-5. [DOI] [PubMed] [Google Scholar]
- 29.Sutcliffe JS, Nelson DL, Zhang F, et al. DNA methylation represses FMR-1 transcription in fragile X syndrome. Hum Mol Genet. 1992;1:397–400. doi: 10.1093/hmg/1.6.397. [DOI] [PubMed] [Google Scholar]
- 30.Kenneson A, Zhang F, Hagedorn CH, Warren ST. Reduced FMRP and increased FMR1 transcription is proportionally associated with CGG repeat number in intermediate-length and premutation carriers. Hum Mol Genet. 2001;10:1449–1454. doi: 10.1093/hmg/10.14.1449. [DOI] [PubMed] [Google Scholar]
- 31.Malter HE, Iber JC, Willemsen R, et al. Characterization of the full fragile X syndrome mutation in fetal gametes. Nat Genet. 1997;15:165–169. doi: 10.1038/ng0297-165. [DOI] [PubMed] [Google Scholar]
- 32.McConkie-Rosell A, Lachiewicz AM, Spiridigliozzi GA, et al. Evidence that methylation of the FMR-I locus is responsible for variable phenotypic expression of the fragile X syndrome. Am J Hum Genet. 1993;53:800–809. [PMC free article] [PubMed] [Google Scholar]
- 33.Hagerman PJ, Hagerman RJ. The fragile-X premutation: a maturing perspective. Am J Hum Genet. 2004;74:805–816. doi: 10.1086/386296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bear MF, Huber KM, Warren ST. The mGluR theory of fragile X mental retardation. Trends Neurosci. 2004;27:370–377. doi: 10.1016/j.tins.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 35.Nakamoto M, Nalavadi V, Epstein MP, Narayanan U, Bassell GJ, Warren ST. Fragile X mental retardation protein deficiency leads to excessive mGluR5-dependent internalization of AMPA receptors. Proc Natl Acad Sci USA. 2007;104:15537–15542. doi: 10.1073/pnas.0707484104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McBride SM, Choi CH, Wang Y, et al. Pharmacological rescue of synaptic plasticity, courtship behavior, and mushroom body defects in a Drosophila model of fragile X syndrome. Neuron. 2005;45:753–764. doi: 10.1016/j.neuron.2005.01.038. [DOI] [PubMed] [Google Scholar]
- 37.Yan QJ, Rammal M, Tranfaglia M, Bauchwitz RP. Suppression of two major Fragile X Syndrome mouse model phenotypes by the mGluR5 antagonist MPEP. Neuropharmacology. 2005;49:1053–1066. doi: 10.1016/j.neuropharm.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 38.Dolen G, Osterweil E, Rao BS, et al. Correction of fragile X syndrome in mice. Neuron. 2007;56:955–962. doi: 10.1016/j.neuron.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sherman S, Pletcher BA, Driscoll DA. Fragile X syndrome: diagnostic and carrier testing. Genet Med. 2005;7:584–587. doi: 10.1097/01.GIM.0000182468.22666.dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rauch A, Hoyer J, Guth S, et al. Diagnostic yield of various genetic approaches in patients with unexplained developmental delay ormental retardation. Am J Med Genet. 2006;140:2063–2074. doi: 10.1002/ajmg.a.31416. [DOI] [PubMed] [Google Scholar]
- 41.McConkie-Rosell A, Abrams L, Finucane B, et al. Recommendations from multi-disciplinary focus groups on cascade testing and genetic counseling for fragile X-associated disorders. J Genet Couns. 2007;16:593–606. doi: 10.1007/s10897-007-9099-y. [DOI] [PubMed] [Google Scholar]
- 42.McConkie-Rosell A, Finucane B, Cronister A, Abrams L, Bennett RL, Pettersen BJ. Genetic counseling for fragile x syndrome: updated recommendations of the national society of genetic counselors. J Genet Couns. 2005;14:249–270. doi: 10.1007/s10897-005-4802-x. [DOI] [PubMed] [Google Scholar]
- 43.Brown WT, Houck GE, Jr, Jeziorowska A, et al. Rapid fragile X carrier screening and prenatal diagnosis using a nonradioactive PCR test. JAMA. 1993;270:1569–1575. [PubMed] [Google Scholar]
- 44.Berry-Kravis E, Potanos K. Psychopharmacology in fragile X syndrome – present and future. Ment Retard Dev Disabil Res Rev. 2004;10:42–48. doi: 10.1002/mrdd.20007. [DOI] [PubMed] [Google Scholar]
- 45.Hagerman RJ. Lessons from fragile X regarding neurobiology, autism, and neurodegeneration. J Dev Behav Pediatr. 2006;27:63–74. doi: 10.1097/00004703-200602000-00012. [DOI] [PubMed] [Google Scholar]
- 46.Slassi A, Isaac M, Edwards L, et al. Recent advances in non-competitive mGlu5 receptor antagonists and their potential therapeutic applications. Curr Top Med Chem. 2005;5:897–911. doi: 10.2174/1568026054750236. [DOI] [PubMed] [Google Scholar]
- 47.Berry-Kravis E, Krause SE, Block SS, et al. Effect of CX516, an AMPA-modulating compound, on cognition and behavior in fragile X syndrome: a controlled trial. J Child Adolesc Psychopharmacol. 2006;16:525–540. doi: 10.1089/cap.2006.16.525. [DOI] [PubMed] [Google Scholar]
- 48.Glaser B, Hessl D, Dyer-Friedman J, et al. Biological and environmental contributions to adaptive behavior in fragile X syndrome. Am J Med Genet. 2003;117:21–29. doi: 10.1002/ajmg.a.10549. [DOI] [PubMed] [Google Scholar]
- 49.Nimchinsky EA, Oberlander AM, Svoboda K. Abnormal development of dendritic spines in FMR1 knock-out mice. J Neurosci. 2001;21:5139–5146. doi: 10.1523/JNEUROSCI.21-14-05139.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bailey DB, Skinner D, Sparkman K, Moore CA, Olney RS, Crawford DC. Delayed diagnosis of fragile X syndrome – United States, 1990–1999. MMWR Morb Mortal Wkly Rep. 2002;51:740–742. [PubMed] [Google Scholar]