Abstract
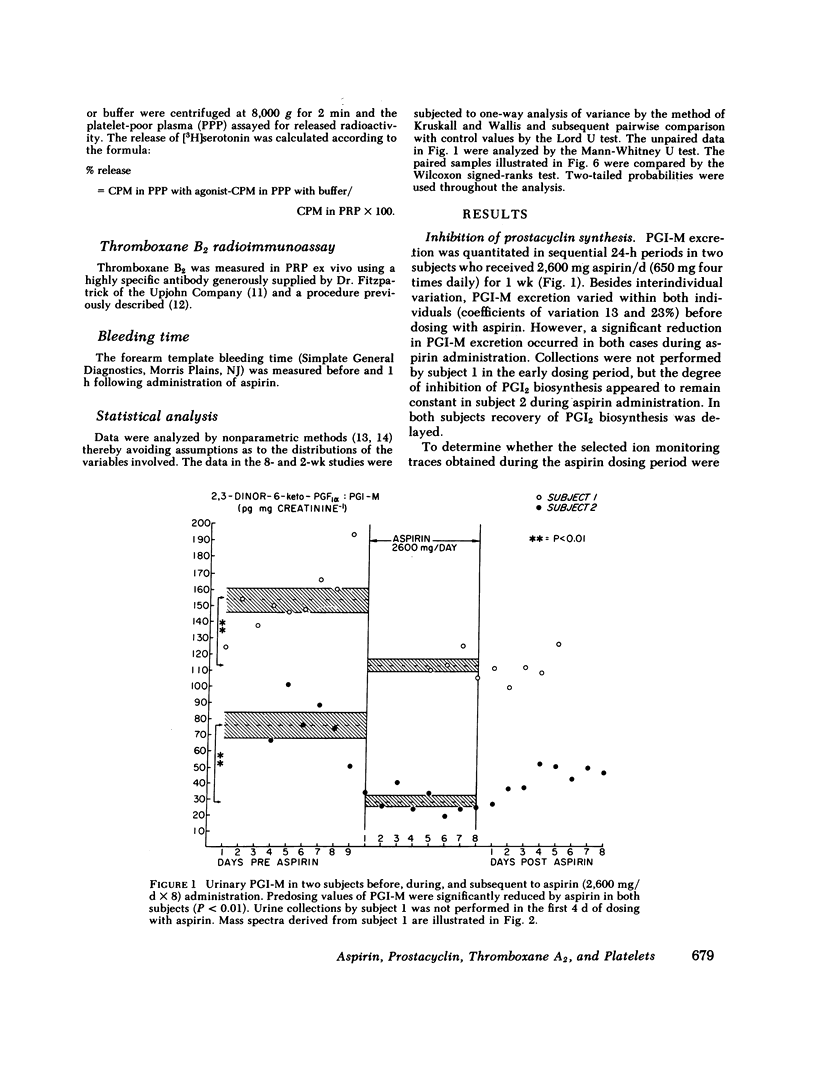
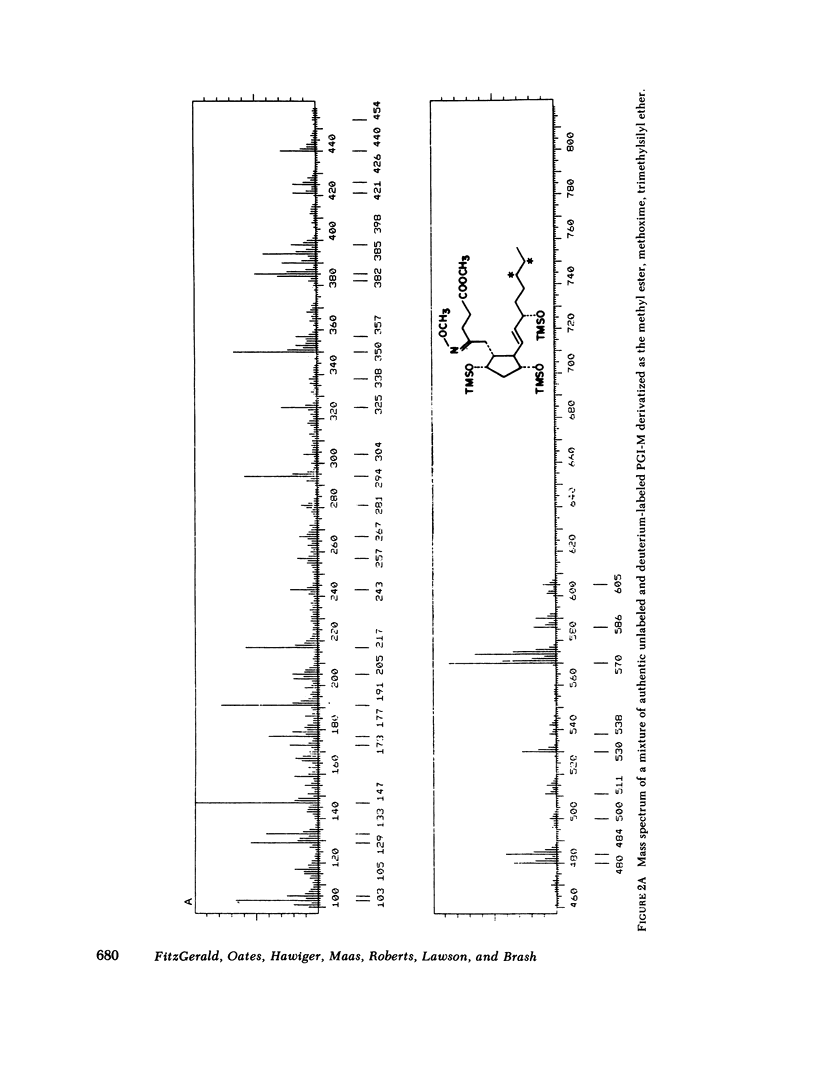
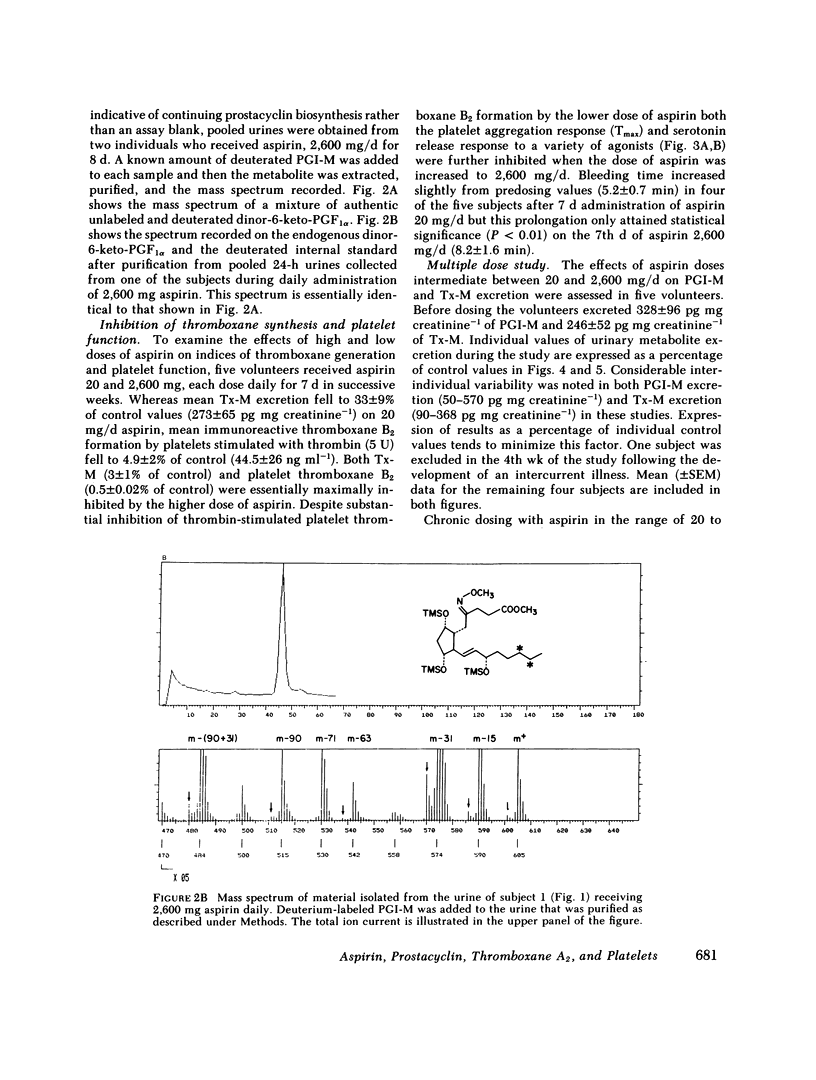
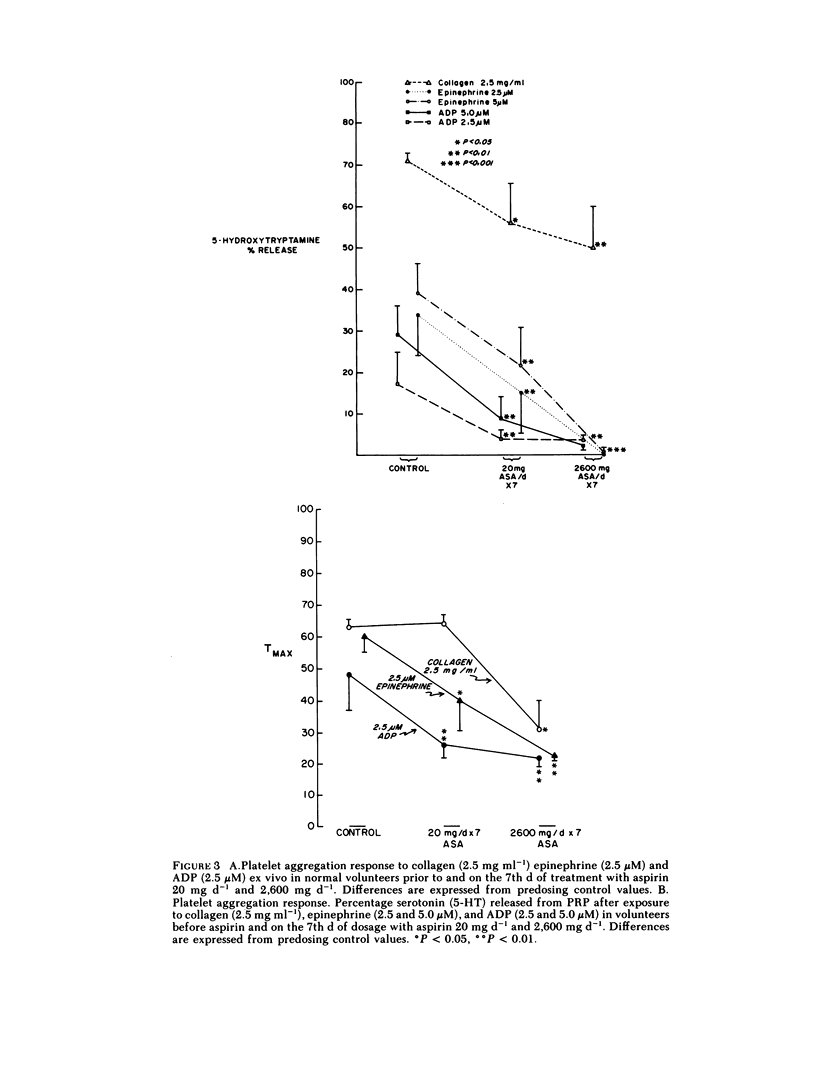
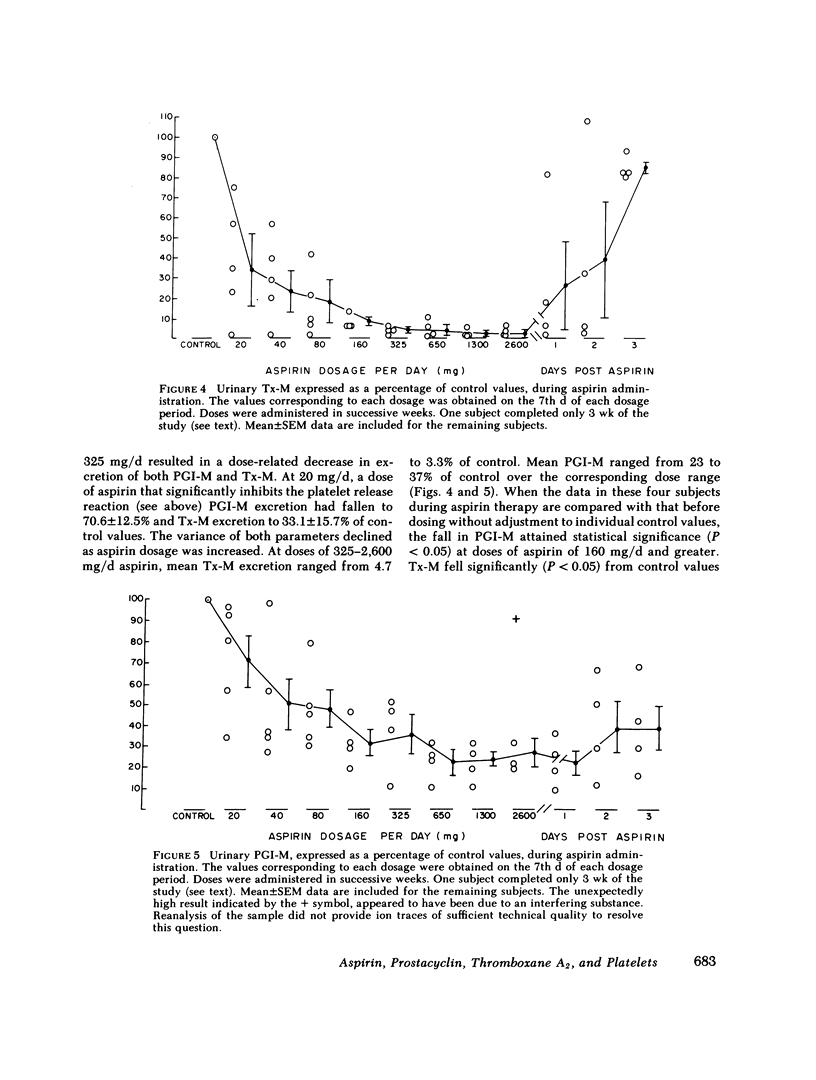
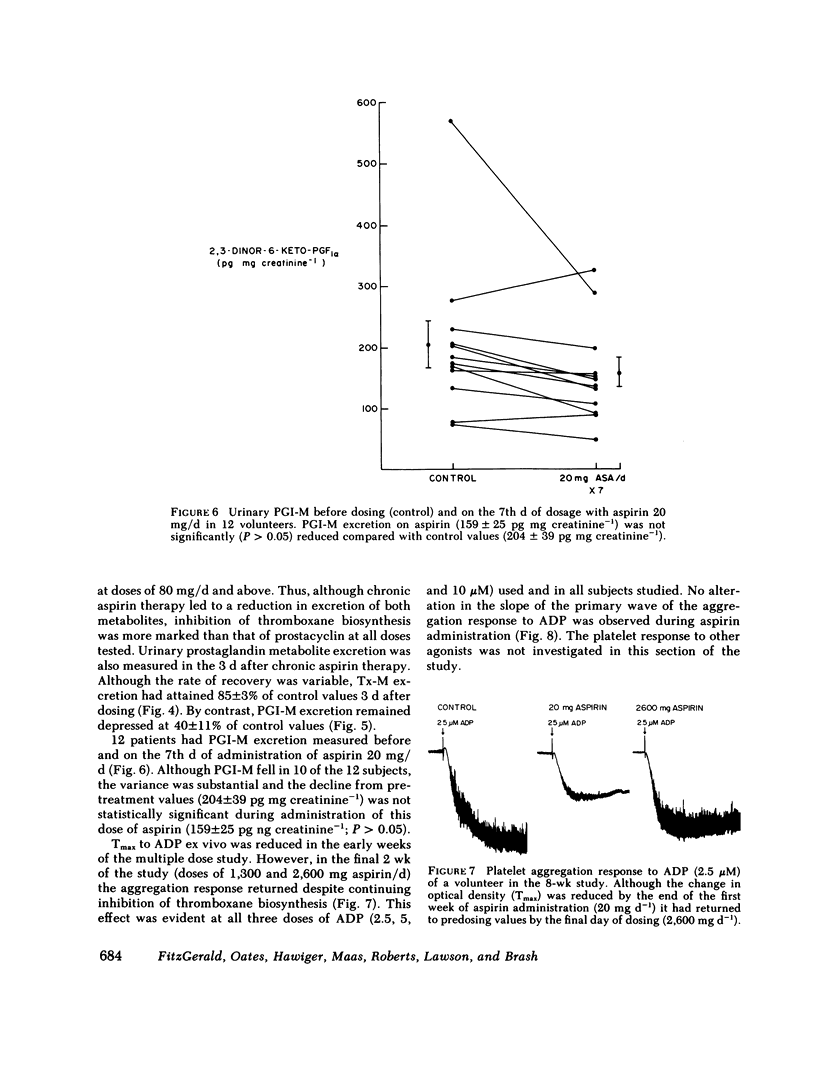
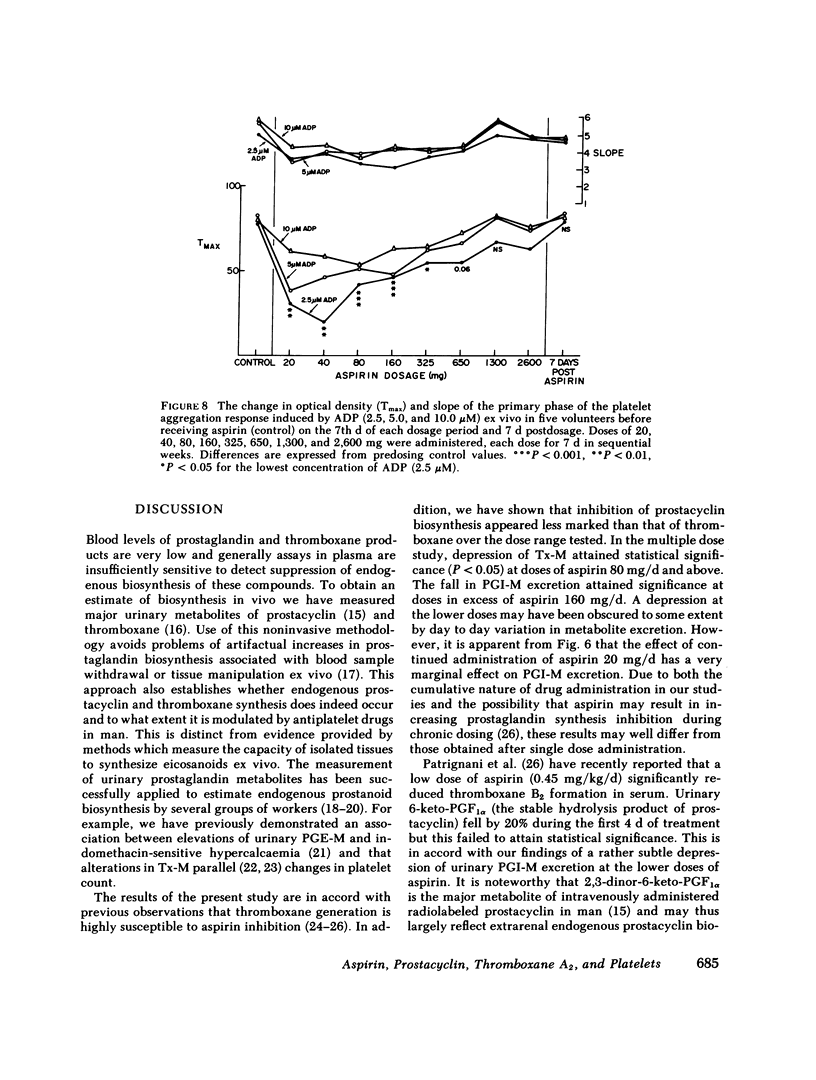
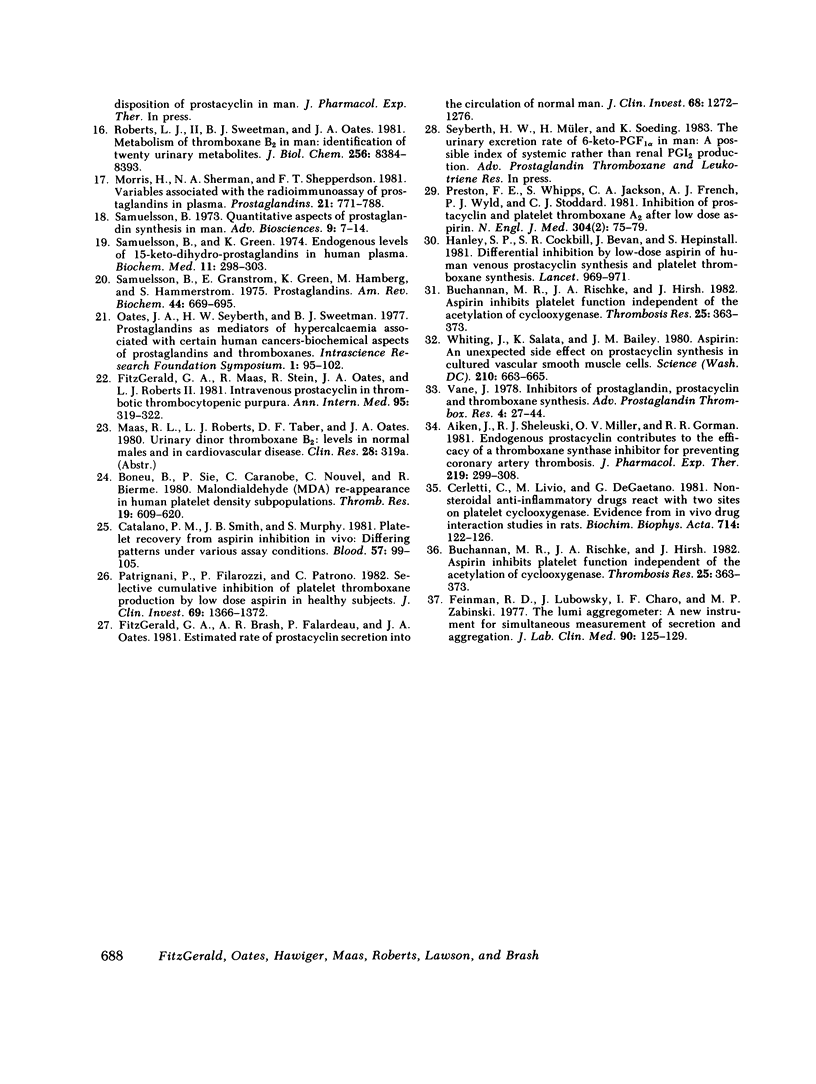
To assess the pharmacologic effects of aspirin on endogenous prostacyclin and thromboxane biosynthesis, 2,3-dinor-6-keto PGF1 alpha (PGI-M) and 2,3-dinor-thromboxane B2 (Tx-M) were measured in urine by mass spectrometry during continuing administration of aspirin. To define the relationship of aspirin intake to endogenous prostacyclin biosynthesis, sequential urines were initially collected in individuals prior to, during, and subsequent to administration of aspirin. Despite inter- and intra-individual variations, PGI-M excretion was significantly reduced by aspirin. However, full mass spectral identification confirmed continuing prostacyclin biosynthesis during aspirin therapy. Recovery of prostacyclin biosynthesis was incomplete 5 d after drug administration was discontinued. To relate aspirin intake to indices of thromboxane biosynthesis and platelet function, volunteers received 20 mg aspirin daily followed by 2,600 mg aspirin daily, each dose for 7 d in sequential weeks. Increasing aspirin dosage inhibited Tx-M excretion from 70 to 98% of pretreatment control values; platelet TxB2 formation from 4.9 to 0.5% and further inhibited platelet function. An extended study was performed to relate aspirin intake to both thromboxane and prostacyclin generation over a wide range of doses. Aspirin, in the range of 20 to 325 mg/d, resulted in a dose-dependent decline in both Tx-M and PGI-M excretion. At doses of 325-2,600 mg/d Tx-M excretion ranged from 5 to 3% of control values while PGI-M remained at 37-23% of control. 3 d after the last dose of aspirin (2,600 mg/d) mean Tx-M excretion had returned to 85% of control, whereas mean PGI-M remained at 40% of predosing values. Although the platelet aggregation response (Tmax) to ADP ex vivo was inhibited during administration of the lower doses of aspirin the aggregation response returned to control values during the final two weeks of aspirin administration (1,300 and 2,600 mg aspirin/d) despite continued inhibition of thromboxane biosynthesis. These results suggest that although chronic administration of aspirin results in inhibition of endogenous thromboxane and prostacyclin biosynthesis over a wide dose range, inhibition of thromboxane biosynthesis is more selective at 20 than at 2,600 mg aspirin/d. However, despite this, inhibition of platelet function is not maximal at the lower aspirin dosage. Doses of aspirin in excess of 80 mg/d resulted in substantial inhibition of endogenous prostacyclin biosynthesis. Thus, it is unlikely that any dose of aspirin can maximally inhibit thromboxane generation without also reducing endogenous prostacyclin biosynthesis. These results also indicate that recovery of endogenous prostacyclin biosynthesis is delayed following aspirin administration and that the usual effects of aspirin on platelet function ex vivo may be obscured during chronic aspirin administration in man.
Full text
PDF




Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aiken J. W., Shebuski R. J., Miller O. V., Gorman R. R. Endogenous prostacyclin contributes to the efficacy of a thromboxane synthetase inhibitor for preventing coronary artery thrombosis. J Pharmacol Exp Ther. 1981 Nov;219(2):299–308. [PubMed] [Google Scholar]
- BORN G. V. Aggregation of blood platelets by adenosine diphosphate and its reversal. Nature. 1962 Jun 9;194:927–929. doi: 10.1038/194927b0. [DOI] [PubMed] [Google Scholar]
- Boeynaems J. M., Waelbroeck M., Dumont J. E. Cholinergic and alpha-adrenergic stimulation of prostaglandin release by dog thyroid in vitro. Endocrinology. 1979 Oct;105(4):988–995. doi: 10.1210/endo-105-4-988. [DOI] [PubMed] [Google Scholar]
- Boneu B., Sie P., Caranobe C., Nouvel C., Bierme R. Malondialdehyde (MDS) re-appearance in human platelet density subpopulations after a single intake of aspirin. 1980 Aug 15-Sep 1Thromb Res. 19(4-5):609–620. doi: 10.1016/0049-3848(80)90033-x. [DOI] [PubMed] [Google Scholar]
- Buchanan M. R., Rischke J. A., Hirsh J. Aspirin inhibits platelet function independent of the acetylation of cyclo-oxygenase. Thromb Res. 1982 Mar 1;25(5):363–373. doi: 10.1016/0049-3848(82)90127-x. [DOI] [PubMed] [Google Scholar]
- Buchanan M. R., Rischke J. A., Hirsh J. Aspirin inhibits platelet function independent of the acetylation of cyclo-oxygenase. Thromb Res. 1982 Mar 1;25(5):363–373. doi: 10.1016/0049-3848(82)90127-x. [DOI] [PubMed] [Google Scholar]
- Burch J. W., Baenziger N. L., Stanford N., Majerus P. W. Sensitivity of fatty acid cyclooxygenase from human aorta to acetylation by aspirin. Proc Natl Acad Sci U S A. 1978 Oct;75(10):5181–5184. doi: 10.1073/pnas.75.10.5181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano P. M., Smith J. B., Murphy S. Platelet recovery from aspirin inhibition in vivo; differing patterns under various assay conditions. Blood. 1981 Jan;57(1):99–105. [PubMed] [Google Scholar]
- Cerletti C., Livio M., De Gaetano G. Non-steroidal anti-inflammatory drugs react with two sites on platelet cyclo-oxygenase. Evidence from "in vivo" drug interaction studies in rats. Biochim Biophys Acta. 1982 Jan 12;714(1):122–128. doi: 10.1016/0304-4165(82)90133-7. [DOI] [PubMed] [Google Scholar]
- Falardeau P., Oates J. A., Brash A. R. Quantitative analysis of two dinor urinary metabolites of prostaglandin I2. Anal Biochem. 1981 Aug;115(2):359–367. doi: 10.1016/0003-2697(81)90018-x. [DOI] [PubMed] [Google Scholar]
- Feinman R. D., Lubowsky J., Charo I., Zabinski M. P. The lumi-aggregometer: a new instrument for simultaneous measurement of secretion and aggregation by platelets. J Lab Clin Med. 1977 Jul;90(1):125–129. [PubMed] [Google Scholar]
- FitzGerald G. A., Brash A. R., Falardeau P., Oates J. A. Estimated rate of prostacyclin secretion into the circulation of normal man. J Clin Invest. 1981 Nov;68(5):1272–1276. doi: 10.1172/JCI110373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgerald G. A., Maas R. L., Stein R., Oates J. A., Roberts L. J. Intravenous prostacyclin in thrombotic thrombocytopenic purpura. Ann Intern Med. 1981 Sep;95(3):319–322. doi: 10.7326/0003-4819-95-3-319. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick F. A., Gorman R. R., Mc Guire J. C., Kelly R. C., Wynalda M. A., Sun F. F. A radioimmunoassay for thromboxane B2. Anal Biochem. 1977 Sep;82(1):1–7. doi: 10.1016/0003-2697(77)90127-0. [DOI] [PubMed] [Google Scholar]
- Hanley S. P., Bevan J., Cockbill S. R., Heptinstall S. Differential inhibition by low-dose aspirin of human venous prostacyclin synthesis and platelet thromboxane synthesis. Lancet. 1981 May 2;1(8227):969–971. doi: 10.1016/s0140-6736(81)91733-5. [DOI] [PubMed] [Google Scholar]
- Hawiger J., Steckley S., Hammond D., Cheng C., Timmons S., Glick A. D., Des Prez R. M. Staphylococci-induced human platelet injury mediated by protein A and immunoglobulin G Fc fragment receptor. J Clin Invest. 1979 Oct;64(4):931–937. doi: 10.1172/JCI109559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffe E. A., Weksler B. B. Recovery of endothelial cell prostacyclin production after inhibition by low doses of aspirin. J Clin Invest. 1979 Mar;63(3):532–535. doi: 10.1172/JCI109332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins C. S., Meyer D., Dreyfus M. D., Larrieu M. J. Willebrand factor and ristocetin. I. Mechanism of rustocetin-induced platelet aggregation. Br J Haematol. 1974 Dec;28(4):561–578. doi: 10.1111/j.1365-2141.1974.tb06675.x. [DOI] [PubMed] [Google Scholar]
- Moncada S., Gryglewski R., Bunting S., Vane J. R. An enzyme isolated from arteries transforms prostaglandin endoperoxides to an unstable substance that inhibits platelet aggregation. Nature. 1976 Oct 21;263(5579):663–665. doi: 10.1038/263663a0. [DOI] [PubMed] [Google Scholar]
- Morris H. G., Sherman N. A., Shepperdson F. T. Variables associated with radioimmunoassay of prostaglandins in plasma. Prostaglandins. 1981 May;21(5):771–788. doi: 10.1016/0090-6980(81)90234-3. [DOI] [PubMed] [Google Scholar]
- Patrignani P., Filabozzi P., Patrono C. Selective cumulative inhibition of platelet thromboxane production by low-dose aspirin in healthy subjects. J Clin Invest. 1982 Jun;69(6):1366–1372. doi: 10.1172/JCI110576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrono C., Ciabattoni G., Pinca E., Pugliese F., Castrucci G., De Salvo A., Satta M. A., Peskar B. A. Low dose aspirin and inhibition of thromboxane B2 production in healthy subjects. Thromb Res. 1980 Feb 1;17(3-4):317–327. doi: 10.1016/0049-3848(80)90066-3. [DOI] [PubMed] [Google Scholar]
- Preston F. E., Whipps S., Jackson C. A., French A. J., Wyld P. J., Stoddard C. J. Inhibition of prostacyclin and platelet thromboxane A2 after low-dose aspirin. N Engl J Med. 1981 Jan 8;304(2):76–79. doi: 10.1056/NEJM198101083040203. [DOI] [PubMed] [Google Scholar]
- Roberts L. J., 2nd, Sweetman B. J., Oates J. A. Metabolism of thromboxane B2 in man. Identification of twenty urinary metabolites. J Biol Chem. 1981 Aug 25;256(16):8384–8393. [PubMed] [Google Scholar]
- Roth G. J., Majerus P. W. The mechanism of the effect of aspirin on human platelets. I. Acetylation of a particulate fraction protein. J Clin Invest. 1975 Sep;56(3):624–632. doi: 10.1172/JCI108132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuelsson B., Granström E., Green K., Hamberg M., Hammarström S. Prostaglandins. Annu Rev Biochem. 1975;44:669–695. doi: 10.1146/annurev.bi.44.070175.003321. [DOI] [PubMed] [Google Scholar]
- Samuelsson B., Gréen K. Endogenous levels of 15-keto-dihydro-prostaglandins in human plasma. Parameters for monitoring prostaglandin synthesis. Biochem Med. 1974 Nov;11(3):298–303. doi: 10.1016/0006-2944(74)90127-6. [DOI] [PubMed] [Google Scholar]
- Vane J. R. Inhibitors of prostaglandin, prostacyclin, and thromboxane synthesis. Adv Prostaglandin Thromboxane Res. 1978;4:27–44. [PubMed] [Google Scholar]
- Weiss H. J. Platelet physiology and abnormalities of platelet function (first of two parts). N Engl J Med. 1975 Sep 11;293(11):531–541. doi: 10.1056/NEJM197509112931105. [DOI] [PubMed] [Google Scholar]
- Whiting J., Salata K., Bailey J. M. Aspirin: an unexpected side effect on prostacyclin synthesis in cultured vascular smooth muscle cells. Science. 1980 Nov 7;210(4470):663–665. doi: 10.1126/science.6776627. [DOI] [PubMed] [Google Scholar]


