Abstract
Study Design Retrospective clinical study.
Objective To investigate the age-related surgical outcomes of laminoplasty.
Methods One hundred patients who underwent an en bloc laminoplasty for cervical spondylotic myelopathy from 2004 to 2008 and were followed for at least 1 year were included in this study. The clinical outcomes were assessed with the Japanese Orthopaedic Association (JOA) score. Acquired points (postoperative JOA score minus preoperative JOA score) were also calculated. To investigate the age-related effect for laminoplasty, two analyses were conducted: (1) the correlation between age and clinical outcome; and (2) the clinical outcomes by decade. Patients were divided into four groups according to their age at the time of operation as follows: group 50s, 50 to 59 years old; group 60s, 60 to 69 years; group 70s, 70 to 79 years; and group 80s, 80 to 89 years. The pre- and postoperative JOA scores, acquired points, preoperative comorbidities, and postoperative complications were then compared among the groups.
Results Significant correlations were detected between age and JOA scores at the preoperative (p = 0.03), postoperative maximum (p < 0.0001), and final assessments (p < 0.0001). An age-related decline of JOA scores was observed over all periods. The analysis by decades showed the same results. On the other hand, the significant differences were not found for acquired points over all periods by either method. The preoperative comorbidities of hypertension and diabetes mellitus increased with age. Delirium was more common postoperatively in elderly patients.
Conclusions Although an age-related decline of JOA scores was found over all periods, there were no severe sequelae and no differences in the acquired points that were age-related.
Keywords: cervical spondylotic myelopathy, elderly patient, laminoplasty, age-related
Introduction
Cervical laminoplasty is a surgical option for patients with compression myelopathy, such as cervical spondylotic myelopathy (CSM), ossification of the posterior longitudinal ligament (OPLL), and cervical disk herniation (CDH).1 2 3 4 5 6 7 8 9 10 11 12 13 14 As the number of elderly individuals in the population is increasing, surgical treatment for cervical myelopathy in elderly patients is becoming a great concern. Although many authors have reported age-related surgical outcomes for myelopathy due to cervical lesions, there were some limitations in terms of the surgical methods, such as anterior fixation, laminectomy, and laminoplasty,15 16 17 18 19 and different pathologies, such as CSM, OPLL, and CDH.16 17 19 20 Furthermore, some publications have reported the surgical outcomes of cervical laminoplasty for CSM in elderly patients, but their definitions of elderly varied.7 14 21 22 23 24 25 26 No standard definitions of elderly might lead to paradoxical conclusions. In fact, some authors have reported poorer outcomes in elderly patients than in younger patients,26 whereas others found no differences among the age groups.21 23 25 To investigate the age-related surgical outcomes of laminoplasty, analyzing the correlation between age and the clinical outcomes appeared reasonable. Therefore, the purpose of this study was to investigate the age-related surgical outcomes of laminoplasty using two types of analysis without defining elderly.
Materials and Methods
Patient Population
From 2004 to 2008, 124 consecutive laminoplasties for CSM were performed at our institution. One hundred patients (50 to 86 years old) who were followed for at least 1 year were included in this study. The follow-up rate was 81%. Patients with rheumatoid arthritis, hemodialysis, OPLL, psychosis, and other neurogenic diseases were excluded. The patients were divided into four groups according to their age at the time of operation: group 50s, 50 to 59 years old (21 patients); group 60s, 60 to 69 years (32 patients); group 70s, 70 to 79 years (37 patients); and group 80s, 80 to 89 years (10 patients). Patients who were under 50 years old (4 cases) and above 89 years old (2 cases) were excluded. The average age of each group was 56, 64.1, 73.3, and 82.9 years, respectively. The symptom duration was investigated by reviewing the clinical records. The average symptom durations were 3.1, 2.7, 3.9, and 2.1 years, respectively. The average follow-up durations were 4.0, 4.4, 3.8, and 4.5 years, respectively (Table 1). There were no significant differences among these groups in symptom duration and follow-up period.
Table 1. Patient demographic data.
| Group 50s | Group 60s | Group 70s | Group 80s | |
|---|---|---|---|---|
| Number | 21 | 32 | 37 | 10 |
| Age | 56 | 64.1 | 73.3 | 82.9 |
| Male/female | 14/7 | 25/7 | 24/13 | 6/4 |
| Symptom duration (y) | 3.1 | 2.7 | 3.9 | 2.1 |
| F/U (y) | 4.0 | 4.4 | 3.8 | 4.5 |
| HT (%) | 5 (24) | 11 (34) | 20 (54) | 8 (80) |
| DM (%) | 3 (14) | 7 (22) | 12 (32) | 5 (50) |
Abbreviations: DM, diabetes mellitus; HT, hypertension; F/U, follow-up.
Surgical Technique
In this study, all patients underwent an en bloc laminoplasty that was introduced by Itoh and Tsuji.8 The surgical sites were: C3–C5 in 1 case, C3–C6 in 13 cases, C3–C7 in 6 cases, and C4–C7 in 1 case in group 50s; C3–C6 in 24 cases, C3–C7 in 7 cases, and C4–C6 in 1 case in group 60s; C3–C6 in 20 cases, C3–C7 in 12 cases, C3–T1 in 1 case, C4–C7 in 2 cases, C5–C6 in 1 case, and C5–C7 in 1 case in group 70s; and C3–C6 in 9 cases and C3–C7 in 1 case in group 80s. After surgery, the patients wore a soft cervical collar, which they were allowed to remove within a week. The mean operation time was 119 minutes (group 50s, 128 minutes; group 60s, 118 minutes; group 70s, 116 minutes; and group 80s, 115 minutes), and the mean estimated blood loss during the laminoplasty was 153 mL (group 50s, 108 mL; group 60s, 164 mL; group 70s, 164 mL; and group 80s, 173 mL). There were no significant differences among these groups in the operation time and blood loss (data not shown).
Clinical Assessment
The clinical outcomes were assessed using the scoring system proposed by the Japanese Orthopaedic Association (JOA). Briefly, the JOA score consists of upper extremity function (4 points), lower extremity function (4 points), sensory (6 points), and urinary bladder function (3 points). A normal JOA score was 17 points.
The clinical assessments were performed for all patients before surgery; at 1, 6, and 12 months after surgery; and then annually thereafter. The acquired points were also calculated in each period. Furthermore, the preoperative comorbidities and postoperative complications were investigated.
Statistical Analysis
To investigate the correlations between age and the clinical outcomes, the Spearman rank correlation coefficient was used for each factor. Values of p < 0.05 indicated significance. The Bonferroni test was performed for analyzing the differences among the four groups. Values of p < 0.005/6 = 0.0083 indicated significance for this analysis.
Results
Age and JOA Scores
Significant negative correlations were detected between age and the total JOA scores at the preoperative (p = 0.03), postoperative maximum (p < 0.0001), and final assessments (p < 0.0001; Fig. 1). For the upper extremity function, significant negative correlations were also detected between age and the JOA scores at the preoperative (p = 0.0028), postoperative maximum (p < 0.0001), and final assessments (p = 0.0002; data not shown). Similarly, with regard to the lower extremity function, significant negative correlations were detected between age and the JOA scores of the lower extremities at the preoperative (p = 0.0037), postoperative maximum (p = 0.0003), and final assessments (p = 0.0004; data not shown). In terms of the analysis by decade, the average total JOA scores at the preoperative, postoperative maximum, and final assessments were 9.7, 14.5, and 14.1 points in group 50s; 9.1, 13.8, and 13.1 points in group 60s; 7.9, 12.3, and 11.6 points in group 70s; and 8.2, 11.5, and 11.1 points in group 80s, respectively (Fig. 2). Although no significant differences were detected in the preoperative JOA scores between the groups, those at the postoperative maximum and final assessments of groups 70s and 80s were significantly lower than those of groups 50s and 60s. Regarding the upper extremity function, the average JOA scores at the preoperative, postoperative maximum, and final assessments were 2.5, 3.6, and 3.5 points in group 50s; 2.0, 3.3, and 3.1 points in group 60s; 1.7, 3.0, and 2.8 points in group 70s; and 1.5, 2.8, and 2.7 points in group 80s, respectively (Fig. 2). The average JOA scores of the upper extremities at the preoperative, postoperative maximum, and final assessments were significantly lower for group 70s and 80s than for group 50s. With regard to lower extremity function, the average JOA scores at the preoperative, postoperative maximum, and final assessments were 1.8, 2.9, and 2.8 points in group 50s; 1.7, 3.0, and 2.6 points in group 60s; 1.3, 2.3, and 2.1 points in group 70s; and 1.1, 1.9, and 1.8 points in group 80s, respectively (Fig. 2). Although no significant differences were detected in the preoperative JOA scores between the groups, those at the postoperative maximum were significantly lower for groups 70s and 80s than for groups 50s and 60s, and those at the final assessments were significantly lower for groups 70s and 80s than for group 50s.
Fig. 1.
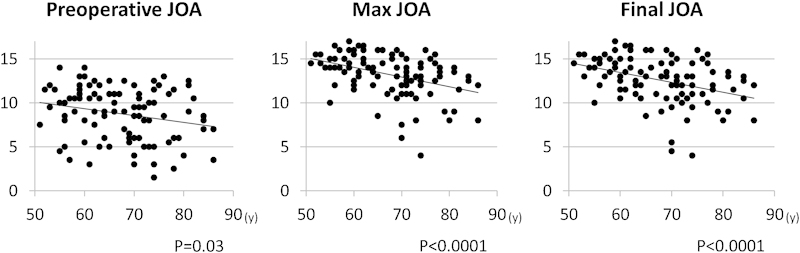
Spearman rank correlation coefficient between age and Japanese Orthopaedic Association (JOA) score.
Fig. 2.
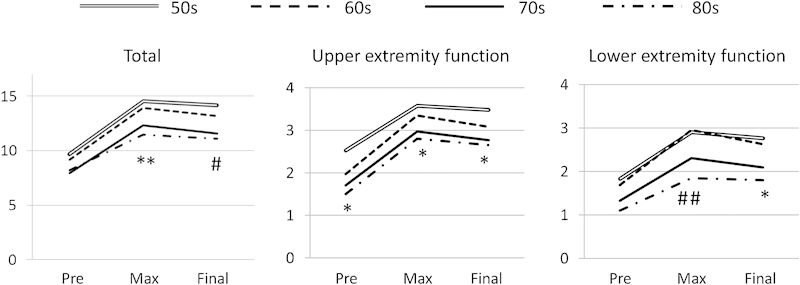
Japanese Orthopaedic Association score. *Group 50s versus group 70s, group 50s versus group 80s: p < 0.0083. **Group 50s versus group 70s, group 50s versus group 80s, group 60s versus group 70s, group 60s versus group 80s: p < 0.0083. #Group 50s versus group 70s, group 50s versus group 80s, group 60s versus group 70s: p < 0.0083. ##Group 50s versus group 80s, group 60s versus group 70s, group 60s versus group 80s: p < 0.0083.
Age and Acquired Points
No correlations were detected between age and the acquired points in each category through all periods (data not shown). In terms of the analysis by decade, the average total acquired points at the postoperative maximum and final assessments were 4.8 and 4.5 in group 50s, 4.8 and 4.0 in group 60s, 4.4 and 3.6 in group 70s, and 3.1 and 2.9 in group 80s, respectively (Fig. 3). Regarding the upper extremity function, the average acquired points at the postoperative maximum and final assessments were 1.0 and 1.0 in group 50s, 1.4 and 1.1 in group 60s, 1.3 and 1.1 in group 70s, and 1.3 and 1.2 in group 80s, respectively. With regard to the lower extremity function, the average acquired points at the postoperative maximum and final assessments were 1.1 and 0.9 in group 50s, 1.3 and 0.9 in group 60s, 1.0 and 0.8 in group 70s, and 0.8 and 0.7 in group 80s, respectively (Fig. 3). Although there were no significant differences in acquired points between the groups in each category through all the periods, the acquired points of the lower extremities tended to be low in groups 70s and 80s.
Fig. 3.
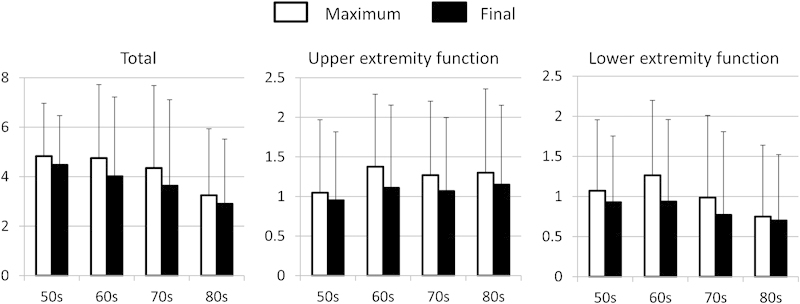
Acquired points (p = not significant).
Preoperative Comorbidities and Postoperative Complications
In terms of the preoperative comorbidities, hypertension was observed in 5 patients (24%) in group 50s, 11 (34%) in group 60s, 20 (54%) in group 70s, and 8 (80%) in group 80s, and diabetes mellitus was detected in 3 patients (14%) in group 50s, 7 (22%) in group 60s, 12 (32%) in group 70s, and 5 (50%) in group 80s (Table 1). In the patients with hypertension (HT+), the average JOA scores at the preoperative, postoperative maximum, and final assessments were 7.9, 12.5, and 11.8 points, respectively. And in the patients without hypertension (HT−), they were 9.3, 13.7, and 13.1 points, respectively. The average acquired points at the postoperative maximum and final assessments were 4.6 and 4.0 in HT+ patients and 4.3 and 3.7 in HT− patients, respectively. Although the average JOA scores at the preoperative, postoperative maximum, and final assessments were significantly lower for HT+ patients than for HT− patients, no significant difference was detected in the average acquired points at the postoperative maximum and final assessments. In the patients with diabetes mellitus (DM+), the average JOA scores at the preoperative, postoperative maximum, and final assessments were 7.9, 11.7, and 11 points, respectively. And in the patients without diabetes mellitus (DM−), they were 9.0, 13.1, and 13.7 points, respectively. The average acquired points at the postoperative maximum and final assessments were 3.8 and 3.1 in DM+ patients and 4.7 and 4.1 in DM− patients, respectively. Although the average JOA scores at the postoperative maximum and final assessments were significantly lower for DM+ patients than for DM− patients, no significant differences were detected in the average preoperative JOA score or average acquired points at the postoperative maximum and final assessments.
Regarding the postoperative complications, C5 nerve palsy was observed in 1 patient each in groups 50s (4.8%), 70s (2.7%), and 80s (10%) and 2 in group 60s (6.3%). Delirium was observed 3 (8%) in group 70s and 2 (20%) in group 80s. One patient in group 60s had a cerebral infarction (3.1%). There were no surgical site infections in this series (Table 2).
Table 2. Postoperative complications.
| Group 50s | Group 60s | Group 70s | Group 80s | |
|---|---|---|---|---|
| C5 palsy (%) | 1 (4.8) | 2 (6.3) | 1 (2.7) | 1 (10) |
| Delirium (%) | 0 | 0 | 3 (8.1) | 2 (20) |
| Cerebral infarction (%) | 0 | 1 (3.1) | 0 | 0 |
| SSI | 0 | 0 | 0 | 0 |
Abbreviation: SSI, surgical site infection.
Discussion
Cervical laminoplasty is a well-reported surgical treatment for cervical myelopathy with CSM, OPLL, and CDH. The long-term clinical and radiologic results of laminoplasty have been investigated, and the risk factors for poor outcomes (age at the time of operation, symptom duration, signal changes in the spinal cord on magnetic resonance imaging, transverse area of the spinal cord at the site of maximum compression, and kyphotic alignment) have been identified.19 20 21 25
In terms of age-related effects on laminoplasty, many authors have reported comparative studies of the surgical outcomes in elderly patients, but their conclusions were controversial because their definitions of elderly varied from 65 to 80 years.7 14 21 22 23 24 25 26 Therefore, in the present study, the surgical outcomes of laminoplasty were examined in two ways: (1) the Spearman rank correlation coefficient between age and clinical outcome; and (2) the surgical outcomes by decade without a definition of elderly.
In the present study, a negative correlation was detected between age and preoperative JOA scores, but the decade classification did not show a significant difference. Furthermore, the postoperative JOA scores decreased significantly with aging. Symptom duration has often been discussed as one of the causes of the poor preoperative condition in elderly patients. Several authors have reported that long symptom duration contributed to the poor surgical outcomes of laminoplasty, especially in elderly patients.19 21 25 Generally, surgeons hesitate to operate on elderly patients due to their comorbidities; however, in the acquired points, there were no significant difference between the patients with or without comorbidities in the present study. Delaying surgical treatment for elderly patients causes prolonged symptom duration, and severe myelopathy may develop. Nagata et al recommended that the surgical treatment be done as soon as possible after onset of progressive myelopathy in elderly patients.19 Moreover, Matsunaga et al reported that the neurologic function deteriorated with increasing age in healthy volunteers.27 The age-related degeneration of the spinal cord, such as a decrease in the number of anterior horn cells and myelinated fibers in the corticospinal tracts and posterior funiculus, might contribute to the preoperative and postoperative status.28 29 30 For these reasons, we chose to operate on elderly patients as soon as possible, and there were no significant differences in symptom duration among the decades in the present series.
On the other hand, no correlation was seen between age and acquired points in each category through all periods. Similarly, the analysis by decade showed the same results. In the present study, the acquired points of the lower extremity tended to be low in groups 70s and 80s, and those of the upper extremity did not show any difference among the decades.
Machino et al pointed out one limitation of the recovery rate of the JOA score: the actual surgical outcomes in patients with the same recovery rate might differ according to the preoperative JOA score.24 Patients with low preoperative JOA scores had poorer surgical outcomes than patients with high preoperative JOA scores, though both of them achieved the same JOA score. They recommended that acquired points should be used for evaluation of elderly patients rather than the recovery rate. Therefore, in the present study, the recovery rate was not calculated, and acquired points were considered for evaluation of surgical outcomes.
One limitation of this study was that the radiologic examinations were not evaluated. Further studies will be necessary to clarify the relationship between the age-related radiologic features and the clinical outcomes. However, to the best of our knowledge, this is the first report of an age-related decline of pre- and postoperative clinical status without defining elderly.
In conclusion, although an age-related decline of JOA scores was detected in all periods, there were no severe sequelae and no differences in the acquired points related to age. These results suggest that laminoplasty for cervical myelopathy is useful in elderly patients.
Acknowledgments
The authors thank the Investigation Committee on the Ossification of the Spinal Ligaments of the Japanese Ministry of Health, Labor, and Welfare.
Footnotes
Disclosures Takafumi Maeno, none Shinya Okuda, none Tomoya Yamashita, none Tomiya Matsumoto, none Ryoji Yamasaki, none Takenori Oda, none Motoki Iwasaki, none
References
- 1.Chiba K, Ogawa Y, Ishii K. et al. Long-term results of expansive open-door laminoplasty for cervical myelopathy—average 14-year follow-up study. Spine (Phila Pa 1976) 2006;31(26):2998–3005. doi: 10.1097/01.brs.0000250307.78987.6b. [DOI] [PubMed] [Google Scholar]
- 2.Fehlings M G, Wilson J R, Kopjar B. et al. Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: results of the AOSpine North America prospective multi-center study. J Bone Joint Surg Am. 2013;95(18):1651–1658. doi: 10.2106/JBJS.L.00589. [DOI] [PubMed] [Google Scholar]
- 3.Fukui K, Kataoka O, Sho T, Sumi M. Pathomechanism, pathogenesis, and results of treatment in cervical spondylotic myelopathy caused by dynamic canal stenosis. Spine (Phila Pa 1976) 1990;15(11):1148–1152. doi: 10.1097/00007632-199011010-00012. [DOI] [PubMed] [Google Scholar]
- 4.Hase H, Watanabe T, Hirasawa Y. et al. Bilateral open laminoplasty using ceramic laminas for cervical myelopathy. Spine (Phila Pa 1976) 1991;16(11):1269–1276. doi: 10.1097/00007632-199111000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Hirabayashi K, Satomi K. Operative procedure and results of expansive open-door laminoplasty. Spine (Phila Pa 1976) 1988;13(7):870–876. doi: 10.1097/00007632-198807000-00032. [DOI] [PubMed] [Google Scholar]
- 6.Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976) 1983;8(7):693–699. doi: 10.1097/00007632-198310000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Ishii M, Wada E, Ishii T, Kawai H, Kaneko N, Fuji T. Laminoplasty for patients aged 75 years or older with cervical myelopathy. J Orthop Surg (Hong Kong) 2008;16(2):211–214. doi: 10.1177/230949900801600217. [DOI] [PubMed] [Google Scholar]
- 8.Itoh T, Tsuji H. Technical improvements and results of laminoplasty for compressive myelopathy in the cervical spine. Spine (Phila Pa 1976) 1985;10(8):729–736. doi: 10.1097/00007632-198510000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Kawaguchi Y, Kanamori M, Ishihara H, Ohmori K, Nakamura H, Kimura T. Minimum 10-year followup after en bloc cervical laminoplasty. Clin Orthop Relat Res. 2003;(411):129–139. doi: 10.1097/01.blo.0000069889.31220.62. [DOI] [PubMed] [Google Scholar]
- 10.Kawai S, Sunago K, Doi K, Saika M, Taguchi T. Cervical laminoplasty (Hattori's method). Procedure and follow-up results. Spine (Phila Pa 1976) 1988;13(11):1245–1250. [PubMed] [Google Scholar]
- 11.Kimura I, Shingu H, Nasu Y. Long-term follow-up of cervical spondylotic myelopathy treated by canal-expansive laminoplasty. J Bone Joint Surg Br. 1995;77(6):956–961. [PubMed] [Google Scholar]
- 12.Lee T T, Green B A, Gromelski E B. Safety and stability of open-door cervical expansive laminoplasty. J Spinal Disord. 1998;11(1):12–15. [PubMed] [Google Scholar]
- 13.Seichi A, Takeshita K, Ohishi I. et al. Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine (Phila Pa 1976) 2001;26(5):479–487. doi: 10.1097/00007632-200103010-00010. [DOI] [PubMed] [Google Scholar]
- 14.Suzuki A, Misawa H, Simogata M, Tsutsumimoto T, Takaoka K, Nakamura H. Recovery process following cervical laminoplasty in patients with cervical compression myelopathy: prospective cohort study. Spine (Phila Pa 1976) 2009;34(26):2874–2879. doi: 10.1097/BRS.0b013e3181bb0e33. [DOI] [PubMed] [Google Scholar]
- 15.Hasegawa K, Homma T, Chiba Y, Hirano T, Watanabe K, Yamazaki A. Effects of surgical treatment for cervical spondylotic myelopathy in patients > or = 70 years of age: a retrospective comparative study. J Spinal Disord Tech. 2002;15(6):458–460. doi: 10.1097/00024720-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Matsuda Y, Shibata T, Oki S, Kawatani Y, Mashima N, Oishi H. Outcomes of surgical treatment for cervical myelopathy in patients more than 75 years of age. Spine (Phila Pa 1976) 1999;24(6):529–534. doi: 10.1097/00007632-199903150-00005. [DOI] [PubMed] [Google Scholar]
- 17.Nagashima H, Morio Y, Yamashita H, Yamane K, Teshima R. Clinical features and surgical outcomes of cervical myelopathy in the elderly. Clin Orthop Relat Res. 2006;(444):140–145. doi: 10.1097/01.blo.0000201156.21701.86. [DOI] [PubMed] [Google Scholar]
- 18.Nagashima H, Dokai T, Hashiguchi H. et al. Clinical features and surgical outcomes of cervical spondylotic myelopathy in patients aged 80 years or older: a multi-center retrospective study. Eur Spine J. 2011;20(2):240–246. doi: 10.1007/s00586-010-1672-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nagata K, Ohashi T, Abe J, Morita M, Inoue A. Cervical myelopathy in elderly patients: clinical results and MRI findings before and after decompression surgery. Spinal Cord. 1996;34(4):220–226. doi: 10.1038/sc.1996.41. [DOI] [PubMed] [Google Scholar]
- 20.Satomi K, Nishu Y, Kohno T, Hirabayashi K. Long-term follow-up studies of open-door expansive laminoplasty for cervical stenotic myelopathy. Spine (Phila Pa 1976) 1994;19(5):507–510. doi: 10.1097/00007632-199403000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Handa Y, Kubota T, Ishii H, Sato K, Tsuchida A, Arai Y. Evaluation of prognostic factors and clinical outcome in elderly patients in whom expansive laminoplasty is performed for cervical myelopathy due to multisegmental spondylotic canal stenosis. A retrospective comparison with younger patients. J Neurosurg. 2002;96(2):173–179. doi: 10.3171/spi.2002.96.2.0173. [DOI] [PubMed] [Google Scholar]
- 22.Ishii M, Wada E, Hamada M. Deterioration of surgical outcomes with aging in patients with cervical spondylotic myelopathy. J Spinal Disord Tech. 2012;25(7):E199–E203. doi: 10.1097/BSD.0b013e318246af8b. [DOI] [PubMed] [Google Scholar]
- 23.Kawaguchi Y, Kanamori M, Ishihara H, Ohmori K, Abe Y, Kimura T. Pathomechanism of myelopathy and surgical results of laminoplasty in elderly patients with cervical spondylosis. Spine (Phila Pa 1976) 2003;28(19):2209–2214. doi: 10.1097/01.BRS.0000085029.65713.B0. [DOI] [PubMed] [Google Scholar]
- 24.Machino M, Yukawa Y, Hida T. et al. Can elderly patients recover adequately after laminoplasty? A comparative study of 520 patients with cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2012;37(8):667–671. doi: 10.1097/BRS.0b013e31823147c9. [DOI] [PubMed] [Google Scholar]
- 25.Tanaka J, Seki N, Tokimura F, Doi K, Inoue S. Operative results of canal-expansive laminoplasty for cervical spondylotic myelopathy in elderly patients. Spine (Phila Pa 1976) 1999;24(22):2308–2312. doi: 10.1097/00007632-199911150-00004. [DOI] [PubMed] [Google Scholar]
- 26.Yamazaki T Yanaka K Sato H Uemura K Tsukada A Nose T Cervical spondylotic myelopathy: surgical results and factors affecting outcome with special reference to age differences Neurosurgery 2003521122–126., discussion 126 [DOI] [PubMed] [Google Scholar]
- 27.Matsunaga S, Koga K, Komiya S. Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ) investigation in healthy volunteers. J Spine Spinal Cord. 2010;23:189–193. [Google Scholar]
- 28.Terao S, Sobue G, Hashizume Y, Shimada N, Mitsuma T. Age-related changes of the myelinated fibers in the human corticospinal tract: a quantitative analysis. Acta Neuropathol. 1994;88(2):137–142. doi: 10.1007/BF00294506. [DOI] [PubMed] [Google Scholar]
- 29.Zhang C, Goto N, Zhou M. Morphometric analyses and aging process of nerve fibers in the human spinal posterior funiculus. Okajimas Folia Anat Jpn. 1995;72(5):259–264. doi: 10.2535/ofaj1936.72.5_259. [DOI] [PubMed] [Google Scholar]
- 30.Zhang C, Goto N, Suzuki M, Ke M. Age-related reductions in number and size of anterior horn cells at C6 level of the human spinal cord. Okajimas Folia Anat Jpn. 1996;73(4):171–177. doi: 10.2535/ofaj1936.73.4_171. [DOI] [PubMed] [Google Scholar]


