Abstract
Study Design Systematic literature review and meta-analysis.
Objective This study is a meta-analysis assessing the fusion rate and the clinical outcomes of cervical pseudarthrosis treated with either a posterior or a revision anterior approach.
Methods A literature search of PubMed, Cochrane, and Embase was performed. Variables of interest included fusion rate and clinical success. The effect size based on logit event rate was calculated from the pooled results. The studies were weighted by the inverse of the variance, which included both within- and between-study error. The confidence intervals were reported at 95%. Heterogeneity was assessed using the Q statistic and I 2, where I 2 is the estimate of the percentage of error due to between-study variation.
Results Sixteen studies reported fusion outcomes; 10 studies reported anterior and/or posterior results. The pooled fusion success was 86.4% in the anterior group and 97.1% in the posterior group (p = 0.028). The anterior group demonstrated significant heterogeneity with Q value of 34.2 and I 2 value of 73.7%; no heterogeneity was seen in the posterior group. The clinical outcomes were reported in 10 studies, with eight reporting results of anterior and posterior approaches. The pooled clinical success rate was 77.0% for anterior and 71.7% for posterior (p = 0.55) approaches. There was significant heterogeneity in both groups (I 2 16.1; 19.2).
Conclusions Symptomatic cervical pseudarthrosis can be effectively managed with either an anterior or a posterior approach. The posterior approach demonstrates a significantly greater fusion rate compared with the anterior approach, though the clinical outcome does not differ between the two groups.
Keywords: cervical spine, pseudarthrosis, nonunion, anterior cervical diskectomy and fusion, ACDF, posterior cervical fusion, iliac crest bone graft, exploration of pseudarthrosis, meta-analysis
Introduction
Anterior cervical diskectomy and fusion (ACDF) is a frequently utilized procedure for the treatment of cervical degenerative disk disease that is refractory to conservative management. Long accepted as the gold standard for the treatment of neurologic deficits and radiculopathy associated with degenerative disease in the cervical spine, ACDF is generally associated with a high clinical success rate.1 2 3 4 5 Despite the proven long-term clinical and radiographic success, ACDF is associated with certain disadvantages, including the loss of motion segments, the potential for accelerated adjacent segment disease, and the reliance on the need for solid bony fusion.6 7 8 9 10 11
The nonunion rates after ACDF can vary based on the number of levels fused, the type of allograft used, and the surgical technique. The pseudarthrosis rates can range from 0 to 20% in single-level ACDF to over 60% in multilevel fusions.12 13 14 15 16 17 The treatment of a symptomatic pseudarthrosis can be accomplished either through a revision anterior procedure or via a posterior approach. To date, there remains considerable debate in the literature as to the optimal method for the treatment of pseudarthrosis. There are no randomized control trials directly comparing the outcomes following treatment of pseudarthrosis.
The purpose of this study is to perform a meta-analysis to compare fusion and clinical success in the treatment of pseudarthrosis between the anterior and posterior approaches.
Materials and Methods
Inclusion and Exclusion Criteria and Review Procedure
A systematic computerized Medline literature search was performed using PubMed, Cochrane Database of Systematic Reviews, and EMBASE. The electronic databases were searched for articles published from January 1980 to December 2013. The searches were performed with Medical Subject Headings (MeSH) used by the National Library of Medicine. Specifically, MeSH terms “cervical pseudoarthrosis,” “cervical nonunion,” “anterior cervical discectomy and fusion (ACDF),” and “posterior cervical fusion” were used. In PubMed, a clinical queries filter was used to delineate only those studies of English language, in adult patients, and with an available abstract. Inclusion criteria in the meta-analysis were: adult patient, subaxial spine, failed anterior cervical fusion, 6-month's follow-up, and a minimum of 10 patients for a given study.
The abstracts of each article were reviewed by two independent authors to assess for inclusion in the meta-analysis. The authors then jointly reviewed the full text of the articles meeting criteria based on the abstract to determine agreement on the inclusion of the studies. In case of a discrepancy, a third author participated in the discussion until a consensus was reached. The methodological quality of each included study was appraised and scored in accordance with the Oxford Levels of Evidence 2.
Data Extraction
A meta-analysis database was created from included studies with the following categories: (1) study ID to include author, journal, and year of publication; (2) reference; (3) study type and level of evidence; (4) study inclusion and exclusion criteria; (5) number of patients; (6) male-to-female ratio; (7) patient age; (8) length of follow-up; (9) number and level of pseudarthroses; (10) secondary operative intervention; (11) fusion success; and (12) clinical success (Table 1). The primary outcomes variables were fusion success and clinical success using Odom's or Prolo criteria. Clinical success was converted into a binary variable with excellent/good equaling success and fair/poor equaling failure.
Table 1. Summary of clinical data from included studies.
| Study, first author and year | Number of patients | Age of patients (y) | Duration of follow-up after revision (mo) | Secondary intervention | Fusion success (binary) | Clinical success (binary) |
|---|---|---|---|---|---|---|
| Brodsky, 199213 | 34 | 47 (31–72) | 60 | 17 ACDF with ICBG without plate; 17 posterior wiring with ICBG | 13/17 anterior (76%); 16/17 posterior (94%) | 10/17 anterior (59%); 15/17 posterior (88%) |
| Carreon, 200619 | 120 (27 anterior, 93 posterior) | Not detailed | 42 (24–132); 52 (24–120) | 27 ACDF with plate and ICBG; 93 posterior fusion | Anterior: 15/27 (56%); posterior: 91/93 (98%) | Not detailed |
| Caspar, 199921 | 37 | 47 (30–66) | 24.7 (20–112) | All with revision ACDF with plate and ICBG | 37/37 (100%) | 31/37 (84%) |
| Coric, 199718 | 19 | 49 (25–72) | 22 (12–42) | All with revision ACDF with plate and allograft | 19/19 (100%) | 15/18 (83%) |
| Farey, 199022 | 19 | 45 (23–57) | 44 (24–54) | All with posterior wiring with ICBG | 19/19 (100%) | Not detailed |
| Gore, 200334 | 25 | Not detailed | 60 (12–168) | All with posterior wiring with ICBG | 25/25 | Not detailed |
| Kuhns, 200523 | 36 (3 lost to follow up) | 47 (28–63) | 46 (20–86) | 17 one-level PCF (6 at C5–C6, 11 at C6–C7), 9 two-level (2 at C4–C6, 7 at C5–C7), 6 three-level (1 at C3–C6, 4 at C4–C7, 1 at C5–T1), 1 four-level (C3–C7) | 33/33 (100%) | 25/33 (72%) |
| Liu, 201224 | 38 | 45 (24–60) | 28 (24–60) | 38 PCF with lateral mass screws | 38/38 (100%) | 32/38 (84%) |
| Lowery, 199520 | 37 (44 procedures) | 47 (18–79) | 28 (12–60) | 20 ACDF with plate (7 ICBG, 13 allo); 17 posterior plating (10 local auto, 2 ICBG, 5 allo) | 9/20 anterior (45%); 16/17 posterior (94%); 7/7 circumferential (100%) | 8/20 anterior (40%); 14/17 posterior (82%); 5/7 circumferential (71%) |
| Mutoh, 199325 | 15 | 56 (36–74) | 27 (16–86) | 12 posterior wiring with ICBG; 2 posterior plating with ICBG (1 fused C1–C7 for multilevel instability); 1 ACDF with ICBG | 15/15 (100%) | 5 of 15 were symptomatic preoperatively; 4/5 recovered completely after |
| Newman, 199331 | 16 | 40 | Not detailed | 16 revision ACDF | 13/16 (81.2) | 5/7 (71.4%) |
| Phillips, 199726 | 48 (32 symptomatic, 22 had revision) | 46 (29–75) | 32 (minimum 12) | 16 ACDF with ICBG without plate; 6 posterior wiring with ICBG | 14/16 anterior (88%); 6/6 posterior (100%) | 14/16 anterior (88%); 6/6 posterior (100%) |
| Siambanes, 199827 | 14 | 43 (33–52) | 42 (6–126) | All with posterior wiring with ICBG | 14/14 (100%) | Not detailed |
| Toohey, 200630 | 18 | All with posterior Halifax clamp fixation | 18/18 | Not detailed | ||
| Tribus, 199928 | 16 | 42 (33–62) | 19.2 (43–61) | All with revision ACDF with plate and ICBG | Grade 1: 10/16; grade 2: 3/16; grade 3: 2/16; grade IV: 1/16 | 13/16 (81%) |
| Zdeblick, 199729 | 23 | 50 (31–63) | 44 (24–216) | 20 ACDF with ICBG without plate; 3 ACCF with autograft fibula strut | 23/23 (100%) | 20/23 (87%) |
Abbreviations: ACCF, anterior cervical corpectomy and fusion; ACDF, anterior cervical diskectomy and fusion; allo, allograft auto, autograft; ICBG, iliac crest bone graft; PCF, posterior cervical fusion.
Meta-Analysis Methods
The pooled results were performed by calculating the effect size based on logit event rate using Comprehensive Meta Analysis, version 2.2.050 (Biostat, Englewood, New Jersey, United States). The studies were weighted in the meta-analysis by the inverse of the variance, which included both within- and between-study error. The effect size and confidence intervals were reported using Forest plots. The confidence intervals (CIs) were reported at 95% levels. The comparison between the groups was performed using the Z distribution and a t test or, for multiple groups, analysis of variance. A p value of 0.05 was set for significance. Heterogeneity was assessed using the Q statistic and I 2, where I 2 is the estimate of the percentage of error due to between-study variation. I 2 values below 25% generally indicate consistent results and homogeneous studies. We selected an a priori random effects model.
The sensitivity analysis was performed by varying the assumptions used in the meta-analysis and by single elimination of the studies from the three institutions with at least four separate control treatment arms. The funnel plots of effect size versus standard error were assessed by visual inspection to determine publication bias.
Results
Systematic Review
The initial PubMed, Embase, and Cochrane Review search resulted in 281 articles. After assessment by two reviewers, 20 articles were identified that met inclusion criteria. Three studies were excluded for an insufficient number of cases or a poor study design. All the studies were level IV evidence. Descriptive information for the studies is given in Table 1. Overall, 217 patients were treated anteriorly and 280 patients posteriorly; patients had a mean age of 46.9 years. Of the patients, 47.9% were male, and the mean clinical follow-up averaged 40.6 months.
Sixteen studies reported fusion outcomes.13 18 19 20 21 22 23 24 25 26 27 28 29 An anterior approach was performed in 10 studies. Similarly, a posterior approach was utilized in 10 studies. Three studies reported the subgroups of both the anterior and posterior approaches. One of these studies also reported a third treatment arm of a combined anterior-posterior approach; however, this was not included in the statistical analysis.
Summary of Investigations
Coric et al performed revision ACDF with an iliac crest bone graft (ICBG) in 19 patients.18 At an average follow-up of 22.4 months, 19 of 19 patients (100%) had radiographic evidence of fusion and 15 of 18 patients (83%) were deemed to have clinical success. Carreon et al performed a retrospective case series of 120 patients with symptomatic pseudarthrosis; 27 had repeat anterior procedures and 93 had posterior procedures.19 In the anterior revision group, 12 of 27 patients (44%), and in the posterior revision group, 2 of 93 patients (2%) required a second revision surgery for persistent nonunion. Lowery et al reported on a retrospective review of 20 patients treated with an anterior revision, 17 patients with a posterior fusion, and 7 patients with a circumferential fusion.20 All 7 patients (100%) with a circumferential fusion achieved solid fusion, 16 of 17 patients (94%) with posterior repairs achieved solid fusion, and only 45% of the anteriorly treated patients achieved solid fusion.
Caspar and Pitzen retrospectively reviewed 41 patients who underwent revision ACDF with ICBG via an anterior approach.21 Thirty-seven patients were available for an average follow-up of 24.7 months, with all 37 (100%) demonstrating radiographic evidence of fusion. Clinical success was achieved in 31/37 (84%) of patients. Farey et al reported on 19 consecutive patients who had a symptomatic pseudarthrosis after a failed anterior cervical arthrodesis treated by posterior nerve-root decompression and arthrodesis.22 A solid fusion was achieved in all patients, and the radiculopathy was relieved in all but one. Kuhns et al reviewed 33 patients with symptomatic pseudarthrosis following ACDF treated with selective nerve root decompression and posterior fusion using an iliac crest or a local bone graft as well as posterior wiring and/or lateral mass plating.23 All 33 patients (100%) demonstrated a solid fusion at their most recent follow-up, and all 33 patients noted a significant improvement in their preoperative symptoms.
Liu et al performed a retrospective review of 38 consecutive patients with pseudarthrosis treated with revision posterior cervical fusion. All patients achieved a solid radiographic fusion at the final follow-up.24 The result was excellent in 10 patients, good in 22, fair in 6, and poor in none. Mutoh et al reported on 14 patients with symptomatic pseudarthrosis treated with posterior cervical fusion with ICBG.25 All 14 patients (100%) went on to radiographic fusion. Phillips et al reviewed 22 patients with symptomatic pseudarthrosis; 16 underwent revision ACDF with ICBG and 6 underwent posterior cervical fusion with ICBG.26 Of the patients in the revision ACDF group, 14 of 16 (88%) went on to radiographic fusion with clinical success observed in all 14. The posterior group had 6 of 6 patients (100%) achieve clinical and fusion success.
Siambanes and Miz reported on 14 patients treated with posterior stabilization after failed ACDF. Radiographic union was achieved in all patients (100%).27 Tribus et al performed a retrospective review of 16 consecutive patients treated with an anterior resection of the pseudarthrosis, autogenous ICBG, and stabilization with an anterior cervical plate.28 Overall, 13 of 16 patients (83%) achieved clinical and fusion success at an average follow-up of 19.2 months. Zdeblick et al retrospectively reviewed 23 patients treated with a revision anterior procedure for pseudarthrosis.29 All 23 (100%) went on to fusion, and 20 of the 23 (87%) were graded as having clinical success.
Toohey et al reviewed 18 cases of pseudarthrosis treated with posterior fusion with ICBG.30 All patients (100%) demonstrated radiographic evidence of fusion. Brodsky et al reviewed 34 patients with pseudarthrosis, with an anterior revision performed in 17 and a posterior revision performed in 17.13 The anterior group achieved a 76% rate of fusion, and the posterior group had a 94% rate of fusion. Excellent or good results were achieved in 59% of the anterior revision and 88% of the posterior fusion group. Newman reported on 16 patients who underwent revision ACDF with ICBG; 13 of 16 (81.2%) achieved fusion and 5 of 7 (71.4) reported clinical success.31
Meta-Analysis Results
Fusion Success
Ten studies reported anterior fusion results, and 10 studies reported posterior fusion results. Four studies reported cohorts of both anterior and posterior approaches. The pooled fusion success was 86.4% (CI: 71.4, 94.2) in the anterior group (Fig. 1) and 97.1% in the posterior (CI: 94.3, 98.6) group (Table 2). The difference between the two groups was statistically significant (p = 0.028). The anterior groups demonstrated significant heterogeneity with a Q value of 34.2 and an I 2 value of 73.7%. There was no heterogeneity in the posterior group with a Q value of 1.94 and an I 2 value of 0.0%. This indicates that significant differences in the fusion rates were present in the anterior approach, and the posterior group demonstrated much more consistent results.
Fig. 1.
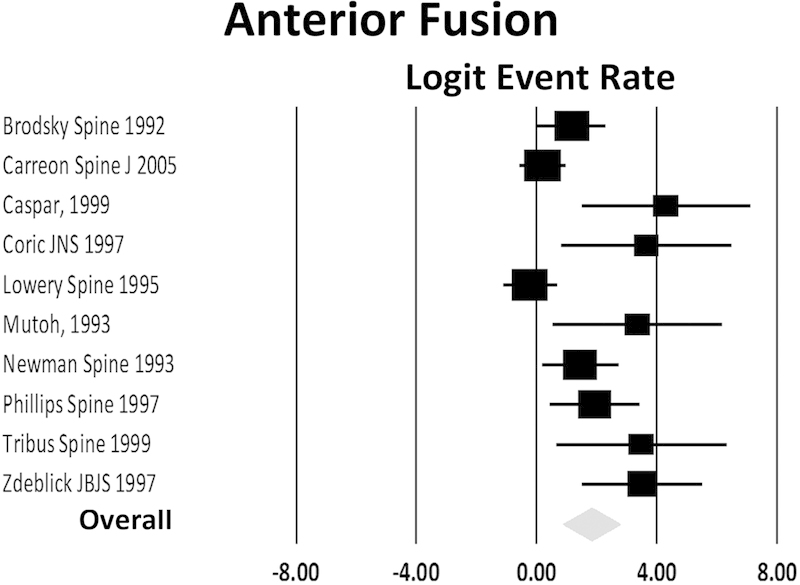
Forest plot of the logit event rate for fusion success with anterior surgery.
Table 2. Effect of surgical technique on fusion success.
| Anterior | Posterior | |||||||
|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | |||||||
| Study, first author and year | n | Fusion success | Lower | Upper | n | Fusion success | Lower | Upper |
| Brodsky, 199213 | 17 | 0.76 | 0.51 | 0.91 | 17 | 0.94 | 0.68 | 0.99 |
| Carreon, 200619 | 27 | 0.56 | 0.37 | 0.73 | 93 | 0.98 | 0.92 | 0.99 |
| Caspar, 199921 | 37 | 0.99 | 0.82 | 0.99 | – | – | – | – |
| Coric, 199718 | 19 | 0.96 | 0.70 | 0.99 | – | – | – | – |
| Farey, 199022 | – | – | – | – | 19 | 0.98 | 0.70 | 0.99 |
| Gore, 200334 | – | – | – | – | 25 | 0.98 | 0.76 | 0.99 |
| Kuhns, 200523 | – | – | – | – | 33 | 0.99 | 0.80 | 0.99 |
| Liu, 201224 | – | – | – | – | 38 | 0.99 | 0.83 | 0.99 |
| Lowery, 199520 | 20 | 0.45 | 0.25 | 0.66 | 17 | 0.94 | 0.68 | 0.99 |
| Mutoh, 199325 | 14 | 0.97 | 0.63 | 0.99 | – | – | – | – |
| Newman 199331 | 16 | 0.81 | 0.55 | 0.95 | – | – | – | – |
| Phillips, 199726 | 16 | 0.88 | 0.61 | 0.97 | 6 | 0.93 | 0.42 | 0.99 |
| Siambanes, 199827 | – | – | – | – | 14 | 0.97 | 0.63 | 0.99 |
| Toohey, 200630 | – | – | – | – | 18 | 0.97 | 0.69 | 0.99 |
| Tribus, 199928 | 16 | 0.81 | 0.55 | 0.94 | – | – | – | – |
| Zdeblick, 199729 | 35 | 0.97 | 0.82 | 0.99 | – | – | – | – |
| Total | 0.86 | 0.71 | 0.97 | 0.97 | 0.94 | 0.99 | ||
Abbreviation: CI, confidence interval.
When selecting only those studies with matched cohorts, four reported fusion results for both an anterior and posterior approach.19 20 26 31 The pooled fusion success was 64.2% (CI: 47.3, 78.1) in the anterior group and 96.0% (CI: 89.1, 98.6) in the posterior group. The difference between the two groups was statistically significant (p < 0.001).
Clinical Results
Adequate clinical outcomes were reported in eight studies, with eight reporting anterior and eight reporting posterior approaches. The pooled clinical success rate was 77.0% (CI: 63.9, 86.3) for the anterior approach and 80.0% (CI: 72.0, 86.2) for the posterior approach (Fig. 2); the difference between the approaches was not statistically significant (p = 0.55; Table 3). The anterior groups demonstrated significant heterogeneity with a Q value of 16.1 and an I 2 value of 56.6%. There was also heterogeneity in the posterior group with a Q value of 19.2 and an I 2 value of 63.5% indicating significant differences in the clinical outcomes in both the anterior and posterior approach-based revision procedures independently.
Fig. 2.
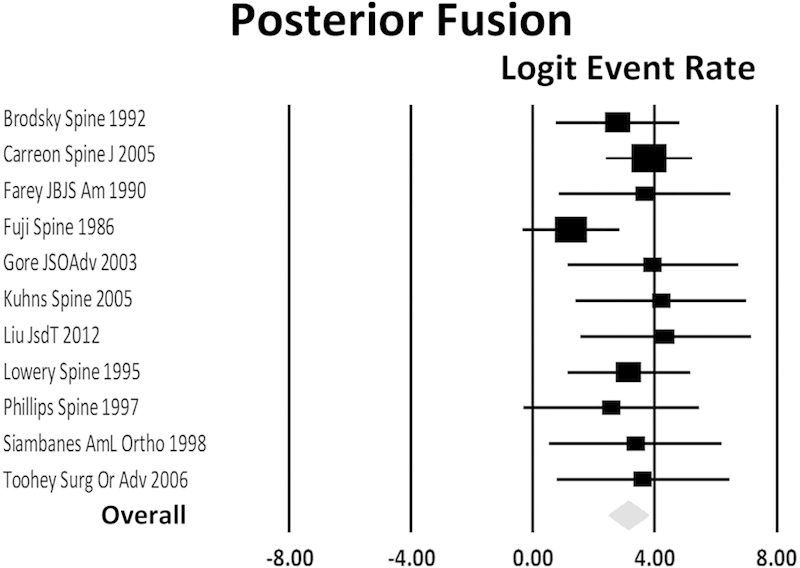
Forest plot of the logit event rate for clinical success with posterior surgery.
Table 3. Effect of surgical technique on clinical success.
| Anterior | Posterior | |||||||
|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | |||||||
| Study, first author and year | n | Clinical success | Lower | Upper | n | Clinical success | Lower | Upper |
| Brodsky, 199213 | 17 | 0.59 | 0.35 | 0.79 | 16 | 0.88 | 0.63 | 0.97 |
| Carreon, 200619 | – | – | – | – | – | – | – | – |
| Caspar, 199921 | 37 | 0.84 | 0.68 | 0.93 | – | – | – | – |
| Coric, 199718 | 18 | 0.83 | 0.59 | 0.94 | – | – | – | – |
| Farey, 199022 | – | – | – | – | 19 | 0.74 | 0.50 | 0.87 |
| Kuhns, 200523 | – | – | – | – | 33 | 0.72 | 0.52 | 0.86 |
| Liu, 201224 | – | – | – | – | 38 | 0.84 | 0.69 | 0.93 |
| Lowery, 199520 | 20 | 0.40 | 0.21 | 0.62 | 17 | 0.82 | 0.57 | 0.94 |
| Mutoh, 199325 | – | – | – | – | – | – | – | – |
| Newman 199331 | 7 | 0.71 | 0.33 | 0.93 | – | – | – | – |
| Phillips, 199726 | 16 | 0.88 | 0.61 | 0.93 | 6 | 0.93 | 0.42 | 0.99 |
| Siambanes, 199827 | – | – | – | – | 9 | 0.11 | 0.015 | 0.50 |
| Toohey, 200630 | – | – | – | – | 18 | 0.86 | 0.70 | 0.94 |
| Tribus, 199928 | 16 | 0.81 | 0.55 | 0.94 | – | – | – | – |
| Zdeblick, 199729 | 35 | 0.86 | 0.70 | 0.94 | – | – | – | – |
| Total | 0.77 | 0.64 | 0.86 | 0.80 | 0.72 | 0.86 | ||
Abbreviation: CI, confidence interval.
When selecting only those studies with matched cohorts, three reported clinical outcome results for both an anterior and a posterior approach.20 26 31 The pooled clinical success rate was 61.0% (CI: 37.3, 80.1) for the anterior and 86.7% (CI: 66.4, 95.6) for the posterior approach; the difference was not statistically significant (p = 0.55). The difference between the two groups was not statistically significant (p = 0.06).
Sensitivity Analysis and Publication Bias
Single elimination of each study resulted in a change of statistical result only once. When the Carreon study, which was a large study, was removed from the analysis, the difference between the groups became not significant (p= 0.07).19
The funnel plots were symmetric about the mean effect for both clinical and fusion success indicating absence of a publication bias. This was confirmed with the fail-safe N, which was 629. This means that we would need to locate and include 629 “null” studies before the combined two-tailed p value is nullified.
Discussion
The treatment of a symptomatic anterior cervical pseudarthrosis requires a choice between performing a revision anterior procedure or a posterior approach procedure. Revision anterior procedures for pseudarthrosis require dissection through scar tissue with the risk of damaging adjacent structures including the recurrent laryngeal nerve, esophagus, contents of the carotid sheath, and trachea.32 33 Coric et al showed a higher incidence of dysphagia in anterior revision procedures.18 Contraindications for the posterior cervical approach include the presence of graft dislodgement or a kyphotic deformity. Posterior cervical fusion has been associated with larger intraoperative blood loss, a longer hospital stay, and a higher overall complication rate.19
Meta-analysis allows for pooling of data from similar study designs to determine if there is a significant effect and if so, the magnitude of the effect. Additionally, the heterogeneity, or variability within studies, is assessed by measuring the consistency of the results between studies. A random-effects model was used in our analysis due to a lack of consistency among the included studies, with considerable variation in methodology and surgical technique both between and within the studies. In the anterior revision group, there was significant heterogeneity with large I 2 values for both fusion and clinical outcomes. The posterior group demonstrated homogeneity for fusion but large heterogeneity for clinical success. Thus, the posterior approach can be considered to result in a consistent result for fusion, but not for clinical success. The reported effect for fusion is likely close to the true effect in a posterior approach-based revision. Conversely, the anterior approach can be considered to produce moderately inconsistent results for both fusion and clinical success, with the reported effect likely divergent from the true effect. Given the moderate heterogeneity observed in the clinical and fusion results for the anterior group, uncertainty in the result can be inferred. In general, when little to no heterogeneity exists, the results that are reported likely represent an accurate reporting of the outcomes or the true effect.
Our meta-analysis indicated that the patients with symptomatic cervical pseudarthrosis can be effectively managed with either an anterior or a posterior approach, with the posterior approach demonstrating a statistically higher and largely reproducible fusion rate when compared with the anterior approach. Three studies in our meta-analysis included patients treated with either an anterior or a posterior approach.19 20 The average anterior fusion rate in these three studies was 59% and the average posterior fusion rate was 95.3%. Specifically, Carreon et al reported a reoperation rate of 44% after an anterior revision due to persistent nonunion.19 Those patients treated with a posterior procedure had a repeat revision rate of 6%. However, there was a significantly higher complication rate seen in the posterior group (8 versus 4%).
Despite significant difference in the rates of fusion, there was no statistically significant difference in the clinical outcomes between the two groups. This divergence could possibly be attributed to the higher complication rate as well as the postoperative neck pain that is seen in the posterior fusion group. Additionally, the rate of asymptomatic nonunion versus radiographic nonunion is not well defined in many of the studies. Our meta-analysis suggests that, for the treatment of anterior cervical pseudarthrosis, the posterior approaches are more likely to end in solid fusion, although there is no difference in clinical outcome between the two groups. Future randomized controlled trials with high methodological quality and long-term follow-ups are needed to better evaluate the two procedures for the treatment of symptomatic anterior cervical pseudarthrosis.
The primary studies did not distinguish between neck and arm pain, which is certainly a consideration when deciding upon an approach. Many authors would choose an anterior approach if anterior pathology is present at the site of pseudarthrosis, and others might perform a foraminotomy and posterior fusion. Unfortunately, we could not analyze differences between these two approached for this clinical scenario from our data. We would hypothesize that the poorer clinical results compared with fusion seen in the posterior group may be caused by residual anterior root compression. Similarly, there was insufficient information as to how the 28% of patients who failed a revision anterior fusion were subsequently treated or their ultimate outcome.
Limitations are inherent with all meta-analyses, including the heterogeneity of the included studies, missed studies within our search, and unknown biases within the primary studies. There is considerable variability among the studies in terms of the operative technique and the means of fixation in both the anterior and posterior groups. For instance, Carreon et al utilized thee different posterior stabilization techniques including wiring, lateral mass screw and plate systems, and lateral mass screw and rod systems.19 However, the type of instrumentation used for the posterior fusion did not appear to impact fusion rates or clinical outcome in any of the studies. Similarly, the older studies did not include anterior plate fixation, which may have increased the fusion success. Another potential limitation of this meta-analysis is the poor overall quality in the studies. The studies utilized a variety of different outcomes assessment tools and fusion criteria, which can also confound the combined results.
The lack of homogeneity, principally in the anterior group, is also a considerable potential limitation. A subgroup analysis to analyze different graft or plate and screw systems could not be performed as this information was not routinely available. Although all included patients were diagnosed with an anterior cervical pseudarthrosis, the heterogeneity of the surgical indications and the patient-dependent factors represent another potential study limitation. There was variability in the number of involved levels among cases, and the results are not stratified based on the number of nonunion levels treated.
Conclusions
Patients with symptomatic cervical pseudarthrosis can be effectively managed with either an anterior or a posterior approach surgery. The posterior approach demonstrated a significantly greater fusion rate compared with the anterior approach, though the clinical outcomes did not differ between the two treatment groups. The anterior approach demonstrated significant heterogeneity for both fusion and clinical success, and the posterior approach demonstrated homogeneity for fusion rates and less heterogeneity, as compared with anterior revisions, for clinical success. The posterior approach can therefore be considered to produce consistent results, and the effect we report is likely close to the true effect.
Footnotes
Disclosures Steven J. McAnany, none Evan O. Baird, none Samuel C. Overley, none Jun S. Kim, none Sheeraz A. Qureshi, Consultant: Stryker, Medtronic, Orthofix, Zimmer Paul A. Anderson, Consultant: Stryker, Pioneer, Aesculap; Royalties: Stryker, Pioneer; Stock/stock options: Si-Bone, Expanding Orthopedics, Titan Surgical
References
- 1.Bohlman H H, Emery S E, Goodfellow D B, Jones P K. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75(9):1298–1307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Carette S, Fehlings M G. Clinical practice. Cervical radiculopathy. N Engl J Med. 2005;353(4):392–399. doi: 10.1056/NEJMcp043887. [DOI] [PubMed] [Google Scholar]
- 3.Cloward R B. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15(6):602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 4.Emery S E, Bolesta M J, Banks M A, Jones P K. Robinson anterior cervical fusion comparison of the standard and modified techniques. Spine (Phila Pa 1976) 1994;19(6):660–663. [PubMed] [Google Scholar]
- 5.Smith G W, Robinson R A. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40-A(3):607–624. [PubMed] [Google Scholar]
- 6.Cho S K, Riew K D. Adjacent segment disease following cervical spine surgery. J Am Acad Orthop Surg. 2013;21(1):3–11. doi: 10.5435/JAAOS-21-01-3. [DOI] [PubMed] [Google Scholar]
- 7.Hou Y, Liu Y, Yuan W. et al. Cervical kinematics and radiological changes after Discover artificial disc replacement versus fusion. Spine J. 2014;14(6):867–877. doi: 10.1016/j.spinee.2013.07.432. [DOI] [PubMed] [Google Scholar]
- 8.Lee J H, Kim J S, Lee J H, Chung E R, Shim C S, Lee S H. Comparison of cervical kinematics between patients with cervical artificial disc replacement and anterior cervical discectomy and fusion for cervical disc herniation. Spine J. 2014;14(7):1199–1204. doi: 10.1016/j.spinee.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 9.Wu J C, Liu L, Wen-Cheng H. et al. The incidence of adjacent segment disease requiring surgery after anterior cervical diskectomy and fusion: estimation using an 11-year comprehensive nationwide database in Taiwan. Neurosurgery. 2012;70(3):594–601. doi: 10.1227/NEU.0b013e318232d4f2. [DOI] [PubMed] [Google Scholar]
- 10.Wu X D, Wang X W, Yuan W. et al. The effect of multilevel anterior cervical fusion on neck motion. Eur Spine J. 2012;21(7):1368–1373. doi: 10.1007/s00586-012-2157-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hilibrand A S, Carlson G D, Palumbo M A, Jones P K, Bohlman H H. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81(4):519–528. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Brodke D S Zdeblick T A Modified Smith-Robinson procedure for anterior cervical discectomy and fusion Spine (Phila Pa 1976) 199217(10, Suppl):S427–S430. [DOI] [PubMed] [Google Scholar]
- 13.Brodsky A E, Khalil M A, Sassard W R, Newman B P. Repair of symptomatic pseudoarthrosis of anterior cervical fusion. Posterior versus anterior repair. Spine (Phila Pa 1976) 1992;17(10):1137–1143. doi: 10.1097/00007632-199210000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Riley L H Jr, Robinson R A, Johnson K A, Walker A E. The results of anterior interbody fusion of the cervical spine. Review of ninety-three consecutive cases. J Neurosurg. 1969;30(2):127–133. doi: 10.3171/jns.1969.30.2.0127. [DOI] [PubMed] [Google Scholar]
- 15.Lindsey R W, Newhouse K E, Leach J, Murphy M J. Nonunion following two-level anterior cervical discectomy and fusion. Clin Orthop Relat Res. 1987;(223):155–163. [PubMed] [Google Scholar]
- 16.Wang J C, McDonough P W, Endow K K, Delamarter R B. Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2000;25(1):41–45. doi: 10.1097/00007632-200001010-00009. [DOI] [PubMed] [Google Scholar]
- 17.Wang J C McDonough P W Kanim L E Endow K K Delamarter R B Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion Spine (Phila Pa 1976) 2001266643–646., discussion 646–647 [DOI] [PubMed] [Google Scholar]
- 18.Coric D, Branch C L Jr, Jenkins J D. Revision of anterior cervical pseudoarthrosis with anterior allograft fusion and plating. J Neurosurg. 1997;86(6):969–974. doi: 10.3171/jns.1997.86.6.0969. [DOI] [PubMed] [Google Scholar]
- 19.Carreon L, Glassman S D, Campbell M J. Treatment of anterior cervical pseudoarthrosis: posterior fusion versus anterior revision. Spine J. 2006;6(2):154–156. doi: 10.1016/j.spinee.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 20.Lowery G L, Swank M L, McDonough R F. Surgical revision for failed anterior cervical fusions. Articular pillar plating or anterior revision? Spine (Phila Pa 1976) 1995;20(22):2436–2441. doi: 10.1097/00007632-199511001-00012. [DOI] [PubMed] [Google Scholar]
- 21.Caspar W Pitzen T Anterior cervical fusion and trapezoidal plate stabilization for re-do surgery Surg Neurol 1999524345–351., discussion 351–352 [DOI] [PubMed] [Google Scholar]
- 22.Farey I D, McAfee P C, Davis R F, Long D M. Pseudarthrosis of the cervical spine after anterior arthrodesis. Treatment by posterior nerve-root decompression, stabilization, and arthrodesis. J Bone Joint Surg Am. 1990;72(8):1171–1177. [PubMed] [Google Scholar]
- 23.Kuhns C A, Geck M J, Wang J C, Delamarter R B. An outcomes analysis of the treatment of cervical pseudarthrosis with posterior fusion. Spine (Phila Pa 1976) 2005;30(21):2424–2429. doi: 10.1097/01.brs.0000184314.26543.7d. [DOI] [PubMed] [Google Scholar]
- 24.Liu H, Ploumis A, Schwender J D, Garvey T A. Posterior cervical lateral mass screw fixation and fusion to treat pseudarthrosis of anterior cervical fusion. J Spinal Disord Tech. 2012;25(3):138–141. doi: 10.1097/BSD.0b013e31821532a5. [DOI] [PubMed] [Google Scholar]
- 25.Mutoh N, Shinomiya K, Furuya K, Yamaura I, Satoh H. Pseudarthrosis and delayed union after anterior cervical fusion. Int Orthop. 1993;17(5):286–289. doi: 10.1007/BF00181700. [DOI] [PubMed] [Google Scholar]
- 26.Phillips F M, Carlson G, Emery S E, Bohlman H H. Anterior cervical pseudarthrosis. Natural history and treatment. Spine (Phila Pa 1976) 1997;22(14):1585–1589. doi: 10.1097/00007632-199707150-00012. [DOI] [PubMed] [Google Scholar]
- 27.Siambanes D, Miz G S. Treatment of symptomatic anterior cervical nonunion using the Rogers interspinous wiring technique. Am J Orthop. 1998;27(12):792–796. [PubMed] [Google Scholar]
- 28.Tribus C B, Corteen D P, Zdeblick T A. The efficacy of anterior cervical plating in the management of symptomatic pseudoarthrosis of the cervical spine. Spine (Phila Pa 1976) 1999;24(9):860–864. doi: 10.1097/00007632-199905010-00005. [DOI] [PubMed] [Google Scholar]
- 29.Zdeblick T A, Hughes S S, Riew K D, Bohlman H H. Failed anterior cervical discectomy and arthrodesis. Analysis and treatment of thirty-five patients. J Bone Joint Surg Am. 1997;79(4):523–532. [PubMed] [Google Scholar]
- 30.Toohey J S, Stromberg L, Neidre A, Ramsey M, Fogel G R. Treatment of cervical pseudarthrosis after Smith-Robinson procedure with Halifax clamp fixation. J Surg Orthop Adv. 2006;15(4):201–202. [PubMed] [Google Scholar]
- 31.Newman M. The outcome of pseudarthrosis after cervical anterior fusion. Spine (Phila Pa 1976) 1993;18(16):2380–2382. doi: 10.1097/00007632-199312000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Beutler W J, Sweeney C A, Connolly P J. Recurrent laryngeal nerve injury with anterior cervical spine surgery risk with laterality of surgical approach. Spine (Phila Pa 1976) 2001;26(12):1337–1342. doi: 10.1097/00007632-200106150-00014. [DOI] [PubMed] [Google Scholar]
- 33.Bertalanffy H, Eggert H R. Complications of anterior cervical discectomy without fusion in 450 consecutive patients. Acta Neurochir (Wien) 1989;99(1–2):41–50. doi: 10.1007/BF01407775. [DOI] [PubMed] [Google Scholar]
- 34.Gore D R, Brechbuler M. Treatment of nonunions following anterior cervical discectomy and fusion with interspinous wiring and bone grafting. J Surg Orthop Adv. 2003;12(4):214–217. [PubMed] [Google Scholar]


