Abstract
Study Design Retrospective study.
Objective Minor trauma, even from a simple fall, can often cause cervical myelopathy, necessitating surgery in elderly patients who may be unaware of their posterior longitudinal ligament ossification (OPLL). The aim of this study is to determine the influence of trauma on the neurologic course in patients who have undergone surgery for cervical OPLL.
Methods Patients who underwent surgery due to OPLL were divided by trauma history and compared (34 in the trauma group; 70 in the nontrauma group).
Results Ground falls were the most common type of trauma (20 patients, low-energy injuries), but 23 patients developed new symptoms after a trauma. Although the symptom duration (17.68 months) was shorter, the Japanese Orthopedic Association (JOA) score and the Nurick scale showed lower values in the trauma group. Trauma histories led patients to earlier hospital visits. Initial JOA scores were associated with a good recovery status upon the last follow-up in both the groups. The narrowest diameter of the spinal canal showed different radiologic parameters: 5.78 mm in the trauma group and 6.52 mm in the nontrauma group.
Conclusion Minor trauma can cause the unexpected development of new symptoms in patients unaware of cervical OPLL. Patients with a history of trauma had lower initial JOA scores and showed a narrower spinal canal compared with a nontrauma group. The initial JOA scores were correlated with a good recovery status upon the last follow-up.
Keywords: ossification of the posterior longitudinal ligament, trauma, cervical spine
Introduction
Given that ossification of the posterior longitudinal ligament (OPLL) is common in the elderly Asian population with myelopathy and contributes to significant neurologic disabilities, the early recognition and the appropriate management of those who may be unaware of their OPLL condition are critical factors in preserving the quality of life of these patients.1 2 3 4 5 It is clear that trauma is hazardous in individuals with cervical OPLL, and recent research has reported an alarmingly high prevalence of OPLL in 34% of patients with cervical spinal cord injuries (SCIs).5 6 7 Surgical treatment for OPLL is clearly indicated when the patient shows moderate to severe cervical myelopathy.1 2 3 4 8 9 Prophylactic surgery, however, in patients who are asymptomatic or in patients with mild myelopathy and OPLL has been a point of controversy among surgeons.6 10 11 12 In fact, several longitudinal cohort studies have revealed that cervical trauma has little effect on the outcomes of asymptomatic patients with OPLL; thus, the current evidence does not allow for firm and broad recommendations to be made regarding prophylactic surgery to reduce the risk of aggravation as caused by a minor cervical trauma.4 12 Moreover, cervical SCIs and related disabilities are more likely to occur in patients with OPLL, and conservatively treated OPLL increases the risk of SCI (4.8 per 1000 person-years).13
Our clinical impression of the patients with cervical OPLL is that even minor trauma such as a fall onto the ground can induce cervical myelopathy, and patients may be unaware of having the condition before the trauma incident. In addition, the surgical outcomes for such patients are not comparable to those of patients without a history of trauma. Hence, we undertook clinical and radiologic evaluations of patients who underwent surgical treatment due to cervical OPLL and identified the influence of trauma on their clinical courses and neurologic recovery characteristics.
Materials and Methods
Patient Population
Between 2000 and 2010, 121 patients with cervical OPLL underwent surgical treatment by two experienced spine surgeons at one institute. According to their histories of trauma obtained from their medical records, 41 (33.8%) had a history of trauma and 80 (66.2%) had experienced no trauma. Patients with a minimum of 1 year of follow-up were included, and patients with cerebrovascular disease, Parkinson disease, or cerebral palsy were excluded. After paring the potential participant list, 104 patients were included in the study: 34 (32.7%) in the trauma group and 70 (67.3%) in the nontrauma group.
Clinical and Radiologic Evaluations
The medical records and radiologic images were reviewed initially and upon the last follow-up. The initial symptoms during the first clinical visit were classified in terms of whether or not the lower extremities were involved. The time between symptom development and surgery was also investigated. In the trauma group, the etiology of trauma in terms of the injury mechanism was divided into high- and low-energy injuries.14 Deterioration of pre-existing symptoms and the development of new symptoms after trauma were also checked. The Japanese Orthopedic Association (JOA) score and the Nurick scale were used to assess the degree of cervical myelopathy.15 16 The recovery rate was calculated as follows: recovery rate (%) = [postoperative JOA score − preoperative JOA score]/[17 − preoperative JOA score] × 100.17 The recovery rate at the last follow-up was ranked at ≥50% for a good recovery status and at <50% for a fair recovery status. The surgical treatments were divided into anterior, posterior, or combined approaches based on the patients' operation records.
Radiographically, bony injuries with spinal instability were investigated. On the plain radiographs, the cervical angle and cervical range of motion (ROM) at C2–C7 were calculated by Cobb's method. On computed tomography (CT) scans, the type of OPLL was classified as segmental, continuous, mixed, or other type.18 The narrowest space available for the spinal cord (SAC) was measured on midsagittal the CT images. The presence and length associated with the high signal intensity were evaluated on the patients' initial T2-weighted magnetic resonance images (MRIs).
Statistical Analysis
The statistical analysis was performed using the Student t test for the continuous variables. A chi-square test or Fisher exact test was used for categorical variables. Logistic regression analysis was used to evaluate the factors affecting a good recovery rate. A value of p < 0.05 was considered significant. To assess this, SPSS software version 19.0 (IBM, Armonk, New York, United States) was used.
Results
Patient Demographics
Previous trauma history was detected in 34 patients (32.7%) who were dividing into the trauma group, with the remaining 70 patients (67.3%) were categorized into the nontrauma group (Table 1).
Table 1. Demographic data.
| Trauma group (n = 34) | Nontrauma group (n = 70) | p Value | |
|---|---|---|---|
| Sex (female: male) | 7: 27 | 17: 53 | 0.678 |
| Age at surgery (y) | 56.24 ± 8.79 | 53.90 ± 9.30 | 0.225 |
| Initial symptom involvement | 0.218 | ||
| Without lower extremities | 13 | 36 | |
| With lower extremities | 21 | 34 | |
| Symptom duration (mo) | 17.68 ± 22.96 | 31.00 ± 39.57 | 0.033 |
| Surgical approach | 0.605 | ||
| Anterior | 14 | 33 | |
| Posterior | 17 | 34 | |
| Combined anterior and posterior | 3 | 3 | |
| Follow-up period (mo) | 56.47 ± 51.25 | 47.73 ± 31.89 | 0.289 |
The 7 women and 27 men in the trauma group had a mean age of 56.24 ± 8.79 years (range, 44 to 77). The etiologies of their incidences of trauma were mostly low-energy injuries. These included 20 falls onto the ground, with 5 falls from a low height (<1 m) and 3 with head trauma and neck extension. In addition, 6 were in motor vehicle accidents with high-energy injuries (Table 2). Pre-existing symptoms deteriorated after the experience of trauma in 11, but only 1 patient was aware of having cervical OPLL and had had surgery as recommended previously. Twenty-three patients showed newly developed symptoms after the trauma. At the moment of the trauma, 5 patients experienced transient quadriparesis, which spontaneously resolved within a few minutes to a few days, and 7 patients underwent surgery within 48 hours after the trauma. With regard to symptom duration between symptom development and the surgery, the durations were 17.68 ± 22.96 months (range, 0 to 60), with all patients showing the symptoms related to cervical myelopathy upon surgery. Thirteen had the symptoms without involvement of the lower extremities and 21 with involvement of the lower extremities. The surgical treatment was given to 14 via the anterior approach, with 17 undergoing the posterior approach and 3 undergoing a combined approach. The mean follow-up period was 56.47 ± 51.25 months (range, 13 to 254) in the trauma group.
Table 2. Etiology of trauma in 34 patients of trauma group.
| Injury mechanism | Etiology of trauma | Number |
|---|---|---|
| Low-energy injury | Fall onto the ground level | 20 |
| Fall at the low height (<1 m) | 5 | |
| Head trauma with neck extension | 3 | |
| High-energy injury | Motor vehicle accident | 6 |
The 70 patients in the nontrauma group (17 women and 53 men) had a mean age of 53.90 ± 9.32 years (range, 38 to 79). Their symptoms gradually developed and continued for 31.00 ± 39.57 months (range, 0.5 to 240). The symptom durations were longer in the nontrauma group than in the trauma group (p = 0.033). Upon the first clinical visit, 36 patients complained of symptoms in their upper extremities, and 34 patients noted that all four extremities were involved. Surgery was performed on 33 patients via the anterior approach, 34 by means of the posterior approach, and 3 in a combined approach. After the surgery, the mean follow-up period was 47.73 ± 31.89 months (range, 12 to 145) in the nontrauma group.
Clinical Outcomes
The initial JOA score was lower in the trauma group (10.53 ± 4.71, range, 0 to 16) than in the nontrauma group (12.89 ± 2.49, range, 5 to 16, Fig. 1A). The final JOA score was also lower in the trauma group (13.38 ± 4.00, range, 3 to 17) than in the nontrauma group (15.49 ± 1.93, range, 8 to 17). The recovery rate was 51.06 ± 35.12% (range, 0 to 100) in the trauma group and 68.76 ± 31.78% (range, 0 to 100) in the nontrauma group. The JOA scores upon the initial and last evaluation and the recovery rate all showed favorable and statistically significant results in the nontrauma group (p = 0.001, p = 0.000, and p = 0.012, respectively). The clinical outcomes using the Nurick scale showed similar results upon the initial and the last evaluations of the two groups (p = 0.002 and p = 0.039, Fig. 1B).
Fig. 1.
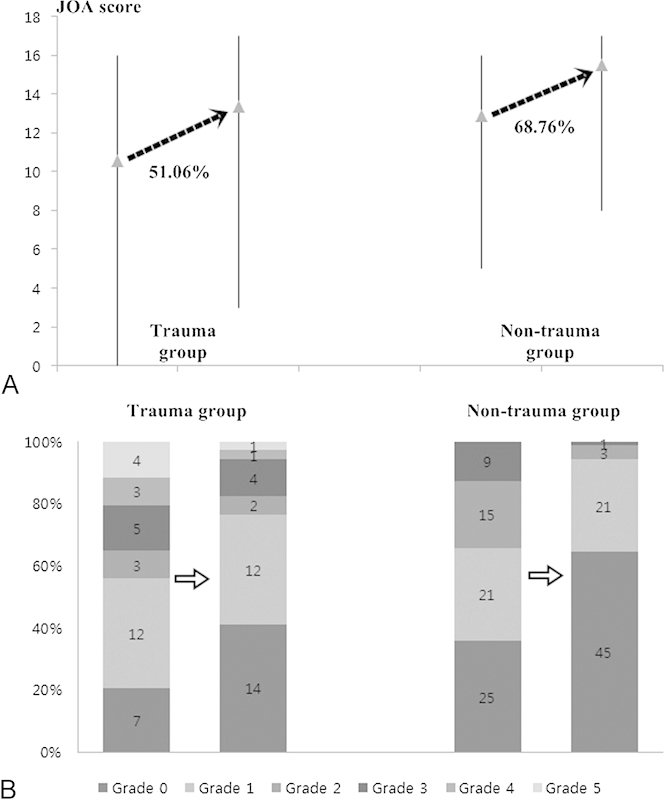
Clinical outcomes. (A) Japanese Orthopedic Association (JOA) score and recovery rate. Clinical parameters according to the JOA score upon the initial and last evaluation showed lower values in the trauma group than in the nontrauma group, with statistical significance. A more favorable recovery rate was also observed in the nontrauma group. (B) Changes of the Nurick scale. The initial Nurick scale was significantly different (p = 0.002), as was the last scale (p = 0.039) between the trauma and nontrauma groups.
Radiologic Outcomes
None of the patients in the trauma group showed bony injury with spinal instability preoperatively.
The cervical angle and ROM at C2–C7 had greater values in the nontrauma group, but the difference was not statistically significant relative to those of the trauma group (Table 3). In the trauma group, the mixed type of OPLL was prominent in 19 (55.88%), and 8 (23.52%) showed other type, 6 (17.64%) showed the segmental type, and 1 (2.94%) showed the continuous type. In the nontrauma group, the mixed type was also the most commonly classified, occurring in 31 (44.28%). The OPLL type differences were not statistically significant between the trauma and the nontrauma groups (p = 0.670). The narrowest SAC was 5.78 ± 1.29 mm (range, 3.59 to 8.03) in the trauma group and 6.52 ± 1.50 mm (range, 3.09 to 9.90) in the nontrauma group (p = 0.028). The presence of a high signal intensity in the T2-weighted sagittal MRIs was observed in 20 patients (58.82%, 13.25 ± 10.33 mm) in the trauma group and 40 (57.14%, 10.03 ± 9.29 mm) in the nontrauma group (p = 0.408).
Table 3. Radiologic outcomes.
| Trauma group | Nontrauma group | p Value | |
|---|---|---|---|
| Cervical angle | |||
| Initial | −8.28 ± 7.37 | −11.29 ± 8.93 | 0.130 |
| Last | −4.43 ± 7.96 | −7.59 ± 9.55 | 0.285 |
| Cervical ROM | |||
| Initial | 29.00 ± 14.19 | 34.92 ± 12.37 | 0.081 |
| Last | 19.16 ± 18.01 | 21.55 ± 10.40 | 0.532 |
| Type of OPLL (%) | 0.670 | ||
| Continuous | 1 (2.94) | 5 (7.14) | |
| Segmental | 6 (17.64) | 13 (18.57) | |
| Mixed | 19 (55.88) | 31 (44.28) | |
| Other | 8 (23.52) | 20 (28.57) | |
| Narrowest SAC (mm) | 5.78 ± 1.29 | 6.52 ± 1.50 | 0.028 |
| Presence of HIS (%) | 20 (58.82) | 40 (57.14) | 0.408 |
| Length of HIS (mm) | 13.25 ± 10.33 | 10.03 ± 9.29 | 0.221 |
Abbreviations: HIS, high signal intensity; OPLL, ossification of the posterior longitudinal ligament; ROM, range of motion; SAC, space available for the spinal canal.
Parameters Influencing a Good Recovery Status
A good recovery status (recovery rate ≥ 50%) was confirmed in 18 patients (52.94%) in the trauma group and 55 (78.57%) in the nontrauma group (p = 0.007). Meanwhile, a fair recovery status upon the last evaluation was noted in 16 (47.05%) in the trauma group and 15 in the nontrauma group (21.42%). The trauma history affected the fair recovery result upon the last evaluation, showing statistical significance (p = 0.001, relative risk = 1.484, 95% confidence interval, 1.057 to 2.084). Among the gender, age, and clinical and radiologic parameters, the logistic regression analysis results identified the initial JOA score as the factor most strongly affecting a good recovery status (p = 0.024, odds ratio= 1.206, 95% confidence interval, 1.025 to 1.418).
Discussion
Influence of Cervical Trauma on the Clinical Course
We analyzed the clinical and radiologic outcomes of patients who underwent surgical treatment for cervical OPLL at one institute between 2002 and 2010. One adverse effect of trauma was the surprisingly common development of new symptoms in elderly patients who had not been aware of their cervical OPLL. As in the previous reports focusing on cervical OPLL and trauma, the etiology of the trauma was mostly low-energy injuries from a fall onto the ground in the present study.19 20 Even when the trauma was minor, 23 patients developed new symptoms, and among them, 5 experienced transient quadriparesis for a short time. Although 7 patients had to undergo surgical treatment within 48 hours post-trauma, symptoms in 27 patients who were conservatively observed became gradually more aggravated. As a result, trauma-induced symptoms led these patients to visit the hospital within relatively short symptom durations with unfavorable neurologic status compared with patients without trauma. Because a good recovery status was associated with no trauma history and a good initial JOA score, the trauma itself adversely affected the patients' clinical courses.
In the present study, a narrow SAC of less than 8 mm was noted in both the groups, but a narrower SAC (5.78 mm) was determined in the trauma group. Although the mixed and segmental types of OPLL were identified in ∼80% of those in the trauma group, a similar proportion was observed in the nontrauma group. The other radiologic parameters as well (i.e., the cervical angle, ROM, and high signal intensity on MRI) were not significantly different between the two groups. Although a narrow spinal canal as confirmed by a radiologic evaluation was not always associated with poor clinical parameters, the authors suggest that a narrow spinal canal is an important risk factor for trauma-induced cervical myelopathy in patients with OPLL.
Surgical Timing for Trauma-Induced Cervical Myelopathy from Cervical OPLL
There is controversy regarding the role of prophylactic surgery in patients who are asymptomatic or who have only mild myelopathy from cervical OPLL.4 10 11 12 Therefore, many surgeons have debated the efficacy of surgery for asymptomatic individuals with narrow spinal canals from cervical OPLL. Matsunaga et al prospectively found that trauma-induced cervical SCI in patients with OPLL could be decreased by informing the patients of the risk. They also showed that the prophylactic surgery was not necessary in the patients with OPLL.4 Several authors have argued that the risk of surgical complications would be higher than the risk of myelopathy after trauma.10 However, once elderly patients sustain a cervical SCI, their quality of life can deteriorate seriously and their lives can be threatened in some cases.6 21 One report found that conservatively treated OPLL increases the risk of SCI, and a comparative study of acute cervical SCI from OPLL reported that laminoplasty showed more satisfactory outcomes than a conservative management strategy.13 22
In the present study, a good recovery status upon the last follow-up was not noted in the trauma group to the extent that it was in the nontrauma group despite the fact that the surgery was performed. Although the relationship between the surgery and prognosis was unclear because the natural course of the clinical symptoms was not fully detailed, a good initial JOA score was found to be important in the determination of a good recovery status in the present study.23 24 Concerning the proper timing of the surgery, early surgical decompression for OPLL was recommended because the outcome of this procedure was better for younger patients and for those with a higher JOA score.25 Although the need for the prophylactic surgery in asymptomatic patients with cervical OPLL cannot be fully supported in this study, if patients with a history of trauma are found to have a narrow spinal canal from OPLL, the surgical treatment should be recommended as soon as possible before further deterioration of their neurologic status.
Limitations of the Study
There has been debate over which surgical approach is better for the treatment of cervical OPLL.22 26 27 In the present study, anterior or posterior, or occasionally a combined approach, was performed with anterior cervical diskectomy and fusion at a single level to three levels. Also performed were corpectomy with/without additional anterior cervical diskectomy and fusion, laminectomy with/without fusion, or laminoplasty. Considering the advantages and disadvantages of each surgical approach, the results of each can offer useful data. Because the surgical approach did not show a significant difference between the trauma and nontrauma groups, the authors left out the details about the surgical approach. The progression of OPLL after the posterior approach can affect the long-term clinical outcomes, but the authors did not measure this owing to a lack of available CT scans during the last evaluations. Adjacent segmental disease after cervical spinal surgery could develop and result in poor clinical outcomes and additional surgeries. As patients age, they often complain of the symptoms related to degenerative lumbar spinal diseases after surgery for cervical OPLL. In addition, a trauma event after the surgery also acted as a risk factor for the neurologic deterioration, even in the patients without a history of trauma.
As described previously, multiple factors can affect the clinical course of the patients who undergo surgical treatment for cervical OPLL. However, cervical myelopathy can be induced after minor trauma via low-energy injuries in patients who are unaware of their cervical OPLL status, and these patients typically undergo the surgery to relieve their symptoms. Minor trauma could develop during one's lifetime, and the alarm to prevent injury alone cannot prevent trauma-induced cervical myelopathy. The prophylactic surgery for asymptomatic patients with narrow spinal canals from OPLL should be tailored based on population-based case–control studies or prospective long-term studies with electrophysiologic evidence of the cervical radicular dysfunction or the central conduction deficits.28
Conclusion
Surprisingly, minor trauma could lead to the development of new symptoms in patients who were not aware of their cervical OPLL status. Patients with a history of trauma showed lower initial JOA scores with a narrower spinal canal compared with a nontrauma group. Initial JOA scores were correlated with a good recovery status upon the last follow-up.
Footnotes
Disclosures Soo Eon Lee, none Tae-Ahn Jahng, none Hyun-Jib Kim, none
References
- 1.Inamasu J Guiot B H Sachs D C Ossification of the posterior longitudinal ligament: an update on its biology, epidemiology, and natural history Neurosurgery 20065861027–1039., discussion 1027–1039 [DOI] [PubMed] [Google Scholar]
- 2.Schmidt M H, Quinones-Hinojosa A, Rosenberg W S. Cervical myelopathy associated with degenerative spine disease and ossification of the posterior longitudinal ligament. Semin Neurol. 2002;22(2):143–148. doi: 10.1055/s-2002-36537. [DOI] [PubMed] [Google Scholar]
- 3.Tsuyama N. Ossification of the posterior longitudinal ligament of the spine. Clin Orthop Relat Res. 1984;(184):71–84. [PubMed] [Google Scholar]
- 4.Matsunaga S Sakou T Taketomi E Komiya S Clinical course of patients with ossification of the posterior longitudinal ligament: a minimum 10-year cohort study J Neurosurg 2004100(3, Suppl Spine):245–248. [DOI] [PubMed] [Google Scholar]
- 5.Epstein N. Ossification of the cervical posterior longitudinal ligament: a review. Neurosurg Focus. 2002;13(2):ECP1. doi: 10.3171/foc.2002.13.2.16. [DOI] [PubMed] [Google Scholar]
- 6.Epstein N E. Laminectomy for cervical myelopathy. Spinal Cord. 2003;41(6):317–327. doi: 10.1038/sj.sc.3101477. [DOI] [PubMed] [Google Scholar]
- 7.Chikuda H, Seichi A, Takeshita K. et al. Acute cervical spinal cord injury complicated by preexisting ossification of the posterior longitudinal ligament: a multicenter study. Spine (Phila Pa 1976) 2011;36(18):1453–1458. doi: 10.1097/BRS.0b013e3181f49718. [DOI] [PubMed] [Google Scholar]
- 8.Sakou T, Matsunaga S, Koga H. Recent progress in the study of pathogenesis of ossification of the posterior longitudinal ligament. J Orthop Sci. 2000;5(3):310–315. doi: 10.1007/s007760050169. [DOI] [PubMed] [Google Scholar]
- 9.Matsunaga S Kukita M Hayashi K et al. Pathogenesis of myelopathy in patients with ossification of the posterior longitudinal ligament J Neurosurg 200296(2, Suppl):168–172. [DOI] [PubMed] [Google Scholar]
- 10.Lauryssen C R, Riew K D, Wang J C. Severe cervical stenosis: operative treatment of continued conservative care? Spine Line. 2006;7(1):21–25. [Google Scholar]
- 11.Matsunaga S Sakou T Hayashi K Ishidou Y Hirotsu M Komiya S Trauma-induced myelopathy in patients with ossification of the posterior longitudinal ligament J Neurosurg 200297(2, Suppl):172–175. [DOI] [PubMed] [Google Scholar]
- 12.Yonenobu K. Is surgery indicated for asymptomatic or mildly myelopathic patients with significant ossification of the posterior longitudinal ligament? Spine (Phila Pa 1976) 2012;37(5):E315–E317. doi: 10.1097/BRS.0b013e318239ccbd. [DOI] [PubMed] [Google Scholar]
- 13.Wu J C, Chen Y C, Liu L. et al. Conservatively treated ossification of the posterior longitudinal ligament increases the risk of spinal cord injury: a nationwide cohort study. J Neurotrauma. 2012;29(3):462–468. doi: 10.1089/neu.2011.2095. [DOI] [PubMed] [Google Scholar]
- 14.Committee on Trauma . Chicago, IL: Committee on Trauma; 1999. Resources for Optimal Care of the Injured Patient. [Google Scholar]
- 15.Yone K Sakou T Yanase M Ijiri K Preoperative and postoperative magnetic resonance image evaluations of the spinal cord in cervical myelopathy Spine (Phila Pa 1976) 199217(10, Suppl):S388–S392. [DOI] [PubMed] [Google Scholar]
- 16.Nurick S. The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain. 1972;95(1):87–100. doi: 10.1093/brain/95.1.87. [DOI] [PubMed] [Google Scholar]
- 17.Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976) 1981;6(4):354–364. doi: 10.1097/00007632-198107000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976) 1983;8(7):693–699. doi: 10.1097/00007632-198310000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Schneider R C, Cherry G, Pantek H. The syndrome of acute central cervical spinal cord injury; with special reference to the mechanisms involved in hyperextension injuries of cervical spine. J Neurosurg. 1954;11(6):546–577. doi: 10.3171/jns.1954.11.6.0546. [DOI] [PubMed] [Google Scholar]
- 20.Frankel H L, Hancock D O, Hyslop G. et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969;7(3):179–192. doi: 10.1038/sc.1969.30. [DOI] [PubMed] [Google Scholar]
- 21.DeVivo M J, Kartus P L, Stover S L, Rutt R D, Fine P R. Seven-year survival following spinal cord injury. Arch Neurol. 1987;44(8):872–875. doi: 10.1001/archneur.1987.00520200074023. [DOI] [PubMed] [Google Scholar]
- 22.Gu Y, Chen L, Dong R B, Feng Y, Yang H L, Tang T S. Laminoplasty versus conservative treatment for acute cervical spinal cord injury caused by ossification of the posterior longitudinal ligament after minor trauma. Spine J. 2014;14(2):344–352. doi: 10.1016/j.spinee.2013.06.083. [DOI] [PubMed] [Google Scholar]
- 23.Goto S, Kita T. Long-term follow-up evaluation of surgery for ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976) 1995;20(20):2247–2256. doi: 10.1097/00007632-199510001-00012. [DOI] [PubMed] [Google Scholar]
- 24.Miyazaki K, Kirita Y. Extensive simultaneous multisegment laminectomy for myelopathy due to the ossification of the posterior longitudinal ligament in the cervical region. Spine (Phila Pa 1976) 1986;11(6):531–542. doi: 10.1097/00007632-198607000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Kato Y, Iwasaki M, Fuji T, Yonenobu K, Ochi T. Long-term follow-up results of laminectomy for cervical myelopathy caused by ossification of the posterior longitudinal ligament. J Neurosurg. 1998;89(2):217–223. doi: 10.3171/jns.1998.89.2.0217. [DOI] [PubMed] [Google Scholar]
- 26.Liu X, Wang H, Zhou Z, Jin A. Anterior decompression and fusion versus posterior laminoplasty for multilevel cervical compressive myelopathy. Orthopedics. 2014;37(2):e117–e122. doi: 10.3928/01477447-20140124-12. [DOI] [PubMed] [Google Scholar]
- 27.Sun Q, Hu H, Zhang Y. et al. Do intramedullary spinal cord changes in signal intensity on MRI affect surgical opportunity and approach for cervical myelopathy due to ossification of the posterior longitudinal ligament? Eur Spine J. 2011;20(9):1466–1473. doi: 10.1007/s00586-011-1813-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilson J R, Barry S, Fischer D J. et al. Frequency, timing, and predictors of neurological dysfunction in the nonmyelopathic patient with cervical spinal cord compression, canal stenosis, and/or ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976) 2013;38(22) 01:S37–S54. doi: 10.1097/BRS.0b013e3182a7f2e7. [DOI] [PubMed] [Google Scholar]


