Abstract
Study Design Retrospective study.
Objective The interlaminar approach represents the standard procedure for the surgical treatment of lumbar disk herniation (LDH). In the case of disk herniations in the “hidden zone,” it could be necessary to perform laminotomies or laminectomies and partial or total facetectomies to remove the herniated fragment, thus leading to iatrogenic instability. The objective of the study is to evaluate the translaminar approach, in terms of the results, safety, and efficacy compared with the standard approach.
Methods Since February 2010, 38 patients (26 men and 12 women; mean age 50.9 years, range 31 to 78 years) with LDH and migration into the hidden zone underwent a microdiskectomy by the translaminar approach. Using a micro-diamond dust-coated burr, a translaminar hole (8 ± 2 mm) was made, with subsequent exposure of the involved root and removal of the fragment. A clinical follow-up was performed at months 1, 3, 6, and 12 using the visual analog scale and the Oswestry Disability Index. All patients were evaluated according to the Spangfort score. Postoperative radiographic evaluations were done at 1, 6, and 12 months (dynamic radiographic studies done at 6 and 12 months).
Results In over 60% of cases, L4–L5 was the involved disk. The visualization of the roots was successfully achieved through a translaminar approach. No laminotomies, laminectomies, or partial or total facetectomies were performed. The flavum ligament was always spared. A severe intraoperative bleeding episode occurred in 5% of the cases, due to involvement of the epidural veins, but it did not result in prolonged operative time (mean duration 60 ± 10 minutes). The patients showed a gradual resolution of the back pain and a progressive resolution of the radicular pain and the neurologic deficits. No sign of radiographic instability was documented during the follow-up. No infections, dural tears, or spinal cord injuries occurred. No revision surgery was performed.
Conclusion The translaminar approach is the only tissue-sparing technique viable in case of cranially migrated LDH encroaching on the exiting nerve root in the preforaminal zones, for the levels above L2–L3, and in the preforaminal and foraminal zones, for the levels below L3–L4 (L5–S1 included, if a total microdiskectomy is not necessary). The possibility to spare the flavum ligament is one of the main advantages of this technique. According to our experience, the translaminar approach is an effective and safe alternative minimally invasive surgical option.
Keywords: lumbar disk hernia, “hidden zone” hernia, translaminar approach, mini-invasiveness, tissue-sparing surgery, flavum ligament, cranially migrated disk herniations, stability
Introduction
Lumbar disk herniation (LDH) is a degenerative disease with an estimated prevalence ∼1 to 3% of the Italian population (male-to-female ratio = 2:1.6).1 Approximately 90% of the adult population will be affected during their lifetime.2 In people aged 25 to 55 years, ∼95% of LDHs occurs at L4–L5 and L5–S1 level, whereas for those over 55 years, it is more common above the L4–L5 level.3 Although LDH generally occurs without migration of the fragment to the levels above or below, in 10% of the cases, this migration might happen.2 In such cases, the standard interlaminar microsurgical approach as described by Caspar cannot be performed without laminotomies, interlaminectomies, or partial or total facetectomies.4 These surgical procedures and specifically the facetectomies may lead to an iatrogenic instability; therefore, a fusion becomes mandatory.5
In the case of cranially extruded LDH,6 7 a minimally invasive approach to respect the anatomy and the biomechanics of the spine becomes the most appropriate technique. The translaminar approach8 9 allows the possibility of sparing the flavum ligament,10 which confers several advantages. The purpose of this study is to evaluate this surgical technique in terms of efficacy and safety.
Materials and Methods
Since February 2010, 38 patients (26 men and 12 women; mean age 50.9 years, range 31 to 78) affected with LDH and fragment migration in the hidden zone underwent a microdiskectomy via the translaminar approach. Level L2–L3 was involved in 8 patients, L3–L4 in 11, L4–L5 in 17, and L5–S1 in 2. Of the 38 patients, 9 were already operated on using a standard interlaminar approach.
Radicular pain and sensory and motor deficits were clinically observed in 38, 29, and 19 patients, respectively. An electromyographic evaluation assessed the peripheral nerve damage.
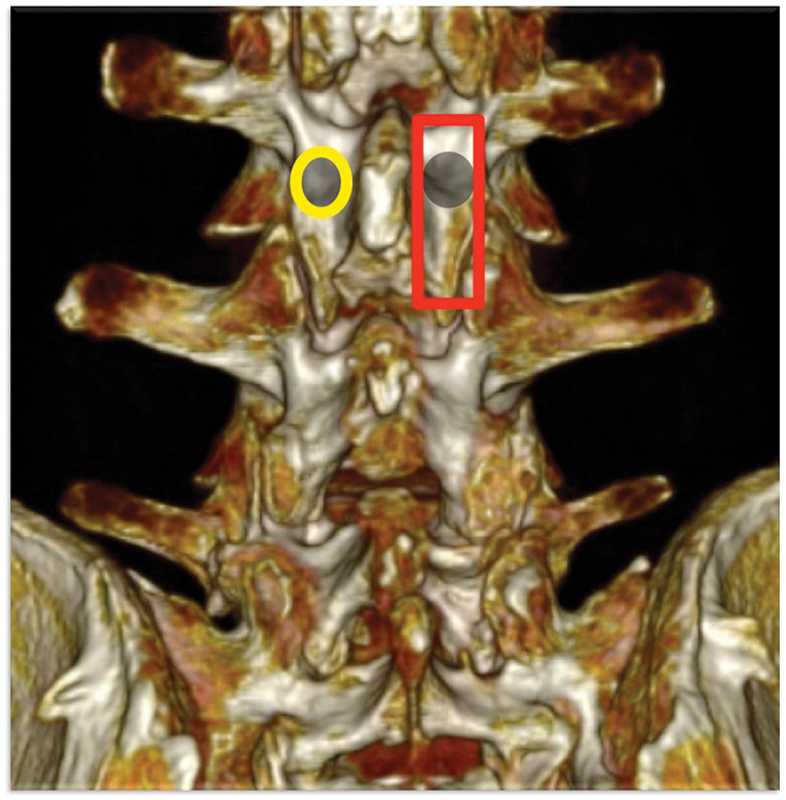
The radiographic exams (including dynamic examinations), computed tomography (CT), and magnetic resonance imaging (MRI) were performed in all patients (Figs. 1, 2, 3, 4, 5, 6, 7, 8, 9).
Fig. 1.

Preoperative anteroposterior radiograph.
Fig. 2.

Preoperative lateral radiograph.
Fig. 3.
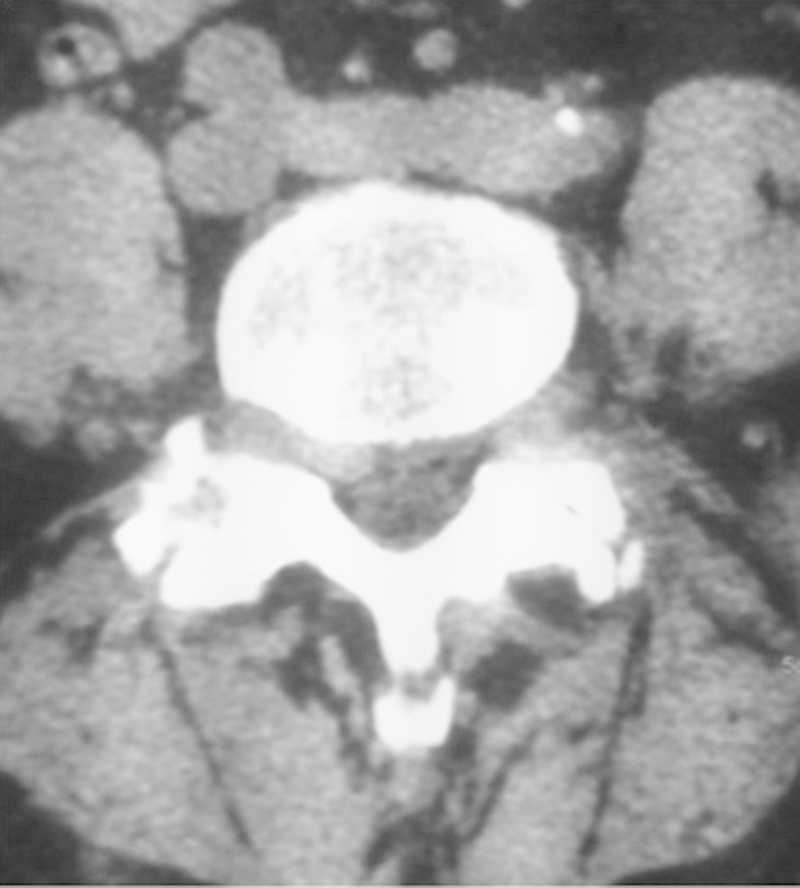
Preoperative computed tomography scan.
Fig. 4.
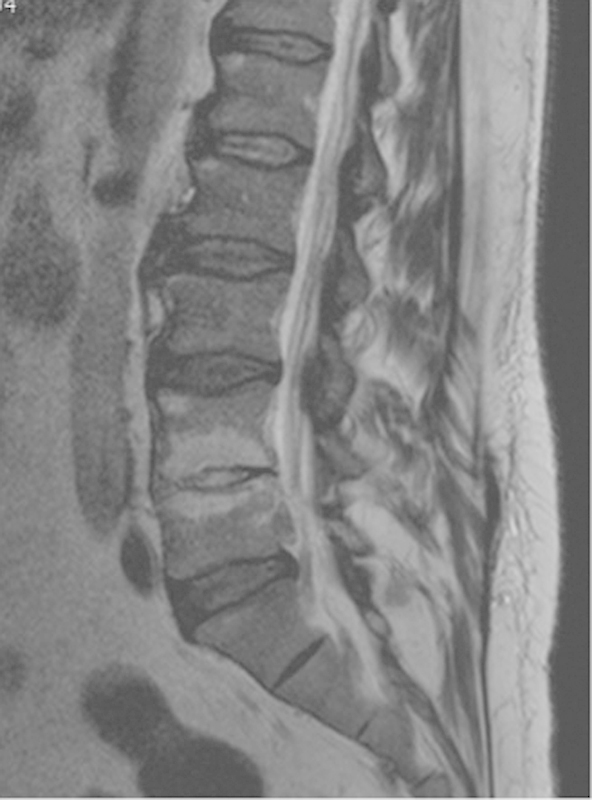
Preoperative nuclear magnetic resonance T2-weighted turbo spin-echo.
Fig. 5.
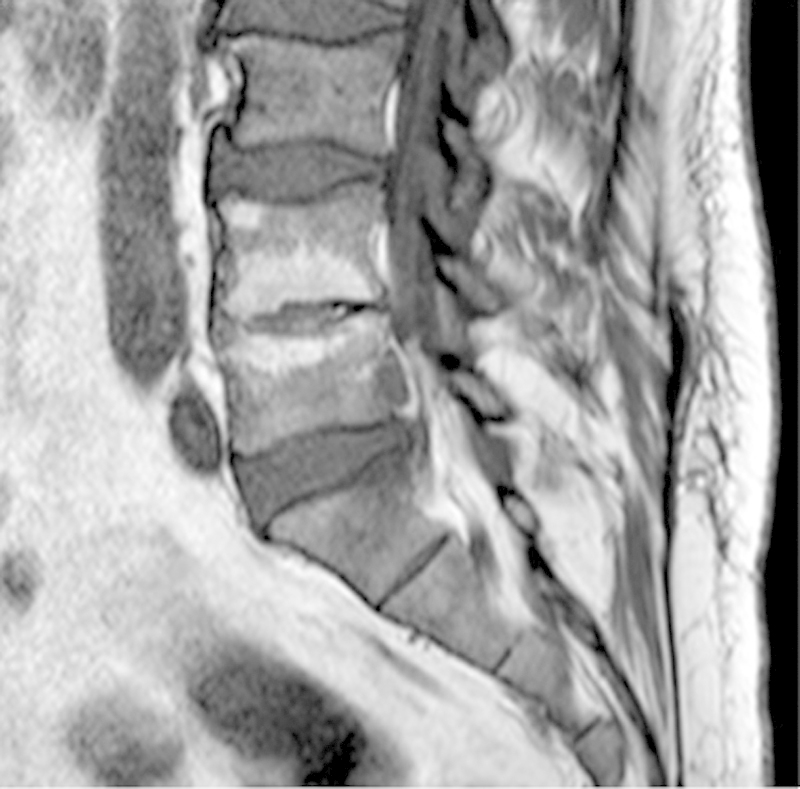
Preoperative nuclear magnetic resonance T1-weighted turbo spin-echo.
Fig. 6.

Preoperative nuclear magnetic resonance short T1 inversion recovery long TE.
Fig. 7.
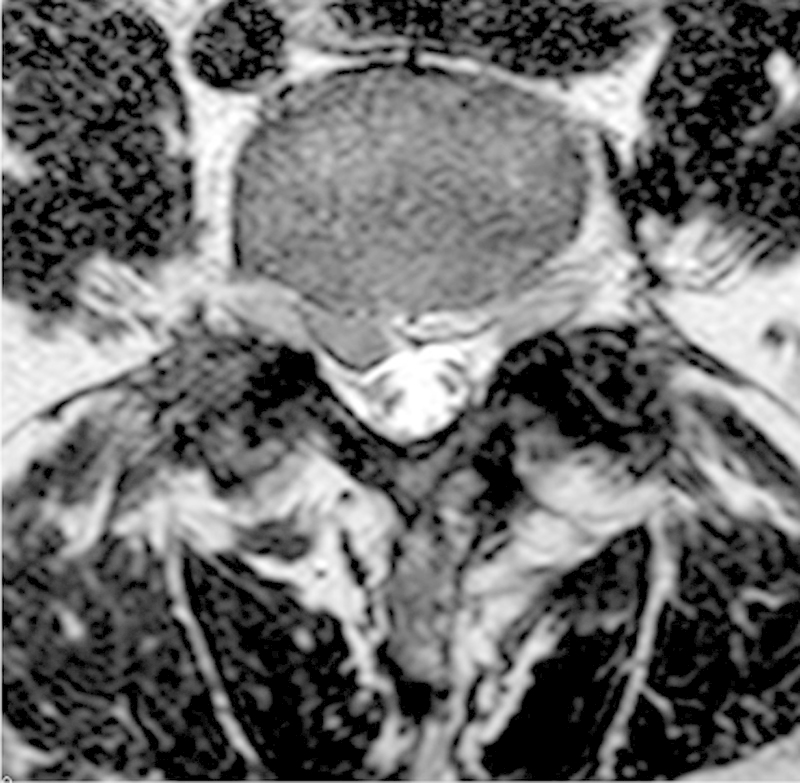
Preoperative (axial view).
Fig. 8.
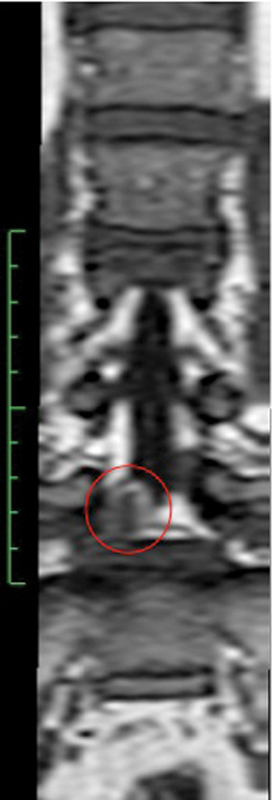
Preoperative nuclear magnetic resonance T1-weighted turbo spin-echo (coronal view).
Fig. 9.
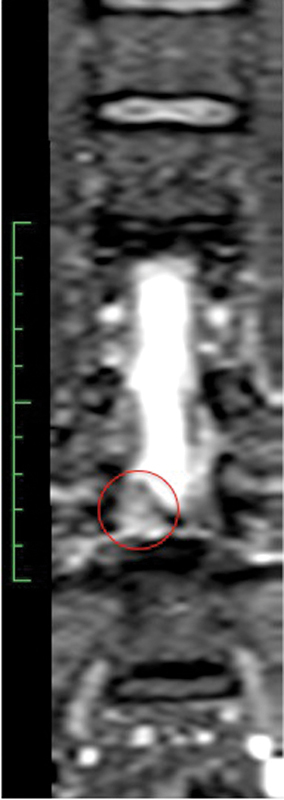
Preoperative nuclear magnetic resonance T2-weighted turbo spin-echo (coronal view).
A clinical follow-up was performed at 1, 3, 6, and 12 months using the visual analog scale (VAS) and the Oswestry Disability Index (ODI). All patients were evaluated according to the Spangfort criteria.11 Postoperative radiographic evaluations were made at 1, 6, and 12 months (dynamic radiographic studies were performed in the last two visits).
Institutional review board approval was not necessary because our work was a retrospective study.
Surgical Technique
After induction of general anesthesia, the patient is placed in a prone position on the surgical table. A positioning device for spinal surgery is used that avoids abdominal compression to prevent the congestion of the perivertebral venous plexus and to reduce the intraoperative bleeding. Under fluoroscopy, the intervertebral space to treat is identified using a 25-gauge spinal needle.
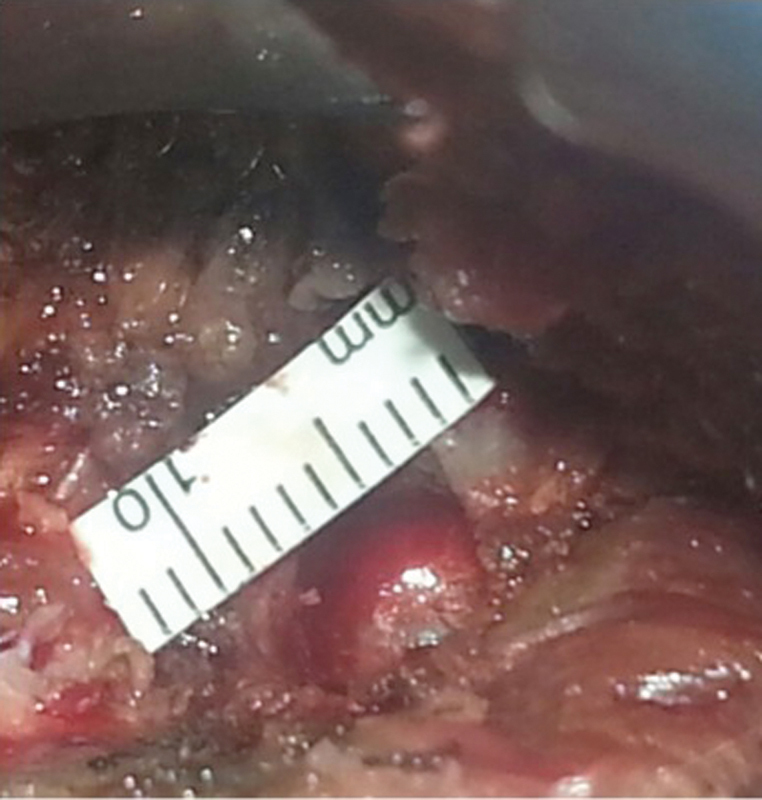
Accurate preoperative planning is essential. Through a three-dimensional CT reconstruction, it is possible to exactly identify the position of the fragment, which is mandatory to accurately place a translaminar hole just above the fragment. After the subcutaneous infiltration of lidocaine, a paramedian skin incision is performed. The infiltration is done not for analgesic purpose, but to decrease the capillary bleeding at the time of the skin incision and especially to limit the risk of telangiectasia, skin hyperpigmentation, and hematomas after surgery. Using a miniaturized Caspar-type speculum-counter-retractor system (Piccolino; Medicon, Tuttlingen, Germany), a mini-invasive approach is used (skin incision average length: 1 cm) to reduce the dissection of the paravertebral muscles and the resulting denervation. Subsequently, the muscular fascia is cut ∼5 mm from the midline, and the fascial splitting is completed in a semicircular manner. The paraspinal muscles are elevated subperiosteally, exposing the lamina and the flavum ligament. Through a 4-mm diamond dust-coated burr, a translaminar hole (8 ± 2 mm) is made, with subsequent exposure of the involved root (Figs. 10, 11, 12). The placement of the hole must respect Reulen parameters (Fig. 13)12: the average width of the isthmus (x1) in L3 is 15.4 mm; in L4 is 18.2 mm; and in L5 is 22 mm; the average distance from lateral margin of the isthmus to lateral border of the vertebral body (x2) in L3 is 6.3 mm; in L4 is 4.8 mm; and in L5 is 2.8 mm; and the average height of the lamina (y) in L3 is 23.1 mm; in L4 is 21.2 mm; and in L5 is 17.3 mm. In fact, the width of the lamina gradually decreases in a cranial-caudal direction, whereas that of the isthmus increases. For this reason, the translaminar fenestration should be more medial and oval-shaped, in the caudal-cranial direction. This is mandatory to avoid fractures of the pars interarticularis. Progressively, the epidural space is reached and the root must be carefully dissected away. The disk fragment can be removed (Fig. 14), with care taken to avoid shattering it in small pieces. Through a Caspar rongeurs with angulated up-biting or down-biting jaws (jaw size 3 mm), the lateral recess must be explored and any other small disk fragments must be removed. With this approach, facetectomies, laminectomies, laminotomies, and flavectomies are not necessary. If the disk fragment is too large to pass through the fenestration, it is possible to gradually cut it outside of the translaminar hole. Epidural bleeding may typically occur after the extraction of the fragment, in which case a fibrin glue can be used.
Fig. 10.
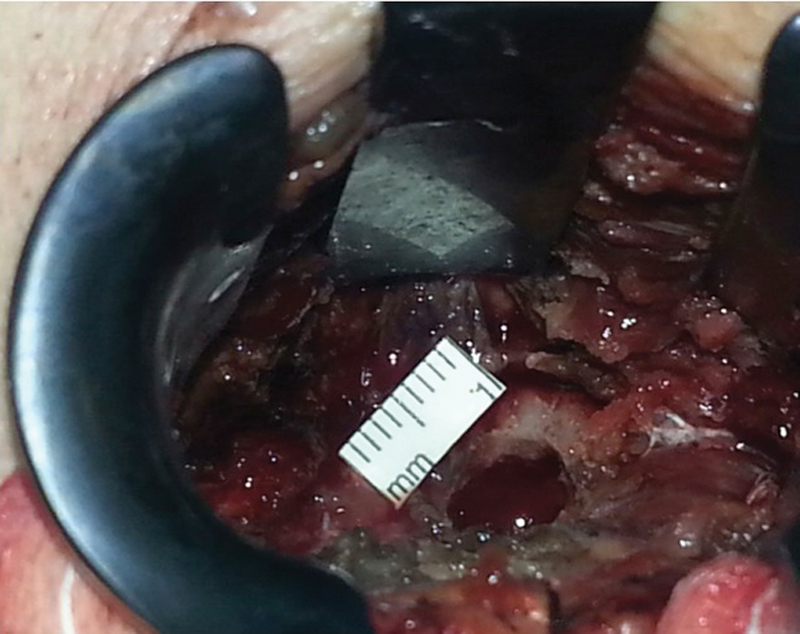
Intraoperative image.
Fig. 11.

Intraoperative image.
Fig. 12.
Intraoperative image.
Fig. 13.
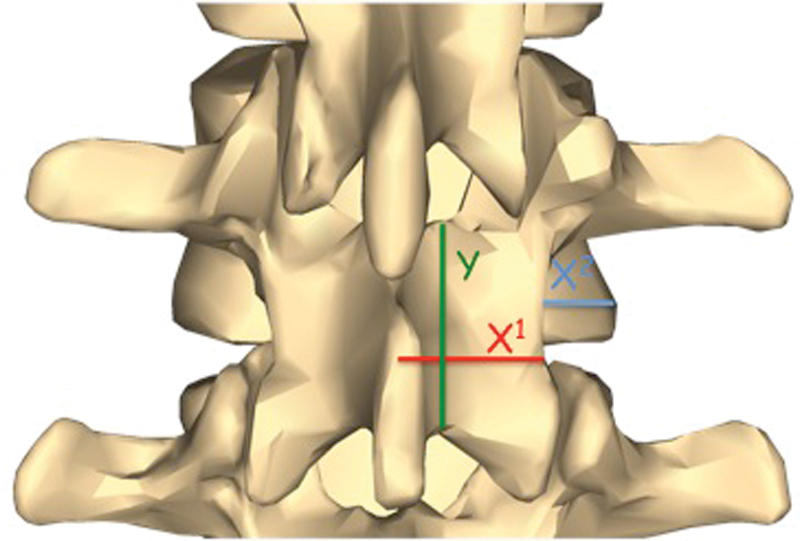
Reulen's criteria.
Fig. 14.

Herniated disk fragment.
Clinical follow-up at 1, 3, 6, and 12 months was performed using the VAS and the ODI.13 Postoperative radiographic evaluations were done at 1, 6, and 12 months, and dynamic radiographic studies were performed in the last two visits. After surgery, the patients were evaluated according to the Spangfort criteria.11
Results
The affected root was evaluated in all the patients. Although a window of only 8 ± 2 mm was available, it was possible to identify the root in all patients and cautiously dissect it from the herniated fragment. The integrity of the root was always verified, especially after the removal of the fragment. Any adhesions or residual small fragments were removed. In addition to the translaminar approach, a microsurgical foraminotomy can be performed if necessary. None of the patients had partial or total facetectomies, laminectomies, laminotomies, or flavectomies. Severe intraoperative bleeding (mandating use of local hemostatic agents) occurred in only 5% of cases, as a result of the involvement of the epidural veins. However, this complication did not prolong the surgical time significantly (mean time: 60 ± 10 minutes). The patients showed a gradual resolution of the back pain and a progressive resolution of the radicular pain and neurologic deficits.
All patients were evaluated according to Spangfort score.11 Twenty-nine patients (76%) reported complete relief of symptoms (grade I); 8 patients (21%) reported only a mild discomfort, and they were able to participate in all life activities without requiring any medications or orthopedic braces (grade II). In only 1 case (3%), the patient was not able to leave the Codivilla spring due to a persistence of the radicular deficit of L5 after surgery (grade III). No patient was classifiable as stage IV. All the data are summarized in Table 1.
Table 1. Spangfort's criteria.
| Grade | Result | Definition | n (%) |
|---|---|---|---|
| I | Excellent | Complete relief of symptoms, back to normal | 29 (76%) |
| II | Good | Mild discomfort, able to participate in all activities; does not require medications or bracing | 8 (21%) |
| III | Fair | Better than preoperative condition, significant limitations of activities, and/or requires medications and/or bracing | 1 (3%) |
| IV | Poor | No better than preoperative status, unable to return to work | 0 (0%) |
All the patients were able to resume work within 30 days of the surgery. No fractures of the laminae or pars interarticularis were reported. In addition, no sign of radiographic instability was documented during the follow-up. In the cases of previous instability, no radiographic signs of worsening were documented. No infections, dural tears, or spinal cord injuries occurred. No revision surgery was performed.
Discussion
A cranially extruded LDH implies a fragment migrated cranially into the preforaminal or foraminal areas. In 1971, Macnab introduced the term hidden areas to characterize this unusual position that is hard to reach.14 In these cases, the surgical approach remains debatable. In fact, the standard technique described by Caspar et al entails wide laminotomies or laminectomies and partial or total facetectomies.15 Therefore, a fusion is mandatory to avoid iatrogenic instability.16 17 This approach may involve severe intraoperative bleeding and long surgical times, leading to increased postoperative pain, convalescence, and risk of complications. Therefore, a minimally invasive approach must always be preferred.18 However, the stability of the spine is not based only on the articular joints and the laminae (together with the interspinous-supraspinous ligament complex). The flavum ligament acts as the main dynamic stabilizer of the posterior column.19 A flavum ligament-sparing approach confers several effects and advantages, because the roles of the flavum ligament are various.
Proprioception: high threshold dynamic mechanoreceptors, able to accomplish low adjustment, are contained in the flavum ligament.20
Protection: the ligament avoids spinal cord damage, especially during flexion-extension motions.21
Stability: the flavum ligament is the essential stabilizer of the lumbar spine,22 23 and especially at the level L4–L5 it is involved in the translational control of the angular and segmental motion.24 Adams et al showed that at full flexion, the interspinous and supraspinous ligaments contribute only 19% to stability in bending.25
Risk of bleeding: the removal of the flavum ligament can promote epidural bleeding, causing acute compressions of the roots or spinal cord (due to epidural hematoma) and/or iatrogenic stenosis (due to fibrosis).26
Postoperative complications and the risk of recurrence: in a microdiskectomy according to Caspar standard technique,15 the complication rate ranges from 3.3 to 18%, the reoperation rate from 5.1 to 9.33%, and the recurrence rate from 2.3 to 12.5%.27 28 29 30 31 32 33 34 Askar et al showed that in cases of preservation of the flavum ligament, the complication rate decreases to 1.75%, the reoperation rate to 2.63%, and the recurrence rate to 1.75%.19 These data are comparable with that obtained by Aydin et al, who noted a complication rate of 2.25%, a reoperation rate of 4.5%, and a recurrence rate of 1.75%.28
The translaminar approach is a mini-invasive but above all a tissue-sparing technique (Fig. 15).18 19 In 1998, Di Lorenzo et al described a different technique, founded on a fenestration at the level of the pars interarticularis.35 Soldner et al used a similar approach, but this technique is considered a combined interlaminar exposure.9 Correct selection of patients and accurate preoperative planning are mandatory. Therefore, the MRI is necessary to identify the herniated fragment that cranially migrated in the preforaminal or foraminal zone, called the “second window of McCulloch.”36 The lumbar spine is made up by the vertebral body and the disk below. According to McCulloch,36 a “three-story anatomic house” is formed. The first story is the disk level. The second story, between the upper rim of the disk space and the lower border of the cephalad pedicle, is the foraminal level and is covered by the lamina. The third story is the pedicle level (Fig. 16).18 The coronal scans are useful to characterize the fragment position and to identify any compression of the roots. The translaminar approach is not indicated in cases of disk herniations located in the first or third window of McCulloch.36
Fig. 15.
Standard versus translaminar approach.
Fig. 16.
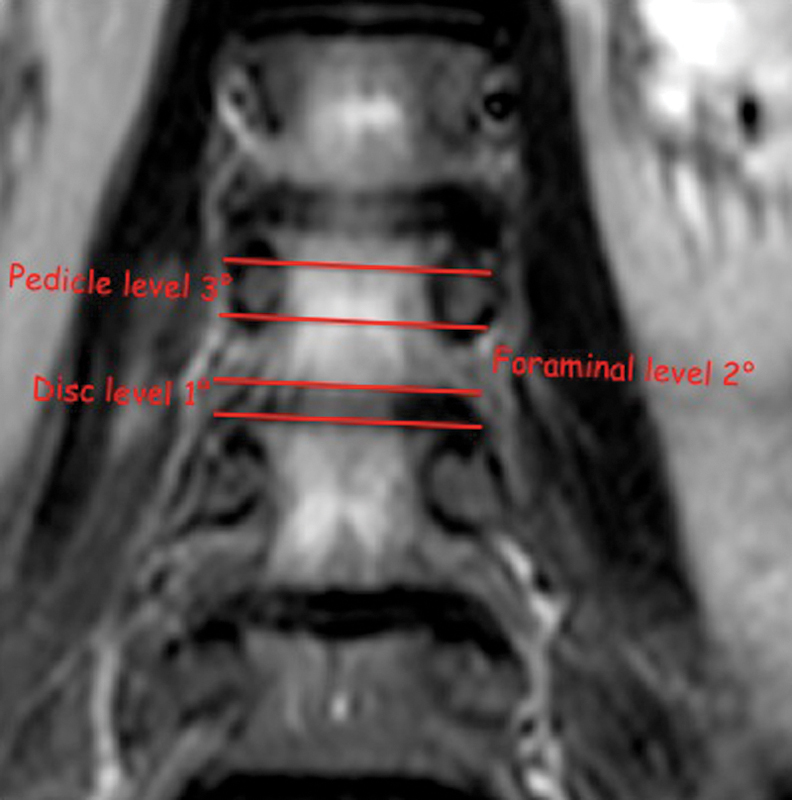
McCulloch's windows.
Finally, the CT examination is useful to exclude boney abnormalities (congenital or acquired) that contraindicate this approach (i.e., lateral recess stenosis and foraminal spondylosis). As the hole is placed a few millimeters from the pars interarticularis, the fracture risk is considerably reduced compared with the technique of Di Lorenzo et al.35 In our experience, none of patients complained of low back pain, and the dynamic radiograph showed no fracture or sign of instability.
For the preoperative planning, it is mandatory to consider the lamina and isthmus width, which vary depending on the lumbar intervertebral space. The width of the lamina gradually decreases in a cranial-caudal direction, whereas the width of the isthmus increases (according to Reulen et al).12 37 According to Ikuta et al,38 this implies that in the levels above L2–L3, the overlapping space between the lamina and the intervertebral disk progressively increases, whereas the degree of the foramen coverage by the lamina decreases. In the levels below L3–L4, the opposite occurs.38 For these reasons, the fenestration should be more medial and oval-shaped, in the caudocranial direction.18
Conclusion
Surgical microdiskectomy allows the successful treatment of patients affected by LDH. If possible, the surgical treatment of low back pain and the resolution of the disk-root conflict should always be done conservatively. According to the standard approach, in case of disk herniations in the hidden zone, this is rarely possible. In these cases, a minimally invasive approach to respect the spine anatomy and biomechanics becomes the gold standard.
The translaminar approach is the only “tissue-sparing” technique (Fig. 6) viable in cases of cranially migrated LDH encroaching on the exiting nerve root in the preforaminal zones,37 38 39 for the levels above L2–L3, and in the preforaminal and foraminal zones, for the levels below L3–L4 (L5–S1 included, if a total microdiskectomy is not necessary).39
This approach is more effective than the standard one, because it resolves the symptoms; it is associated with less postoperative pain and faster recovery times without the risk of iatrogenic instability, and it can also be used in cases with previous signs of radiographic instability. The possibility to spare the flavum ligament is one of the main advantages of this technique.9 18 According to our experience, the translaminar approach is a valid technique in terms of safety and efficacy.
Footnotes
Disclosures Daniele Vanni, none Francesco S. Sirabella, none Matteo Guelfi, none Andrea Pantalone, none Renato Galzio, none Vincenzo Salini, none Vincenzo Magliani, none
References
- 1.Kamper S J, Ostelo R W, Rubinstein S M. et al. Minimally invasive surgery for lumbar disc herniation: a systematic review and meta-analysis. Eur Spine J. 2014;23(5):1021–1043. doi: 10.1007/s00586-013-3161-2. [DOI] [PubMed] [Google Scholar]
- 2.Ma D, Liang Y, Wang D. et al. Trend of the incidence of lumbar disc herniation: decreasing with aging in the elderly. Clin Interv Aging. 2013;8:1047–1050. doi: 10.2147/CIA.S49698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schultz A, Andersson G, Ortengren R, Haderspeck K, Nachemson A. Loads on the lumbar spine. Validation of a biomechanical analysis by measurements of intradiscal pressures and myoelectric signals. J Bone Joint Surg Am. 1982;64(5):713–720. [PubMed] [Google Scholar]
- 4.Garrido E, Connaughton P N. Unilateral facetectomy approach for lateral lumbar disc herniation. J Neurosurg. 1991;74(5):754–756. doi: 10.3171/jns.1991.74.5.0754. [DOI] [PubMed] [Google Scholar]
- 5.Abdullah A F, Wolber P G, Warfield J R, Gunadi I K. Surgical management of extreme lateral lumbar disc herniations: review of 138 cases. Neurosurgery. 1988;22(4):648–653. doi: 10.1227/00006123-198804000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Fankhauser H, de Tribolet N. Extreme lateral lumbar disc herniation. Br J Neurosurg. 1987;1(1):111–129. doi: 10.3109/02688698709034347. [DOI] [PubMed] [Google Scholar]
- 7.Faulhauer K, Manicke C. Fragment excision versus conventional disc removal in the microsurgical treatment of herniated lumbar disc. Acta Neurochir (Wien) 1995;133(3–4):107–111. doi: 10.1007/BF01420059. [DOI] [PubMed] [Google Scholar]
- 8.Seiz M, Pechlivanis I, Bag S, Schmieder K, Thome C, Tuettenberg J. [Translaminar fenestration for caudally herniated lumbar discs—a technical note] Z Orthop Unfall. 2009;147(5):597–599. doi: 10.1055/s-0029-1186107. [DOI] [PubMed] [Google Scholar]
- 9.Soldner F, Hoelper B M, Wallenfang T, Behr R. The translaminar approach to canalicular and cranio-dorsolateral lumbar disc herniations. Acta Neurochir (Wien) 2002;144(4):315–320. doi: 10.1007/s007010200043. [DOI] [PubMed] [Google Scholar]
- 10.Hansson T, Suzuki N, Hebelka H, Gaulitz A. The narrowing of the lumbar spinal canal during loaded MRI: the effects of the disc and ligamentum flavum. Eur Spine J. 2009;18(5):679–686. doi: 10.1007/s00586-009-0919-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spangfort E V. The lumbar disc herniation. A computer-aided analysis of 2,504 operations. Acta Orthop Scand Suppl. 1972;142:1–95. doi: 10.3109/ort.1972.43.suppl-142.01. [DOI] [PubMed] [Google Scholar]
- 12.Reulen H J, Pfaundler S, Ebeling U. The lateral microsurgical approach to the “extracanalicular” lumbar disc herniation. I: A technical note. Acta Neurochir (Wien) 1987;84(1–2):64–67. doi: 10.1007/BF01456353. [DOI] [PubMed] [Google Scholar]
- 13.Chung E J, Hur Y G, Lee B H. A study of the relationship among fear-avoidance beliefs, pain and disability index in patients with low back pain. J Exerc Rehabil. 2013;9(6):532–535. doi: 10.12965/jer.130079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Macnab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am. 1971;53(5):891–903. [PubMed] [Google Scholar]
- 15.Caspar W Campbell B Barbier D D Kretschmmer R Gotfried Y The Caspar microsurgical discectomy and comparison with a conventional standard lumbar disc procedure Neurosurgery 199128178–86., discussion 86–87 [DOI] [PubMed] [Google Scholar]
- 16.Kotilainen E, Valtonen S. Clinical instability of the lumbar spine after microdiscectomy. Acta Neurochir (Wien) 1993;125(1–4):120–126. doi: 10.1007/BF01401838. [DOI] [PubMed] [Google Scholar]
- 17.Padua R, Padua S, Romanini E, Padua L, de Santis E. Ten- to 15-year outcome of surgery for lumbar disc herniation: radiographic instability and clinical findings. Eur Spine J. 1999;8(1):70–74. doi: 10.1007/s005860050129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Papavero L Langer N Fritzsche E Emami P Westphal M Kothe R The translaminar approach to lumbar disc herniations impinging the exiting root Neurosurgery 200862301173–177., discussion 177–178 [DOI] [PubMed] [Google Scholar]
- 19.Askar Z, Wardlaw D, Choudhary S, Rege A. A ligamentum flavum-preserving approach to the lumbar spinal canal. Spine (Phila Pa 1976) 2003;28(19):E385–E390. doi: 10.1097/01.BRS.0000085100.10349.15. [DOI] [PubMed] [Google Scholar]
- 20.Olszewski A D, Yaszemski M J, White A A III. The anatomy of the human lumbar ligamentum flavum. New observations and their surgical importance. Spine (Phila Pa 1976) 1996;21(20):2307–2312. doi: 10.1097/00007632-199610150-00001. [DOI] [PubMed] [Google Scholar]
- 21.Losiniecki A J, Serrone J C, Keller J T, Bohinski R J. Lumbar ligamentum flavum: spatial relationships to surrounding anatomical structures and technical description of en bloc resection. J Neurol Surg A Cent Eur Neurosurg. 2013;74(6):388–392. doi: 10.1055/s-0033-1348350. [DOI] [PubMed] [Google Scholar]
- 22.Chau A M, Pelzer N R, Hampton J. et al. Lateral extent and ventral laminar attachments of the lumbar ligamentum flavum: cadaveric study. Spine J. 2014;14(10):2467–2471. doi: 10.1016/j.spinee.2014.03.041. [DOI] [PubMed] [Google Scholar]
- 23.Pintar F A, Yoganandan N, Myers T, Elhagediab A, Sances A Jr. Biomechanical properties of human lumbar spine ligaments. J Biomech. 1992;25(11):1351–1356. doi: 10.1016/0021-9290(92)90290-h. [DOI] [PubMed] [Google Scholar]
- 24.Kong M H, Morishita Y, He W. et al. Lumbar segmental mobility according to the grade of the disc, the facet joint, the muscle, and the ligament pathology by using kinetic magnetic resonance imaging. Spine (Phila Pa 1976) 2009;34(23):2537–2544. doi: 10.1097/BRS.0b013e3181b353ea. [DOI] [PubMed] [Google Scholar]
- 25.Adams M A, Hutton W C, Stott J RR. The resistance to flexion of the lumbar intervertebral joint. Spine (Phila Pa 1976) 1980;5(3):245–253. doi: 10.1097/00007632-198005000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Okuda T, Fujimoto Y, Tanaka N, Ishida O, Baba I, Ochi M. Morphological changes of the ligamentum flavum as a cause of nerve root compression. Eur Spine J. 2005;14(3):277–286. doi: 10.1007/s00586-004-0782-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tullberg T, Isacson J, Weidenhielm L. Does microscopic removal of lumbar disc herniation lead to better results than the standard procedure? Results of a one-year randomized study. Spine (Phila Pa 1976) 1993;18(1):24–27. doi: 10.1097/00007632-199301000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Aydin Y Ziyal I M Duman H Türkmen C S Başak M Sahin Y Clinical and radiological results of lumbar microdiskectomy technique with preserving of ligamentum flavum comparing to the standard microdiskectomy technique Surg Neurol 20025715–13., discussion 13–14 [DOI] [PubMed] [Google Scholar]
- 29.Andrews D W, Lavyne M H. Retrospective analysis of microsurgical and standard lumbar discectomy. Spine (Phila Pa 1976) 1990;15(4):329–335. doi: 10.1097/00007632-199004000-00015. [DOI] [PubMed] [Google Scholar]
- 30.Loupasis G A, Stamos K, Katonis P G, Sapkas G, Korres D S, Hartofilakidis G. Seven- to 20-year outcome of lumbar discectomy. Spine (Phila Pa 1976) 1999;24(22):2313–2317. doi: 10.1097/00007632-199911150-00005. [DOI] [PubMed] [Google Scholar]
- 31.Pappas C TE, Harrington T, Sonntag V K. Outcome analysis in 654 surgically treated lumbar disc herniations. Neurosurgery. 1992;30(6):862–866. doi: 10.1227/00006123-199206000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Salenius P, Laurent L E. Results of operative treatment of lumbar disc herniation. A survey of 886 patients. Acta Orthop Scand. 1977;48(6):630–634. doi: 10.3109/17453677708994809. [DOI] [PubMed] [Google Scholar]
- 33.Thomas A M, Afshar F. The microsurgical treatment of lumbar disc protrusion. Follow-up of 60 cases. J Bone Joint Surg Br. 1987;69(5):696–698. doi: 10.1302/0301-620X.69B5.3680326. [DOI] [PubMed] [Google Scholar]
- 34.Yorimitsu E, Chiba K, Toyama Y, Hirabayashi K. Long-term outcomes of standard discectomy for lumbar disc herniation: a follow-up study of more than 10 years. Spine (Phila Pa 1976) 2001;26(6):652–657. doi: 10.1097/00007632-200103150-00019. [DOI] [PubMed] [Google Scholar]
- 35.Di Lorenzo N Porta F Onnis G Cannas A Arbau G Maleci A Pars interarticularis fenestration in the treatment of foraminal lumbar disc herniation: a further surgical approach Neurosurgery 199842187–89., discussion 89–90 [DOI] [PubMed] [Google Scholar]
- 36.McCulloch J A. Philadelphia, PA: Lippincott-Raven; 1998. Foraminal and extraforaminal lumbar disc herniations. In: Young PH, ed. Essentials of Spinal Microsurgery; pp. 385–387. [Google Scholar]
- 37.Reulen H J Müller A Ebeling U Microsurgical anatomy of the lateral approach to extraforaminal lumbar disc herniations Neurosurgery 1996392345–350., discussion 350–351 [DOI] [PubMed] [Google Scholar]
- 38.Ikuta K, Tono O, Senba H. et al. Translaminar microendoscopic herniotomy for cranially migrated lumbar disc herniations encroaching on the exiting nerve root in the preforaminal and foraminal zones. Asian Spine J. 2013;7(3):190–195. doi: 10.4184/asj.2013.7.3.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tessitore E de Tribolet N Far-lateral lumbar disc herniation: the microsurgical transmuscular approach Neurosurgery 2004544939–942., discussion 942 [DOI] [PubMed] [Google Scholar]


