Abstract
Study Design A retrospective analysis of a prospective database.
Objective Meta-analyses suggest that computer-assisted systems can increase the accuracy of pedicle screw placement for dorsal spinal fusion procedures. The results of further meta-analyses report that in the thoracic spine, both the methods have comparable placement accuracy. These studies are limited due to an abundance of screw classification systems. The aim of this study was to assess the placement accuracy and potentially influencing factors of three-dimensionally navigated versus conventionally inserted pedicle screws.
Methods This was a retrospective analysis of a prospective database at a level I trauma center of pedicle screw placement (computer-navigated versus traditionally placed) for dorsal spinal stabilizations. The cases spanned a 5.5-year study period (January 1, 2005, to June 30, 2010). The perforations of the pedicle were differentiated in three grades based on the postoperative computed tomography.
Results The overall placement accuracy was 86% in the conventional group versus 79% in the computer-navigated group (grade 0). The computer-navigated procedures were superior in the lumbar spine and the conventional procedures were superior in the thoracic spine, but both failed to be of statistical significance. The level of experience of the performing surgeon and the patient's body mass index did not influence the placement accuracy. The only significant influence was the spinal segment: the higher the spinal level where the fusion was performed, the more likely the screw was displaced.
Conclusions The computer-navigated and conventional methods are both safe procedures to place transpedicular screws at the traumatized thoracic and lumbar spine. At the moment, three-dimensionally based navigation does not significantly increase the placement accuracy.
Keywords: computer assisted pedicle screw placement, computer navigation, spine, pedicle screw, image based guidance
Introduction
Stabilizing the spine with dorsal transpedicular screws is an internationally accepted and commonly performed procedure.1 2 3 However, it remains challenging, and although rare, complications can have serious consequences for the patients.4 5 Navigation systems have been used in orthopedic surgery for over 20 years.6 Certain advantages have been reported, but still the worldwide distribution rate is low.7 8 A major reason may be the high costs; another reason may be that their superiority over conventional techniques has not been proven convincingly so far.7 Pedicle screw insertions were among the first procedures to be performed frequently with this relatively new technology, and abundant literature exists on the technology's advantages and disadvantages. Most of the studies in the literature are case series or they examine small numbers of patients and pedicle screws.9 10 11 12 The initial intention of computer-navigated techniques was to improve the placement accuracy of the pedicle screws and with it outcome parameters of surgical procedures, such as reduced neurologic complications and mechanical failures. Reports in the literature contradict its accuracy for placement of pedicle screws, questioning the main argument for using navigation in spine surgery.13 14
Pedicle screws are commonly used to stabilize both the traumatized spine and degenerative instabilities.15 The evidence for improved screw placement accuracy when using navigation systems is even thinner in spinal trauma in comparison with degenerative changes or mixed study groups.
Several types of navigation are available [i.e., computed tomography (CT), two-dimensional (2D), and three-dimensional (3D)], with 3D the most commonly used for the traumatized spine.6 14
Many factors other than technique potentially influence the accuracy of pedicle screw placement, such as the experience of the surgeon and the patient's body mass index (BMI).16 17
Our main hypothesis is that 3D-based navigation increases the accuracy of pedicle screw placement for dorsal spinal fusion. We further hypothesize that the patient's BMI and the surgeon's experience influence the rate of screw misplacements.
Materials and Methods
A retrospective analysis of a prospective database during a 5.5-year study period (January 1, 2005, to June 30, 2010) was conducted at a level I trauma center on all computer-navigated and conventionally placed pedicle screws for spinal fusion procedures. The inclusion criteria consisted of all patients who had pedicle screws placed in the inclusion period (Table 1). The exclusion criteria were fixation without pedicle screws, missing postoperative CT, and 2D and CT-based navigation.
Table 1. Demographic data of patients treated with and without assistance of a navigation system.
| Demographic | Without navigation (n = 250, 59.6% male) |
With navigation (n = 202, 64.9% male) |
Total (n = 452, 61.9% male) |
p | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Median | SD | Min | Max | Mean | Median | SD | Min | Max | Mean | Median | SD | Min | Max | ||
| Age (y) | 49.3 | 50 | 18.1 | 16 | 89 | 51.6 | 53 | 19.6 | 16 | 88 | 50.4 | 51 | 18.8 | 16 | 89 | 0.20 |
| Body weight (kg) | 75.3 | 75 | 14.2 | 40 | 130 | 77.4 | 75 | 14.2 | 45 | 134 | 76.2 | 75 | 14.2 | 40 | 134 | 0.12 |
| BMI (kg/m2) | 25.5 | 25 | 4.5 | 15.6 | 45.9 | 25.9 | 25.2 | 4.6 | 14.5 | 47.5 | 25.7 | 25.1 | 4.5 | 14.5 | 47.5 | 0.39 |
Abbreviations: BMI, body mass index; Max, maximum; Min, minimum; SD, standard deviation.
Patients were not randomized to the groups. The decision to use or not to use a navigation system was discussed in a conference the day before surgery and depended on the spinal level and the surgeon's preference as well as the experience with the different techniques. The indication for the surgical treatment was based on the clinical findings and the preoperative imaging, which consisted in the majority of cases in a CT in addition to conventional X-ray images and additional magnetic resonance images.
Surgical Technique in the Computer-Navigated Group
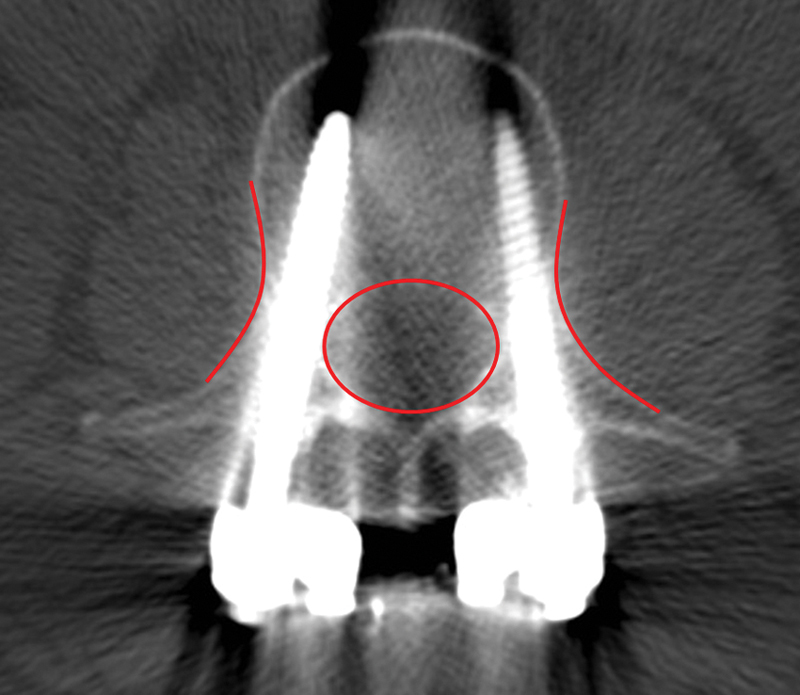
Patients were placed in a prone position on a radiolucent carbon table. Using lateral fluoroscopic images, the surgical approach was determined and marked prior to fixing the sterile drapes to the surgical site. Via a midline approach, the dorsal spinal segments were visualized. A reference clamp was attached to the spinous process, in most cases at the most caudal vertebra. Next, a 3D scan was performed. The data were transferred automatically to the workstation of the navigation system (Vector Vision, Brainlab, Feldkirch, Germany). The data set was verified with a navigation pointer. Then screw placement was planned, following the steps of the navigation software. The pedicle was opened with either a computer-navigated awl or drill guide. The bone channel was tested with a non-navigated ball tip probe. Finally, using a navigated hand drill, the screw was inserted following the previously determined trajectory (Fig. 1). In addition to the navigation system, the screws were controlled with fluoroscopic images in 2D mode in both the anteroposterior and lateral planes.
Fig. 1.
All screws were analyzed with postoperative computed tomography. All perforations were measured using the PACS (picture archiving and communication system) of the hospital (perforations were measured in mm). A screw without perforation (complete intraosseous) in transverse, sagittal, and frontal plane was classified as “grade 0.”
Surgical Technique in the Conventional Group
Patients were placed in a prone position on a radiolucent carbon table. Using lateral fluoroscopic images, the surgical approach was determined and marked prior to fixing the sterile drapes to the surgical site. Via a midline approach, the dorsal spinal segments were visualized. The entry point was determined under anteroposterior fluoroscopic control. The pedicle was opened either with an awl or a drill. Then the bone channel was tested with a ball tip probe. Screw depth was determined under lateral fluoroscopic control.
During the study period, the same pedicle screws and instruments were used in both the groups (Universal Spine System, Synthes, Umkirch, Germany). Two different fluoroscopes were used in both the groups (Iso-C 3D or Arcadis Orbic 3D, both Siemens, Erlangen, Germany), although the C-arms were used in 2D mode in the conventional group. Surgeons were free to perform an intraoperative 3D scan to control the final result, which was done in less than 10% in both groups.
All patient-related data as documented in the patients' files were recorded as well as all complications and revision surgeries in the study period. All included patients received a postoperative CT with multiplanar reconstruction and a slice thickness of 1 mm of the fused region to control the position of the implant in the sagittal, coronal, and transverse plane.
The images were analyzed by a blinded viewer (J.W.), and the position of the screw was determined regarding the distance to the medial and lateral bone margin of the pedicle and the position of the tip of the screw in the vertebral body (Figs. 1 and 2). In an unclear situation, which was the case with only 24 screws, a second viewer (M.K.) reassessed the grading and both viewers had to agree. Perforations of the pedicle were differentiated in three grades: grade 0, accurate (no breach of the compact tissue); grade 1, perforation less than 2 mm; grade 2, perforation of 2 mm or more.
Fig. 2.
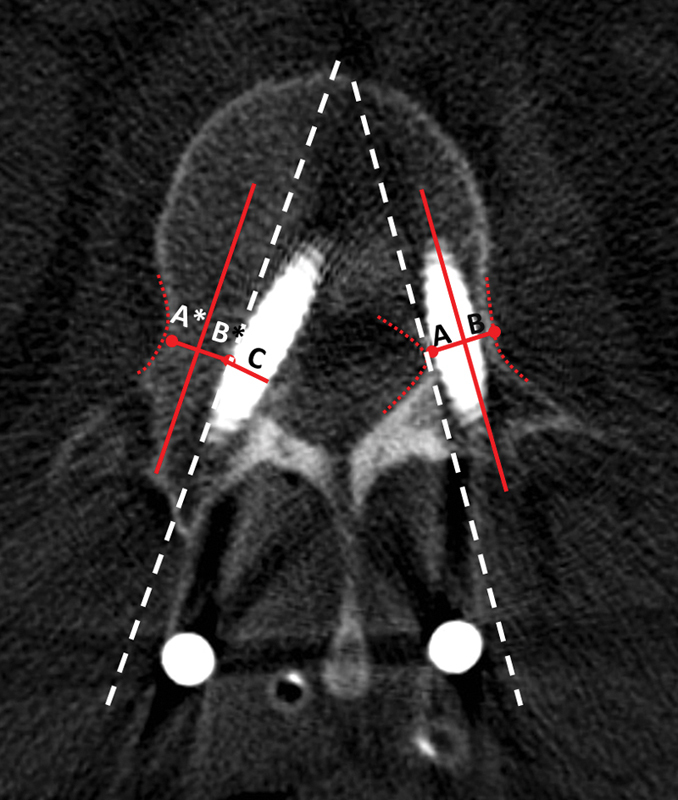
All perforations were measured in mm. If the perforated part of the pedicle was not visible due to interferences caused by the screw, the diameter of the nonperforated side was measured, serving as reference (A and B). Assuming a similar pedicle size on the perforated side, these distances were used to define the invisible pedicle wall on the perforated side (A* and B* = A and B). Then the magnitude of the perforation was determined (C). (Red line: midline of the pedicle; dashed white line: assumed pedicle wall; dotted red line: exactly definable bony margins).
Statistical Methods
Continuous variables were summarized as means, standard deviations, medians, minimums and maximums. Nominal and ordinal variables were analyzed using frequencies. The group comparisons for nominal variables at the patient's level were performed using the chi-square test or Fisher exact test as appropriate. The group comparisons for continuous variables at the patient's level were performed using the two-sample t test. For regression analyses, the perforation of the pedicle was dichotomized: grade 0 and grade 1 were summarized in one category, and grade 2 was the other category. The influence of the group (3D-navigated versus conventional), segments of the spine, BMI, and level of experience were analyzed using mixed-effects regression analysis. Mixed-effects regression models for a binary outcome were used for the investigation of the mentioned variables influencing perforation of the pedicle. In all regression models, the single patient is included as random effect.
Statistical analyses were performed using SAS 9.2 (SAS Institute, Cary, North Carolina, United States). PROC GLIMMIX was used to fit the mixed-effects regression models. Because of the explorative nature of this study, no adjustment for multiple testing was made. A p value less than 0.05 was considered as significant. The results of all the statistical tests are interpreted in an exploratory sense.
Results
If not stated otherwise, all values are reported as mean ± standard deviation (minimum; maximum). During the 5.5-year study period, 461 patients were identified in the database. Using the previously mentioned inclusion and exclusion criteria, 452 (98%) patients with a total of 2,021 pedicle screws were included. Due to incomplete or missing postoperative imaging of these, 2,003 (99%) pedicle screws were analyzed. The demographic data in both groups were comparable (Table 1). In the conventional group, 250 patients received a total of 1,069 screws, and 934 pedicle screws were inserted with 3D navigation. The main reasons for surgery were trauma-related fractures of the spine followed by malignant processes needing surgical intervention (Table 2). It took on average 12 minutes longer to navigate the procedure [109.3 ± 50.4 (40; 321) minutes versus 97.3 ± 49.1 (30; 300) minutes]. There were no differences between the groups regarding the duration of inpatient treatment [15.8 ± 9.2 (4; 58) days for conventional cases versus 16.0 ± 9.7 (1; 73) days, p = 0.85]. In the conventional group, 36 patients (14.4%) were fused ventrally, 12 of which were done in the same session, compared with 5 patients (7.4%) in the computer-navigated group, 9 of which were done in the same procedure as the dorsal fusion. The rate of patients undergoing laminectomy was not comparable in both groups: 69 patients (27.6%) in the conventional group versus 39 (19.3%; p = 0.04).
Table 2. Reasons for surgical posterior fusion.
| Reasons | Without navigation | With navigation | Total | p | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Fracture, fall from a height | 128 | 51 | 90 | 44.3 | 218 | 48 | 0.17 |
| Fracture, traffic accident | 53 | 21.1 | 53 | 26.1 | 106 | 23.3 | 0.21 |
| Tumor | 47 | 18.7 | 40 | 19.7 | 87 | 19.2 | 0.79 |
| Other | 23 | 9.2 | 20 | 9.9 | 43 | 9.5 | 0.80 |
| Total | 251 | 100 | 203 | 100 | 454 | 100 | |
In the conventional group, 27 patients (10.8%) had a preoperative neurologic disorder compared with 21 patients (10.4%) in the computer-navigated group. Postoperatively, 3 patients in the conventional group (1.2%) and 2 patients in the computer-navigated group (1.0%) had a procedure-related neurologic deficit. Other complications were comparably low for both modalities, although there were no mechanical implant failures in the computer-navigated group, whereas 5 patients receiving 23 screws in the conventional group needed surgical revision due to mechanical failure (Table 3).
Table 3. Screw-associated and general complications with and without surgical revision.
| Complication | Conventional | 3D navigated | Total | p | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Revisions | 21 | 8.4 | 9 | 4.5 | 30 | 6.6 | 0.09 |
| Screw associated complications undergoing surgical revision | |||||||
| Inacceptable position | 4 | 1.6 | 2 | 1.0 | 6 | 1.3 | 0.70 |
| Mechanical failure | 5 | 2.0 | 0 | 0.0 | 5 | 1.1 | 0.07 |
| General complications undergoing surgical revision | |||||||
| Wound-healing disorder | 3 | 1.2 | 3 | 1.5 | 6 | 1.3 | >0.99 |
| Deep infection | 4 | 1.6 | 4 | 2.0 | 8 | 1.8 | >0.99 |
| Bleeding | 1 | 0.4 | 1 | 0.5 | 2 | 0.4 | >0.99 |
| Intraspinal fragment | 7 | 2.8 | 1 | 0.5 | 8 | 1.8 | 0.08 |
| General complications without surgical intervention | |||||||
| Neurologic | 1 | 0.4 | 1 | 0.5 | 2 | 0.4 | >0.99 |
| Vascular | 1 | 0.4 | 0 | 0.0 | 1 | 0.2 | >0.99 |
Abbreviation: 3D, three-dimensionally.
Note: % = percent of all patients of the respective group.
The majority of screws were implanted in the thoracolumbar junction with a clear tendency to use the navigation system for procedures at the high thoracic spine (Table 4). The only parameter that significantly influenced the accuracy of pedicle screw placement was the spinal level. The accuracy of screw placement in the high thoracic spine (T1–T6) was significantly lower in comparison with screws in the thoracolumbar junction [T12–L1: odds ratio 4.283, 95% confidence interval (CI) 2.617 to 7.008, p < 0.01] and the lumbar spine (odds ratio 3.583, 95% CI 1.851 to 6.937; p < 0.01). Comparing screws of the higher thoracic levels (T1–T6) and the lower thoracic levels (T7–T10), there was a tendency of greater placement accuracy for lower levels without a statistically significant distinction (odds ratio 1.489, 95% CI 0.901 to 2.460; p = 0.12). Screws implanted in lower levels of the thoracic spine (T7–T10) were more likely to be placed inaccurately than screws in the lumbar spine (odds ratio 2.407, 95% CI 1.236–4.685; p < 0.01). The data show no difference in placement accuracy between screws inserted in the first sacral vertebra and the lumbar spine (odds ratio 0.701, 95% CI 0.135 to 3.637, p = 0.67). Analyzing the screws using the “in versus out” grading, there was no significant difference between computer-navigated and conventionally implanted screws when comparing the overall placement accuracy of all spinal levels (odds ratio 0.820, 95% CI 0.523 to 1.285, p = 0.39). Dividing the spine in clinically relevant segments did not reveal significant differences between the two groups (T1–T6: odds ratio 1.057, 95% CI 0.414 to 2.698, p = 0.91; T7–T10: odds ratio 0.569, 95% CI 0.238 to 1.364, p = 0.21; T10–L2: odds ratio 0.687, 95% CI 0.354 to 1.337, p = 0.27; L3–L5: odds ratio 2.593, 95% CI 0.537 to 12.522, p = 0.23). Due to the small numbers of screws, no comparative statistical testing was done in the cervical spine. Differentiating between each single vertebra, there were surprisingly more accurately inserted pedicle screws in the conventional group for the thoracic vertebrae, whereas computer-navigated systems showed better results in the lumbar levels (Table 4). The majority of screws showed a ventral displacement of the vertebral body. In comparison with the non-navigated screws, the computer-navigated screws perforated significantly more often in the lateral aspect of the pedicle (p = 0.0001). Medial breeches were distributed evenly in both the groups (p = 0.996; Table 5).
Table 4. Number of screws of each instrumented vertebra and distribution on grades.
| Position | Grade 0 | Grade 1 | Grade 2 | Total | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Conventional | 3D navigated | Conventional | 3D navigated | Conventional | 3D navigated | ||||||||||
| Spinal level | Vertebra | n | % | n | % | n | % | n | % | n | % | n | % | Conventional (n) | 3D navigated (n) |
| Cervical | 1/2 | 0 | 0 | 9 | 90 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 10 | 0 | 10 |
| 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 4 | 2 | 100 | 2 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | |
| 5 | 4 | 100 | 4 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 4 | |
| 6 | 0 | 0 | 4 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | |
| 7 | 4 | 100 | 6 | 75 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 25 | 4 | 8 | |
| Subtotal (n) | 10 | 100 | 16 | 89 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 11 | 10 | 18 | |
| Thoracic | 1 | 2 | 100 | 14 | 88 | 0 | 0 | 1 | 6 | 0 | 0 | 1 | 6 | 2 | 16 |
| 2 | 3 | 75 | 15 | 68 | 0 | 0 | 2 | 9 | 1 | 25 | 5 | 23 | 4 | 22 | |
| 3 | 5 | 71 | 32 | 68 | 0 | 0 | 8 | 17 | 2 | 29 | 7 | 15 | 7 | 47 | |
| 4 | 6 | 75 | 23 | 59 | 0 | 0 | 9 | 23 | 2 | 25 | 7 | 18 | 8 | 39 | |
| 5 | 10 | 83 | 50 | 69 | 1 | 8 | 11 | 15 | 1 | 8 | 11 | 15 | 12 | 72 | |
| 6 | 13 | 72 | 41 | 68 | 2 | 11 | 10 | 17 | 3 | 17 | 9 | 15 | 18 | 60 | |
| 7 | 15 | 83 | 48 | 65 | 3 | 17 | 11 | 15 | 0 | 0 | 15 | 20 | 18 | 74 | |
| 8 | 27 | 75 | 36 | 72 | 5 | 14 | 8 | 16 | 4 | 11 | 6 | 12 | 36 | 50 | |
| 9 | 26 | 76 | 42 | 75 | 7 | 21 | 8 | 14 | 1 | 3 | 6 | 11 | 34 | 56 | |
| 10 | 32 | 82 | 33 | 79 | 2 | 5 | 7 | 17 | 5 | 13 | 2 | 5 | 39 | 42 | |
| 11 | 83 | 73 | 60 | 83 | 19 | 17 | 8 | 11 | 11 | 10 | 4 | 6 | 113 | 72 | |
| 12 | 155 | 89 | 76 | 84 | 16 | 9 | 6 | 7 | 4 | 2 | 8 | 9 | 175 | 90 | |
| Subtotal (n) | 377 | 81 | 470 | 73 | 55 | 12 | 89 | 14 | 34 | 7 | 81 | 13 | 466 | 640 | |
| Lumbar | 1 | 145 | 88 | 67 | 88 | 13 | 8 | 5 | 7 | 6 | 4 | 4 | 5 | 164 | 76 |
| 2 | 183 | 94 | 76 | 86 | 9 | 5 | 11 | 13 | 3 | 2 | 1 | 1 | 195 | 88 | |
| 3 | 91 | 89 | 39 | 93 | 6 | 6 | 2 | 5 | 5 | 5 | 1 | 2 | 102 | 42 | |
| 4 | 67 | 91 | 23 | 96 | 5 | 7 | 0 | 0 | 2 | 3 | 1 | 4 | 74 | 24 | |
| 5 | 29 | 73 | 21 | 88 | 5 | 13 | 3 | 13 | 6 | 15 | 0 | 0 | 40 | 24 | |
| Subtotal (n) | 515 | 90 | 226 | 89 | 38 | 7 | 21 | 8 | 22 | 4 | 7 | 3 | 575 | 254 | |
| Sacral | 1 | 16 | 89 | 12 | 100 | 0 | 0 | 0 | 0 | 2 | 11 | 0 | 0 | 18 | 12 |
| Total (n) | 918 | 86 | 724 | 78 | 93 | 9 | 110 | 12 | 58 | 5 | 90 | 10 | 1,069 | 934 | |
Abbreviation: 3D, three-dimensionally.
Note: % = percent of all screws of the respective vertebra of each method.
Table 5. Direction of screw perforationa .
| Perforation | Conventional | 3D navigated | |||
|---|---|---|---|---|---|
| Direction | Extent (mm) | n | % | n | % |
| Lateral | ≤2 | 40 | 3.7 | 54 | 5.8 |
| >2 | 30 | 2.8 | 67 | 7.2 | |
| Medial | ≤2 | 53 | 4.9 | 56 | 6.0 |
| >2 | 22 | 2.0 | 19 | 2.0 | |
| Superior | 4 | 0.4 | 1 | 0.1 | |
| Inferior | 2 | 0.2 | 1 | 0.1 | |
| Ventral | 60 | 5.6 | 75 | 8.0 | |
Abbreviation: 3D, three-dimensionally.
Ventral dislocation was often combined with lateral perforation, so one screw was able to count for two directions of perforation.
Other than the spinal level, no other examined modality influenced the accuracy of pedicle screw placement. A total of 16 surgeons performed the surgical procedures during the study period. They were classified depending on their level of experience in five grades; grade 1: less than 6 years of training, not specialized in orthopedic surgery; grade 2: specialized in orthopedic surgery but not a senior physician; grade 3: senior physician (more than 2 years after specialization); grade 4: spine surgeon (more than 50 cases in the inclusion period); grade 5: head of department (most experienced surgeon). The majority of procedures were performed by surgeons of level 3 and 4. The experience grade (grades 4, 5 versus grades 1, 2, 3) had no statistically significant influence on the placement accuracy of pedicle screws (odds ratio 0.990, 95% CI 0.650 to 1.509, p = 0.96). The BMI did not influence the placement accuracy, either (BMI < 30 versus BMI ≥ 30: odds ratio 0.684, 95% CI 0.396 to 1.181, p = 0.17). Looking at the four surgeons with the most cases in this series, no preference for one or the other technique was found [n(total) = 291, n(navigated) = 152, n(not navigated) = 139]. We performed another subanalysis taking the personally favored technique into account and were not able to determine a significant difference regarding the accuracy of pedicle screw placement. There was a clear preference to use the navigation system in higher spinal levels (Table 5). The presence of polytrauma did not significantly influence the placement accuracy, either (p = 0.6406). Further results are demonstrated in Table 6.
Table 6. Additional results of the regression analysis.
| Variable | Group 1 | Group 2 | Odds ratio | 95% confidence limit | p |
|---|---|---|---|---|---|
| Technique | T1–6 (navigated) | T1–6 (conventional) | 1.06 | 0.41–2.69 | 0.91 |
| Technique | T7–T10 (navigated) | T7-T10 (conventional) | 0.57 | 0.24–1.36 | 0.21 |
| Technique | T10–L2 (navigated) | T10-L2 (conventional) | 0.69 | 0.35–1.34 | 0.27 |
| Technique | L1–L5 (navigated) | L 1-L5 (conventional) | 2.59 | 0.54–12.62 | 0.23 |
| BMI | ≤30 (all screws) | >30 (all screws) | 0.69 | 0.39–1.18 | 0.17 |
| BMI | ≤25 (all screws) | ≥30 (all screws) | 0.75 | 0.42–1.34 | 0.33 |
| BMI/technique | >30 (navigated) | >30 (conventional) | 0.91 | 0.55–1.51 | 0.72 |
| BMI/technique | >30 (T1–6, navigated) | >30 (T1–6, conventional) | 1.27 | 0.43–3.75 | 0.66 |
| BMI/technique | >30 (T7–10, navigated) | >30 (T7–10, conventional) | 0.75 | 0.29–1.93 | 0.55 |
| Spinal level | S1 (all screws) | L1–L5 (all screws) | 0.7 | 0.14–3.64 | 0.67 |
Abbreviation: BMI, body mass index.
Discussion
In this retrospective analysis, we examined 452 patients receiving a total of 2,003 pedicle screws with postoperative computed tomography eligible for evaluation. We hypothesized that computer-navigated procedures are more accurate, that the BMI influences the accuracy, and that the experience of the performing surgeon influences the accuracy. None of these hypotheses could be confirmed with our study. The modality (computer-navigated or conventionally placed), the experience, and the BMI did not influence the accuracy of pedicle screw placement for spinal fusions. The exclusively significant factor was the spinal level of fusion: the higher the level, the more inaccurate the screw position. Overall, 85.9% of the non-navigated screws and 78.5% of all the computer-navigated screws were placed completely intraosseous; adding grade 1 screws (displacement less 2 mm), an acceptable screw position was achieved in 94.6% of the conventionally placed screws and 90.3% of the computer-navigated screws.
The strength of this analysis is the huge number of patients and screws all being treated in a single center and the complex mathematical analysis of our data: mixed-effects regression models for a binary outcome were used to address multiple (statistically dependent) measurements within the patients.
The limitations are the study's retrospective design, which impairs the data quality and leads to a loss of important information. Furthermore, because of the explorative nature of our study, the results from the statistical tests have to be interpreted with caution: all significant differences (p < 0.05) showed only a tendency. However, the major bias is the missing randomization to one or the other group, leaving it to the choice of the surgeon whether to use a navigation system. Surgeons experienced with the system may tend to use it in every situation the system was available, and surgeons less familiar with navigation systems may choose to go without.
In this study, the experience of the surgeon did not show any statistically significant impact. In a teaching hospital, where young doctors are trained to become orthopedic surgeons, all surgical procedures are performed under guidance of a more experienced, senior physician. Although younger surgeons inserted the screws and performed the procedures, the senior physicians advised the younger ones how to do it and, if required, corrected mistakes (for example, the position of the hand while drilling the screw in the pedicle). This effect cannot be determined retrospectively, and therefore it is not astonishing that the experience of the surgeon did not show significant differences regarding the screw placement accuracy.
Whether navigation increases placement accuracy is still lively discussed, and the reports in the literature are contradictory. Entering the search term “pedicle screw” and setting filters to “meta-analysis,” the PubMed database delivers five publications (as of January 28, 2013). Setting filters to “systematic review” produces a total of 56 articles, of which 7 contribute directly to the topic. Based on 43 publications (28 clinical, 14 cadaveric, and 1 model study), Tian and Xu concluded that navigation systems can increase the accuracy for pedicle screw placement and that the best accuracy can be achieved with 3D-based navigation,18 which is the modality we examined in this project. They did not explicitly differentiate between spinal segments but focused on different navigation modalities (i.e., CT, 2D, and 3D). The majority of included studies consisted of small collectives with degenerative or not further determined spinal conditions. Similar results were reported by another meta-analysis examining 5,992 pedicle screws. Verma et al found 93.3% of the computer-navigated screws and 84.7% of the conventionally inserted screws were accurately placed (p < 0.00001).19 Tian et al examined different navigation methods and found 90.76% accurate screw placement in the CT-based group versus 85.48% in the 2D-based group. This analysis did not report on conventionally inserted screws.20 Kosmopoulos and Schizas reported an in vivo median placement accuracy of 95.1% with and 90.3% without computer navigation, although half of the studies did not report on how placement accuracy was determined.13 The overall placement accuracy without these studies was 86.7% (our study: 82.4%). Interestingly, differences in the weighted mean placement accuracy in the navigation-assisted subgroup (90.6%) compared with the computer-navigated subgroup (90.7%) could not be demonstrated, although the authors noted that the descriptive statistics suggested greater placement accuracy for most of the computer-navigated subgroups. As in our study, the placement accuracy in the thoracic spine in the in vivo group was greater in the conventional group (94.3% versus 82.2%; our study: grade 0: conventional 80.9% versus 73.4%, grade 0 + 1: 92.7% versus 87.3%). Analyzing the subsegments in our study, navigation can increase the placement accuracy for certain levels of the lumbar spine, whereas the conventional method delivers better results in the thoracic spine. In their discussion, Kosmopoulos and Schizas described the strongest limitation to be the missing statement of how the placement accuracy was determined in many studies and cite the discussion presented by Laine et al.13 21 The authors discussed the influence on placement accuracy classification systems on final outcome, as some authors define a “safe zone” (in the cited publication at the lumbar spine) of 4 mm adjacent to the pedicle and classify screws in this zone as correct,22 whereas other studies (as we did in our examination) define placement accuracy in grades and describe exactly how the distribution was performed. Tjardes et al performed a review on 276 publications dealing with image-guided spine surgery and came to a similar conclusion.14
In contrast to most studies analyzed in the previously mentioned meta-analyses and reviews, the main indication for fusing spinal segments in our population was trauma-related. This may explain slight differences in the placement accuracy rate, although most hitherto published results are well reflected in our work.
In this study, the computer-navigated screws had a tendency to perforate the lateral aspect of the pedicle, which conforms to results published by Gelalis et al.23 Therefore our study is the second survey to demonstrate such an astonishing effect of a certain technique on screw position. The authors of the latter-mentioned study reported that conventional screws are more likely to perforate the medial side, which we did not see in our study. They argue that surgeons are more likely to accept lateral screws than medial screws because a correlation between medially displaced screws and neurologic disorders has been reported; the authors question whether improved patient outcome of computer-navigated procedures may be based more on the lateral screw placement rather than on positive effects of the navigation technique.24 25
In a recent study, Waschke and his team examined the influence of CT-based navigation in 4,500 screws and demonstrated greater placement accuracy in the computer-navigated group.17 However, only half of the included patients had fractures of the spine, and, more importantly, the navigation technique was different than the modality of our work. The authors used a mobile CT gantry attached to a mobile CT examination table, whereas we used a mobile 3D C-arm. The image quality is vital to successful navigation; the CT can deliver clear images also in upper thoracic levels, but the image quality of a 3D C-arm is limited due to artifacts caused by the shoulder region of the patient. Second, the main indications in our patients were fractures, probably causing a higher mobility of the instrumented spinal segments in comparison with degenerative indications, which is a potential bias difficult to determine.
Conclusion
In the traumatized spine, pedicle screw insertion with and without the use of a navigation system are safe methods. In contrast to other studies, which showed greater placement accuracy of different computer-navigated modalities in comparison with non-navigated techniques, we found that a 3D-based navigation technique does not contribute greater placement accuracy in spinal trauma care. Besides the placement accuracy, there may be others reasons to use this technique (e.g., reduced emission of radiation, image fusion, tumor surgery), which we did not evaluate in this study. With technical improvements and new developments, the navigation technique might have the potential in the future to increase the placement accuracy as well and finally to help improve outcome parameters for the patients. To our best knowledge, there is no published study reporting on improved patient outcome if navigation systems are used, but we agree with Altman and Bland that the “absence of evidence is not evidence of absence,”26 and prospective randomized long-term studies are necessary to finally answer these questions.
Ethical Approval
The study was approved by the local ethics committee and was performed in accordance with the ethical standards in the 1964 Declaration of Helsinki.
Footnotes
Disclosures Michael Kraus, none Julia Weiskopf, none Jens Dreyhaupt, none Gert Krischak, none Florian Gebhard, none
References
- 1.Harrington P R, Tullos H S. Reduction of severe spondylolisthesis in children. South Med J. 1969;62(1):1–7. doi: 10.1097/00007611-196901000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986;(203):7–17. [PubMed] [Google Scholar]
- 3.Weinstein J N, Spratt K F, Spengler D, Brick C, Reid S. Spinal pedicle fixation: reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine (Phila Pa 1976) 1988;13(9):1012–1018. doi: 10.1097/00007632-198809000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Gautschi O P, Schatlo B, Schaller K, Tessitore E. Clinically relevant complications related to pedicle screw placement in thoracolumbar surgery and their management: a literature review of 35,630 pedicle screws. Neurosurg Focus. 2011;31(4):E8. doi: 10.3171/2011.7.FOCUS11168. [DOI] [PubMed] [Google Scholar]
- 5.Hicks J M, Singla A, Shen F H, Arlet V. Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine (Phila Pa 1976) 2010;35(11):E465–E470. doi: 10.1097/BRS.0b013e3181d1021a. [DOI] [PubMed] [Google Scholar]
- 6.Hüfner T, Gebhard F, Grützner P A, Messmer P, Stöckle U, Krettek C. Which navigation when? Injury. 2004;35 01:S-A30–S-A34. doi: 10.1016/j.injury.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 7.Hartl R, Lam K S, Wang J. et al. Worldwide survey on the use of navigation in spine surgery. World Neurosurg. 2013;79(1):162–172. doi: 10.1016/j.wneu.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 8.Kraus M D, Krischak G, Keppler P, Gebhard F T, Schuetz U H. Can computer-assisted surgery reduce the effective dose for spinal fusion and sacroiliac screw insertion? Clin Orthop Relat Res. 2010;468(9):2419–2429. doi: 10.1007/s11999-010-1393-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amiot L P, Lang K, Putzier M, Zippel H, Labelle H. Comparative results between conventional and computer-assisted pedicle screw installation in the thoracic, lumbar, and sacral spine. Spine (Phila Pa 1976) 2000;25(5):606–614. doi: 10.1097/00007632-200003010-00012. [DOI] [PubMed] [Google Scholar]
- 10.Kotani Y Abumi K Ito M Minami A Improved accuracy of computer-assisted cervical pedicle screw insertion J Neurosurg 200399(3, Suppl):257–263. [DOI] [PubMed] [Google Scholar]
- 11.Lavallée S, Sautot P, Troccaz J, Cinquin P, Merloz P. Computer-assisted spine surgery: a technique for accurate transpedicular screw fixation using CT data and a 3-D optical localizer. J Image Guid Surg. 1995;1(1):65–73. doi: 10.1002/(SICI)1522-712X(1995)1:1<65::AID-IGS10>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 12.Merloz P, Troccaz J, Vouaillat H. et al. Fluoroscopy-based navigation system in spine surgery. Proc Inst Mech Eng H. 2007;221(7):813–820. doi: 10.1243/09544119JEIM268. [DOI] [PubMed] [Google Scholar]
- 13.Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: a meta-analysis. Spine (Phila Pa 1976) 2007;32(3):E111–E120. doi: 10.1097/01.brs.0000254048.79024.8b. [DOI] [PubMed] [Google Scholar]
- 14.Tjardes T, Shafizadeh S, Rixen D. et al. Image-guided spine surgery: state of the art and future directions. Eur Spine J. 2010;19(1):25–45. doi: 10.1007/s00586-009-1091-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carl A L Tromanhauser S G Roger D J Pedicle screw instrumentation for thoracolumbar burst fractures and fracture-dislocations Spine (Phila Pa 1976) 199217(8, Suppl):S317–S324. [DOI] [PubMed] [Google Scholar]
- 16.Kim M C, Chung H T, Cho J L, Kim D J, Chung N S. Factors affecting the accurate placement of percutaneous pedicle screws during minimally invasive transforaminal lumbar interbody fusion. Eur Spine J. 2011;20(10):1635–1643. doi: 10.1007/s00586-011-1892-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Waschke A, Walter J, Duenisch P, Reichart R, Kalff R, Ewald C. CT-navigation versus fluoroscopy-guided placement of pedicle screws at the thoracolumbar spine: single center experience of 4,500 screws. Eur Spine J. 2013;22(3):654–660. doi: 10.1007/s00586-012-2509-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tian N F, Xu H Z. Image-guided pedicle screw insertion accuracy: a meta-analysis. Int Orthop. 2009;33(4):895–903. doi: 10.1007/s00264-009-0792-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verma R, Krishan S, Haendlmayer K, Mohsen A. Functional outcome of computer-assisted spinal pedicle screw placement: a systematic review and meta-analysis of 23 studies including 5,992 pedicle screws. Eur Spine J. 2010;19(3):370–375. doi: 10.1007/s00586-009-1258-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tian N F, Huang Q S, Zhou P. et al. Pedicle screw insertion accuracy with different assisted methods: a systematic review and meta-analysis of comparative studies. Eur Spine J. 2011;20(6):846–859. doi: 10.1007/s00586-010-1577-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laine T, Mäkitalo K, Schlenzka D, Tallroth K, Poussa M, Alho A. Accuracy of pedicle screw insertion: a prospective CT study in 30 low back patients. Eur Spine J. 1997;6(6):402–405. doi: 10.1007/BF01834068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gertzbein S D, Robbins S E. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 1990;15(1):11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Gelalis I D, Paschos N K, Pakos E E. et al. Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J. 2012;21(2):247–255. doi: 10.1007/s00586-011-2011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lonstein J E, Denis F, Perra J H, Pinto M R, Smith M D, Winter R B. Complications associated with pedicle screws. J Bone Joint Surg Am. 1999;81(11):1519–1528. doi: 10.2106/00004623-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 25.West J L III, Ogilvie J W, Bradford D S. Complications of the variable screw plate pedicle screw fixation. Spine (Phila Pa 1976) 1991;16(5):576–579. doi: 10.1097/00007632-199105000-00016. [DOI] [PubMed] [Google Scholar]
- 26.Altman D G, Bland J M. Absence of evidence is not evidence of absence. BMJ. 1995;311(7003):485. doi: 10.1136/bmj.311.7003.485. [DOI] [PMC free article] [PubMed] [Google Scholar]


