Abstract
Objective
To assess whether adoption of the patient-centered medical home (PCMH) reduces emergency department (ED) utilization among patients with and without chronic illness.
Data Sources
Data from approximately 460,000 Independence Blue Cross patients enrolled in 280 primary care practices, all converting to PCMH status between 2008 and 2012.
Research Design
We estimate the effect of a practice becoming PCMH-certified on ED visits and costs using a difference-in-differences approach which exploits variation in the timing of PCMH certification, employing either practice or patient fixed effects. We analyzed patients with and without chronic illness across six chronic illness categories.
Principal Findings
Among chronically ill patients, transition to PCMH status was associated with 5–8 percent reductions in ED utilization. This finding was robust to a number of specifications, including analyzing avoidable and weekend ED visits alone. The largest reductions in ED visits are concentrated among chronic patients with diabetes and hypertension.
Conclusions
Adoption of the PCMH model was associated with lower ED utilization for chronically ill patients, but not for those without chronic illness. The effectiveness of the PCMH model varies by chronic condition. Analysis of weekend and avoidable ED visits suggests that reductions in ED utilization stem from better management of chronic illness rather than expanding access to primary care clinics.
Keywords: Patient-centered medical home, emergency department, chronic illness
The patient-centered medical home (PCMH) model has shown early promise as a vehicle for reorganizing health care systems and improving the management of chronic illness. Studies of the medical home and related interventions have shown improvements in provider experience (Reid et al. 2010), patient experience (Reid et al. 2009, 2010; Solberg et al. 2011), processes of care (Zuckerman et al. 2004; Wise et al. 2006; Domino et al. 2009), practice-level measures of quality and preventive care utilization (Paustian et al. 2013), and economic outcomes such as reductions in total costs (Devries et al. 2012; Paustian et al. 2013) and use of high-intensity domains of care, such as hospital admissions or emergency department (ED) visits (Reid et al. 2010).
However, systematic reviews of evaluations of the PCMH demonstrate that the work to date is inconclusive and often yields conflicting results (Peikes et al. 2012; Jackson et al. 2013). For example, the transition to a PCMH model has been shown, variously, to reduce total costs (Devries et al. 2012) or increase costs (Domino et al. 2009), while others found spending rose in some areas and fell in others (Reid et al. 2010) or found no significant effects (Leff et al. 2009; Werner et al. 2013). In addition, several reviews of the PCMH literature point out methodological concerns regarding the existing work: studies examine too few practices, include inadequate follow-up, and have failed to account for the clustering of results by practice (Peikes et al. 2011).
This article intends to contribute to the growing literature evaluating the impact of adoption of the PCMH model by primary care practices. By using a novel identification strategy and a rigorous difference-in-differences approach to study a large administrative dataset—over 1 million patient-years across 280 PCMH-certified primary care practices—we aim to address the methodological concerns raised elsewhere to sort through the uncertainty and point toward a research agenda for future evaluations of the PCMH model. In particular, we are interested in the mechanisms through which the PCMH affects ED utilization. One possibility is that expanding access would allow some patients, who might otherwise present to the ED, to receive medical attention in a primary care setting. Other ED patients require urgent care to treat acute episodes of chronic illness, but many of these encounters could have been prevented if patients’ conditions were appropriately managed by primary care. We shed some light on these issues by analyzing a subset of weekend ED visits and avoidable ED visits.
The Patient-Centered Medical Home
Recent literature on primary care emphasizes significant challenges, such as perverse incentives related to fee-for-service reimbursement (American College of Physicians 2006), the supply of primary care physicians relative to specialists (Moore and Showstack 2003; Bodenheimer, Grumbach, and Berenson 2009), and an orientation poorly suited to effectively managing chronic illness (Wagner, Austin, and Von Korff 1996; Bodenheimer, Wagner, and Grumbach 2002). In light of these challenges, as well as the optimism surrounding initiatives to improve primary care, the PCMH model has garnered considerable interest. Comprehensive discussion of the PCMH and its history can be found elsewhere (American Academy of Family Physicians 2007; Friedberg et al. 2009; Kilo and Wasson 2010). Generally speaking, the medical home model calls for the following: improved coordination of services, orchestrated by a personal physician; a “whole person” orientation to care; expanded patient access to primary care practices; increased usage of health information technology; and aligning reimbursement incentives to better compensate this expanded role for primary care (American Academy of Family Physicians 2007).
The National Committee for Quality Assurance (NCQA) publishes guidelines for primary care practices looking to adopt the PCMH model, and it accredits practices as having adopted these improvements using a three-level typology reflecting the number of reforms in place. To gain recognition at each level, practices must demonstrate successful adoption of a group of “must pass” elements, and they are graded using a point-based system for additional improvements (National Committee for Quality Assurance 2008). Though competing standards exist, the NCQA guidelines are the most widely used in the PCMH literature (Friedberg et al. 2009; Cassidy 2010).
The 2011 NCQA guidelines include 28 specific practice improvements across six categories, including enhanced access and continuity, identifying and managing patient populations, planning and managing care, providing self-care support and community resources, tracking and coordinating care, and measuring and improving performance (National Committee for Quality Assurance 2011). In terms of their impact on ED utilization, these categories can be grouped under two headings, divided by their hypothesized effect. Some improvements expand access to clinics (such as extended operating hours, electronic access, etc.), potentially leading to substitution of primary care for expensive and intensive ED services; others are aimed at improving population health (like use of data for population management, identifying high-risk patients, care coordination, use of electronic prescribing, and implementation of evidence-based guidelines). Disentangling the effects of these two categories of the PCMH has important implications for medical care and future policy.
PCMH and Emergency Departments Utilization
A number of drivers of high ED volume are offered in the literature (Billings, Parikh, and Mijanovich 2000). Some visits are for nonurgent health issues; some are urgent but could be safely and effectively addressed in the realm of primary care; and still others are appropriate for the ED at the time of visit but could have been avoided with better disease management. These visits not only increase health system spending but also may lead to excessive or unnecessary treatment and testing. Though estimates vary, a substantial fraction of visits to EDs are avoidable. One study calculated that between 13.7 and 27.1 percent of all ED encounters were for conditions that could have been addressed in retail or urgent care clinics, saving roughly $4.4 billion each year (Weinick, Burns, and Mehrotra 2010). Expanding access to primary care clinics may help address these problems, as patients reporting fewer barriers to after-hours contact with their physicians reported fewer ED visits (O'Malley 2013). Conceptual models of the PCMH suggest that adoption of such reforms may lead to fewer ED visits by patients, both by improving the coordination of care and by reducing delays in treatment, thereby reducing the likelihood of complications (Hearld and Alexander 2012).
Data
Program Description
The data for this project were obtained from Independence Blue Cross (IBC) of Pennsylvania. IBC is the largest commercial health plan in the Philadelphia area and was a key figure in Pennsylvania's Chronic Care Initiative, a multistakeholders effort aimed at improving the quality of primary care for patients with chronic illness. Medical practices participating in the program were required to achieve PCMH designation from the NCQA at Level 1 or higher. As of November 2012, 280 practices in the IBC network were recognized as having implemented the PCMH model. These practices are responsible for the care of more than a third of all IBC's commercially insured HMO patients in Pennsylvania, including IBC members enrolled in Medicare Advantage plans.
Practices transitioning to the PCMH model between May 2008 and December 2011 received financial and logistical support from IBC and the Commonwealth of Pennsylvania. Payments helped practices to cover the cost of transition to PCMH, including the cost of practice coaches and the infrastructure required to achieve NCQA recognition. In addition, practices were offered resource guides, webinars, reports, clinical programs, and other tools to support their transition to PCMH status. These tools include clinical alerts, clinical care reports, daily hospital census, the Practice Advisor tool (offered through American College of Physicians), and a PCMH resource library (offered via NaviNet). The Commonwealth of Pennsylvania provided a learning collaborative for practices transitioning over this period.
From January 2012 on, practices that adopted the PCMH model did not receive upfront financial assistance from IBC. Instead, incentive payments for eligible providers were paid based on the number of IBC patients and the level of NCQA recognition for each practice. For this reason, our analysis focuses on ED visits and expenditures between 2008 and 2011, but it includes patients in all practices reaching PCMH status between 2008 and 2012, including 95 practices which received NCQA certification during 2012, when incentive payments from IBC changed. Figure1 presents the cumulative number of NCQA-certified PCMH practices over time.
Figure 1.
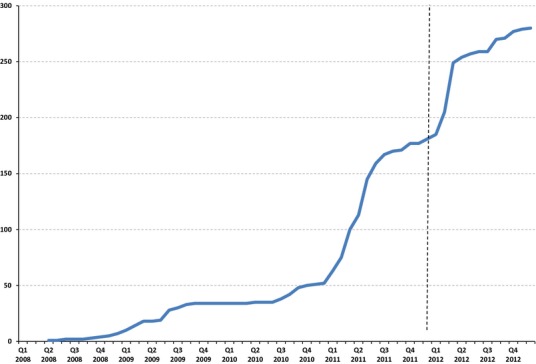
Cumulative Number of IBC's NCQA-Certified Patient-Centered Medical Homes (PCMHs) between January 2008 and November 2012
Note. The vertical line marks the end of 2011. Our analysis focuses on ED visits and expenditures between 2008 and 2011, but it includes patients in all practices reaching PCMH status between 2008 and 2012, including 95 practices that received NCQA certification during 2012, when incentive payments from IBC changed.
Patient and Practice Selection
Using patient-level data for the years 2008 through 2011, we focus on one set of outcomes—ED utilization and expenditures—for approximately 460,000 Health Plan HMO members across all practices which converted to PCMH status during the years from 2008 through 2012. All practices in our analysis achieved PCMH certification but differ in the timing of accreditation. Practices not receiving recognition as a PCMH by December 2012 were excluded from the analysis due to concerns about potential inherent differences with practices that achieved PCMH status.1
From the complete IBC dataset of 947 practices with a patient panel size of 300 or more, we identified 280 that made the switch to PCMH status by December 2012. These practices represent a diverse cross-section of primary care fields: 130 were designated “family practice” clinics, with an additional 87 identified as “internal medicine;” a further 55 were labeled as “pediatrics” clinics. The remaining practices (8) were spread across other multispecialty clinics. Sixty-four of the practices studied were located within the city of Philadelphia, with the remainder found throughout the Philadelphia suburbs. Nearly two-thirds of these practices (178) achieved Level 3 PCMH status, the highest level recognized by the NCQA. Of the remaining clinics, 79 and 23 received Level 1 and Level 2 recognition, respectively.
Patients enrolled in an IBC Preferred Provider Organization (PPO) plan were excluded from the study, as they were not required to select a primary care physician and could not be reliably attributed to any one practice. Finally, member-years with unusually high ED expenditures2 were also excluded (approximately a third of a percent of the sample). Applying these exclusion criteria generated two datasets: the first includes 1,083,773 patient-year observations; and a second, referred to as “patient panel sample,” is comprised of 459,676 patient-years for members enrolled during all 4 years of the study period. We analyzed chronically ill patients separately from those without chronic illness to ascertain whether and to what extent the transition to a PCMH framework affects such patients in terms of ED utilization and costs. An attrition diagram describing these steps in detail appears in Appendix SA2.
Patients with chronic illness make up 36.3 percent of all patient-years, and 42.1 percent of the patient-years in the patient panel sample. Chronic illness is defined here by diagnosis of any of the following: asthma, hypertension, coronary artery disease (CAD), chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), or diabetes. Approximately 65 percent of chronically ill patients have one chronic condition, 20 percent have two chronic conditions, 9 percent have three chronic conditions, and 6 percent have four or more.
Covariates
Patient-Level Characteristics
A number of variables from the IBC dataset were used to control for patient attributes. In addition to demographic information like gender and age, each patient-year observation includes a risk score estimated using the Verisk Health DxCG Risk Solutions model, which incorporates clinical and demographic data for each patient (Verisk Health, Inc. 2010). Information about insurance plan type (individual vs. family coverage, subscriber vs. dependent, and whether the group providing insurance coverage was self-funded or fully insured) is also included to control for differences in plan benefit structure. Further demographic information (including income, rate of college graduation, and information on race and ethnicity) for each patient's zip code of residence was extracted from the 2000 Census (U.S. Census Bureau 2002). To proxy for both access and convenience of ED use, we calculate the distance traveled in miles from the patient's residence to the ED for patients who visited an ED during a given year. This variable is used in our analysis of visits and expenditures conditional on at least one visit. In addition, we are able to observe the day of week for each ED encounter, and construct an indicator variable for weekend ED visits. Note that because the hour of ED visit was not available, we could not perfectly assign visits as occurring when practices were open or closed to patients. Hence, the day of week serves as a proxy.
Practice-Level Characteristics
A number of practice descriptors, such as panel size, location (Philadelphia vs. rest of southeastern PA), and medical specialty were included. Summary statistics describing this pool of eligible patient-years appear in Table1.
Table 1.
Summary Statistics—Patient Attributes
| All Patients | Patient Panel | |||
|---|---|---|---|---|
| Chronic | Nonchronic | Chronic | Nonchronic | |
| (a) | ||||
| Number of observations | 393,317 | 690,456 | 193,435 | 266,241 |
| PCMH status | 0.293 | 0.303 | 0.316 | 0.305 |
| Year of observation | ||||
| 2008 | 0.242 | 0.257 | 0.224 | 0.269 |
| 2009 | 0.269 | 0.258 | 0.246 | 0.253 |
| 2010 | 0.248 | 0.246 | 0.261 | 0.242 |
| 2011 | 0.241 | 0.239 | 0.268 | 0.237 |
| Risk score | 5.00 | 0.99 | 4.12 | 0.91 |
| Chronic illness | ||||
| Asthma | 0.366 | 0.345 | ||
| Hypertension | 0.621 | 0.648 | ||
| CAD | 0.193 | 0.204 | ||
| COPD | 0.115 | 0.115 | ||
| CHF | 0.090 | 0.090 | ||
| Diabetes | 0.256 | 0.259 | ||
| Other demographics | ||||
| Age | 52.11 | 30.28 | 54.27 | 32.30 |
| Female | 0.557 | 0.550 | 0.559 | 0.556 |
| African American (zip 2000) | 0.194 | 0.175 | 0.187 | 0.173 |
| Hispanic (zip 2000) | 0.032 | 0.033 | 0.031 | 0.032 |
| Annual income (zip 2000) | $51,859 | $53,204 | $52,273 | $53,659 |
| College grads (zip 2000) | 0.296 | 0.316 | 0.298 | 0.320 |
| Single contract member | 0.573 | 0.394 | 0.588 | 0.362 |
| Subscriber member | 0.739 | 0.556 | 0.759 | 0.553 |
| Self-funded member | 0.125 | 0.165 | 0.134 | 0.194 |
| Medicare advantage | 0.294 | 0.030 | 0.340 | 0.039 |
| Median distance to ED (miles)* | 4.838 | 4.836 | 5.318 | 5.130 |
| Mean distance to ED (miles)* | 8.631 | 8.422 | 10.239 | 9.481 |
| Outcomes | ||||
| ED visits (all) | 0.250 | 0.131 | 0.239 | 0.135 |
| ED visits (avoidable) | 0.168 | 0.091 | 0.158 | 0.092 |
| Weekend ED visits | 0.093 | 0.048 | 0.087 | 0.049 |
| No. of ED visits* | 1.24 | 1.07 | 1.18 | 1.06 |
| ED expenditures | $189.6 | $107.1 | $158.3 | $92.6 |
| ED expenditures* | $759.8 | $818.8 | $662.8 | $688.2 |
| (b) | ||||
| Panel size | 2,133.1 | 2,214.8 | 2,125.1 | 2,215.3 |
| Practice in Philadelphia | 0.295 | 0.298 | 0.290 | 0.298 |
| Clinic type | ||||
| Internal medicine | 0.362 | 0.244 | 0.380 | 0.259 |
| Family practice | 0.517 | 0.487 | 0.500 | 0.458 |
| Pediatric | 0.118 | 0.264 | 0.118 | 0.279 |
| CRNP | 0.003 | 0.005 | 0.002 | 0.003 |
Note: *Conditional on one or more visits.
CRNP, certified registered nurse practitioner.
Empirical Framework
We estimate the aggregate effects of a practice switching to PCMH status on ED utilization and associated medical costs using an empirical difference-in-differences approach. This research design employs a novel identification strategy which exploits the fact that the transition to PCMH status occurred at different times across primary care clinics, so patient outcomes could be tracked before and after the switch at different points in time and across practices. These effects were estimated using the model below:
 |
1 |
In the tables that follow, linear probability models are used to estimate the effect of PCMH status on the number of patients with at least one ED visit during a given patient year3 (i.e., PCMH effects on extensive margins). Poisson models are used to estimate the effect of PCMH status on the number of ED visits, conditional on at least one ED visit in a given year (i.e., intensive margins), and coefficient estimates are transformed to marginal effects. To study the effect of PCMH status on ED expenditures (also conditional on nonzero ED visits), including both facility and professional components of ED payments, we used ordinary least-squares regression and transformed the dollar-denominated dependent variable to logarithms. All specifications include either practice or patient fixed effects and robust standard errors.
The outcome variable Yjit for patient j enrolled at primary care practice i during year t is (1) a dichotomous variable tracking whether a patient-year observation has any ED visit (=1) or no ED visit (=0), (2) the number of ED visits conditional on at least one ED visit, and (3) log ED expenditures conditional on at least one ED visit. The key explanatory variables are (During × PCMH)it and (Post × PCMH)it, which are indicator variables capturing each practice's PCMH status during a given year. (During × PCMH)it equals 1 if an observation was recorded during the year of practice i's transition to PCMH status and is set to zero otherwise; (Post × PCMH)it equals 1 in subsequent years and zero otherwise. Fracit captures the fraction of the transition year during which practice i had achieved PCMH recognition.4 Distinguishing between the transitional year in which the switch to the PCMH model was made and subsequent full years of PCMH status is important, given the documented challenges of PCMH implementation in the literature (Berenson et al. 2008; Kilo and Wasson 2010; Harbrecht and Latts 2012). Studies of other health system reforms, including the Massachusetts health insurance reforms, have noted the importance of accounting for such transitional periods in analytical design (Chandra, Gruber, and McKnight 2011; Joynt et al. 2013). λt is a year fixed effects term. We employ two different sets of specifications, using practice fixed effects (μi) and using patient fixed effects (μj), respectively, to account for the characteristics of individual practices or patients.
In addition, the model expressed in equation 1 controls for a range of patient and practice characteristics. Ait captures clinic characteristics, including physician panel size and number of physicians per practice, as well as time-invariant clinic characteristics such as location within Philadelphia, practice specialty, and NCQA certification level. Xjit captures time-varying patient characteristics such as risk score, age, and comorbidities, as well as time-invariant attributes such as gender, insurance plan details, and residence. Xjit also includes time-invariant characteristics of the zip code in which the patient resides, including median household income, percent of residents with college degrees, percent African American, and percent Hispanic, as reported in the 2,000 decennial Census. The error term εjit represents the remaining, unobserved variation in patient and practice attributes.
Results
In this section, we present estimates of the impact of primary care practices switching to PCMH status on ED utilization and costs as derived by estimating equation 1. Results for the models estimating the PCMH effect on the number of patients with “any ED visit” are reported in Tables4 as percentage point changes. In the text that follows, these results have been translated to percent reductions from baseline utilization rates for ease of interpretation. Baseline rates of patients with any ED visit and weekend/avoidable ED visits appear in Table1. Table2 provides estimates for the impact of PCMH adoption on whether patients had any ED visits in a given year, as well as the number of ED visits (conditional on nonzero visits) and log ED expenditures (conditional on nonzero visits) for patients with and without chronic illnesses.
Table 4.
The Effect of Patient-Centered Medical Home (PCMH) on the Likelihood of Emergency Department (ED) Visits by Chronic Condition
| Dependent Variable | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Any ED Visit (Yes = 1) | [1] | [2] | [3] | [4] | [1] | [2] | [3] | [4] | [1] | [2] | [3] | [4] |
| Chronic Condition | Asthma | Hypertension | Coronary Artery Disease (CAD) | |||||||||
| Post × PCMH | −0.00579 [0.00678] | −0.0124 [0.00974] | −0.0116 [0.00727] | −0.0163* [0.00898] | −0.0157*** [0.00516] | −0.0186*** [0.00694] | −0.0189*** [0.00559] | −0.0181*** [0.00660] | −0.0134 [0.0105] | −0.0315** [0.0139] | −0.0274** [0.0113] | −0.0353*** [0.0131] |
| During × PCMH | −0.00705 [0.00431] | −0.00152 [0.00617] | −0.00364 [0.00454] | −1.31E-03 [0.00580] | −0.00852*** [0.00327] | −0.00786* [0.00437] | −0.0121*** [0.00348] | −0.0107** [0.00423] | −0.00979 [0.00651] | −0.0180** [0.00854] | −0.0160** [0.00682] | −0.0216*** [0.00811] |
| Observations | 143,900 | 66,759 | 143,900 | 66,759 | 244,294 | 125,327 | 244,294 | 125,327 | 75,729 | 39,471 | 75,729 | 39,471 |
| R2 | 0.091 | 0.093 | 0.577 | 0.459 | 0.13 | 0.129 | 0.583 | 0.476 | 0.144 | 0.143 | 0.578 | 0.479 |
| Chronic Condition | Congestive Heart Failure (CHF) | Chronic Obstructive Pulmonary Disease (COPD) | Diabetes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Post × PCMH | −0.0262* [0.0159] | −0.0346 [0.0219] | −0.0304* [0.0178] | −0.0311 [0.0208] | −0.0208 [0.0136] | −0.0246 [0.0187] | −0.0431*** [0.0149] | −0.0446** [0.0177] | −0.0273*** [0.00818] | −0.0317*** [0.0112] | −0.0346*** [0.00863] | −0.0312*** [0.0103] |
| During × PCMH | −0.0176* [0.00990] | −0.0251* [0.0133] | −0.0145 [0.0107] | −0.0153 [0.0128] | −0.00691 [0.00843] | −0.00444 [0.0114] | −0.0153* [0.00893] | −0.0118 [0.0109] | −0.0137*** [0.00516] | −0.0175** [0.00700] | −0.0173*** [0.00537] | −0.0187*** [0.00660] |
| Observations | 35,212 | 17,505 | 35,212 | 17,505 | 45,158 | 22,181 | 45,158 | 22,181 | 100,679 | 50,015 | 100,679 | 50,015 |
| R2 | 0.133 | 0.145 | 0.597 | 0.504 | 0.155 | 0.153 | 0.606 | 0.499 | 0.145 | 0.141 | 0.58 | 0.468 |
| Practice fixed effects | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| Patient fixed effects | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| Patient panel sample | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
Note: Robust standard errors in brackets.
Bold values indicate ***p < .01, **p < .05, *p < .1.
Table 2.
The Effect of Patient-Centered Medical Home (PCMH) on Emergency Department Visits and Emergency Department (ED) Expenditures for Patients with and without Chronic Illness
| [1] | [2] | [3] | [4] | [1] | [2] | [3] | [4] | [1] | [2] | [3] | [4] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dependent Variable | Any ED Visit (Yes = 1) | Number of ED Visits (Cond.) | Log ED Expenditures (Cond.) | |||||||||
| All chronic patients | ||||||||||||
| Post × PCMH | −0.0131*** [0.00401] | −0.0155*** [0.00552] | −0.0190*** [0.00472] | −0.0186*** [0.00523] | −0.00667 [0.02112] | −0.00839 [0.02509] | −0.03672 [0.02481] | −0.03588 [0.02992] | 0.0166 [0.0159] | 0.0083 [0.0218] | −0.0119 [0.0339] | −0.0102 [0.0355] |
| During × PCMH | −0.00842*** [0.00255] | −0.00648* [0.00353] | −0.0105*** [0.00293] | −0.00874*** [0.00338] | −0.01766 [0.01355] | −0.02292 [0.01605] | −0.03003* [0.01510] | −0.01757 [0.01776] | 0.022 [0.0801] | 0.0238 [0.0337] | 0.0124 [0.0215] | 0.016 [0.0230] |
| Observations | 393,317 | 193,435 | 393,317 | 193,435 | 98,158 | 46,193 | 98,158 | 46,193 | 98,158 | 46,193 | 98,158 | 46,193 |
| R2 | 0.103 | 0.103 | 0.564 | 0.448 | 0.156 | 0.112 | 0.618 | 0.571 | 0.138 | 0.142 | 0.794 | 0.706 |
| All nonchronic patients | ||||||||||||
| Post × PCMH | −0.000902 [0.00241] | −0.00083 [0.00380] | −0.0011 [0.00311] | 0.000246 [0.00363] | 0.01957 [0.01472] | 0.01769 [0.02091] | 0.03209 [0.02479] | 0.04530 [0.03027] | 0.0566 [0.1417] | 0.0631 [0.1113] | 0.0508 [0.0470] | 0.0745 [0.0472] |
| During × PCMH | −0.00193 [0.00155] | −0.00175 [0.00247] | −0.000109 [0.00194] | −8.15E-04 [0.00240] | 0.01205 [0.00937] | 0.02636 [0.01367] | 0.03944 [0.01718] | 0.03511 [0.02152] | 0.0535 [0.0926] | 0.0767 [0.1373] | 0.0756* [0.0416] | 0.0951 [0.0663] |
| Observations | 690,456 | 266,241 | 690,456 | 266,241 | 90,285 | 35,824 | 90,285 | 35,824 | 90,285 | 35,824 | 90,285 | 35,824 |
| R2 | 0.034 | 0.047 | 0.534 | 0.391 | 0.030 | 0.031 | 0.381 | 0.413 | 0.071 | 0.073 | 0.86 | 0.762 |
| Practice fixed effects | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| Patient fixed effects | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| Patient panel sample | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
Robust standard errors in brackets.
Note: Bold values indicate ***p < .01, **p < .05, *p < 0.1.
The rows of Table2 labeled “Post × PCMH” and “During × PCMH” show the estimated coefficients derived from equation 1 with respect to the three different outcomes discussed above. We employ these models in four different pairings of sample and specification (labeled [1] through [4]). First, practice fixed effects are used and all eligible patients are analyzed. Next, the same specification is used again, but only for patients who have four full years of continuous enrollment in the IBC data. Subsequently, patient fixed effects are substituted into the model in place of practice fixed effects, and the model is rerun using first all patient-year observations and then using only the panel data. Each combination of specification and sample was used to analyze patients with and without chronic illness separately. Results for patients with chronic illness appear in the top half of the table, and patients without chronic illness appear below.
The coefficient estimates on the (Post × PCMH)it term in the first four columns of Table2 (top half) indicate a significant reduction in the number of chronically ill patients with at least one ED visit. Switching to PCMH status was associated with reductions of between 5.24 percent and 7.78 percent, compared to baseline rates of ED utilization among chronically ill patients. In addition, the coefficients on the (During × PCMH)it terms indicate reductions in patients with ED visits of between 2.7 and 4.2 percent; effects during the transition year were roughly halved in terms of magnitude.
Turning to the intensive margins—analyzing changes in number of ED visits and expenditures conditional on having at least one ED visit—none of the four specifications produced statistically significant coefficient estimates for (Post × PCMH)it. This may not be surprising for two reasons: first, patients who avoided ED visits due to their practices’ transition to PCMH status may come from the low end of the distributions of both expenditures and the annual visits (i.e., patients who were likely to experience fewer ED visits and lower ED expenditures); second, the distribution of number of visits is extremely skewed, with approximately 95 percent of patient-years, including either no ED visits or a single visit. This figure reaches 99 percent when adding patient-years with two and three ED visits. This may explain why most of the effect on ED visits among commercially insured patients is captured by the dichotomous variable, “any ED visit”.
For patients without chronic illness (bottom half of Table2), the results differ sharply from our findings with respect to chronically ill patients, indicating that PCMH implementation did not result in statistically significant reductions in the number of patients with ED visits, the number of visits, or ED expenditures, under any of the specifications used.
In Table3, we repeat the analysis from the first four columns of Table2, but restrict our outcome variables to ED visits occurring on Saturdays and Sundays and avoidable ED visits. Avoidable visits are defined using the methodology developed by Billings, Parikh, and Mijanovich (2000). In this typology, ED visits are assigned a vector of probabilities representing the likelihood of belonging to the following four categories:
Nonemergent: where immediate medical care was not required;
Emergent, yet primary care treatable: where care was needed, but could have been provided safely and effectively in a primary care setting;
Emergent, ED care needed, yet preventable: where emergent care was needed and the ED was the appropriate setting for care, but the emergency could potentially have been avoided through better management of illness; and
Emergent, ED care needed and not preventable: where ED care was necessary and the patient's condition could not have been prevented by appropriate primary care, as in the case of trauma.
Table 3.
The Effect of Patient-Centered Medical Home (PCMH) on Weekend and Avoidable Emergency Department (ED) Utilization
| [1] | [2] | [3] | [4] | [1] | [2] | [3] | [4] | |
|---|---|---|---|---|---|---|---|---|
| Dependent Variable | Any Weekend ED Visit (Chronic) | Any Avoidable ED Visit (Chronic) | ||||||
| All chronic patients | ||||||||
| Post × PCMH | −0.00721*** [0.00277] | −0.00356 [0.00376] | −0.00620* [0.00335] | −0.00447 [0.00371] | −0.00588** [0.00229] | −0.00970*** [0.00354] | −0.0107** [0.00482] | −0.0152*** [0.00418] |
| During × PCMH | −0.00529*** [0.00177] | −0.00478** [0.00241] | −0.00655*** [0.00209] | −0.00553** [0.00240] | −0.00382*** [0.00146] | −0.00642*** [0.00225] | −0.00481 [0.00309] | −0.00800*** [0.00259] |
| Observations | 393,317 | 193,435 | 393,317 | 193,435 | 393,317 | 393,317 | 193,435 | 393,317 |
| R2 | 0.046 | 0.046 | 0.508 | 0.367 | 0.025 | 0.069 | 0.066 | 0.544 |
| Dependent Variable | Any Weekend ED Visit (Nonchronic) | Any Avoidable ED Visit (Nonchronic) | ||||||
|---|---|---|---|---|---|---|---|---|
| All nonchronic patients | ||||||||
| Post × PCMH | −0.000232 [0.00155] | −0.00192 [0.00244] | −0.00094 [0.00205] | −0.00161 [0.00241] | 0.000438 [0.00207] | 0.000563 [0.00325] | 0.00138 [0.00269] | 0.00269 [0.00314] |
| During × PCMH | −8.76E-05 [0.000992] | 9.40E-05 [0.00159] | 0.000897 [0.00129] | 0.000716 [0.00160] | −0.000222 [0.00132] | 0.00206 [0.00211] | 0.00209 [0.00167] | 0.00288 [0.00207] |
| Observations | 690,456 | 266,241 | 690,456 | 266,241 | 690,456 | 266,241 | 690,456 | 266,241 |
| R2 | 0.013 | 0.018 | 0.49 | 0.328 | 0.024 | 0.03 | 0.524 | 0.372 |
| Practice fixed effects | ✓ | ✓ | ✓ | ✓ | ||||
| Patient fixed effects | ✓ | ✓ | ✓ | ✓ | ||||
| Patient panel sample | ✓ | ✓ | ✓ | ✓ | ||||
Note: Robust standard errors in brackets.
Bold values indicate ***p < 0.01, **p < 0.05, *p < 0.1.
The algorithm was constructed using IBC's detailed claims system and based on the primary diagnosis for each ED visit. Probabilities were calculated for each category, and ED visits for which the sum of the probabilities from categories (A) through (C) was greater than the probability for category (D), were labeled “avoidable” visits. We then calculated the number of avoidable and nonavoidable visits for each patient-year pair.
In addition to serving as a robustness check on the findings in Table2, using these results we can begin to disentangle the two hypothesized channels for the PCMH effect on ED utilization—improved chronic illness management versus expanded access. As primary care clinics are frequently closed to patients on weekends, we treat weekends as a proxy for “clinic closed,” and weekdays as a proxy for “clinic open.” If the PCMH effect were primarily a result of expanded office hours, we would expect to find greater effect sizes for ED utilization when most primary care clinics are closed. Similarly, while the PCMH model would be expected to reduce the frequency of ED visits resulting from poor management of chronic illness, it could do little to reduce the likelihood of events such as car accidents or other traumatic injuries. As a result, the combination of avoidable and unavoidable visits into a single category (as in Table2) may bias our estimates of PCMH effectiveness downward.
The results in Table3 indicate that PCMH implementation led to significant reductions in weekend and avoidable ED visits, among patients with chronic illness. Reductions in avoidable ED visits were significant using all four specifications and ranged from 3.50 to 9.62 percent. As expected, the reduction in avoidable ED visits is higher than for all ED visits, although the effects are similar in magnitude. On the other hand, for weekend ED visits, the results are statistically significant in the stable panel of patients (6.65 and 7.73 percent), but not in the sample of all patients. This suggests that the PCMH effect is not concentrated among weekend ED visits and lends support to the idea that the prevailing mechanism leading to reduction in ED visits is superior management of chronic conditions, rather than expanded access.
Table4 contributes additional texture to the finding that the PCMH effect on ED visits was limited to patients with chronic illness by splitting this group into its six constituent disease categories. Note again that baseline rates of ED utilization vary by chronic illness category. The achievement of PCMH recognition was associated with particularly noteworthy reductions in number of patients with ED visits for patients with diabetes. Compared to baseline rates of ED utilization among this group, PCMH status was associated with reductions ranging from 9.5 to 12.1 percent in ED visits. The PCMH effect was statistically significant in all four specifications for hypertension (ranging from 6 to 7.6 percent), three specifications for CAD (ranging from 7.4 to 10.3 percent), two specifications for CHF (ranging from 5.4 to 6.3 percent), two specifications for COPD (ranging from 10.8 to 12.2 percent), and one specification for asthma (6.1 percent). The loss of statistical significance in some cases may be the result of reduction in the number of observation within each chronic condition subset.
The reliability of results from difference-in-differences analysis depends critically upon confirming the assumption of parallel trends, which requires that the error term is uncorrelated with the term of interest (Post × PCMH)it. This assumption is important in our context, as early adopters of the PCMH model may be different than late adopters on both observable and unobservable dimensions, which may lead to issues with selection bias in our results. For example, practices that met (or were close to meeting) NCQA certification standards required comparatively minimal investments to receive certification. Nevertheless, such selection on the timing of certification would bias our results toward not finding an effect of PCMH status on ED visits, as early switchers would not have experienced drastic changes in operations and standards of service. The parallel trends assumption can be tested by plotting the time effect coefficient estimates from equation 2, which follows, versus time-to-switch.
 |
2 |
When plotting the coefficient estimates and standard errors for the various time-to-switch indicator variables, no trend is visible in the preperiod, confirming the parallel trends assumption. The full set of plots used can be found in Appendix SA3.
Discussion
Our analysis provides consistent evidence that the adoption of the PCMH model by primary care practices lowers the probability of an ED visit for chronically ill patients. Consistent with prior study (Flottemesch et al. 2012), no such effects were found for patients without chronic illness. This heterogeneity in the impact of the PCMH model suggests that the magnitude of the effect depends on the fraction of avoidable ED visits. For low medical-need patients without chronic illness, there are comparatively few ED visits to prevent. In our data, 25 percent of patient-year observations in the chronically ill patient group included at least one ED visit, compared to 13.1 percent in the patient group without chronic illness.
Even within the population of patients with chronic illness, we find that the reductions in ED visits were concentrated among certain subpopulations—namely, patients with diabetes, hypertension, and coronary artery disease. Diabetes has been of particular interest to researchers studying the PCMH model (Bojadzievski and Gabbay 2011), in part because it has been identified as an illness where early intervention and active management can offset long-term complications and reduce the substantial human and economic costs they impose (Clark et al. 2000). Though there is disagreement regarding whether the PCMH model should be applied to all patients or limited to relevant subpopulations (Berenson et al. 2008), these findings suggest that the magnitude of the PCMH effect depends on the increased fraction of avoidable ED visits among chronically ill patients as compared to patients without chronic illness.
In addition, our findings provide some insights into the mechanisms by which the PCMH impacts ED utilization. Table2 suggests that PCMH implementation reduces ED utilization, but not conditional expenditure. In other words, the changes appear to be occurring on extensive, rather than intensive margins. The results with respect to weekend visits were mixed: while reductions in “any ED visit” were significant in analyses of the patient panel sample, the two specifications using the full sample produced results that did not reach statistical significance. In addition, examining the distribution of ED encounters by day of week for patients with chronic illness, we find that it is nearly uniform. Taken together with the findings of a significant overall PCMH effect on ED utilization and larger reductions in avoidable ED visits than among visits overall, these results suggest that the PCMH effect occurred at least in part as a result of better management of chronic illness by PCMH-certified primary care practices, rather than improved access to primary care clinics.
Importantly, this study offers a number of methodological improvements including use of a dataset which represents over a million patient-years and 280 practices that received PCMH certification over 5 years. The large number of observations and the ability to exploit the timing of switch to PCMH status allowed for the use of practice or patient fixed effects terms to account for unobserved time-invariant practice or patient characteristics. We also find that these results are robust to various specifications.
Though the ability to explore the impact of the PCMH model on ED utilization in detail is one of this article's contributions, we acknowledge that emergency services are only one component of total medical spending. In addition, the PCMH model requires resources, both for achieving the various NCQA accreditation levels, and perhaps more important, maintaining them. As such, the results cannot be interpreted as net welfare effects, and further study is needed to provide the same level of detail regarding the cost of PCMH implementation as well as its effect on utilization of other medical services. As pointed out above, the determinants for the timing of PCMH certification for individual practices is difficult to ascertain and is largely beyond the scope of this study. As such understanding may yield insights into the challenges and promise of transitioning a practice to the PCMH model (Crabtree et al. 2011), we believe it should be a part of the future PCMH research agenda. While further work is needed to study other dimensions of the cost and quality impacts of the PCMH, these findings suggest that among relevant chronic illnesses, the PCMH model may be an effective tool for reducing ED utilization.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This study was funded by Independence Blue Cross. Independence Blue Cross is an independent licensee of the Blue Cross and Blue Shield Association. R. Chawla and S. Nigam are employed by Independence Blue Cross. G. David is an academic affiliate of, C. Gunnarsson is an employee of, and P. Saynisch is an consultant to CTI Clinical Trial and Consulting, which is a paid consultant to Independence Blue Cross.
The authors thank David Bishai, David Bradford, Scott Harrington, Lorens Helmchen, Jason Hockenberry, Sherry Glied, Tal Gross, Michael Grossman, Robert Town, Lindsey Sabik, and participants in the Southeastern Health Economics Study Group 2013 Conference, the American Economic Association 2014 Meetings, the American Society of Health Economists 2014 Meetings, as well as seminars participants at the University of Alabama at Birmingham, Columbia University, and Harvard University for their helpful comments and suggestions. We also thank Aaron Smith-McLallen and Cindy Wang for research support throughout the project.
Disclosures: None.
Disclaimers: None.
Notes
Results are robust to the use of propensity-score matching, as in Gilfillan et al. (2010), to create a pool of matched non-PCMH practices for use as controls in our analysis. Results were qualitatively similar and are available from the authors upon request.
“Unusually high ED expenditures” were defined by adding three times the inter-quartile range to the 75th percentile ED expenditure.
Marginal effects estimated using a Probit model yield highly comparable results. This information is available from the authors upon request.
Results are robust to the exclusion of Fracit.
Supporting Information
Appendix SA1: Author Matrix.
Appendix SA2: Attrition Diagram.
Appendix SA3: Testing for Parallel Trends.
References
- American Academy of Family Physicians. Joint Principles of the Patient-Centered Medical Home. Washington, DC: Patient-Centered Primary Care Collaborative; 2007. American Academy of Pediatrics, American College of Physicians, and American Osteopathic Association. [Google Scholar]
- American College of Physicians. Reform of the Dysfunctional Healthcare Payment and Delivery System. Philadelphia, PA: American College of Physicians; 2006. [Google Scholar]
- Berenson RA, Hammons T, Gans DN, Zuckerman S, Merrell K, Underwood WS. Williams AF. A House is Not a Home: Keeping Patients at the Center of Practice Redesign. Health Affairs. 2008;27(5):1219–30. doi: 10.1377/hlthaff.27.5.1219. [DOI] [PubMed] [Google Scholar]
- Billings J, Parikh N. Mijanovich T. Emergency Department Use: The New York Story. New York, NY: The Commonwealth Fund; 2000. [PubMed] [Google Scholar]
- Bodenheimer T, Grumbach K. Berenson RA. A Lifeline for Primary Care. The New England Journal of Medicine. 2009;360(26):2693–6. doi: 10.1056/NEJMp0902909. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Wagner EH. Grumbach K. Improving Primary Care for Patients with Chronic Illness. Journal of the American Medical Association. 2002;288(14):1775–9. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- Bojadzievski T. Gabbay RA. Patient-Centered Medical Home and Diabetes. Diabetes Care. 2011;34(4):1047–53. doi: 10.2337/dc10-1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy A. Patient-Centered Medical Homes. Health Affairs. 2010 September 14. [Google Scholar]
- Chandra A, Gruber J. McKnight R. The Importance of the Individual Mandate–Evidence from Massachusetts. New England Journal of Medicine. 2011;364(4):293–5. doi: 10.1056/NEJMp1013067. [DOI] [PubMed] [Google Scholar]
- Clark CM, Fradkin JE, Hiss RG, Lorenz RA, Vinicor F. Warren-Boulton E. Promoting Early Diagnosis and Treatment of Type 2 Diabetes: The National Diabetes Education Program. Journal of the American Medical Association. 2000;284(3):363–5. doi: 10.1001/jama.284.3.363. [DOI] [PubMed] [Google Scholar]
- Crabtree BF, Chase SM, Wise CG, Schiff GD, Schmidt LA, Goyzueta JR, Malouin RA, Payne SM, Quinn MT, Nutting PA, Miller WL. Jaen CR. Evaluation of Patient Centered Medical Home Practice Transformation Initiatives. Medical Care. 2011;49(1):10–6. doi: 10.1097/MLR.0b013e3181f80766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devries A, Li CH, Sridhar G, Hummel JR, Breidbart S. Barron JJ. Impact of Medical Homes on Quality, Healthcare Utilization, and Costs. American Journal of Managed Care. 2012;18(9):534–44. [PubMed] [Google Scholar]
- Domino ME, Humble C, Lawrence WW., Jr Wegner S. Enhancing the Medical Homes Model for Children with Asthma. Medical Care. 2009;47(11):1113–20. doi: 10.1097/MLR.0b013e3181adcc65. [DOI] [PubMed] [Google Scholar]
- Flottemesch TJ, Anderson LH, Solberg LI, Fontaine P. Asche SE. Patient-Centered Medical Home Cost Reductions Limited to Complex Patients. American Journal of Managed Care. 2012;18(11):677–86. [PubMed] [Google Scholar]
- Friedberg MW, Lai DJ, Hussey PS. Schneider EC. A Guide to the Medical Home as a Practice-Level Intervention. American Journal of Managed Care. 2009;15(10 Suppl):S291–9. [PubMed] [Google Scholar]
- Gilfillan RJ, Tomcavage J, Rosenthal MB, Davis DE, Graham J, Roy JA. Steele GD. Value and the Medical Home: Effects of Transformed Primary Care. American Journal of Managed Care. 2010;16(8):607–14. [PubMed] [Google Scholar]
- Harbrecht MG. Latts LM. Colorado's Patient-Centered Medical Home Pilot Met Numerous Obstacles, Yet Saw Results Such as Reduced Hospital Admissions. Health Affairs. 2012;31(9):2010–7. doi: 10.1377/hlthaff.2012.0359. [DOI] [PubMed] [Google Scholar]
- Hearld LR. Alexander JA. Patient-Centered Care and Emergency Department Utilization: A Path Analysis of the Mediating Effects of Care Coordination and Delays in Care. Medical Care Research and Review. 2012;69(5):560–80. doi: 10.1177/1077558712453618. [DOI] [PubMed] [Google Scholar]
- Jackson GL, Powers BJ, Chatterjee R, Bettger JP, Kemper AR, Hasselblad V, Dolor RJ, Irvine RJ, Heidenfelder BL, Kendrick AS, Gray R. Williams JW., Jr The Patient-Centered Medical Home: A Systematic Review. Annals of Internal Medicine. 2013;158(3):169–78. doi: 10.7326/0003-4819-158-3-201302050-00579. [DOI] [PubMed] [Google Scholar]
- Joynt KE, Chan D, Orav EJ. Jha AK. Insurance Expansion in Massachusetts Did Not Reduce Access among Previously Insured Medicare Patients. Health Affairs. 2013;32(3):571–8. doi: 10.1377/hlthaff.2012.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilo CM. Wasson JH. Practice Redesign and the Patient-Centered Medical Home: History, Promises, and Challenges. Health Affairs. 2010;29(5):773–8. doi: 10.1377/hlthaff.2010.0012. [DOI] [PubMed] [Google Scholar]
- Leff B, Reider L, Frick KD, Scharfstein DO, Boyd CM, Frey K, Karm L. Boult C. Guided Care and the Cost of Complex Healthcare: A Preliminary Report. American Journal of Managed Care. 2009;15(8):555–9. [PubMed] [Google Scholar]
- Moore G. Showstack J. Primary Care Medicine in Crisis: Toward Reconstruction and Renewal. Annals of Internal Medicine. 2003;138(3):244–7. doi: 10.7326/0003-4819-138-3-200302040-00032. [DOI] [PubMed] [Google Scholar]
- National Committee for Quality Assurance. Standards and Guidelines for Physician Practice Connections®—Patient-Centered Medical Home (PPC-PCMH™) Washington, DC: National Committee for Quality Assurance; 2008. [Google Scholar]
- National Committee for Quality Assurance. NCQA Standards Workshop: Patient-Centered Medical Home—PCMH 2011. Washington, DC: National Committee for Quality Assurance; 2011. [Google Scholar]
- O'Malley AS. After-Hours Access to Primary Care Practices Linked with Lower Emergency Department Use and Less Unmet Medical Need. Health Affairs. 2013;32(1):175–83. doi: 10.1377/hlthaff.2012.0494. [DOI] [PubMed] [Google Scholar]
- Paustian ML, Alexander JA, El Reda DK, Wise CG, Green LA. Fetters MD. Partial and Incremental PCMH Practice Transformation: Implications for Quality and Costs. Health Services Research. 2013;49(1):52–74. doi: 10.1111/1475-6773.12085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peikes D, Dale S, Lundquist E, Genevro J. Meyers D. Building the Evidence Base for the Medical Home: What Sample and Sample Size Do Studies Need? Rockville, MD: 2011. , and White Paper (Prepared by Mathematica Policy Research). [Google Scholar]
- Peikes D, Zutshi A, Genevro JL, Parchman ML. Meyers DS. Early Evaluations of the Medical Home: Building on a Promising Start. American Journal of Managed Care. 2012;18(2):105–16. [PubMed] [Google Scholar]
- Reid RJ, Fishman PA, Yu O, Ross TR, Tufano JT, Soman MP. Larson EB. Patient-Centered Medical Home Demonstration: A Prospective, Quasi-Experimental, before and after Evaluation. American Journal of Managed Care. 2009;15(9):e71–87. [PubMed] [Google Scholar]
- Reid RJ, Coleman K, Johnson EA, Fishman PA, Hsu C, Soman MP, Trescott CE, Erikson M. Larson EB. The Group Health Medical Home at Year Two: Cost Savings, Higher Patient Satisfaction, and Less Burnout for Providers. Health Affairs. 2010;29(5):835–43. doi: 10.1377/hlthaff.2010.0158. [DOI] [PubMed] [Google Scholar]
- Solberg LI, Asche SE, Fontaine P, Flottemesch TJ. Anderson LH. Trends in Quality during Medical Home Transformation. Annals of Family Medicine. 2011;9(6):515–21. doi: 10.1370/afm.1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verisk Health Inc. Sightlines DxCG Risk Solutions: Concepts and Methodologies Guide for UNIX. Waltham, MA: Verisk Health Inc; 2010. [Google Scholar]
- Wagner EH, Austin BT. Von Korff M. Organizing Care for Patients with Chronic Illness. The Milbank Quarterly. 1996;74(4):511–44. [PubMed] [Google Scholar]
- Weinick RM, Burns RM. Mehrotra A. Many Emergency Department Visits Could Be Managed at Urgent Care Centers and Retail Clinics. Health Affairs. 2010;29(9):1630–6. doi: 10.1377/hlthaff.2009.0748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner RM, Duggan M, Duey K, Zhu J. Stuart EA. The Patient-Centered Medical Home: An Evaluation of a Single Private Payer Demonstration in New Jersey. Medical Care. 2013;51(6):487–93. doi: 10.1097/MLR.0b013e31828d4d29. [DOI] [PubMed] [Google Scholar]
- Wise CG, Bahl V, Mitchell R, West BT. Carli T. Population-Based Medical and Disease Management: An Evaluation of Cost and Quality. Disease Management. 2006;9(1):45–55. doi: 10.1089/dis.2006.9.45. [DOI] [PubMed] [Google Scholar]
- Zuckerman B, Parker S, Kaplan-Sanoff M, Augustyn M. Barth MC. Healthy Steps: A Case Study of Innovation in Pediatric Practice. Pediatrics. 2004;114(3):820–6. doi: 10.1542/peds.2003-0999-L. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Appendix SA2: Attrition Diagram.
Appendix SA3: Testing for Parallel Trends.


