Abstract
Breast cancer and its treatment can significantly affect a woman’s body image. As such, it would be useful to understand the importance or value these patients place on their appearance. We evaluated the factor structure of the Appearance Schemas Inventory- Revised (ASI-R), a measure of body image investment, with a sample of 356 breast cancer patients undergoing mastectomy and breast reconstruction. Using confirmatory and exploratory factor analyses, we found that a 3-factor model demonstrated an improvement in fit over the original 2-factor structure of the ASI-R. These factors were named Appearance Self-Evaluation, Appearance Power/Control, and Appearance Standards and Behavior. The three aforementioned factors demonstrated acceptable internal consistency reliabilities. Our findings have implications for the use of the ASI-R in an oncology setting, specifically for breast cancer patients undergoing reconstruction.
Keywords: body image, body image investment, exploratory factor analysis, confirmatory factor analysis, breast cancer, breast reconstruction
Breast cancer treatment often results in significant alteration to one’s breast(s), including changes in appearance (e.g., size and symmetry), skin texture, and sensation. For women undergoing a mastectomy, breast reconstruction offers a treatment option to assist in rebuilding their breast(s) and is known to provide important psychological benefits related to body image, sexuality, and quality of life (Cordeiro, 2008; Wilkins et al., 2000). Although there are many factors women must consider when choosing whether to undergo breast reconstruction following mastectomy, restoration of body image is found to be a primary motivating reason (Duggal, Metcalfe, Sackeyfio, Carlson, & Losken, 2013; Figueiredo, Cullen, Hwang, Rowland, & Mandelblatt, 2004). Research suggests that 42–67% of women who receive surgical treatment for breast cancer opt for reconstruction (Jagsi et al., 2014; Morrow et al., 2014).
Women undergoing breast reconstruction often face an extensive period of appearance alterations involving multiple surgical procedures occurring over a span of months to years. Although breast reconstruction has been shown to have positive benefits for women’s social and psychological well-being (Cordeiro, 2008), many women receiving reconstruction are found to endorse body image difficulties that can persist even years post treatment (Sackey, Sandelin, Frisell, Wickman, & Brandberg, 2010). Considerable research is devoted to comparing body image and quality of life outcomes for women undergoing breast conservation therapy (BCT), mastectomy alone, or mastectomy with reconstruction. Studies report conflicting findings; however, higher rates of body image concerns have been repeatedly found among patients treated with mastectomy and reconstruction compared to BCT (Fobair et al., 2006; Rosenberg et al., 2012; Sackey et al., 2010; Shoma et al., 2009). A recent meta-analysis by Fang and colleagues offers further insight in this area showing that women with breast reconstruction experience significantly higher levels of body stigma compared to women treated with BCT (Fang, Shu, & Chang, 2013). Body stigma encompasses the loss of bodily integrity due to alteration of the body and removal of the breast. These findings reflect the complex nature of body image which encompass more than satisfaction with appearance.
Another component of body image which may be particularly relevant for patients undergoing breast reconstruction is body image investment, which refers to the value or importance placed on appearance and physical attributes. Adachi et al., found that patients having immediate breast reconstruction valued appearance and attractiveness to their partner more significantly than patients undergoing mastectomy alone or BCT (Adachi, Ueno, Fujioka, Fujitomi, & Ueo, 2007). Other studies have found associations between appearance investment, depression, and quality of life outcomes for breast cancer survivors irrespective of type of treatment (Moreira & Canavarro, 2010, 2012). A longitudinal study evaluating body image and psychosocial adjustment of breast cancer patients during the course of treatment further found that body image investment was a significant predictor of subsequent self-consciousness of appearance, body shame, and appearance satisfaction (Moreira, Silva, & Canavarro, 2010). As such, it is believed that further efforts to examine body image investment in breast cancer patients in warranted. This may be particularly valuable to study in women choosing reconstructive treatment, as understanding the importance these women place on their appearance may help explain variance in their satisfaction with reconstruction outcomes.
Most research evaluating body image investment in breast cancer survivors has used the Appearance Schemas Inventory-Revised (ASI-R) (Cash, 2003; Cash, Melnyk, & Hrabosky, 2004). This measure was originally developed and validated for use in college-aged individuals. Previous work found the ASI-R to be comprised of 2 factors: (1) Self-Evaluative Salience, the extent someone believes his or her looks influences personal worth and sense of self, and (2) Motivational Salience, the extent one engages in behaviors to manage his or her appearance (Cash et al., 2004). Important distinctions have been found between these factors, such that high motivational salience has been associated with better body image outcomes whereas high self-evaluative salience has shown a negative relationship with appearance satisfaction following breast cancer treatment (Moreira et al., 2010).
Prior to conducting further research utilizing the ASI-R with breast cancer patients, it is important to evaluate the factor structure of this measure to determine its usefulness with this patient group. A common research error is to rely on published reports of psychometric validity when using a scale with a different population (Rusticus, Hubley, & Zumbo, 2008; Thompson, 2004). Our purpose was to examine the dimensions/latent constructs underlying the ASI-R for breast cancer patients undergoing reconstruction. We hypothesized that breast cancer patients who undergo reconstructive treatment will have a unique response pattern on the ASI-R compared to college-age individuals. As far as we know, this is the first study to examine the factor structure of the ASI-R in a breast cancer population.
Method
Participants
This study involves a secondary analysis of a larger ongoing longitudinal project designed to evaluate appearance changes and body image outcomes for women undergoing breast reconstruction. Only data from participants who completed all ASI-R items at their baseline study visit were included in the current study. Participants were recruited from the Center for Reconstructive Surgery at The University of Texas MD Anderson Cancer Center (MDACC). To be eligible, participants had to be female, English-speaking, 21 years or older, and planning to undergo breast reconstruction following mastectomy. Participants were asked to complete the ASI-R as part of an initial psychosocial assessment. All procedures were reviewed and approved by the MDACC Institutional Review Board.
Measures
The Appearance Schemas Inventory-Revised (ASI-R) is a 20-item self-report measure designed to assess body image investment (Cash, 2003; Cash et al., 2004). Items are rated on a 5-point Likert scale from 1 ‘strongly disagree’ to 5 ‘strongly agree’. Principal component analysis (PCA) with varimax rotation revealed that the best solution was a two-factor structure with 12 items loading on the first factor (Self-Evaluative Salience) and 8 items on the second factor (Motivational Salience) (Cash et al., 2004).
Analytic Plan
We generated descriptive statistics for our sample and individual items on the ASI-R. We then entered items from the previously established factors of Self-Evaluative Salience and Motivational Salience as the two latent variables for a 2-factor confirmatory analysis (CFA). We used the chi-square goodness-of-fit test for the difference between expected and observed covariance matrices to test the appropriateness of the 2-factor structure. We also assessed likelihood-ratio test, Akaike’s information criteria (AIC), standardized root mean square residual (SRMR), Goodness of Fit Index (GFI), Bentler-Bonett Normed Fit Index (NFI), and Root Mean Square Error of Approximation (RMSEA) (Hu & Bentler, 1999).
Due to lack of fit of CFA, we conducted an exploratory factor analysis (EFA) with principal axis factoring (PAF) extraction method to further identify the number of latent constructs for the ASI-R. In order to reduce bias, we randomly split our sample (N = 356) into two datasets of equal size, a “training sample” (n = 178), and a “holdout sample” (n = 178). Utilizing the training sample, the final factor structure was extracted using factor analysis with oblique promax rotation with eigenvalue > 1.0 rule and via an examination of the scree plot (Tabachnick & Fidell, 2001).The oblique rotation method was employed because the inter-item correlations revealed moderate correlations (r > .40) for more than half of the items within the ASI-R measure via Spearman correlation analysis. Subsequently, using the weighted least square mean and variance (WLSMV) estimation, a CFA was carried out for the holdout sample to confirm the model identified from the EFA. Model fit was evaluated through the indices used in our first CFA model. In assessing the reliability of the final factor structure, we also calculated the internal consistency with Cronbach’s alpha for each factor via the holdout sample. We implemented all analyses in SAS Version 9.3 (SAS Institute Inc., Cary, NC).
Results
Descriptive Statistics
Of the 373 participants who completed the ASI-R, 17 participants had one or more missing response(s) for the 20 items. Thus, 356 participants were included in the analysis. Our sample of 356 women had a mean age of 49.43 (SD = 10.3); 74.3% were White, 11.3% were Black, and most participants (77.25%) were non-Hispanic. The majority (72.75%) were married and 68.6% had a college education or higher. Cancer types included invasive ductal carcinoma (53.4%), ductal carcinoma in situ (21.57%), invasive lobular carcinoma (9.6%), lobular carcinoma in situ (1.29%), and other (13.28%). Some participants had received adjuvant treatment consisting of chemotherapy (45.8%), radiation therapy (28.32%) or both (21.81%). Distributions of the ASI-R scores showed skewness and kurtosis within normal limits. When considering the original 2-factor structure of the ASI-R, our sample had the following mean scores: Self-Evaluative Salience M = 2.96 (SD = 0.72), Motivational Salience M = 3.77 (SD = 0.67), composite M = 3.28 (SD = 0.59).
Factor Analyses
None of the model fit indices for the 2-factor CFA indicated a good fit (χ2= 650.26, AIC = 732.26, SRMR = .09, GFI = .84, NFI = .71, and RMSEA = .09). Thus, the EFA was performed on the training sample. The inspection of scree plot, factor and structure matrices showed three factors explained the majority of the variance in the data (Table 1). Factor 1 consisted of 8 items, representing “Appearance Self-Evaluation” with an eigenvalue of 3.92, accounting for 50.95% of variance. Factor 2 consisted of 5 items, representing “Appearance Power/Control” with an eigenvalue of 2.21, accounting for 28.76% of variance. Lastly, factor 3 consisted of 7 items, representing “Appearance Standards & Behaviors” with an eigenvalue of 1.17, accounting for 15.22% of variance.
Table 1.
Pattern Matrix with Factor Loadings for ASI-R items (n = 178)
| Factor | |||
|---|---|---|---|
| Factor/Scale Name and Item | 1 | 2 | 3 |
| Factor 1: Appearance Self-Evaluation | |||
| 2. When I see good-looking people, I wonder how my own looks measure up. | .63 | .17 | .02 |
| 5. I seldom compare my appearance to that of other people I see.a | .50 | −.01 | .14 |
| 7. When something makes me feel good or bad about my looks, I tend to dwell on it. | .61 | .15 | .06 |
| 9. If somebody had a negative reaction to what I look like, it wouldn’t bother me.a | .50 | −.06 | .08 |
| 11. My physical appearance has had little influence on my life.a | .48 | −.07 | .27 |
| 13. When I meet people for the first time, I wonder what they think about how I look. | .47 | .28 | .02 |
| 15. If I dislike how I look on a given day, it’s hard to feel happy about other things. | .56 | .30 | .16 |
| 16. I fantasize about what it would be like to be better looking than I am. | .49 | .29 | .28 |
| Factor 2: Appearance Power/Control | |||
| 8. If I like how I look on a given day, it’s easier to feel happy about other things. | .24 | .41 | .13 |
| 14. In my everyday life, lots of things happen that make me think about what I look like. | .26 | .48 | .07 |
| 18. What I look like is an important part of who I am. | .04 | .73 | .22 |
| 19. By controlling my appearance, I can control many aspects of the social and emotional events in my life. | .06 | .78 | .07 |
| 20. My appearance is responsible for much of what’s happened to me in my life. | .21 | .68 | .03 |
| Factor 3: Appearance Standards & Behavior | |||
| 1. I spend little time on my physical appearance.a | −.15 | −.04 | .37 |
| 3. I try to be as physically attractive as I can be. | −.05 | .09 | .51 |
| 4. I have never paid much attention to what I look like.a | .16 | −.02 | .45 |
| 6. I often check my appearance in a mirror just to make sure I look okay. | .15 | .24 | .51 |
| 10. When it comes to my physical appearance, I have high standards. | −.04 | .28 | .59 |
| 12. Dressing well is not a priority for me.a | .09 | −.04 | .56 |
| 17. Before going out, I make sure I look as good as I possibly can. | −.16 | .25 | .51 |
| Eigenvalue | 3.92 | 2.21 | 1.17 |
| Variance explained (%) | 50.95 | 28.76 | 15.22 |
| Cumulative variance explained (%) | 50.95 | 79.71 | 94.94 |
Note. Factor loadings > .30 are in boldface. The copyrighted ASI-R and its items may not be used without obtaining the assessment and its author’s permission via www.body-images.com. Permission for the current use was given by Thomas F. Cash, Ph.D.
Reverse-scored item.
Utilizing Cohen’s (1988) criteria, the inter-factor correlation matrix for the three factors revealed a moderate correlation between Appearance Self-Evaluation and Appearance Power/Control (r = .32) and low correlations for the following factor pairs: (1) Appearance Standards and Behavior and Appearance Power/Control (r = .16), and (2) Appearance Self-Evaluation and Appearance Standards and Behavior (r = .15), confirming that the oblique rotation was an appropriate technique for the EFA. These correlations fell within the criteria for a separate factor consideration (r < .80) within the realm of oblique rotations (Meyers, Gamst, & Guarino, 2006; Tabachnick & Fidell, 2001).
Finally, the CFA for this 3-factor model utilizing the holdout sample (Figure 1) resulted in the following indices values: χ2= 418.7, AIC = 504.7, SRMR = .09, GFI = .91, NFI = .88, and RMSEA = .08, thus demonstrating an improved fit from the previous 2-factor model. Cronbach’s alphas of .78, .77, and .72 for Appearance Self-Evaluation, Appearance Power/Control, and Appearance Standards and Behavior, respectively, provided evidence of internal consistency reliabilities for the three subscales.
Figure 1.
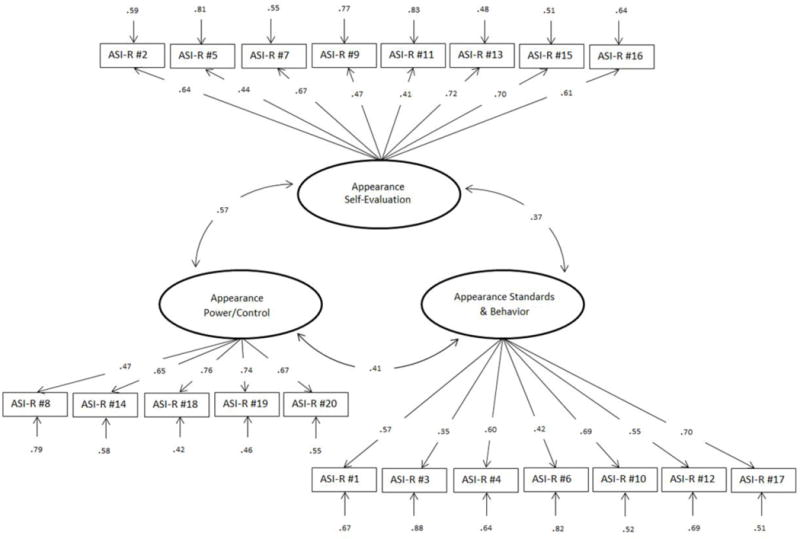
First-order Confirmatory Factor Analysis (CFA) model for a 3-factor solution in the ASI-R measure (n = 178). Please refer to Table 1 for full item description.
Discussion
Our primary aim was to evaluate the factor structure of the ASI-R, a measure of body image investment, in a sample of breast cancer patients undergoing reconstruction. These women can face significant appearance alterations over an extended period of time and are at risk of experiencing difficulties adjusting to body image changes resulting from breast cancer treatment. Greater understanding of the value they place on their physical appearance prior to undergoing reconstruction is clinically warranted, and may be an important predictor of their resulting body image and satisfaction with treatment outcomes. Prior to conducting further research examining body image investment using the ASI-R with this patient population, it is necessary to conduct a more thorough examination of its psychometric properties. As far as we know, this is the first study to examine the factor structure of the ASI-R in a sample of women with breast cancer.
We found evidence supporting a 3-factor structure for the ASI-R and named these factors (1) Appearance Self-Evaluation, (2) Appearance Power/Control and (3) Appearance Standards/Behaviors. Factors 1 and 3 closely align with previously identified factors of the ASI-R found in Cash et al. (2004). Factor 1, Appearance Self-Evaluation, reflects preoccupation with appearance and negative self-evaluation of one’s appearance and aligns most closely with the previously identified Self-Evaluative Salience scale. Factor 3, Appearance Standards and Behavior, reflects time and effort spent on appearance-fixing behaviors and holding high standards for one’s appearance. Factor 3 most closely aligns and shares items derived from the Motivational Salience scale. Most notably, we found evidence supporting the emergence of an additional factor, which we labeled Appearance Power/Control (Factor 2). This factor reflects appearance being an important part of one’s identity, and appearance having power/control over one’s emotions, thoughts, and behaviors. Factor 2 is comprised of four items from the previous Self-Evaluative Salience scale (Items 8, 14, 19, and 20) and one item from the previous Motivational Salience scale (Item 18). The Appearance Power/Control factor may have specific relevance for women with breast cancer when they perceive appearance changes stemming from their illness and its treatment as being beyond their control and having a significant negative influence on their lives. Breast reconstruction can be considered a means by which one can exert some control over appearance changes from breast cancer, thereby offering further clinical considerations in this regard.
Additional research is needed to understand how the ASI-R can be optimally used by healthcare professionals working with breast cancer survivors. It is important to determine if patient scores using the newly identified factor structure are predictive of scores on other body image measures evaluating appearance satisfaction, body stigma, body image coping, and bodily integrity. There is a further need to examine whether ASI-R scores are predictive of other patient-reported outcomes relevant to breast cancer treatment. It is hoped that further understanding of patients’ body image investment prior to undergoing breast cancer treatment can aid healthcare professionals in more effectively addressing their body image concerns and identifying when more comprehensive psychosocial support may be needed.
This study has several limitations. Our study sample included a select group of breast cancer patients (i.e., those undergoing reconstruction). Future studies need to include breast cancer patients treated with BCT or mastectomy alone, as there is reason to suspect body image investment may differ significantly between these groups. The modest sample sizes of the training and holdout samples (n = 178) may have reduced the generalizability of our findings. Nevertheless, the internal consistency reliabilities for the factor scores still hold (α ≥ .70), indicating that the factors are valid for our sample. Also, the majority of our sample consisted of white women, affecting the generalization of findings to other racial groups. In terms of the CFA model’s goodness-of-fit, although we are convinced that the 3-factor is the best fitting model, the solution remains borderline adequate by traditional CFA standards, particularly for the GFI and NFI indices (Byrne, 2013). Despite these limitations, this study provides relevant information about the factor structure of the ASI-R in a breast cancer sample and contributes to further exploring the construct of body image investment within this patient population.
Highlights.
The ASI-R is a relevant measure for breast cancer patients undergoing reconstruction.
The factor structure of our sample differed from that of a female college sample.
We found evidence supporting a 3-factor model.
Our findings provide insight on assisting this population with body image changes.
Acknowledgments
This work was supported in part by Grant R01CA133190 from the National Institutes of Health and by the University of Texas MD Anderson Cancer Support Grant CA016772.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Alicia S. Chua is now at Department of Neurology, Brigham and Women’s Hospital, Boston, Massachusetts.
References
- Adachi K, Ueno T, Fujioka T, Fujitomi Y, Ueo H. Psychosocial factors affecting the therapeutic decision-making and postoperative mood states in Japanese breast cancer patients who underwent various types of surgery: Body image and sexuality. Japanese Journal of Clinical Oncology. 2007;37:412–418. doi: 10.1093/jjco/hym041. [DOI] [PubMed] [Google Scholar]
- Byrne BM. Structural equation modeling with AMOS: Basic concepts, applications, and programming. New York, NY: Routledge; 2013. [Google Scholar]
- Cash TF. Brief manual for the Appearance Schemas Inventory-Revised. 2003 Retrieved September 29 2014, from http://www.body-images.com/assessments/order.html.
- Cash TF, Melnyk SE, Hrabosky JI. The assessment of body image investment: An extensive revision of the Appearance Schemas Inventory. International Journal of Eating Disorders. 2004;35:305–316. doi: 10.1002/eat.10264. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale NJ: Erlbaum; 1988. [Google Scholar]
- Cordeiro PG. Breast reconstruction after surgery for breast cancer. New England Journal of Medicine. 2008;359:1590–1601. doi: 10.1056/NEJMct0802899. [DOI] [PubMed] [Google Scholar]
- Duggal CS, Metcalfe D, Sackeyfio R, Carlson GW, Losken A. Patient motivations for choosing postmastectomy breast reconstruction. Annals of Plastic Surgery. 2013;70:574–580. doi: 10.1097/SAP.0b013e3182851052. [DOI] [PubMed] [Google Scholar]
- Fang SY, Shu BC, Chang YJ. The effect of breast reconstruction surgery on body image among women after mastectomy: A meta-analysis. Breast Cancer Research and Treatment. 2013;137:13–21. doi: 10.1007/s10549-012-2349-1. [DOI] [PubMed] [Google Scholar]
- Figueiredo MI, Cullen J, Hwang YT, Rowland JH, Mandelblatt JS. Breast cancer treatment in older women: Does getting what you want improve your long-term body image and mental health? Journal of Clinical Oncology. 2004;22:4002–4009. doi: 10.1200/JCO.2004.07.030. [DOI] [PubMed] [Google Scholar]
- Fobair P, Stewart SL, Chang S, D’Onofrio C, Banks PJ, Bloom JR. Body image and sexual problems in young women with breast cancer. Psycho-Oncology. 2006;15:579–594. doi: 10.1002/pon.991. [DOI] [PubMed] [Google Scholar]
- Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Jagsi R, Jiang J, Momoh AO, Alderman A, Giordano SH, Smith BD. Trends and variation in use of breast reconstruction in patients with breast cancer undergoing mastectomy in the United States. Journal of Clinical Oncology. 2014 doi: 10.1200/JCO.2013.52.2284. [DOI] [PMC free article] [PubMed]
- Meyers LS, Gamst G, Guarino AJ. Applied multivariate research design and interpretation. Newbury Park, CA: Sage; 2006. [Google Scholar]
- Moreira H, Canavarro MC. A longitudinal study about the body image and psychosocial adjustment of breast cancer patients during the course of the disease. European Journal of Oncology Nursing. 2010;14:263–270. doi: 10.1016/j.ejon.2010.04.001. [DOI] [PubMed] [Google Scholar]
- Moreira H, Canavarro MC. The association between self-consciousness about appearance and psychological adjustment among newly diagnosed breast cancer patients and survivors: The moderating role of appearance investment. Body Image. 2012;9:209–215. doi: 10.1016/j.bodyim.2011.11.003. [DOI] [PubMed] [Google Scholar]
- Moreira H, Silva S, Canavarro MC. The role of appearance investment in the adjustment of women with breast cancer. Psycho-Oncology. 2010;19:959–966. doi: 10.1002/pon.1647. [DOI] [PubMed] [Google Scholar]
- Morrow M, Li Y, Alderman AK, Jagsi R, Hamilton AS, Graff JJ, Katz SJ. Access to breast reconstruction after mastectomy and patient perspectives on reconstruction decision making. JAMA Surgery. 2014;149:1015–1021. doi: 10.1001/jamasurg.2014.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg SM, Tamimi RM, Gelber S, Ruddy KJ, Kereakoglow S, Borges VF, Partridge AH. Body image in recently diagnosed young women with early breast cancer. Psycho-Oncology. 2012;22:1848–1855. doi: 10.1002/pon.3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusticus SA, Hubley AM, Zumbo BD. Measurement invariance of the Appearance Schemas Inventory–Revised and the Body Image Quality of Life Inventory across age and gender. Assessment. 2008;15:60–71. doi: 10.1177/1073191107306805. [DOI] [PubMed] [Google Scholar]
- Sackey H, Sandelin K, Frisell J, Wickman M, Brandberg Y. Ductal carcinoma in situ of the breast. Long-term follow-up of health-related quality of life, emotional reactions and body image. European Journal of Surgical Oncology. 2010;36:756–762. doi: 10.1016/j.ejso.2010.06.016. [DOI] [PubMed] [Google Scholar]
- Shoma AM, Mohamed MH, Nouman N, Amin M, Ibrahim IM, Tobar SS, William SG. Body image disturbance and surgical decision making in egyptian post menopausal breast cancer patients. World Journal of Surgical Oncology. 2009;7:66. doi: 10.1186/1477-7819-7-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 4. New York, NY: Allyn & Bacon; 2001. [Google Scholar]
- Thompson JK. The (mis) measurement of body image: Ten strategies to improve assessment for applied and research purposes. Body Image. 2004;1:7–14. doi: 10.1016/S1740-1445(03)00004-4. [DOI] [PubMed] [Google Scholar]
- Wilkins EG, Cederna PS, Lowery JC, Davis JA, Kim HM, Roth RS, Shaheen KW. Prospective analysis of psychosocial outcomes in breast reconstruction: One-year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plastic and Reconstructive Surgery. 2000;106:1014–1025. doi: 10.1097/00006534-200010000-00010. [DOI] [PubMed] [Google Scholar]


