Abstract
The purpose of this pilot study was to determine the inter-rater reliability of four clinical manifestations of catheter-associated urinary tract infections (CAUTI) among hospitalized adults with short-term indwelling urinary catheters using a tool developed for this purpose: the CAUTI Assessment Profile (CAP). Study participants included 30 non-pregnant English-speaking adults, recruited from 2 community hospitals. Three nurses assessed each participant for fever, suprapubic tenderness, flank tenderness, and delirium using standardized techniques. Based on the generalized kappa statistic and 95% confidence intervals, there was evidence of strong inter-rater reliability for fever (K = 1.00, 0.793 – 1.207), suprapubic tenderness (K = 0.39, 0.185 – 0.598), and delirium (K = 0.58, 0.379 – 0.792), but not for flank tenderness (K = 0.29, −0.036 – 0.617). This study provides preliminary evidence that the CAUTI Assessment Profile (CAP) can be used to consistently identify these clinical signs and symptoms of CAUTI in hospitalized adults.
Keywords: Reliability, Urinary Tract Infection, Catheter Associated Urinary Tract Infection, CAUTI, Kappa
Hospital-acquired urinary tract infections (UTI), which includes catheter-associated UTI (CAUTI), account for 40% of all nosocomial infections in U.S. hospitals each year (Cairns et al., 2011; Tambyah, Knasinski, & Maki, 2002). Approximately 25% of hospitalized patients will undergo urinary catheterization (Saint, 2000), and nearly 30% of these will develop CAUTI (Warren, 2001; Weber et al., 2011), or another non-infectious complication of catheterization (Dellimore, Helyer, & Franklin, 2013; Hollingsworth et al., 2013). CAUTI has been associated with a variety of undesirable clinical outcomes, including antimicrobial resistance, urinary calculi, bloodstream infection, sepsis, and death (Kang et al., 2011; Ko et al., 2008; Milan & Ivan, 2009), although the frequency of these complications may not be as high as once thought (Kizilbash, Petersen, Chen, Naik, & Trautner, 2013). Through these and other complications, CAUTI can substantially raise the cost of hospitalization by as much as 31% (Kennedy, Greene, & Saint, 2013; Kurtzman & Buerhaus, 2008; Zimlichman et al., 2013). Furthermore, the inappropriate, and often prolonged, use of indwelling urinary catheters in the hospital setting places patients at unnecessary risk for harm (Gokula, Hickner, & Smith, 2004; Janzen et al., 2013; Leuck et al., 2012; Tiwari, Charlton, Anderson, Hermsen, & Rupp, 2012). Clearly, CAUTI represents a common hospital-acquired condition with potentially devastating clinical and economic consequences.
CAUTI results from a significant concentration of pathogens and manifests in a host inflammatory response. A combination of biochemical, microbiological, and/or molecular laboratory techniques are used to identify significant bacteriuria, but these testing methods have limitations that can interfere with the timely and accurate diagnosis of CAUTI. Biochemical tests, such as urinary dipstick testing for nitrite and leukocyte esterase, can be performed quickly at the point-of-care with little cost. However, several factors affect the reliability and validity of these tests including the patient’s intake of certain substances, urine color, the type of catheter materials used, and the strain of microorganism present in the urine (Kayalp, Dogan, Ceylan, Senes, & Yucel, 2013; Kupelian et al., 2013). Microbiological tests, such as quantitative urine culture, are considered to be the “gold standard” for determining significant bacteriuria. However, the diagnostic cut-point for significant bacteriuria remains unclear and can vary between populations (Horan, Andrus, & Dudeck, 2008). Furthermore, microbiological tests are unable to differentiate pathogenic microorganisms from non-pathogenic ones, and a considerable length of time and labor are required to complete these tests. Finally, although molecular testing methods, such as real-time polymerase chain reaction, have emerged as highly accurate and rapid diagnostic strategies for UTI (Lehmann et al., 2009, 2011), these tests are expensive, require advanced training and highly specialized equipment, and are not yet widely available outside of university settings.
Tests detecting significant bacteriuria need to be accurate and reliable, rapidly performed, and widely available. Because a test that possesses all of these characteristics has not yet been developed, clinical diagnosis of CAUTI is initially made based on clinical signs and symptoms of a host inflammatory response while microbiological tests of significant bacteruiria are pending. However, evidence suggests that the diagnosis of CAUTI based on clinical signs varies widely among clinicians and is often inaccurate when compared to published guidelines (Al-Qas Hanna, Sambirska, Iyer, Szpunar, & Fakih, 2013; Smithson, 2011; Trautner et al., 2013).
To monitor the catheterized patient for clinical evidence of CAUTI, clinicians assess indicators of localized and/or systemic inflammatory response (Perla, Peden, Goldmann, & Lloyd, 2009). Clinical practice guidelines identify several such indicators, including fever, suprapubic tenderness, flank tenderness, and delirium (Hooton et al., 2010; Horan et al., 2008). Unfortunately, standardized procedures to assess some of these indicators have not yet been described in the literature, and information about the consistency of some of these assessment findings from one clinician to another has yet to be reported.
The purpose of this paper is to describe the development of a tool to standardize the assessment of fever, suprapubic tenderness, flank tenderness, and delirium in hospitalized patients with short-term indwelling urinary catheters and to report preliminary data on the inter-rater reliability of the items in this tool. The findings noted here were obtained in conjunction with a pilot study to examine the validity of clinical manifestations of CAUTI.
Methods
Development of the CAUTI Assessment Profile
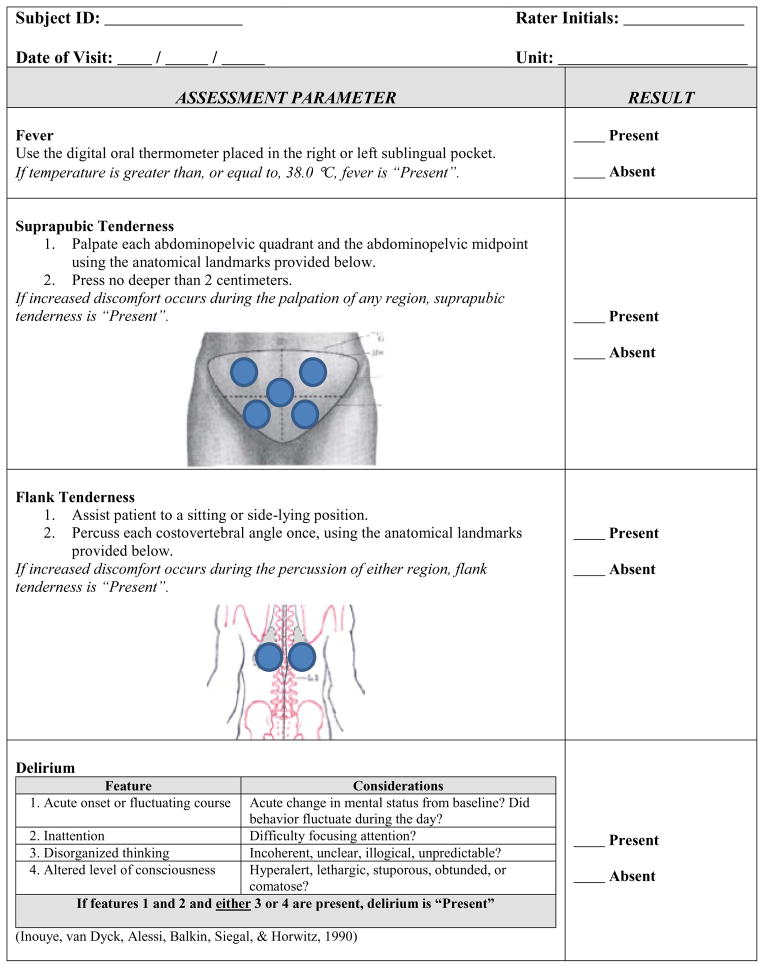
Although suprapubic tenderness, flank tenderness, and delirium are clinical signs and symptoms of CAUTI identified in clinical practice guidelines, a standardized method for assessment of these manifestations is lacking. Therefore, we developed the CAUTI Assessment Profile (CAP) to measure the presence or absence of fever, suprapubic tenderness, flank tenderness, and delirium (Figure 1). The CAP instrument contains definitions of each clinical sign and symptom, as well as diagrams, to aid in their consistent assessment. Definitions were developed after a thorough review of the literature with a goal of providing a tool that would be practical for use in research protocols as well as in clinical practice. After development, the CAP instrument was submitted to a panel of five experts in UTI and CAUTI diagnosis (3 physicians, 2 doctorally prepared nurses) for opinions about face validity. Three of the five content experts (1 physician and 2 doctorally prepared nurses) responded to the request for instrument review. All felt that the CAP was suitable for research purposes, appropriately parsimonious, and would make a useful contribution to the literature. The instrument was then submitted for academic purposes to a second panel of medical and nursing faculty (2 physicians, 4 doctorally prepared nurses) who were not CAUTI content experts. The faculty members on this second review panel were asked to provide feedback on whether or not the CAP was sufficiently aligned with the reviewed literature, as well as to evaluate the appropriateness of the selected data analysis plan given the level of data that would be collected using the instrument. All of these reviewers responded to these requests for feedback, and supported use of the CAP for data collection in this pilot study.
FIGURE 1.
CAUTI ASSESSMENT PROFILE (CAP) CASE REPORT FORM
Measures
To be consistent with evidence-based clinical practice guidelines, fever was defined as a core body temperature greater than, or equal to, 38 degrees Celsius (Hooton et al., 2010; Horan et al., 2008).
Suprapubic tenderness was defined as discomfort in the suprapubic region elicited during palpation of the lower abdomen, which is indicative of cystitis. The participant was asked to notify the rater of an increase in discomfort from the time period immediately prior to palpation when the area overlying the bladder was compressed. Participants who were unable to communicate verbally were similarly assessed for discomfort using the Behavioral Pain Scale, which measures the severity of discomfort through observation of nonverbal, or behavioral, indicators of pain when a potentially painful stimulus is applied (Gélinas, Puntillo, Joffe, & Barr, 2013; Li, Puntillo, & Miaskowski, 2008). Any increase in discomfort from the time immediately prior to palpation of the suprapubic region was indicative of suprapubic tenderness.
Flank tenderness was defined as discomfort in the flank regions elicited during percussion of the costovertebral angles, which is indicative of pyelonephritis. The participant was asked to notify the rater of an increase in discomfort from the time period immediately prior to percussion to when the areas overlying the bilateral costovertebral angles were percussed. Participants who were unable to communicate verbally were similarly assessed for tenderness using the Behavioral Pain Scale. Any increase in discomfort from the time immediately prior to costovertebral angle percussion was indicative of flank tenderness.
Infection is a common precipitating factor for delirium, particularly in the elderly (Inouye et al., 1990; Vasilevskis et al., 2011). Delirium was defined as an acute change in cognitive status resulting from an underlying medical, psychiatric, environmental, or multifactorial cause (Inouye et al., 1990). This manifestation of CAUTI has four indicators: acute onset with fluctuating course, inattention, disorganized thinking, and altered level of consciousness.
Reliability of the CAUTI Assessment Profile
After expert validation, the reliability of the CAP was examined using a cross-sectional design consisting of participants recruited from two settings. Both were community medical centers in the Midwest, one urban and one suburban, each with approximately 130 inpatient beds. Human subjects approval was obtained from the Institutional Review Boards at the author’s affiliated university and from the study setting before enrollment and data collection.
Potential participants were identified through concurrent medical record review based on the following criteria: 1) 18 years of age or older, 2) an indwelling urinary catheter placed during the current hospitalization, and 3) is not pregnant. Because this study was designed to test clinical manifestations of CAUTI in patients with a current indwelling urinary catheter, those who had the indwelling urinary catheter removed prior to the study visit were excluded from the study. Informed consent was obtained from all participants or, if unable to provide informed consent, from the participant’s health care proxy before participation in this study.
Data Collection Procedures
In addition to the principal investigator, two advanced practice nurses were trained in the use of the CAP for study data collection. All raters, including the principal investigator, were employed at the study setting as advanced practice nurses at the time of data collection. Each rater reviewed the CAP and practiced using the tool on healthy adults to assess fever, suprapubic tenderness, flank tenderness, and delirium together with the principal investigator. Raters were instructed to use only the procedures described in the CAP tool for study data collection. Discrepancies in technique were noted and discussed. Practice was repeated until each nurse achieved 100% agreement with the principal investigator, which was typically achieved in one or two practice attempts.
For resource and feasibility reasons, convenience sampling was used to recruit a target sample size of 30 participants for this study. To offset some of the impact this small sample size would have on standard error of the reliability estimates, three raters, rather than two, independently collected data using the CAP tool from each study participants. Using three raters instead of two has been shown to reduce agreement variance, thus reducing the likelihood of a type II error, in inter-rater reliability studies with a small sample size (O’Leary, Lund, Ytre-Hauge, Holm, Naess, Dalland, et al, 2014; Sadatsafavi, Najafzadeh, Lynd, & Marra, 2008). The second and third rater began their assessment within 5 to 10 minutes of the previous assessment in order to reduce differences in assessment that were based on changes in clinical condition rather than variation in assessment. Participants were asked to refrain from drinking or eating during the study period to minimize fluctuations in body temperature that would not be related to CAUTI. Participants were positioned in a hospital bed with the head elevated to a 30-degree angle (or higher if needed for clinical reasons) for assessment of fever, suprapubic tenderness, and delirium. Participants were assisted to a side-lying position with head of bed no higher than 30 degrees for assessment of flank tenderness as directed by the CAP. These positions were chosen to standardize conditions between raters.
Fever
Techniques for measuring body temperature are well established in the literature. Core body temperature was measured using a digital oral thermometer (SureTemp Plus Model 692, WelchAllyn). The thermometer was inserted into the participant’s left or right sublingual pocket and maintained in this position until an audible signal from the thermometer was heard, indicating that the temperature data was available. The thermometer was calibrated prior to each use according to the manufacturer’s instructions.
Suprapubic Tenderness
To assess suprapubic tenderness, the rater exposed the participant’s skin between the umbilicus and the mons pubis, then used the pads of the first, second, and third fingers of the dominant hand to palpate the lower abdomen. Palpation was no deeper than two centimeters. The roughly ovoid shape bounded by the umbilicus superiorly, the superior aspect of the mons pubis inferiorly, and the iliac crests bilaterally was identified. The abdominal midline and an imaginary line drawn between the two anterior superior iliac spines were used to divide this region into four quadrants. Each quadrant was palpated once, as well as the point of intersection formed by the two imaginary lines. This technique was chosen because it ensured the use of physiological landmarks to identify the area overlying the bladder that would have been identifiable on adults with normal or near-normal anatomical features (abnormal anatomical features might have included abdominal hernia, evidence of surgical manipulation of abdominopelvic organs [e.g. abdominal hysterectomy, ileal-conduit, colostomy], or morbid/super-morbid obesity), and it provided a consistent depth of compression to prevent the potential effect of false positive suprapubic tenderness due to blunt force instead of an inflamed bladder.
Flank Tenderness
Unless medically contraindicated (e.g. spinal surgery) or deferred due to participant refusal, participants were assisted to a side-lying position to facilitate percussion of the costovertebral angles. Since the act of repositioning may contribute to discomfort in this region that is unrelated to the urinary tract (e.g. back muscle spasms), verbally communicative participants were supported in a self-reported comfortable position while site percussion occurred. Participants who were unable to self-report a comfortable position were assisted to a side-lying position that supported proper alignment of hips and shoulders using electronic bed controls and padding of knee joints with pillows. Participants who were unable to assume this position, but who otherwise met inclusion criteria for the study, were not excluded from the study since data for the other variables (fever, suprapubic tenderness, or delirium) could still have been collected.
To assess for flank tenderness, the rater percussed the bilateral costovertebral angles, which were identified as the triangular regions found at the mid-back and bound superiolaterally by the 12th ribs, medially by the vertebral column, and inferiorly by the posterior iliac crests. This technique was chosen because it ensured the use of physiological landmarks to identify the area overlying the kidneys that would have been identifiable on adults with normal or near-normal anatomical features.
Delirium
To assess for delirium, raters used the Confusion Assessment Method according to a modified procedure described by Inouye and colleagues (1990), in which the Six-Item Screener was used during the cognitive status interview instead of the Mini Mental Status Examination. This modification was made from the original protocol because there is evidence that the Six-Item Screener performs as well as the Mini Mental Status Examination to detect global cognitive impairment (Callahan et al., 2002; Carpenter, DesPain, Keeling, Shah, & Rothenberger, 2011), and it requires relatively less time and training to correctly administer than other cognitive impairment instruments. Data regarding acute onset and fluctuating course were collected from the participant’s staff nurse and/or family caregiver. Data regarding inattention, disorganized thinking, and altered level of consciousness were collected by direct observation. Delirium was categorized as “Present” if acute onset with fluctuating course, inattention, and either disorganized thinking or altered level of consciousness were present. If these criteria were not met, delirium was categorized as “Absent”.
Data Analysis
This study examined the inter-rater reliability of each item on the CAP by comparing the three independent assessments of each participant using the generalized (Fleiss’) Kappa coefficient (O’Leary et al., 2014; Sadatsafavi, Najafzadeh, Lynd, & Marra, 2008). The generalized Kappa coefficient is used to calculate agreement of nominal data (i.e., data without a natural order) between more than two raters. This statistic has two major advantages over other tests of inter-rater agreement. First, it allows for testing of agreement between two or more raters, as opposed to Cohen’s Kappa coefficient, which only allows for two raters. Second, the Kappa statistic takes into account the opportunity for agreement between raters by chance alone. Because considerable controversy remains about the meaning of various Kappa coefficient ranges, a 95% confidence interval was determined for each Kappa coefficient to identify the statistical significance of these results. Descriptive and reliability analyses were performed using Microsoft Excel (2010).
Results
Eighty patients were approached to arrive at the final sample size of thirty participants, all of whom completed study procedures. The mean age of participants was 74.3 years (SD ± 11.99). They were predominant white (73.3%), with African-Americans representing the remaining 26.7% of the sample. Half of participants were female, and half were male. Frequency of assessment findings, inter-rater reliability estimates, and 95% confidence intervals for these estimates are listed in Table 1. It is important to note that only twelve of the thirty participants permitted raters to assess for flank tenderness due to difficulty moving to a side lying position.
TABLE 1.
FREQUENCY AND INTER-RATER RELIABILITY OF CAUTI SIGNS AND SYMPTOMS
| CAUTI Sign or Symptom | Frequency/# Participants (%) | Generalized Kappa Coefficient | 95% Confidence Limits |
|---|---|---|---|
| Fever | 5/30 (16.7) | 1.00 | 0.793 – 1.207 |
| Suprapubic Tenderness | 10/30 (33.3) | 0.58 | 0.379 – 0.792 |
| Flank Tenderness | 5/12 (41.6) | 0.29 | 0 – 0.617 |
| Delirium | 6/30 (20) | 0.39 | 0.185 – 0.598 |
Discussion
In this pilot study, the inter-rater reliability of a newly developed tool to guide the assessment of CAUTI clinical signs and symptoms, the CAP, was examined. Each item on the CAP represents an assessment finding that has previously been identified in clinical practice guidelines as indicative of CAUTI. Their associations with CAUTI are biologically plausible, although their diagnostic validity has not yet been reported in the literature. Three of these clinical manifestations – fever, suprapubic tenderness, and delirium – had acceptable and statistically significant consistency between three nurse raters, while flank tenderness did not.
Fever had perfect agreement, which was not necessarily surprising given the use of standardized thermometry equipment between raters and the absolute cut-off value greater than 38° Celsius to detect the presence of fever. In contrast, assessment of suprapubic tenderness and flank tenderness required the use of subjective judgment and thus had greater variability between raters. Furthermore, the perception and interpretation of pain can vary widely over brief periods of time, which may have contributed to participants providing inconsistent reports of pain between raters. Since many participants declined to be repositioned for the assessment of flank tenderness, the number of participants assessed for flank tenderness was considerably lower than the number of participants assessed for the other signs and symptoms. Therefore, the reliability estimate for flank tenderness had inherently greater variability than the other assessment parameters, which may be the reason for it not demonstrating statistically significant reliability. The reliability estimates for delirium compare favorably with other studies that have examined inter-rater agreement on delirium assessment (Hestermann et al., 2009; Inouye et al., 1990; Radtke et al., 2010; Vasilevskis et al., 2011; Wang et al., 2013).
This study had several important limitations. First, the sample size was too small to draw conclusive results about the study aim. Given the wide 95% confidence intervals, as well as the highly variable nature of the clinical signs and symptoms assessed, replication of this study using a larger sample size would be a necessary and appropriate next step to clarify the inter-rater reliability of the CAP instrument. Second, since assessment findings were not compared to clinical laboratory data (e.g. urine culture results), there can be no conclusions drawn from this study about the diagnostic validity of the CAP instrument. While this was not the aim of the current study, the overall utility of the CAP instrument for research and clinical practice can only be determined after rigorous study of both its reliability between several types of raters and its validity compared to microbiologic and molecular characteristics of uropathogens. Therefore, future studies that are designed to examine the diagnostic validity of the CAP tool would need to include these types of comparisons to calculate validity estimates such as sensitivity, specificity, positive predictive value, and negative predictive value of the CAP. Third, the presence of abnormal abdominopelvic features (e.g. hernia, oophorectomy, colostomy, morbid/super-morbid obesity) may have influenced the location and/or depth of palpation points between raters, thereby potentially affecting the inter-rater reliability estimate of suprapubic tenderness. Data regarding abdominal anatomy, body mass index, and abdominal circumference were not collected in this study. Future research that explores the psychometric properties of the CAP instrument would benefit from such measurements so that reliability and validity estimates can be calculated while statistically controlling for these variables. Alternatively, eligibility criteria could be modified to exclude potential participants with abnormal abdominopelvic anatomy or morbid obesity/super-obesity.
Despite these issues, this was the first study to examine the inter-rater reliability of fever, suprapubic tenderness, flank tenderness, and delirium among hospitalized adults with a short-term indwelling urinary catheter using standardized assessment procedures. This study provides preliminary evidence that advanced practice nurses can use the CAP tool to consistently identify fever, suprapubic tenderness, and delirium in this population. Further research is necessary to determine if the CAP can be used with similar consistency among staff nurses.
Implications for Using the CAUTI Assessment Profile in Practice
Nurses and other clinicians who are responsible for monitoring patients with an indwelling urinary catheter need to follow standardized procedures to assess the signs and symptoms of CAUTI. Although all of the nurse raters in this study had previous experience caring for patients with indwelling urinary catheter, they practiced in diverse acute care settings, including medical-surgical, critical care, and the emergency department. Training sessions, data collection forms with instructions and diagrams, and consistency checks after training were required to achieve the level of agreement found in this study. In this pilot study, each rater’s assessment was completed in less than 5 minutes, with the majority of the time used to assess delirium.
A deliberate approach to monitoring for evidence of CAUTI is not common among hospital staff nurses. Instead, these signs and symptoms of CAUTI are assessed along with other routine assessment parameters, and their meaning may be ascribed to another clinical condition such as gastrointestinal discomfort, flatus, chronic back pain, dementia, or another infection source. Including the CAP as part of the standardized assessment for hospitalized patients with an indwelling urinary catheter may improve the systematic identification of CAUTI signs and symptoms.
Contributor Information
Tom J. Blodgett, Email: tom.blodgett@valpo.edu, Valparaiso University College of Nursing and Health Professions, 836 LaPorte Avenue, Valparaiso, Indiana, 46383.
Sue E. Gardner, Email: sue-gardner@uiowa.edu, University of Iowa College of Nursing, 150 Newton Road, Iowa City, Iowa, 52242.
Nicole P. Blodgett, Email: nicole.blodgett@purduecal.edu, Purdue University Calumet College of Nursing, Hammond, Indiana, 46320.
Lisa V. Peterson, Email: lisa.peterson@franciscanalliance.org, Franciscan St. Margaret Health, 5454 Hohman Avenue, Hammond, Indiana, 46320.
Melissa Pietraszak, Email: melissa.pietraszak@franciscanalliance.org, Franciscan St. Margaret Health, 5454 Hohman Avenue, Hammond, Indiana, 46320.
References
- Al-Qas Hanna F, Sambirska O, Iyer S, Szpunar S, Fakih MG. Clinician practice and the National Healthcare Safety Network definition for the diagnosis of catheter-associated urinary tract infection. American Journal of Infection Control. 2013 doi: 10.1016/j.ajic.2013.05.024. [DOI] [PubMed] [Google Scholar]
- Cairns S, Reilly J, Stewart S, Tolson D, Godwin J, Knight P. The prevalence of health care-associated infection in older people in acute care hospitals. Infection Control and Hospital Epidemiology: The Official Journal of the Society of Hospital Epidemiologists of America. 2011;32(8):763–767. doi: 10.1086/660871. [DOI] [PubMed] [Google Scholar]
- Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care. 2002;40(9):771–781. doi: 10.1097/01.MLR.0000024610.33213.C8. [DOI] [PubMed] [Google Scholar]
- Carpenter CR, DesPain B, Keeling TN, Shah M, Rothenberger M. The Six-Item Screener and AD8 for the detection of cognitive impairment in geriatric emergency department patients. Annals of Emergency Medicine. 2011;57(6):653–661. doi: 10.1016/j.annemergmed.2010.06.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dellimore KH, Helyer AR, Franklin SE. A scoping review of important urinary catheter induced complications. Journal of Materials Science: Materials in Medicine. 2013;24(8):1825–1835. doi: 10.1007/s10856-013-4953-y. [DOI] [PubMed] [Google Scholar]
- Gélinas C, Puntillo K, Joffe A, Barr J. A Validated Approach to Evaluating Psychometric Properties of Pain Assessment Tools for Use in Nonverbal Critically Ill Adults. Seminars in Respiratory and Critical Care Medicine. 2013;34(02):153–168. doi: 10.1055/s-0033-1342970. [DOI] [PubMed] [Google Scholar]
- Gokula RRM, Hickner JA, Smith MA. Inappropriate use of urinary catheters in elderly patients at a midwestern community teaching hospital. American Journal of Infection Control. 2004;32(4):196–199. doi: 10.1016/j.ajic.2003.08.007. [DOI] [PubMed] [Google Scholar]
- Hestermann U, Backenstrass M, Gekle I, Hack M, Mundt C, Oster P, Thomas C. Validation of a German version of the Confusion Assessment Method for delirium detection in a sample of acute geriatric patients with a high prevalence of dementia. Psychopathology. 2009;42(4):270–276. doi: 10.1159/000224151. [DOI] [PubMed] [Google Scholar]
- Hollingsworth JM, Rogers MAM, Krein SL, Hickner A, Kuhn L, Cheng A, Saint S. Determining the Noninfectious Complications of Indwelling Urethral Catheters: A Systematic Review and Meta-analysis. Annals of Internal Medicine. 2013;159(6):401–410. doi: 10.7326/0003-4819-159-6-201309170-00006. [DOI] [PubMed] [Google Scholar]
- Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC Infectious Diseases Society of America. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2010;50(5):625–663. doi: 10.1086/650482. [DOI] [PubMed] [Google Scholar]
- Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care–associated infection and criteria for specific types of infections in the acute care setting. American Journal of Infection Control. 2008;36(5):309–332. doi: 10.1016/j.ajic.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Annals of Internal Medicine. 1990;113(12):941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- Janzen J, Buurman BM, Spanjaard L, de Reijke TM, Goossens A, Geerlings SE. Reduction of unnecessary use of indwelling urinary catheters. BMJ Quality & Safety. 2013 doi: 10.1136/bmjqs-2013-001908. [DOI] [PubMed] [Google Scholar]
- Kang CI, Song JH, Chung DR, Peck KR, Ko KS, Yeom JS Korean Network for Study of Infectious Diseases (KONSID) Risk factors and pathogenic significance of severe sepsis and septic shock in 2286 patients with gram-negative bacteremia. The Journal of Infection. 2011;62(1):26–33. doi: 10.1016/j.jinf.2010.10.010. [DOI] [PubMed] [Google Scholar]
- Kayalp D, Dogan K, Ceylan G, Senes M, Yucel D. Can routine automated urinalysis reduce culture requests? Clinical Biochemistry. 2013;46(13–14):1285–1289. doi: 10.1016/j.clinbiochem.2013.06.015. [DOI] [PubMed] [Google Scholar]
- Kennedy EH, Greene MT, Saint S. Estimating hospital costs of catheter-associated urinary tract infection. Journal of Hospital Medicine: An Official Publication of the Society of Hospital Medicine. 2013;8(9):519–522. doi: 10.1002/jhm.2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kizilbash QF, Petersen NJ, Chen GJ, Naik AD, Trautner BW. Bacteremia and Mortality with Urinary Catheter-Associated Bacteriuria. Infection Control and Hospital Epidemiology: The Official Journal of the Society of Hospital Epidemiologists of America. 2013;34(11):1153–1159. doi: 10.1086/673456. [DOI] [PubMed] [Google Scholar]
- Ko MC, Liu CK, Woung LC, Lee WK, Jeng HS, Lu SH, Li CY. Species and antimicrobial resistance of uropathogens isolated from patients with urinary catheter. The Tohoku Journal of Experimental Medicine. 2008;214(4):311–319. doi: 10.1620/tjem.214.311. [DOI] [PubMed] [Google Scholar]
- Kupelian AS, Horsley H, Khasriya R, Amussah RT, Badiani R, Courtney AM, Malone-Lee J. Discrediting microscopic pyuria and leucocyte esterase as diagnostic surrogates for infection in patients with lower urinary tract symptoms: results from a clinical and laboratory evaluation: Pyuria as a surrogate marker of UTI in patients with LUTS. BJU International. 2013;112(2):231–238. doi: 10.1111/j.1464-410X.2012.11694.x. [DOI] [PubMed] [Google Scholar]
- Kurtzman ET, Buerhaus PI. New Medicare payment rules: danger or opportunity for nursing? The American Journal of Nursing. 2008;108(6):30–35. doi: 10.1097/01.NAJ.0000324370.71532.b7. [DOI] [PubMed] [Google Scholar]
- Lehmann LE, Hauser S, Malinka T, Klaschik S, Stüber F, Book M. Real-time polymerase chain-reaction detection of pathogens is feasible to supplement the diagnostic sequence for urinary tract infections: PCR DETECTION OF PATHOGENS FOR DIAGNOSING UTI. BJU International. 2009;106(1):114–120. doi: 10.1111/j.1464-410X.2009.09017.x. [DOI] [PubMed] [Google Scholar]
- Lehmann LE, Hauser S, Malinka T, Klaschik S, Weber SU, Schewe JC, Book M. Rapid Qualitative Urinary Tract Infection Pathogen Identification by SeptiFast® Real-Time PCR. PLoS ONE. 2011;6(2):e17146. doi: 10.1371/journal.pone.0017146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leuck AM, Wright D, Ellingson L, Kraemer L, Kuskowski MA, Johnson JR. Complications of Foley catheters--is infection the greatest risk? The Journal of Urology. 2012;187(5):1662–1666. doi: 10.1016/j.juro.2011.12.113. [DOI] [PubMed] [Google Scholar]
- Li D, Puntillo K, Miaskowski C. A review of objective pain measures for use with critical care adult patients unable to self-report. The Journal of Pain: Official Journal of the American Pain Society. 2008;9(1):2–10. doi: 10.1016/j.jpain.2007.08.009. [DOI] [PubMed] [Google Scholar]
- Milan PB, Ivan IM. Catheter-associated and nosocomial urinary tract infections: antibiotic resistance and influence on commonly used antimicrobial therapy. International Urology and Nephrology. 2009;41(3):461–464. doi: 10.1007/s11255-008-9468-y. [DOI] [PubMed] [Google Scholar]
- O’Leary S, Lund M, Ytre-Hauge TJ, Holm SR, Naess K, Dalland LN, McPhail SM. Pitfalls in the use of kappa when interpreting agreement between multiple raters in reliability studies. Physiotherapy. 2014;100(1):27–35. doi: 10.1016/j.physio.2013.08.002. [DOI] [PubMed] [Google Scholar]
- Perla RJ, Peden CJ, Goldmann D, Lloyd R. Health care-associated infection reporting: the need for ongoing reliability and validity assessment. American Journal of Infection Control. 2009;37(8):615–618. doi: 10.1016/j.ajic.2009.03.003. [DOI] [PubMed] [Google Scholar]
- Radtke FM, Franck M, Schust S, Boehme L, Pascher A, Bail HJ, Spies CD. Acomparison of three scores to screen for delirium on the surgical ward. World Journal of Surgery. 2010;34(3):487–494. doi: 10.1007/s00268-009-0376-9. [DOI] [PubMed] [Google Scholar]
- Sadatsafavi M, Najafzadeh M, Lynd L, Marra C. Reliability studies of diagnostic tests are not using enough observers for robust estimation of interobserver agreement: a simulation study. Journal of Clinical Epidemiology. 2008;61(7):722–727. doi: 10.1016/j.jclinepi.2007.10.023. [DOI] [PubMed] [Google Scholar]
- Saint S. Clinical and economic consequences of nosocomial catheter-related bacteriuria. American Journal of Infection Control. 2000;28(1):68–75. doi: 10.1016/s0196-6553(00)90015-4. [DOI] [PubMed] [Google Scholar]
- Smithson A. Are health care–associated urinary tract infections properly defined? The American Journal of Emergency Medicine. 2011;29(4):467–468. doi: 10.1016/j.ajem.2010.12.034. [DOI] [PubMed] [Google Scholar]
- Tambyah PA, Knasinski V, Maki DG. The direct costs of nosocomial catheter-associated urinary tract infection in the era of managed care. Infection Control and Hospital Epidemiology: The Official Journal of the Society of Hospital Epidemiologists of America. 2002;23(1):27–31. doi: 10.1086/501964. [DOI] [PubMed] [Google Scholar]
- Tiwari MM, Charlton ME, Anderson JR, Hermsen ED, Rupp ME. Inappropriate use of urinary catheters: a prospective observational study. American Journal of Infection Control. 2012;40(1):51–54. doi: 10.1016/j.ajic.2011.03.032. [DOI] [PubMed] [Google Scholar]
- Trautner BW, Bhimani RD, Amspoker AB, Hysong SJ, Garza A, Kelly PA, Naik AD. Development and validation of an algorithm to recalibrate mental models and reduce diagnostic errors associated with catheter-associated bacteriuria. BMC Medical Informatics and Decision Making. 2013;13:48. doi: 10.1186/1472-6947-13-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasilevskis EE, Morandi A, Boehm L, Pandharipande PP, Girard TD, Jackson JC, Wesley Ely E. Delirium and Sedation Recognition Using Validated Instruments: Reliability of Bedside Intensive Care Unit Nursing Assessments from 2007 to 2010. Journal of the American Geriatrics Society. 2011;59:S249–S255. doi: 10.1111/j.1532-5415.2011.03673.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Wu Y, Yue P, Ely EW, Huang J, Yang X, Liu Y. Delirium assessment using Confusion Assessment Method for the Intensive Care Unit in Chinese critically ill patients. Journal of Critical Care. 2013;28(3):223–229. doi: 10.1016/j.jcrc.2012.10.004. [DOI] [PubMed] [Google Scholar]
- Warren JW. Catheter-associated urinary tract infections. International Journal of Antimicrobial Agents. 2001;17(4):299–303. doi: 10.1016/s0924-8579(00)00359-9. [DOI] [PubMed] [Google Scholar]
- Weber DJ, Sickbert-Bennett EE, Gould CV, Brown VM, Huslage K, Rutala WA. Incidence of catheter-associated and non-catheter-associated urinary tract infections in a healthcare system. Infection Control and Hospital Epidemiology: The Official Journal of the Society of Hospital Epidemiologists of America. 2011;32(8):822–823. doi: 10.1086/661107. [DOI] [PubMed] [Google Scholar]
- Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, Bates DW. Health Care-Associated Infections: A Meta-analysis of Costs and Financial Impact on the US Health Care System. JAMA Internal Medicine. 2013 doi: 10.1001/jamainternmed.2013.9763. [DOI] [PubMed] [Google Scholar]