Abstract
Purpose
To investigate the risk factors for initial central scotoma (ICS) compared with initial peripheral scotoma (IPS) in normal-tension glaucoma (NTG).
Methods
Fifty-six NTG patients (56 eyes) with an ICS and 103 NTG patients (103 eyes) with an IPS were included. Retrospectively, the differences were assessed between the two groups for baseline characteristics, ocular factors, systemic factors, and lifestyle factors. Also, the mean deviation of visual field was compared between the two groups.
Results
Patients from both ICS and IPS groups were of similar age, gender, family history of glaucoma, and follow-up periods. Frequency of disc hemorrhage was significantly higher among patients with ICS than in patients with IPS. Moreover, systemic risk factors such as hypotension, migraine, Raynaud's phenomenon, and snoring were more prevalent in the ICS group than in the IPS group. There were no statistical differences in lifestyle risk factors such as smoking or body mass index. Pattern standard deviation was significantly greater in the ICS group than in the IPS group, but the mean deviation was similar between the two groups.
Conclusions
NTG Patients with ICS and IPS have different profiles of risk factors and clinical characteristics. This suggests that the pattern of initial visual field loss may be useful to identify patients at higher risk of central field loss.
Keywords: Low tension glaucoma, Risk factors, Scotoma, Visual fields
Glaucoma affects more than 66 million patients and is the second leading cause of visual loss worldwide [1,2]. Because glaucoma is usually asymptomatic until the end stage, early diagnosis and treatment is essential to prevent the progression of visual loss.
Open-angle glaucoma (OAG) can be classified, according to the intraocular pressure (IOP), into normal-tension glaucoma (NTG) and high-tension glaucoma [3]. Previous studies in the Asian population have revealed that normal-tension glaucoma is more prevalent than high-tension glaucoma. In the Tajimi study, 92% of the patients with primary open-angle glaucoma (POAG) were classified as NTG, with IOP lower than 21 mmHg [4]. Similarly, the number of NTG patients was 4-fold greater than those with high-tension glaucoma in a study of Japanese Americans [5]. Also, in the Namil study [6], 77% of POAG cases had an IOP of lower than 21 mmHg.
The best-known risk factor for glaucoma is increased IOP; it has been established that IOP is a part of the pathogenic process of NTG [7]. This pressure theory, however, cannot sufficiently explain how NTG contributes to loss of vision. Alternatively, vascular dysfunction and ischemia have been considered as more important factors in the progression of NTG [8,9,10,11]. Non-IOP-related, potential cardiovascular dysregulation factors, such as systemic hypertension, systemic hypotension, nocturnal hypotension, migraine, and cardiac arrhythmia, are implicated as well. Mojon et al. [12] suggested that patients with sleep apnea syndrome constitute a population at high risk for glaucoma.
In addition to these systemic risk factors, lifestyle factors, represented by smoking and body mass index (BMI, calculated as weight in kilograms divided by height in meters squared), have been implicated in the progression of glaucomatous visual field defect (VFD). Whether this relationship is causal or coincident remains to be seen in many other studies. In the Blue Mountain Eye Study, smokers were found to have IOP that is slightly elevated in comparison to non-smokers [13]. However, in another study on the relationship between smoking and glaucoma, POAG was associated with a higher frequency of heavy smoking [14]. Only a few studies have directly investigated the potential relationship between obesity and glaucoma, and they suggest that there may be an inverse association between BMI and POAG [15].
Patterns of glaucomatous VFD vary among previous studies. Among these patterns, paracentral VFD is the most concerning because of its proximity to fixation. Also, previous reports indicate that the patients with glaucomatous VFDs within 5 degrees have greater risk factor of visual loss [16]. Central VFD affects the quality of life, and the progression of glaucoma is associated with significant quality of life losses such as difficulties in walking on stairs, driving or engaging in sports activities [17].
In this study, because of this clinical relevance, we focused on clarifying which aspects of patients' medical history and clinical examination are more commonly associated with a central versus peripheral VFD. Previous studies suggest that the gene level pathogenesis of the OAG is related with early loss of central VF [18,19]. Another study compared the risk factors between initial parafoveal and peripheral scotomas in glaucoma [20], but they did not investigate the risk factors related to lifestyle among the patients. In this study, we investigated the risk factors for initial central scotoma (ICS) and initial peripheral scotoma (IPS) in normal-tension glaucoma, and this may be useful in understanding the pathogenesis of ICS and IPS.
Materials and Methods
Study design and patients
A retrospective review was performed for patients with normal-tension glaucoma who visited the Konkuk University Hospital from January 2008 to October 2011. We included the treatment-naïve patients with first diagnosis of normal-tension glaucoma, who were followed for more than 3 months. Any patients with previous history of intraocular surgery or any systemic or ocular medication that might affect IOP were excluded. This study was performed in accordance with the principles of the Declaration of Helsinki, and institutional review board approval was not required for this retrospective study. NTG was diagnosed on the following criteria: glaucomatous optic neuropathy and reproducible VFDs determined by a Humphrey Field Analyzer, with the central 24-2 threshold test using SITA-standard test strategy; IOP lower than 21 mmHg measured by Goldmann applanation tonometry without any medication; and, normal open angle on gonioscopy. Optic disc was observed by direct ophthalmoscopy, stereoscopic observation with a biomicroscope, and fundus photography.
Visual field defects classification
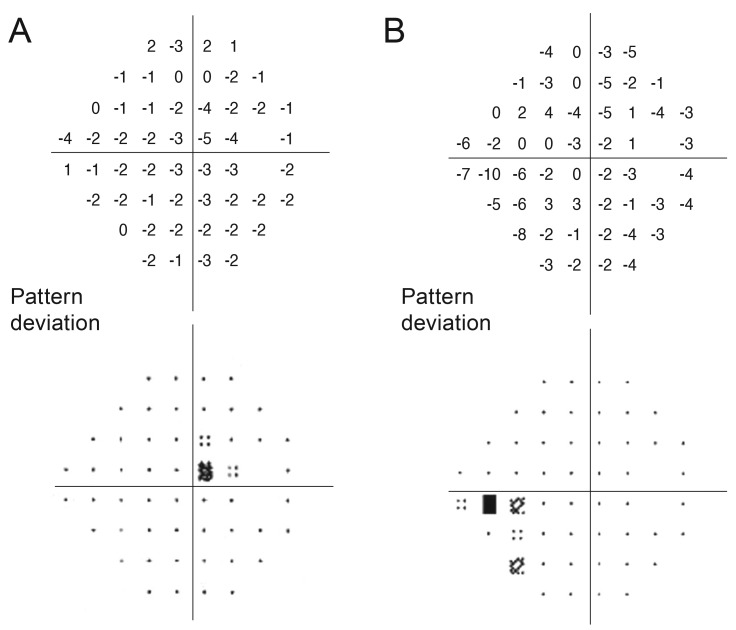
Visual field (VF) test was performed on at least two consecutive examinations. Considering the learning effect of the VF test, the results of the first test were excluded from the analysis. Of all the VF data, we excluded the unreliable VF results (fixation loss >20%, false positive and false negative >15%). The VFDs were classified into ICS and IPS by the following criteria. A VFD was defined as ICS in the presence of more than three adjacent VFD points at P <5% within the central 10 degrees, with at least one point at P <1% lying within the central 10 degrees, and without any involvement outside the central 10 degrees (Fig. 1A). Conversely, a VFD was defined as IPS if there were more than three adjacent VFD points at P <5% in the periphery outside of the central 10 degrees, with at least one point at P <1% in the periphery outside of the central 10 degrees, and without any involvement within the central 10 degrees (Fig. 1B). Only eyes with isolated ICS or IPS were included in this study.
Fig. 1. Visual field defect pattern on the Humphrey 24-2 standard pattern deviation plot. (A) Representative case of initial central scotoma with mean deviation -0.30 dB and pattern standard deviation 1.32 dB. (B) Representative case of initial peripheral scotoma with mean deviation -5.41 dB and pattern standard deviation 2.97 dB.
Clinical characteristics
For each patient, we recorded the baseline factors such as age, gender, and family history of glaucoma in first-degree relatives at the initial visit. The results of ocular examination and tests, such as spherical equivalent, central corneal thickness (CCT), and disc hemorrhage (DH) detection and maximum untreated IOP during follow-up period, were also obtained. At the initial visit, the questionnaire survey was reviewed for cardiovascular dysregulation factors, such as hypotension, migraine, Raynaud's phenomenon, cardiac arrhythmia, and hypertension, as well as for other systemic factors such as snoring and diabetes mellitus. The questionnaire also provided data regarding lifestyle risk factors such as smoking and body mass index. These baseline, ocular, systemic, and lifestyle factors of the ICS group were compared with those of the IPS group. Also, mean deviation (MD) and pattern standard deviation (PSD) of VF test were recorded and compared between the two groups.
Statistical analysis
Statistical analysis was performed using SPSS ver.17.0 (SPSS Inc., Chicago, IL, USA). All values are presented as mean ± standard deviation and percentage. The data were analyzed by student t-test and Fisher exact test between the ICS and IPS groups. A p-value of less than 0.05 was considered to be statistically significant.
Results
Baseline patient characteristics are shown in Table 1. A total of 159 eyes of 159 patients (85 males and 74 females) with NTG were analyzed. The mean age was 47.06 ± 12.77 years. According to the VFD classification, 56 patients (56 eyes) were assigned to the ICS group and 103 patients (103 eyes) to the IPS group. There were no significant differences between these two groups with regards to age (p = 0.297), gender (p = 0.983), family history of glaucoma (p = 0.400), and follow-up period (p = 0.059).
Table 1. Baseline characteristics of patients.
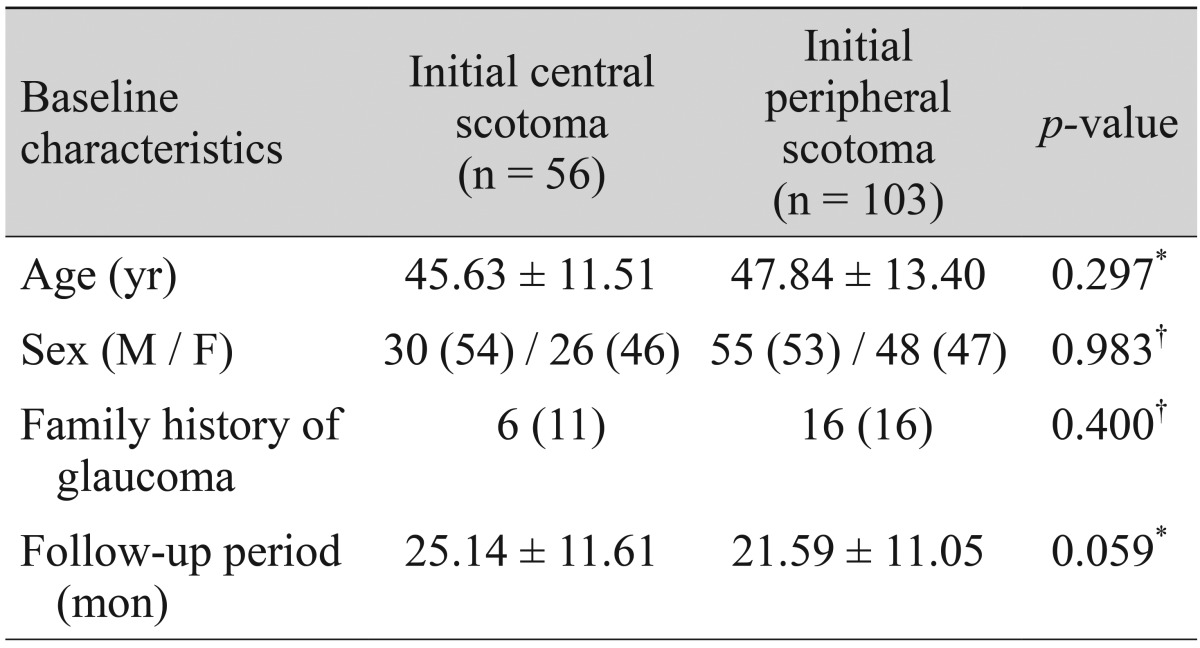
Values are presented as mean ± SD or n (%).
*Student t-test; †Fisher exact test.
Comparison of ocular factors between the initial central scotoma and initial peripheral scotoma groups
Across the two groups, no significant differences existed in spherical equivalent refractive error (p = 0.483), CCT (p = 0.669) or maximum untreated IOP (p = 0.668). DH detection was the only ocular factor that showed significant difference (p < 0.001), and it was more prevalent among patients in the ICS group (36%) than those in the IPS group (6%) (Table 2).
Table 2. Ocular factors for the visual field defect groups.
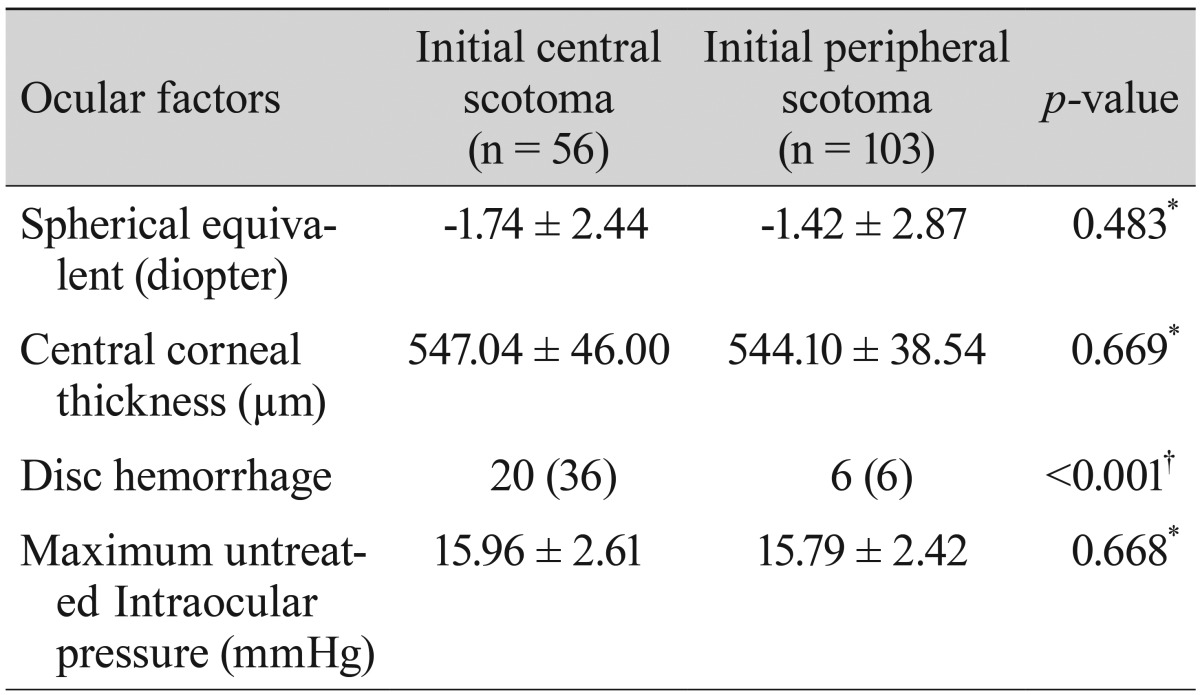
Values are presented as mean ± SD or n (%).
*Student t-test; †Fisher exact test.
Comparison of systemic factors between the initial central scotoma and initial peripheral scotoma groups
The ICS group was found to have a significantly higher prevalence of hypotension, migraine, Raynaud's phenomenon, and snoring than the IPS group (p < 0.001, p = 0.003, p = 0.001, p = 0.001, respectively). No significant differences in the prevalence of cardiac arrhythmia, hypertension, or diabetes mellitus existed between the groups (all p > 0.05) (Table 3).
Table 3. Systemic factors for the visual field defect groups.
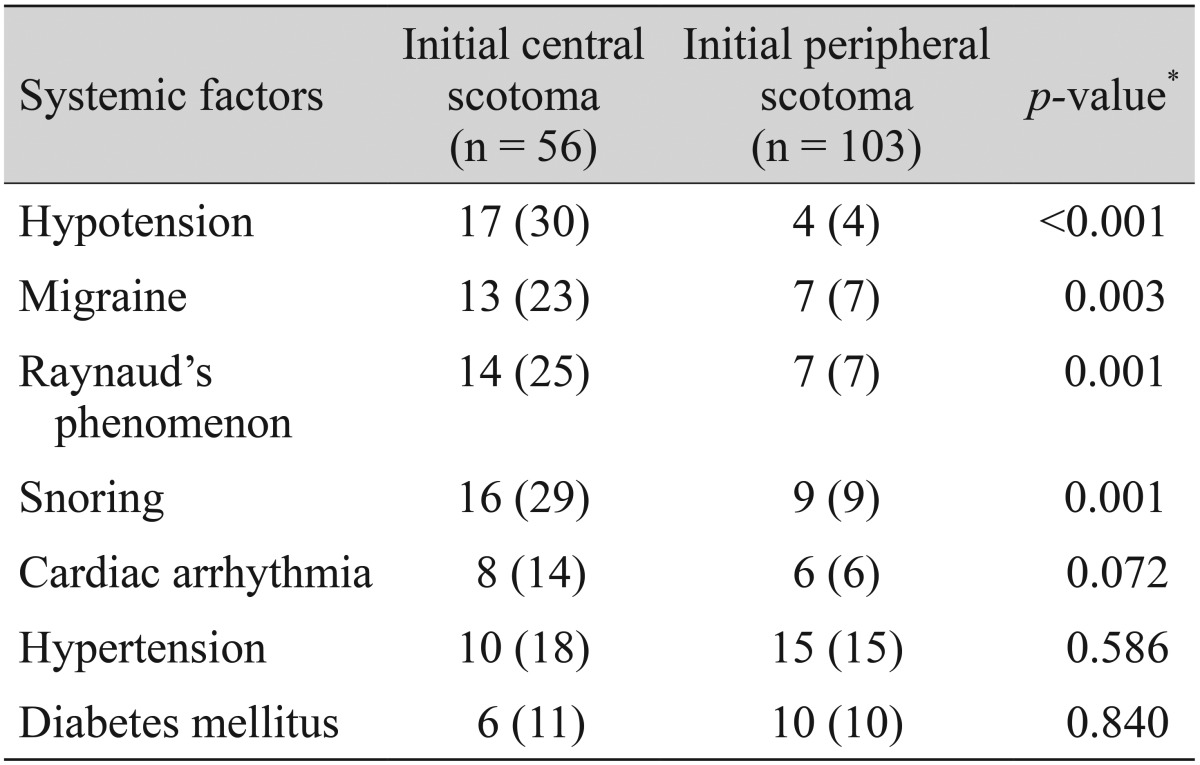
Values are presented as n (%).
*Fisher exact test.
Comparison of lifestyle risk factors between the initial central scotoma and initial peripheral scotoma groups
The percentage of smokers in the IPS group was slightly higher than that of the smokers in the ICS group, but the difference was not statistically significant (p = 0.413). Moreover, there were no statistical differences in BMI (ICS, 23.41 ± 3.72; IPS, 23.03 ± 2.68; respectively, p = 0.466) (Table 4).
Table 4. Lifestyle factors for the visual field defect groups.
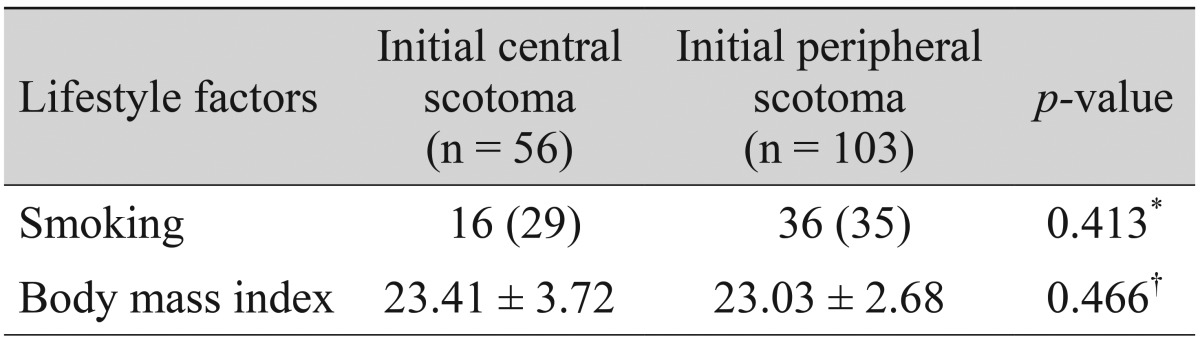
Values are presented as mean ± SD or n (%).
*Fisher exact test; †Student t-test.
Comparison of perimetric parameters between the initial central scotoma and initial peripheral scotoma groups
PSD was significantly lower in the ICS group than in the IPS group (p = 0.026). MD was not significantly different between the groups (p = 0.074) (Table 5).
Table 5. Visual field parameters for the visual field defect groups.
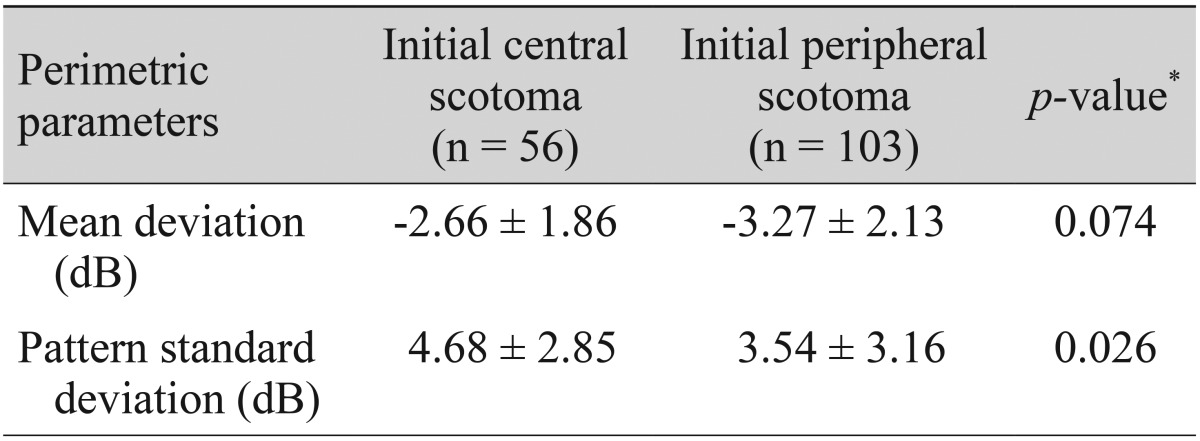
*Student t-test.
Discussion
Patients with glaucomatous central VF loss may be at greater risk of losing visual acuity [16]. Also, central and peripheral VF loss cause different problems for performing daily life activities [21,22].
Paracentral VFDs have been reported to occur more commonly in glaucomatous patients who are found to have IOPs within the normal range [23,24,25]. This has led the researchers to suggest that central scotoma, as opposed to peripheral scotoma, may develop in response to risk factors other than elevated IOP. As we mentioned before, Park et al. [20] reported that patients with initial parafoveal scotoma have different risk factor profiles compared to those with initial nasal step in the POAG group. However, in this study, we only analyzed the risk factors in patients with NTG, which is more prevalent in South Korea [6], because we wanted to see whether the same results would consistently be obtained when we only compared these patients.
The purpose of this study was to investigate the risk factors related to the location of VFD among patients with NTG. Thus, the patients were classified according to VFD pattern and the risk factors were compared between the ICS and IPS groups.
DH is a clinical feature of glaucoma and a predictor for the onset or progression of VFD [26]. While prevalence of DH is low in the healthy population, it occurs frequently in glaucoma, and particularly more so in NTG [27]. DH is associated with an increased risk of developing a POAG in the Ocular Hypertension Treatment Study [28], and DH is an independent risk factor of disease progression in OAG and NTG [29,30,31]. However, the pathogenesis behind DH is not fully understood. Various hypotheses related to an underlying hemodynamic disturbance have been postulated. Feke and Pasquale [32] reported that retinal vascular autoregulation is lacking in patients with OAG, and this vascular dysregulation may be related to the presence of DH in glaucoma. Grieshaber et al. [33] hypothesized that primary vascular dysregulation may be the underlying mechanism in DH, and a disturbed blood-retina barrier may be the cause of the DH. In this study, the patients in the ICS group had a higher frequency of DH detection during the follow-up period than those in the IPS group (ICS, 36%; IPS, 6%; p < 0.001). Moreover, studies have suggested that hypotension, Raynaud's phenomenon, and migraine are related to primary vascular dysregulation. Primary vascular dysregulation has been known to cause unstable ocular perfusion and act as a strong pathogenic mechanism of glaucoma [8,34]. In this study, reported hypotension, migraine, and Raynaud's phenomenon were found in higher frequency in the ICS group than in the IPS group (p < 0.001, p = 0.003, p = 0.001, respectively).
Additionally, snoring is a sign of sleep apnea [35], which has been reported to be a vascular dysregulatory risk factor for glaucoma. NTG is associated with a higher rate of sleep apnea than the normal population [36]. The higher prevalence of glaucoma, especially NTG, in patients with sleep apnea may be due to decreased ocular blood flow during sleep apnea [37]. In this study, we found that the reported snoring was significantly more frequent among patients with ICS than in patients with IPS (p = 0.001). Thus, based on the comparison of non-IOP-related risk factors, we found that vascular dysregulatory factors were more commonly reported in patients with ICS when compared with IPS.
The previous studies have reported a possible connection between smoking and glaucoma with conflicting results [13,14]. Wilson et al. [38], exploring the relationship between smoking and OAG, found a positive association of smoking with OAG. Other studies of similar nature, however, could not find smoking to be associated with OAG, nor with increased IOPs [39,40,41]. Regarding obesity, only a few studies have directly examined the association between BMI and glaucoma. Obesity seems not to be a risk factor for glaucoma by some [42], but BMI has been reported to be inversely related to OAG by others [43,44]. Also, another study has reported that a patient with higher BMI has a greater likelihood of being diagnosed with glaucoma [45]. In the Singapore Malay Eye Study, it was reported that higher BMI patients show small cup-disc ratios, and this suggests a protective effect of high BMI on OAG [46,47]. However, it is still unclear whether obesity may increase or decrease the likelihood of glaucoma. Therefore, this study was designed to determine whether lifestyle related risk factors, such as smoking or obesity, were associated with ICS in NTG patients. However, our results did not reveal a clear relationship among smoking, obesity and characteristics of VFDs. Although these findings coincided with those of previous studies, our results are based on a relatively small sampling of NTG patients and the results cannot be considered conclusive.
In this study, PSD was significantly greater in the ICS group than in the IPS group. This suggests that central field defects are of a more localized nature when compared with peripheral field defects. The reason for this phenomenon is unclear and requires further investigation.
Recently, Cho et al. [48] demonstrated that there are no differences in the clinical characteristics between ICS and IPS groups, except for the initial VF index and occurrence of superior hemifield; prevalence of DH, hypotension, migraine, and Raynaud's phenomenon are not significantly different between the two groups. These discrepancies seem to arise from the different characteristics of the two study groups, which are the follow-up period and the number of patients. The follow-up period of the study was more than 7 years, but that of the present study was about 2 years, which is a relatively short period compared with the previous study. Moreover, the total number of patients in the study was 66 and the total in this study was 159. An additional long-term follow-up study is needed to compare the results.
This study has some shortcomings due to the retrospective nature of its design and the relatively small number of patients. Also, data regarding the prevalence of systemic risk factors were collected from the questionnaire survey, which is subject to error, ignorance and recall bias. Future large-scale prospective case-control studies are needed to validate the results of this study.
In conclusion, this study found that NTG patients with ICS had a distinctive set of vascular risk factors, such as reported systemic hypotension, migraine, Raynaud's phenomenon, and self-reported snoring when compared to the patients with IPS. Likewise, DH occurs more often in patients with ICS. Awareness of the relationship between vascular risk factors and ICS may be useful in managing patients with NTG. Because patients with ICS may be at a greater risk of losing sight, NTG patients with systemic vascular factors or DH should be followed more carefully. Further study is needed to elucidate the relationship between the non-IOP vascular pathogenesis and initial VF characteristics.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–267. doi: 10.1136/bjo.2005.081224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berenson K, Kymes S, Walt JG, Siegartel LR. The relationship of mean deviation scores and resource utilization among patients with glaucoma: a retrospective United States and European chart review analysis. J Glaucoma. 2009;18:390–394. doi: 10.1097/IJG.0b013e3181879ea0. [DOI] [PubMed] [Google Scholar]
- 3.Kamal D, Hitchings R. Normal tension glaucoma: a practical approach. Br J Ophthalmol. 1998;82:835–840. doi: 10.1136/bjo.82.7.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iwase A, Suzuki Y, Araie M, et al. The prevalence of primary open-angle glaucoma in Japanese: the Tajimi Study. Ophthalmology. 2004;111:1641–1648. doi: 10.1016/j.ophtha.2004.03.029. [DOI] [PubMed] [Google Scholar]
- 5.Pekmezci M, Vo B, Lim AK, et al. The characteristics of glaucoma in Japanese Americans. Arch Ophthalmol. 2009;127:167–171. doi: 10.1001/archophthalmol.2008.593. [DOI] [PubMed] [Google Scholar]
- 6.Kim CS, Seong GJ, Lee NH, et al. Prevalence of primary open-angle glaucoma in central South Korea the Namil study. Ophthalmology. 2011;118:1024–1030. doi: 10.1016/j.ophtha.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 7.Flammer J, Mozaffarieh M. What is the present pathogenetic concept of glaucomatous optic neuropathy? Surv Ophthalmol. 2007;52(Suppl 2):S162–S173. doi: 10.1016/j.survophthal.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 8.Collaborative Normal-Tension Glaucoma Study Group. Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Am J Ophthalmol. 1998;126:487–497. doi: 10.1016/s0002-9394(98)00223-2. [DOI] [PubMed] [Google Scholar]
- 9.Flammer J, Orgul S, Costa VP, et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res. 2002;21:359–393. doi: 10.1016/s1350-9462(02)00008-3. [DOI] [PubMed] [Google Scholar]
- 10.Demailly P, Cambien F, Plouin PF, et al. Do patients with low tension glaucoma have particular cardiovascular characteristics? Ophthalmologica. 1984;188:65–75. doi: 10.1159/000309344. [DOI] [PubMed] [Google Scholar]
- 11.Tielsch JM, Katz J, Sommer A, et al. Hypertension, perfusion pressure, and primary open-angle glaucoma: a population-based assessment. Arch Ophthalmol. 1995;113:216–221. doi: 10.1001/archopht.1995.01100020100038. [DOI] [PubMed] [Google Scholar]
- 12.Mojon DS, Hess CW, Goldblum D, et al. High prevalence of glaucoma in patients with sleep apnea syndrome. Ophthalmology. 1999;106:1009–1012. doi: 10.1016/S0161-6420(99)00525-4. [DOI] [PubMed] [Google Scholar]
- 13.Lee AJ, Rochtchina E, Wang JJ, et al. Does smoking affect intraocular pressure? Findings from the Blue Mountains Eye Study. J Glaucoma. 2003;12:209–212. doi: 10.1097/00061198-200306000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Renard JP, Rouland JF, Bron A, et al. Nutritional, lifestyle and environmental factors in ocular hypertension and primary open-angle glaucoma: an exploratory case-control study. Acta Ophthalmol. 2013;91:505–513. doi: 10.1111/j.1755-3768.2011.02356.x. [DOI] [PubMed] [Google Scholar]
- 15.Pasquale LR, Kang JH. Lifestyle, nutrition, and glaucoma. J Glaucoma. 2009;18:423–428. doi: 10.1097/IJG.0b013e31818d3899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kolker AE. Visual prognosis in advanced glaucoma: a comparison of medical and surgical therapy for retention of vision in 101 eyes with advanced glaucoma. Trans Am Ophthalmol Soc. 1977;75:539–555. [PMC free article] [PubMed] [Google Scholar]
- 17.Nah YS, Seong GJ, Kim CY. Visual function and quality of life in Korean patients with glaucoma. Korean J Ophthalmol. 2002;16:70–74. doi: 10.3341/kjo.2002.16.2.70. [DOI] [PubMed] [Google Scholar]
- 18.Wiggs JL, Hewitt AW, Fan BJ, et al. The p53 codon 72 PRO/PRO genotype may be associated with initial central visual field defects in caucasians with primary open angle glaucoma. PLoS One. 2012;7:e45613. doi: 10.1371/journal.pone.0045613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buys ES, Ko YC, Alt C, et al. Soluble guanylate cyclase α1-deficient mice: a novel murine model for primary open angle glaucoma. PLoS One. 2013;8:e60156. doi: 10.1371/journal.pone.0060156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park SC, De Moraes CG, Teng CC, et al. Initial parafoveal versus peripheral scotomas in glaucoma: risk factors and visual field characteristics. Ophthalmology. 2011;118:1782–1789. doi: 10.1016/j.ophtha.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 21.Coeckelbergh TR, Brouwer WH, Cornelissen FW, et al. The effect of visual field defects on driving performance: a driving simulator study. Arch Ophthalmol. 2002;120:1509–1516. doi: 10.1001/archopht.120.11.1509. [DOI] [PubMed] [Google Scholar]
- 22.Fujita K, Yasuda N, Oda K, Yuzawa M. Reading performance in patients with central visual field disturbance due to glaucoma. Nihon Ganka Gakkai Zasshi. 2006;110:914–918. [PubMed] [Google Scholar]
- 23.Hitchings RA, Anderton SA. A comparative study of visual field defects seen in patients with low-tension glaucoma and chronic simple glaucoma. Br J Ophthalmol. 1983;67:818–821. doi: 10.1136/bjo.67.12.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Caprioli J, Spaeth GL. Comparison of visual field defects in the low-tension glaucomas with those in the high-tension glaucomas. Am J Ophthalmol. 1984;97:730–737. doi: 10.1016/0002-9394(84)90505-1. [DOI] [PubMed] [Google Scholar]
- 25.Thonginnetra O, Greenstein VC, Chu D, et al. Normal versus high tension glaucoma: a comparison of functional and structural defects. J Glaucoma. 2010;19:151–157. doi: 10.1097/IJG.0b013e318193c45c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uhler TA, Piltz-Seymour J. Optic disc hemorrhages in glaucoma and ocular hypertension: implications and recommendations. Curr Opin Ophthalmol. 2008;19:89–94. doi: 10.1097/ICU.0b013e3282f3e6bc. [DOI] [PubMed] [Google Scholar]
- 27.Healey PR, Mitchell P, Smith W, Wang JJ. Optic disc hemorrhages in a population with and without signs of glaucoma. Ophthalmology. 1998;105:216–223. doi: 10.1016/s0161-6420(98)92704-x. [DOI] [PubMed] [Google Scholar]
- 28.Budenz DL, Anderson DR, Feuer WJ, et al. Detection and prognostic significance of optic disc hemorrhages during the Ocular Hypertension Treatment Study. Ophthalmology. 2006;113:2137–2143. doi: 10.1016/j.ophtha.2006.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leske MC, Heijl A, Hyman L, et al. Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology. 2007;114:1965–1972. doi: 10.1016/j.ophtha.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 30.Drance S, Anderson DR, Schulzer M Collaborative Normal-Tension Glaucoma Study Group. Risk factors for progression of visual field abnormalities in normal-tension glaucoma. Am J Ophthalmol. 2001;131:699–708. doi: 10.1016/s0002-9394(01)00964-3. [DOI] [PubMed] [Google Scholar]
- 31.Siegner SW, Netland PA. Optic disc hemorrhages and progression of glaucoma. Ophthalmology. 1996;103:1014–1024. doi: 10.1016/s0161-6420(96)30572-1. [DOI] [PubMed] [Google Scholar]
- 32.Feke GT, Pasquale LR. Retinal blood flow response to posture change in glaucoma patients compared with healthy subjects. Ophthalmology. 2008;115:246–252. doi: 10.1016/j.ophtha.2007.04.055. [DOI] [PubMed] [Google Scholar]
- 33.Grieshaber MC, Terhorst T, Flammer J. The pathogenesis of optic disc splinter haemorrhages: a new hypothesis. Acta Ophthalmol Scand. 2006;84:62–68. doi: 10.1111/j.1600-0420.2005.00590.x. [DOI] [PubMed] [Google Scholar]
- 34.Mozaffarieh M, Grieshaber MC, Flammer J. Oxygen and blood flow: players in the pathogenesis of glaucoma. Mol Vis. 2008;14:224–233. [PMC free article] [PubMed] [Google Scholar]
- 35.Anstead M, Phillips B. The spectrum of sleep-disordered breathing. Respir Care Clin N Am. 1999;5:363–377. [PubMed] [Google Scholar]
- 36.Mojon DS, Hess CW, Goldblum D, et al. Normal-tension glaucoma is associated with sleep apnea syndrome. Ophthalmologica. 2002;216:180–184. doi: 10.1159/000059625. [DOI] [PubMed] [Google Scholar]
- 37.Karakucuk S, Goktas S, Aksu M, et al. Ocular blood flow in patients with obstructive sleep apnea syndrome (OSAS) Graefes Arch Clin Exp Ophthalmol. 2008;246:129–134. doi: 10.1007/s00417-007-0656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wilson MR, Hertzmark E, Walker AM, et al. A case-control study of risk factors in open angle glaucoma. Arch Ophthalmol. 1987;105:1066–1071. doi: 10.1001/archopht.1987.01060080068030. [DOI] [PubMed] [Google Scholar]
- 39.Ramdas WD, Wolfs RC, Hofman A, et al. Lifestyle and risk of developing open-angle glaucoma: the Rotterdam study. Arch Ophthalmol. 2011;129:767–772. doi: 10.1001/archophthalmol.2010.373. [DOI] [PubMed] [Google Scholar]
- 40.Klein BE, Klein R, Ritter LL. Relationship of drinking alcohol and smoking to prevalence of open-angle glaucoma: the Beaver Dam Eye Study. Ophthalmology. 1993;100:1609–1613. doi: 10.1016/s0161-6420(93)31429-6. [DOI] [PubMed] [Google Scholar]
- 41.Edwards R, Thornton J, Ajit R, et al. Cigarette smoking and primary open angle glaucoma: a systematic review. J Glaucoma. 2008;17:558–566. doi: 10.1097/IJG.0b013e31815f530c. [DOI] [PubMed] [Google Scholar]
- 42.Gasser P, Stumpfig D, Schotzau A, et al. Body mass index in glaucoma. J Glaucoma. 1999;8:8–11. [PubMed] [Google Scholar]
- 43.Leske MC, Connell AM, Wu SY, et al. Risk factors for open-angle glaucoma: the Barbados Eye Study. Arch Ophthalmol. 1995;113:918–924. doi: 10.1001/archopht.1995.01100070092031. [DOI] [PubMed] [Google Scholar]
- 44.Pasquale LR, Willett WC, Rosner BA, Kang JH. Anthropometric measures and their relation to incident primary open-angle glaucoma. Ophthalmology. 2010;117:1521–1529. doi: 10.1016/j.ophtha.2009.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zang EA, Wynder EL. The association between body mass index and the relative frequencies of diseases in a sample of hospitalized patients. Nutr Cancer. 1994;21:247–261. doi: 10.1080/01635589409514323. [DOI] [PubMed] [Google Scholar]
- 46.Amerasinghe N, Wong TY, Wong WL, et al. Determinants of the optic cup to disc ratio in an Asian population: the Singapore Malay Eye Study (SiMES) Arch Ophthalmol. 2008;126:1101–1108. doi: 10.1001/archopht.126.8.1101. [DOI] [PubMed] [Google Scholar]
- 47.Zheng Y, Cheung CY, Wong TY, et al. Influence of height, weight, and body mass index on optic disc parameters. Invest Ophthalmol Vis Sci. 2010;51:2998–3002. doi: 10.1167/iovs.09-4470. [DOI] [PubMed] [Google Scholar]
- 48.Cho HK, Lee J, Lee M, Kee C. Initial central scotomas vs peripheral scotomas in normal-tension glaucoma: clinical characteristics and progression rates. Eye (Lond) 2014;28:303–311. doi: 10.1038/eye.2013.285. [DOI] [PMC free article] [PubMed] [Google Scholar]