Abstract
BACKGROUND:
This study aimed to investigate the prevalence rate of critical illness-related corticosteroid insufficiency (CIRCI) and the effect of low-dose glucocorticoid on prognosis of CIRCI in patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD).
METHODS:
Since January 2010 to December 2012, 385 patients, who met the criteria of AECOPD, were enrolled in the Intensive Care Unit (ICU) of the First People’s Hospital and Municipal Central Hospital of Xiangtan City. The AECOPD patients complicated with CIRCI screened by an adrenalcorticotrophic hormone test within 12 hours after admission to ICU were divided into a treatment group (n=32) and a control group (n=31) for a prospective, randomized and controlled clinical trial. Hydrocortisone (150 mg/d) or normal saline was injected intravenously for 7 days. The patients were followed up for 28 days after injection. The endpoint included 28-day survival time, non-shock time, ICU stay and the period of non-mechanical ventilation. The markers of inflammation C-reactive protein, tumor necrosis factor-α, interleukin 6 and procalcitonin were measured at baseline and 7 days after treatment. The variables were analyzed by Student’s t test, the non-parametric statistical test, the Chi-square test or the Kaplan-Meier method with SPSS18.0 statistic software. A P value <0.05 was considered statistically significant.
RESULTS:
Totally 63 patients were diagnosed with CIRCI by an adrenalcorticotrophic hormone test and the prevalence rate was 16.4%. The shock rate of the AECOPD patients complicated with CIRCI was higher than that of the AECOPD patients without CIRCI (23.8% vs. 8.7%, P<0.01). Kaplan-Meier analysis revealed that the 28-day survival time of the treatment group was obviously longer than that of the control group (P<0.05). Compared with the control group, shock-free days within 28 days was longer in the treatment group (18.2±9.5 vs. 25.8±4.1, P<0.05). Treatment with low-dose glucocorticoid obviously decreased the markers of infection and inflammation (P<0.01), such as C-reactive protein (13.2±5.5 mg/L vs. 8.3±3.1 mg/L for the control group; 13.5±5.9 mg/L vs. 5.1±2.3 mg/L for the treatment group), tumor necrosis factor-α (26.1±16.2 μg/L vs. 17.5±11.7 μg/L for the control group; 25.0±14.8 μg/L vs. 10.4±7.8 μg/L for the treatment group) and procalcitonin (3.88 μg/L vs. 2.03 μg/L for the control group; 3.77 μg/L vs. 1.26 μg/L for the treatment group). Furthermore, the markers in the treatment group decreased more obviously than those in the control group (P<0.01).
CONCLUSION:
The prevalence rate of CIRCI was higher in the patients with AECOPD in the department of critical medicine, and low-dose glucocorticoid treatment for one week reduced the 28-day mortality, shock time and markers of infection and inflammation.
KEY WORDS: Chronic obstructive pulmonary disease, Acute exacerbation, Glucocorticoid, Critical illness, Corticosteroid insufficiency, Prevalence rate, Prognosis, Inflammation
INTRODUCTION
Critical illness-related corticosteroid insufficiency (CRICI) is associated with critical illness leading to hypothalamus-hyposhysis-adrenal-axis insufficiency and the organization systematic inflammation-relating glucocorticoid resistance, which comes with micro-circulatory disturbance, inflammatory spreading and metabolism disorder.[1] Studies[2,3] found that glucocorticoid treatment significantly improved septic shock and blood pressure in patients with early severe acute respiratory distress syndrome (ARDS), while decreasing the mortality by 30%. The glucocorticoid response in 50% patients with chronic obstructive pulmonary disease (COPD) who had used overall glucocorticoid was decreased,[4] but it was not clear either for the prevalence rate of acute exacerbation in chronic obstructive pulmonary disease (AECOPD) patients with CIRCI or if it was beneficial to use glucocorticoid hormone therapy. This study aimed to observe the prevalence rate of AECOPD patients with CIRCI and the effect of low-dose glucocortcoid treatment on the AECOPD patients with CIRCI.
METHODS
Patients
Patients who had been admitted to the Department of Critical Medicine of the First People’s Hospital and Municipal Central Hospital of Xiangtan City from January 1, 2010 to December 31, 2012 were enrolled. Inclusion criteria for the patients were as follows: 1) age above 35 years; 2) the criteria of AECOPD set in the China 2007 COPD Guidelines; 3) the diagnostic criteria of CIRCI:[1,5] randomized total cortisol was less than 10 μg/dL or the increase of total cortisol after stimulation was less than 9 μg/dL. Exclusion criteria were: 1) pregnancy or lactation; 2) cirrhosis or kidney disease syndrome or other significant hypoproteinemia (serum albumin <25 g/L); 3) primary or secondary adrenal insufficiency; 4) autoimmune diseases (AID) or use of immunosuppressants; 5) Cushing’s disease; 6) active tuberculosis and active hepatitis. The study was approved by the Ethics Committee of the First People’s Hospital of Xiangtan City, and met the criteria of the Helsinki Declaration. The enrolled patients signed written informed consent.
Methods
Patients meeting the criteria of AECOPD were subjected to adrenocorticotropic hormone test (ACTH) within 12 hours after admission to the Department of Critical Medicine, by intravenous injection of 250 μg adrenocorticotropic hormone (Shanghai No.1 Biochemical & Pharmaceutical Co., Ltd.). The total cortisol level of plasma was monitored 30 minutes and 60 minutes before and after the intravenous injection respectively (Chemiluminescent Microparticle Immunoassay, America Abbott Laboratories). Adrenal insufficiency in patients with critical illness was diagnosed by the increased levels of total cortisol (after 250 μg cosyntropin) of <9 μg/dL or random total cortisol of <10 μg/dL. The AECOPD patients with CIRCI were randomly divided into a treatment group and a control group. The patients in the treatment group were intravenously injected with hydrocortisone 50 mg per time (Shanghai Modern Hasen Pharmaceutical Co., Ltd.), 3 times a day for 7 days. The patients in the control group were intravenously injected with physiological saline of the same amount, and followed up for 28 days. Other kind of glucocorticoid was not used in both groups, but other treatment was given clinically.
Data collection
The primary endpoint was survival time of 28-day; the secondary endpoint included non-shock time, the time of admitting to the ICU as well as the time of non-mechanical ventilation. General clinical data assessment included the demographic data of the patients, and the incidence and shock rate of AECOPD patients with CIRCI. Acute physiology and chronic health evaluation (APACHE II), clinical pulmonary infection score (CPIS) and chronic obstructive pulmonary disease and asthma physiology score (CAPS) were assessed when the patients joined the group and after a 7-day treatment. The changes of interleukin 6 (IL-6, ELISA, Rapidbio, USA), tumor necrosis factor alpha (TNF-α, ELISA, Rapidbio, USA), C reactive protein (CRP, Immune Turbidimetry, Roche, Germany) and procalcitonin (PCT, immunofluorescence assay, bioMerieux, France) were observed both after the enrollment of the patients and a 7-day treatment. Pulse blood gas analysis, arterial blood pH, PaO2, PaCO2, and BE were assessed both after the enrollment of the patients and a 7-day treatment.
Safety assessment
Adverse reactions, such as double infection, gastrointestinal bleeding, hyperglycemia, hypernatronemia, stroke, acute myocardial infarction and mental disorder were evaluated.
Statistical analysis
The data were analyzed with SPSS18.0 for Windows and presented as mean±SD or median (P25, P75). Student’s t test or non-parametric test was used appropriately. The Kaplan-Meier method was used for survival analysis. P<0.05 was considered statistically significant.
RESULTS
Clinical and biochemical parameters in AECOPD patients
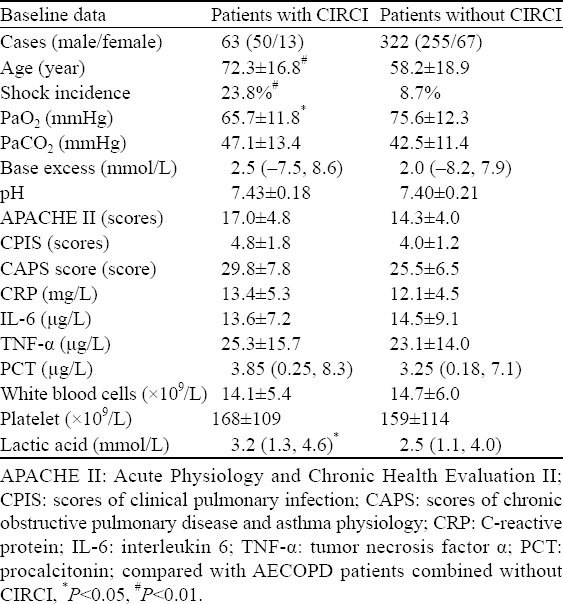
A total of 385 AECOPD patients were enrolled in the study. Of these patients, 63 (16.4%) were diagnosed with CIRCI by ACTH stimulation test. The AECOPD patients with CIRCI were at age of 72.3±16.8 and those without CIRCI were at age of 58.2±18.9 (P<0.01). Shock occurred in 15 (23.8%) AECOPD patients with CIRCI and in 28 (8.7%) AECOPD patients without CIRCI (P<0.01). Compared with AECOPD patients without CIRCI, AECOPD patients with CIRCI had a lower concentration of PaO2 but a higher plasma concentration of lactic acid (P<0.01). However, no significant difference was found in arterial blood pH, PaCO2, base excess (BE), white blood cells, platelets, IL-6, TNF-α, CRP, PCT, APACHE II score, CPIS score and CAPS score between the two groups (Table 1).
Table 1.
Clinical and biochemical parameters of the AECOPD patients with or without CIRCI
Prognostic effect of hydrocortisone on AECOPD patients with CIRCI
All the patients were followed up for 28 days. After one week of hydrocortisone treatment, the 28-day mortality rate of the treatment group was 2/32, which was lower than that of the control group (8/31). Kaplan-Meier analysis revealed that the 28-day survival time of the treatment group was longer than that of the control group (P<0.05) (Figure 1).
Figure 1.
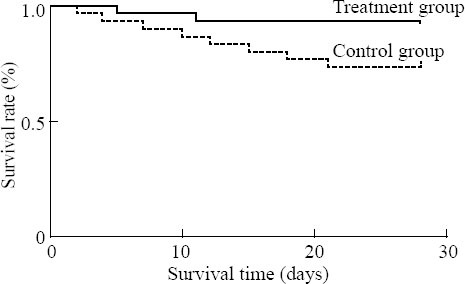
Effect of glucocorticoid on the survival rate of the corticosteroid insufficient patients with AECOPD.
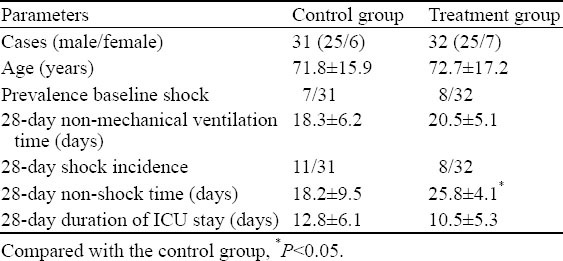
Effect of hydrocortisone on AECOPD patients with CIRCI
After one week of hydrocortisone treatment, the prevalence rate of shock in 28 days in the treatment group was 8/32, lower than 11/31 of the control group (P>0.05). Similarly, there was no significant difference between admission to ICU and non-mechanical ventilation for 28 days (P>0.05). However, the average time of 28-day non-shock was longer in the treatment group than in the control group (25.8±4.1 days vs. 18.2±9.5, P<0.05). After one-week treatment, the scores of APACHE II, CPIS and CAPS were significant in the two groups (P<0.05), but no significant difference was seen between the two groups after treatment (P>0.05). In addition, no significant difference was seen in arterial blood pH, PaO2, PaCO2, base excess (BE), etc between the two groups (P>0.05) (Table 2).
Table 2.
Effect of glucocorticoid on prognosis, disease severity and markers of infection and inflammation in the corticosteroid insufficient patients with AECOPD
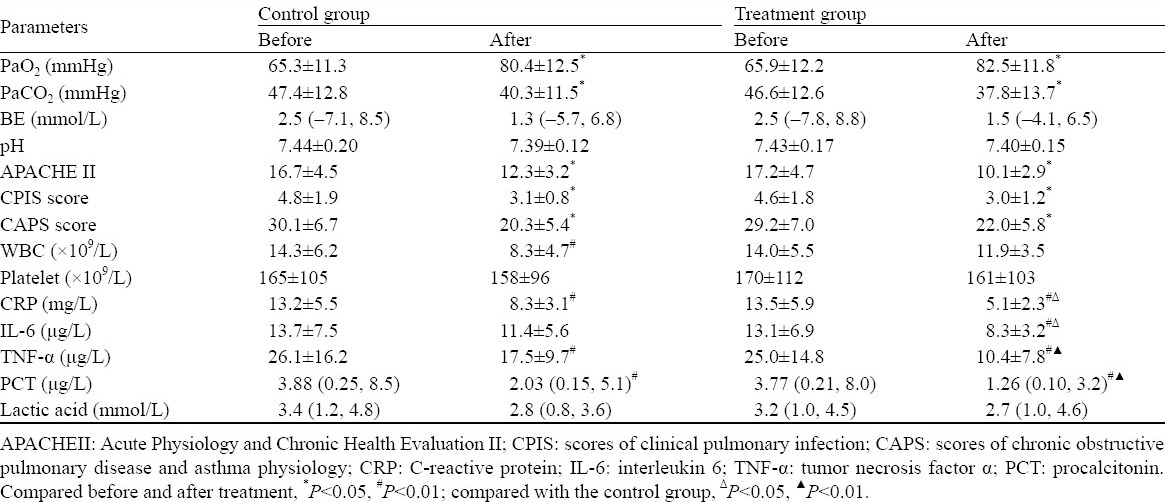
Effect of hydrocortisone on inflammation and infection of AECOPD patients with CIRCI
CRP, TNF-α, IL-6 and PCT were sensitive indexes for the assessment of inflammation and infection. After 7-day treatment, the CRP levels of the two groups decreased significantly (the control group: 13.2±5.5 mg/L vs. 8.3±3.1 mg/L; the treatment group: 13.5±5.9 mg/L vs. 5.1±2.3 mg/L) (P<0.01). The levels of TNF-α, IL-6, and PCT decreased more significantly in the treatment group than in the control group (Table 3).
Table 3.
Changes of CRP, TNF-α, IL-6 and PCT before and after treatment
Side-effects
Three patients from each group were diagnosed with stress ulcer. After treatment by relieving hyperacidity, stomach protection, fasting, these patients returned to normal. They did not develop ventilator associated pneumonia or mental symptoms. After 7-day treatment, no significant difference was seen in blood glucose and electrolytes between the two groups.
DISCUSSION
It is generally considered that adrenal insufficiency is rare, but in recent years, its morbidity has been increasing. From 1996 to 2008, the annual rate of adrenal insufficiency of inpatients in Taiwan was increased by 1.5 times.[6] In ICU patients, there is a higher prevalence rate of adrenal insufficiency, with a rate of 60% in patients with septic shock. The prevalence rate of adrenal insufficiency in ICU patients was reported to be 10% –20%.[1] In Taiwan, approximately 4.5% of COPD patients among inpatients suffered from adrenal cortical insufficiency.[6] However, there is no report concerning the prevalence rate of adrenal insufficiency in AECOPD patients. The present study found that the prevalence rate adrenal insufficiency in AECOPD patients with CIRCI admitted to ICU was 16.4%. The causes of increased incidence of CIRCI may be associated with hypothalamic-pituitary-adrenal-axis suppression, glucocorticoid resistance and chronic hypoxia. Generally, a short-term (14 days) corticosteroid treatment has little effect on suppression of the hypothalamic-pituitary-adrenal-axis in AECOPD patients.[7,8] As the function of the hypothalamic-pituitary-adrenal-axis has been inhibited after one-day glucocorticoid treatment, the inhibition lasts for several days to 3 weeks.[4] COPD patients repeatedly use intravenous corticosteroids or inhaled corticosteroids in a long period, which may cause further or persisting inhibition of the adrenal cortex. Glucocorticoid resistance also exists in some chronic inflammatory diseases, such as COPD, severe asthma, etc. Acute inflammation like pneumonia further exacerbates glucocorticoid resistance in AECOPD patients.[1] Therefore, it is common for AECOPD patients to suffer from adrenal insufficiency, while increasing the incidence of shock and decreasing oxygen saturation.
It has been controversial whether CIRCI patients need glucocorticoid treatment or not. Early studies showed that hydrocortisone is ineffective or harmful in patients with septic shock. Recent studies[2,9] have found that hydrocortisone at a dose of 200–300 mg/day is beneficial to patients with relative adrenal insufficiency. Hydrocortisone can significantly increase the percentage of ventilator weaning and blood pressure in intubated patients with adrenal insufficiency.[10,11] Glucocorticoids can decrease the 28-day mortality of CIRCI patients with septic shock by 30%. Glucocorticoid treatment for patients with early ARDS, severe community acquired pneumonia, hepatic failure, pancreatitis and cardiopulmonary bypass after operation has been reported.[1,12] However, it has not been reported whether it is beneficial to use hydrocortisone in AECOPD patients with CIRCI or not. In this study we found that the low-dose of glucocorticoid prolonged the 28-day survival time of the patients in the treatment group compared with that in the control group. Moreover, glucocorticoid treatment also improved the 28-day non-shock time of AECOPD patients with CIRCI. Possibly, glucocorticoid treatment enhanced the vascular activity and catecholamine reactivity, and inhibited inflammatory reaction. Although glucocorticoid treatment of AECOPD patients with CIRCI is still under investigation, the results of this study are promising.
COPD is a chronic inflammatory disease characterized by the increase of inflammatory mediators including interleukin 8, interleukin 6 and tumor necrosis factor α.[13] Infection exacerbates the inflammatory status of the disease. COPD patients with adrenal insufficiency may suffer from uncontrolled inflammation or extensive infection. Glucocorticoid is an anti-inflammatory agent for inhibition of cytokine production, prevention of inflammatory cell migration from the circulation to the organization.[14–15] Early treatment with methylprednisolone can decrease the level of inflammatory factors in patients with early ARDS.[16] The present study revealed that glucocorticoid treatment has a strong effect on indexes of inflammation and infection, such as IL-6, TNF-α, CRP, and PCT. It was also suggested that the low-dose of glucocorticoid would not deteriorate the infection of AECOPD patients with adrenal insufficiency. Glucocorticoid treatment would be more effective to control infection and suppress inflammation. Whether this leads to a shorter shock time and longer survival time of the patients in the treatment group is worth further investigating.
Our study has limitations. First, only 63 patients were diagnosed with CIRCI, hence the sample size was small. Second, we did not analyze the relationship among disease severity, infection markers, inflammation and prognosis. Third, we did not observe the effect of low-dose glucocorticoid on the long-term prognosis.
In conclusion, the prevalence rate of CIRCI is high in patients with AECOPD, and low-dose glucocorticoid can promote the stabilization of hemodynamics, control inflammation, and decrease the mortality of the patients.
Footnotes
Funding: None.
Ethical approval: The present study was approved by the Ethical Committee of the First People’s Hospital of Xiangtan City and Xiangtan Municipal Central Hospital.
Conflicts of interest: No any benefits have been received from a commercial party related directly or indirectly to the study.
Contributors: Sun WP and Yuan GX contributed equally to the paper. Sun WP and Yuan GX proposed the study, and Sun WP wrote the first draft. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
- 1.Marik PE, Pastores SM, Annane D, Meduri GU, Sprung CL, Arlt W, et al. Recommendations for the diagnosis and management of corticosteroid insufficiency in critically ill adult patients: consensus statements from an international task force by the American College of Critical Care Medicine. Crit Care Med. 2008;36:1937–1949. doi: 10.1097/CCM.0b013e31817603ba. [DOI] [PubMed] [Google Scholar]
- 2.Annane D, Sébille V, Charpentier C, Bollaert PE, François B, Korach JM, et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA. 2002;288:862–871. doi: 10.1001/jama.288.7.862. [DOI] [PubMed] [Google Scholar]
- 3.Liu L, Li J, Huang YZ, Liu SQ, Yang CS, Guo FM, et al. The effect of stress dose glucocorticoid on patients with acute respiratory distress syndrome combined with critical illness-related corticosteroid insufficiency. Zhonghua Nei Ke Za Zhi. 2012;51:599–603. [PubMed] [Google Scholar]
- 4.Schuetz P, Christ-Crain M, Schild U, Süess E, Facompre M, Baty F, et al. Effect of a 14-day course of systemic corticosteroids on the hypothalamic-pituitary-adrenal-axis in patients with acute exacerbation of chronic obstructive pulmonary disease. BMC Pulm Med. 2008;8:1–8. doi: 10.1186/1471-2466-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang YC, Zhang SJ, Teng GL, Tian GL, Xu L, Cao RF, et al. Adrenal insufficiency evaluation by using low-dose ACTH stimulation test in critical illness children. Zhonghua Er Ke Za Zhi. 2012;21:472–477. [Google Scholar]
- 6.Chen YC, Lin YH, Chen SH, Chen YC, Chou LF, Chen TJ, et al. Epidemiology of adrenal insufficiency: a nationwide study of hospitalizations in Taiwan from 1996 to 2008. J Chin Med Assoc. 2013;76:140–145. doi: 10.1016/j.jcma.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 7.Niewoehner DE, Erbland ML, Deupree RH, Collins D, Gross NJ, Light RW, et al. Effect of systemic glucocorticoids on exacerbations of chronic obstructive pulmonary disease. Department of Veterans Affairs Cooperative Study Group. N Engl J Med. 1999;340:1941–1947. doi: 10.1056/NEJM199906243402502. [DOI] [PubMed] [Google Scholar]
- 8.Vondracek SF, Hemstreet BA. Is there an optimal corticosteroid regimen for the management of an acute exacerbation of chronic obstructive pulmonary disease? Pharmacotherapy. 2006;26:522–532. doi: 10.1592/phco.26.4.522. [DOI] [PubMed] [Google Scholar]
- 9.He J, Hou XY. The potential contributions of traditional Chinese medicine to emergency medicine. World J Emerg Med. 2013;4:92–97. doi: 10.5847/wjem.j.issn.1920-8642.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang CJ, Lin HC. Association between adrenal insufficiency and ventilator weaning. Am J Respir Crit Care Med. 2006;173:276–280. doi: 10.1164/rccm.200504-545OC. [DOI] [PubMed] [Google Scholar]
- 11.Sprung CL, Annane D, Keh D, Moreno R, Singer M, Freivogel K, et al. Hydrocortisone therapy for patients with septic shock. N Engl J Med. 2008;358:111–124. doi: 10.1056/NEJMoa071366. [DOI] [PubMed] [Google Scholar]
- 12.Thomas Z, Fraser GL. An update on the diagnosis of adrenal insufficiency and the use of corticotherapy in critical illness. Ann Pharmacother. 2007;41:1456–1465. doi: 10.1345/aph.1K082. [DOI] [PubMed] [Google Scholar]
- 13.Xie J, Yang XY, Shi JD, Deng XQ, Long W. A new inflammation marker of chronic obstructive pulmonary disease–adiponectin. World J Emerg Med. 2010;1:190–195. [PMC free article] [PubMed] [Google Scholar]
- 14.Liu ZH, Zhang XR, Hu XY, Cheng MY, Xu JY, Du YC. Effect of glucocorticoid on MIP-1α and NF-κb expressing in the lung of rats undergoing mechanical ventilation with a high tidal volume. World J Emerg Med. 2011;2:66–69. [PMC free article] [PubMed] [Google Scholar]
- 15.Arafah BM. Hypothalamic pituitary adrenal function during critical illness: limitations of current assessment methods. J Clin Endocrinol Metab. 2006;91:3725–3745. doi: 10.1210/jc.2006-0674. [DOI] [PubMed] [Google Scholar]
- 16.Seam N, Meduri GU, Wang H, Nylen ES, Sun J, Schultz MJ, et al. Effects of methylprednisolone infusion on markers of inflammation, coagulation, and angiogenesis in early acute respiratory distress syndrome. Crit Care Med. 2012;40:495–501. doi: 10.1097/CCM.0b013e318232da5e. [DOI] [PMC free article] [PubMed] [Google Scholar]


