Abstract
The occurrence of ventricular fibrillation, induced by bipolar electrocautery during elective dual chamber pacemaker implantation, is reported in a patient affected by Myotonic Distrophy type 1 with normal left ventricular ejection fraction
Key words: ventricular fibrillation, bipolar electrocautery, pacemaker implantation, Myotonic Dystrophy type 1
Introduction
Electrocautery is often used to minimize bleeding during surgery. The probe used to perform electrocautery generates a high frequency electrical current that may be identified as noise, or mis-identified as an intrinsic heart activity by implanted pacemakers or defibrillators (1, 2).
Seven cases of electrocautery-induced ventricular tachycardia/fibrillation (VT/VF) during the implantation of pacemaker/defibrillators have been recently reported (3-6), four of them in patients with ischemic cardiomyopathy. In all cases the monopolar electrocautery system was used.
We report the first case of the occurrence of a ventricular fibrillation induced by bipolar electrocautery during elective dual chamber pacemaker implantation, in a patient affected by Myotonic Distrophy type 1 with preserved left ventricular function.
Case report
A 46-years-old man with Myotonic Dystrophy type 1 (DM1) was referred to our division for pre-syncopal episodes. Electrocardiogram (ECG) revealed sinus rhythm, extreme left axis deviation, 2:1 atrioventricolar block with a wide QRS complex. Trans-thoracic echocardiogram showed left ventricular concentric remodeling, a preserved left ventricular systolic function with an ejection fraction (EF) of 55%, calculated by the Simpson's biplane method.
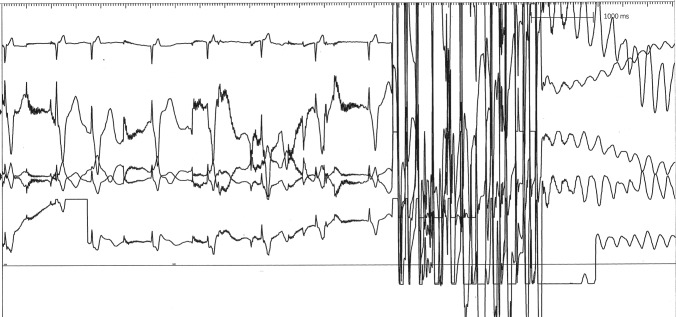
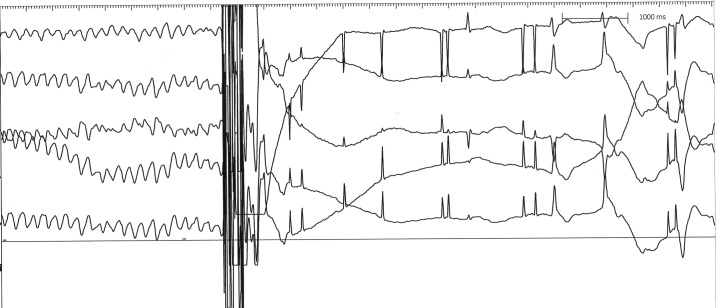
The patient was taking warfarin therapy for the occurrence of episodes of paroxysmal atrial fibrillation, and ACE-inhibitors. According to the current guidelines and personal experience, a dual chamber pacemaker implantation was performed. Because the high tromboembolic risk (CHA2DS2Vasc2: 2) warfarin therapy was not discontinued before procedure and bipolar electrocautery system was used for cutting (setting: 40 watts) and coagulation (setting: 30 watts) during the pacemaker implantation. In the last step of the procedure, after the leads and generator placement, while applying short electrocautery pulses, in coagulating mode, near the subclavian vein lead access, the patient suddenly lost consciousness with ventricular fibrillation (VF) rhythm (rate 230 bpm) documented on the monitor (Fig. 1A). VF was immediately treated using an external biphasic defibrillator through a nonsynchronized 200 J shock, that restored sinus rhythm resulting in hemodynamic stability (Fig. 1B). Lead parameters remained stable. The procedure of the pacemaker implantation was completed and the patient was discharged after two days, in which no further ventricular arrhythmias were reported. In the following 12 month follow-up, the patient did not experienced episodes of pre-syncope nor episodes of ventricular arrhythmias were documented at the device interrogation.
Figure 1.
Rhythm strips during bipolar electrocautery application in coagulating mode. Ventricular fibrillation was seen after electrocautetry was stopped (1A) and was treated (1B) using an 200 J external biphasic defibrillator non synchronized shock.
Discussion
Myotonic dystrophy type 1, or Steinert Disease, is a severe autosomal-dominant hereditary disease with an estimated incidence of 1 in 8000 in adults. The phenotype is characterized by myotonia and muscle weakness, but a multisystemic involvement with highly variable clinical manifestation is very frequent. Cardiac involvement, often preceding the skeletal muscle involvement, occurs in 80% of MD1 patients and represents the second most common cause of death, after respiratory causes (7). The most frequent clinical event in DM1 patients is the development of a supraventricular arrhythmia (8-12), commonly observed on 12 lead ECG, 24 hour Holter monitoring or device interrogation, and often asymptomatic (12, 13). The supraventricular arrhythmias most commonly observed in up to 25% of patients – both as not sustained and sustained forms (10, 14, 15) – are atrial fibrillation, atrial flutter and atrial tachycardia.
On the other hand, ventricular arrhythmias in MD1 patients may be related to the heterogeneity of ventricular repolarization, shown by an increase in QTc and JTc dispersion, as it has been reported in congenital (16-18) or acquired (19- 21) heart diseases and in neuromuscular disorders (22-24).
The occurrence of VT/VF induced by electrocautery is uncommon; in the few cases so far reported (3-6), a monopolar electrocautery system was always used. The present report is the first case of VF induced by electrocautery during bipolar configuration. A possibily mechanism explaining the ventricular fibrillation induction may be attributed to the continuous transmission of the electrocautery radiofrequency pulses to the interface with the myocardium, through the ventricular electrode. The histopathological alterations observed in DM1 patient's heart represent a highly sensitive arrhythmogenic substrate, with life-threatening consequence during the procedure of pacemaker/defibrillator implantation, also when bipolar electrocautery system is used in patients with preserved global systolic function. Therefore, the use of electrical scalpel should be only reserved to very high bleeding risk patients. In cases in which the electrocautery cannot be avoided, we strongly recommend to continuously monitor the patients and have advanced resuscitation equipment available during the procedure (25). Furthermore we suggest to perform short, intermittent, and irregular bursts at the lowest feasible energy levels in order to minimize the potential electromagnetic interference.
References
- 1.Mangar D, Atlas GM, Kane PB. Electrocautery-induced pacemaker malfunction during surgery. Can J Anaesth. 1991;38:616–618. doi: 10.1007/BF03008198. [DOI] [PubMed] [Google Scholar]
- 2.Dalibon N, Pelle-Lancien E, Puyo P, et al. Recurrent asystole during electrocauterization: an uncommon hazard in common situations. Eur J Anaesthesiol. 2005;22:476–478. doi: 10.1017/s0265021505240814. [DOI] [PubMed] [Google Scholar]
- 3.Lo R, Mitrache A, Quan W, et al. Electrocautery-induced ventricular tachycardia and fibrillation during device implantation and explantation. J Invasive Cardiol. 2007;19:12–15. [PubMed] [Google Scholar]
- 4.Goel AK, Korotkin S, Walsh D, et al. Monomorphic ventricular tachycardia caused by electrocautery during pacemaker generator change in a patient with normal left ventricular function. Pacing Clin Electrophysiol. 2009;32:957–958. doi: 10.1111/j.1540-8159.2009.02418.x. [DOI] [PubMed] [Google Scholar]
- 5.Pachón M, Arias MA, Puchol A, et al. Malignant ventricular arrhythmias during surgical procedures for pacemaker generator replacement: description of two cases. Rev Esp Cardiol (Engl Ed) 2012;65:1136–1138. doi: 10.1016/j.recesp.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 6.Cassagneau R, Hanninen M, Yee R. Electrocautery-induced ventricular fibrillation during routine implantable cardioverter-defibrillator generator replacement. Europace. 2014;16:319–319. doi: 10.1093/europace/eut267. [DOI] [PubMed] [Google Scholar]
- 7.Russo AD, Mangiola F, Della Bella P, et al. Risk of arrhythmias in myotonic dystrophy: trial design of the RAMYD study. J Cardiovasc Med (Hagerstown) 2009;10:51–58. doi: 10.2459/jcm.0b013e328319bd2c. [DOI] [PubMed] [Google Scholar]
- 8.Nigro G, Russo V, Politano L, et al. Does Bachmann's bundle pacing prevent atrial fibrillation in myotonic dystrophy type 1 patients? A 12 months follow-up study. Europace. 2010;12:1219–1223. doi: 10.1093/europace/euq170. [DOI] [PubMed] [Google Scholar]
- 9.Nigro G, Russo V, Politano L, et al. Does Bachmann's bundle pacing prevent atrial fibrillation in Myotonic Dystrophy type 1 patients? A 12 months follow-up study. Europace. 2010;12:1219–1223. doi: 10.1093/europace/euq170. [DOI] [PubMed] [Google Scholar]
- 10.Russo V, Rago A, Politano L, et al. The effect of atrial preference pacing on paroxysmal atrial fibrillation incidence in Myotonic Dystrophy type 1 patients: a prospective, randomized, single-bind cross over study. Europace. 2012;14:486–489. doi: 10.1093/europace/eur373. [DOI] [PubMed] [Google Scholar]
- 11.Russo V, Rago A, Papa AA, et al. Does a high percentage of right ventricular pacing influence the incidence of paroxysmal atrial fibrillation in Myotonic Dystrophy type 1 patients? Kardiol Pol. 2013;71:1147–1153. doi: 10.5603/KP.2013.0295. [DOI] [PubMed] [Google Scholar]
- 12.Nigro G, Russo V, Politano L, et al. Right atrial appendage versus Bachmann's bundle stimulation: a two year comparative study of electrical parameters in Myotonic Dystrophy type 1 patients. Pacing Clin Electrophysiol. 2009;32:1192–1197. doi: 10.1111/j.1540-8159.2009.02464.x. [DOI] [PubMed] [Google Scholar]
- 13.Nigro G, Russo V, Vergara P, et al. Optimal site for atrial lead implantation in Myotonic Dystrophy patients. The role of Bachmann's Bundle stimulation. Pacing Clin Electrophysiol. 2008;31:1463–1466. doi: 10.1111/j.1540-8159.2008.01210.x. [DOI] [PubMed] [Google Scholar]
- 14.Nigro G, Russo V, Rago A, et al. Right atrial preference pacing algorithm in the prevention of paroxysmal atrial fibrillation in Myotonic Dystrophy type 1 patients: a long term follow-up study. Acta Myol. 2012;31:139–143. [PMC free article] [PubMed] [Google Scholar]
- 15.Russo V, Nigro G, Rago A, et al. Atrial fibrillation burden in Myotonic Dystrophy type 1 patients implanted with dual chamber pacemaker: the efficacy of the overdrive atrial algorithm at 2 year follow-up. Acta Myol. 2013;32:142–147. [PMC free article] [PubMed] [Google Scholar]
- 16.Nigro G, Russo V, Rago A, et al. Heterogeneity of ventricular repolarization in newborns with severe aortic coarctation. Pediatr Cardiol. 2012;33:302–306. doi: 10.1007/s00246-011-0132-4. [DOI] [PubMed] [Google Scholar]
- 17.Nigro G, Russo V, Rago A, et al. The effect of aortic coarctation surgical repair on QTc and JTc dispersion in severe aortic coarctation newborns: a short term follow up study. Physiol Res. 2014;63:27–33. doi: 10.33549/physiolres.932491. [DOI] [PubMed] [Google Scholar]
- 18.Russo V, Rago A, Pannone B, et al. Dispersion of repolarization and beta-thalassemia major: the prognostic role of QT and JT dispersion for identifying the high-risk patients for sudden death. Eur J Haematol. 2011;86:324–331. doi: 10.1111/j.1600-0609.2011.01579.x. [DOI] [PubMed] [Google Scholar]
- 19.Nigro G, Russo V, Salvo G, et al. Increased heterogeneity of ventricular repolarization in obese non hypertensive children. Pacing Clin Electrophysiol. 2010;33:1533–1539. doi: 10.1111/j.1540-8159.2010.02889.x. [DOI] [PubMed] [Google Scholar]
- 20.Russo V, Ammendola E, Crescenzo I, et al. Effect of weight loss following bariatric surgery on myocardial dispersion of repolarization in morbidly obese patients. Obes Surg. 2007;17:857–865. doi: 10.1007/s11695-007-9160-9. [DOI] [PubMed] [Google Scholar]
- 21.Santangelo L, Ammendola E, Russo V, et al. of biventricular pacing on myocardial dispersion of repolarization in dilated cardiomyopathy patients. Europace. 2006;8:502–505. doi: 10.1093/europace/eul054. [DOI] [PubMed] [Google Scholar]
- 22.Nigro G, Russo V, Rago A, et al. Regional and transmural dispersion of repolarisation in patients with Emery-Dreifuss Muscular Dystrophy. Kardiol Pol. 2012;70:1154–1159. [PubMed] [Google Scholar]
- 23.Russo V, Rago A, Politano L, et al. Increased dispersion of ventricular repolarization in Emery Dreifuss Muscular Dystrophy patients. Med Sci Monit. 2012;18:CR643–CR647. doi: 10.12659/MSM.883541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nigro G, Nigro G, Politano L, et al. Is the value of QT dispersion a valid method to foresee the risk of sudden death? A study in Becker patients. Heart. 2002;87:156–157. doi: 10.1136/heart.87.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crossley GH, Poole JE, Rozner MA, et al. The Heart Rhythm Society (HRS)/American Society of Anesthesiologists (ASA) Expert Consensus Statement on the perioperative management of patients with implantable defibrillators, pacemakers and arrhythmia monitors: facilities and patient management. Heart Rhythm. 2011;8:1114–1154. doi: 10.1016/j.hrthm.2010.12.023. [DOI] [PubMed] [Google Scholar]