Abstract
Background and Objectives:
The need for more cost- and time-efficient provision of medical care has prompted an interest in remote or telehealth approaches to delivery of health care. We present a study examining the feasibility and outcomes of implementation of a telephone follow-up program for laparoscopic inguinal hernia repair.
Methods:
This is a retrospective review of consecutive patients who prospectively agreed to undergo telephone follow-up after laparoscopic inguinal hernia repair instead of standard face-to-face clinic visits. Patients received a telephone call from a dedicated physician assistant 2 to 3 weeks after surgery and answered a predetermined questionnaire. A face-to-face clinic visit was scheduled based on the results of the call or on patient request.
Results:
Of 62 patients who underwent surgery, all agreed to telephone follow-up instead of face-to-face clinic visits. Their mean round-trip distance to the hospital was 122 miles. Fifty-five patients (88.7%) successfully completed planned telephone follow-up. Three patients (4.8%) were lost to follow-up, and 4 (6.5%) were erroneously scheduled for a clinic appointment. Of the 55 patients who were reached by telephone, 50 (90.9%) were satisfied and declined an in-person clinic visit. Five patients (9.1%) returned for a clinic appointment based on concerns raised during the telephone call. Of these, 1 was found to have an early hernia recurrence and 1 had a seroma.
Conclusion:
Telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair is feasible and effective and is well received by patients.
Keywords: Telehealth, Laparoscopy, Inguinal hernia, Follow-up
INTRODUCTION
The postoperative evaluation of a patient who has undergone an operation is a fundamental part of surgical care. Proper recovery from surgery, success of an operation, and potential surgical complications are all routinely assessed at an outpatient follow-up visit.
However, the need for more cost- and time-efficient provision of medical care has prompted an interest in remote or telehealth approaches to delivery of health care.1,2 In surgical practice, there has been a growing interest in curtailing or modifying the long-practiced face-to-face clinic visit for the postoperative patient who has undergone low-risk surgery. Postoperative telephone follow-up has been found to be feasible, cost-effective, and acceptable to patients.3
Patients undergoing herniorrhaphy at our institution often travel great distances to the ambulatory surgical center and to the outpatient clinic. The patients thus frequently invest a significant amount of time and personal cost in keeping these appointments. It was previously shown that in this environment, telehealth is a safe and effective substitution for a face-to-face follow-up visit in patients undergoing open-groin hernia repair, with high patient satisfaction.4 We present a study examining the feasibility and outcomes of implementation of a telephone follow-up program for laparoscopic inguinal hernia repair.
METHODS
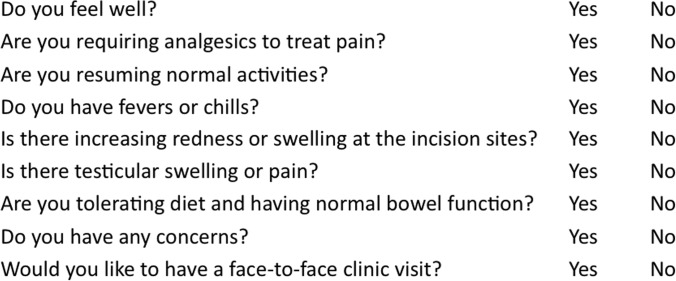
Patients undergoing laparoscopic inguinal hernia repair by 2 surgeons between March 2013 and June 2014 were offered telephone follow-up instead of face-to-face clinic visits after surgery. The operative and follow-up data were retrospectively reviewed. A certified physician assistant called the patients 2 weeks after surgery using a predetermined telephone script (Figure 1); the telephone call was not recorded. Data obtained during the telephone call included the patient's overall well-being, pain and use of analgesics, fever or chills, appearance of the incision, testicular pain or swelling, activity level, tolerated diet or appetite, and bowel function. A decision regarding the need for a face-to-face clinic visit was made during this telephone call based on the data obtained. A yes answer to any question typically prompted a clinic visit.
Figure 1.
Telephone questionnaire used during telephone follow-up call.
If no concerns were raised during the telephone call, the patient was asked if he or she was satisfied with the telephone follow-up and was offered a face-to-face visit if requested. If both the physician assistant and the patient were satisfied with the telephone follow-up, then no face-to-face clinic visit was scheduled.
Loss to follow-up was determined when the physician assistant failed to reach the patient by telephone on 3 attempts over the course of several days. We noted the number of patients who successfully completed telephone follow-up and those patients who required a clinic visit, in addition to any postoperative complications.
RESULTS
During the 15-month period of the study, 62 patients underwent a laparoscopic inguinal hernia repair. All (100%) agreed to forego a postoperative face-to-face clinic visit and be available for telephone follow-up 2 to 3 weeks after laparoscopic inguinal hernia repair. All patients were men, with a mean age of 65.8 years (range, 44–82 years). The mean round-trip travel distance to the hospital and outpatient clinic was 122 miles. Most patients (90.3%) underwent a laparoscopic inguinal hernia repair by the total extraperitoneal approach, whereas the rest underwent a transabdominal preperitoneal repair. Thirty-one patients (50%) underwent bilateral repairs, whereas 50% underwent unilateral repairs. Fifty patients (80.6%) had primary hernias repaired, whereas 12 patients had recurrent hernias (Table 1). There were no conversions to open procedures.
Table 1.
Patient Demographic Data
| Data | |
|---|---|
| No. of patients | 62 |
| Mean age (range), y | 65.8 (44–82) |
| Gender (male/female), n | 62/0 |
| TAPPa/TEPa repair, n (%) | 6 (9.7)/56 (90.3) |
| Bilateral/unilateral, n (%) | 31 (50)/31 (50) |
| Primary/recurrent, n (%) | 50 (80.6)/12 (19.4) |
| Mean round-trip distance to hospital (range), miles | 122 (18–494) |
TAPP = transabdominal preperitoneal; TEP = total extraperitoneal.
Of the 62 patients in the cohort, 55 (88.7%) successfully completed planned telephone follow-up. That is, they were reached by telephone with the intention that the call represented their follow-up visit. Three patients (4.8%) were lost to follow-up and could not be reached by telephone, whereas 4 patients (6.5%) showed up for face-to-face clinic follow-up visits because of scheduling errors (Table 2).
Table 2.
Results of Telephone Follow-Up
| Data, n (%) | |
|---|---|
| Agreed to telephone follow-up | 62 (100) |
| Successfully completed telephone follow-up | 55 (88.7) |
| Lost to follow-up | 3 (4.8) |
| Scheduling errors | 4 (6.5) |
| Requested clinic visit | 5 (9.1) |
| Satisfied with telephone follow-up | 50 (90.9) |
Of the 55 patients who completed the telephone follow-up, 5 (9.1%) presented for a face-to-face clinic appointment based on the patient's request or concerns raised during the telephone call. Two of these patients presented with a recurrent bulge: 1 patient had a postoperative seroma and received reassurance, and 1 patient who underwent a total extraperitoneal repair of a recurrent inguinal hernia presented with an early recurrence and was scheduled for reoperation. The other 3 patients had minimal groin discomfort and no clinical findings and received reassurance.
Of the 55 patients reached by telephone, 50 (90.9%) were satisfied with telephone follow-up and declined face-to-face postoperative clinic visits. Of these patients, 1 had postoperative testicular pain and was seen by a local physician and treated for epididymitis. None of these patients presented later with complications.
DISCUSSION
In this study we showed that a standardized protocol for telephone follow-up by a dedicated midlevel provider could be used instead of a face-to-face clinic visit in patients undergoing laparoscopic inguinal hernia repair. To date, telehealth has been used with success in the fields of general adult and pediatric surgery, gynecology, and urology.3–9
Primary care medicine has long relied on the use of telephone follow-up for health maintenance between outpatient clinic visits. For example, at our institution, it is common for patients to monitor their blood pressure and blood glucose level at home and provide the primary care physician with the results electronically or by telephone, which can then guide their hypertension and diabetes management, without necessitating a face-to-face visit. Complex issues, such as chronic musculoskeletal pain, can be treated with telephone-based interventions. In a randomized trial, Kroenke et al10 recently showed the efficacy of a standardized approach using telephone follow-up, implemented by a nurse care manager in consultation with a physician pain specialist, in the treatment of chronic pain.
Given the large geographic area that is served by our Veterans Affairs (VA) hospital, our patients routinely travel large distances to receive care, including ambulatory and inpatient surgery and outpatient services. This may explain why 100% of our patients accepted a telephone-based follow-up visit, and thus findings may not necessarily be relevant to the general population. However, we noted that those patients who did not need to travel large distances also had a preference for telephone follow-up over a clinic visit. It seems reasonable that there be a strong patient preference for the convenience of a telephone visit. The vast majority of the patients who were called (>90%) were satisfied with telephone follow-up and declined further outpatient visits. To our knowledge, there were no patient complaints received by the physician or the hospital.
There is the possibility of a delayed presentation of a postoperative complication that will not be apparent to the patient at the time of the 2-week postoperative telephone call. This, however, may also be true of the patient presenting to the clinic at 2 weeks. We have implemented a follow-up system that takes advantage of the single-payer VA Health Care System and its electronic medical record to search for evidence of delayed complications because our patients receive nearly all of their care within the VA system. The midlevel provider searches the electronic medical record at 30 days postoperatively to assess for any emergency department or clinic visits that relate to delayed complications of inguinal hernia repair surgery. In our experience, we have found no additional complaints that were not previously apparent during the 2-week telephone call.
Our study findings suggest that implementation of telephone follow-up does not compromise patient care. The overall complication rate was low and did not appear related to the method of follow-up. In fact, our data suggest that telephone follow-up is effective at identifying patients who would benefit from a face-to-face evaluation. Of the 55 patients who only had a telephone follow-up, only 1 was identified with a clinical problem that was readily treated on an outpatient basis. Otherwise, none of the patients presented at a later time with a clinical problem.
In addition to the possible benefit to the patient and the physician, a telephone follow-up program has been shown to have significant benefit for the hospital system. Hwa and Wren4 showed that clinic availability increases with implementation of an ambulatory surgery telephone follow-up program, allowing for enhanced patient access to clinic and ambulatory services overall.
This study was designed to assess the feasibility of a telephone follow-up program for patients undergoing laparoscopic inguinal hernia repair. It is limited by the retrospective review of the data. The results of this study, however, provide data to suggest efficacy and high patient satisfaction. A randomized cohort study is needed to compare the outcomes of patients randomly assigned to a face-to-face clinic visit versus a telephone follow-up by a midlevel provider.
CONCLUSION
Telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair is feasible and effective and is well received by patients. Telephone follow-up may prove to be a substitute for routine face-to-face clinic follow-up for patients undergoing laparoscopic inguinal hernia repair and is especially attractive for patients who have to travel long distances for their clinic visit.
Contributor Information
Dan Eisenberg, Department of Surgery, Palo Alto Veterans Affairs Health Care System, Palo Alto, CA, USA.; Department of Surgery, Stanford School of Medicine, Palo Alto, CA, USA.
Kimberly Hwa, Department of Surgery, Palo Alto Veterans Affairs Health Care System, Palo Alto, CA, USA..
Sherry M. Wren, Department of Surgery, Palo Alto Veterans Affairs Health Care System, Palo Alto, CA, USA.; Department of Surgery, Stanford School of Medicine, Palo Alto, CA, USA.
References:
- 1. Car J, Sheikh A. Telephone consultations. Br Med J. 2003;326:966–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Moran SJ, Jarvis S, Ewings P, Parkin FA. It's good to talk, but is it effective? A comparative study of telephone support following day surgery. Clin Eff Nurs. 1998;2:175–182. [Google Scholar]
- 3. Gray RT, Sut MK, Badger SA, Harvey CF. Post-operative telephone review is cost-effective and acceptable to patients. Ulster Med J. 2010;79:76–79. [PMC free article] [PubMed] [Google Scholar]
- 4. Hwa K, Wren SM. Telehealth follow-up in lieu of postoperative clinic visit for open hernia repair surgery. JAMA Surg. 2013;148:823–827. [DOI] [PubMed] [Google Scholar]
- 5. Kimman ML, Bloebaum MM, Dirksen CD, Houben RM, Lambin P, Boersma LJ. Patient satisfaction with nurse-led telephone follow-up after curative treatment for breast cancer. BMC Cancer. 2010;10:174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rosbe KW, Jones D, Jalisi S, Bray MA. Efficacy of postoperative follow-up telephone calls for patients who underwent adenotonsillectomy. Arch Otolaryngol Head Neck Surg. 2000;126:718–721. [DOI] [PubMed] [Google Scholar]
- 7. Brough RJ, Pidd H, O'Flynn KJ, Payne SR. Identification of patients requiring out-patient follow-up after transurethral prostatectomy: is there a role for nurse led screening of post-operative outcomes by telephone? Br J Urol. 1996;78:401–404. [DOI] [PubMed] [Google Scholar]
- 8. Glavind K, Bjork J, Lindquist ASI. A retrospective study on telephone follow-up of anterior colporrhaphy by a specialized nurse. Int Urogynecol J. In press 2014. [DOI] [PubMed] [Google Scholar]
- 9. Bateman AG, Neilens H, Gericke CA, George J, Freeman RM. Is there a need for postoperative follow-up after routine urogynaecological procedures? Patients will self-present if they have problems. Int Urogynecol. J 2014;25:381–386. [DOI] [PubMed] [Google Scholar]
- 10. Kroenke K, Krebs EE, Wu J, Yu Z, Chumbler NR, Blair MJ. Telecare collaborative management of chronic pain in primary care: a randomized clinical trial. JAMA. 2014;312:240–248. [DOI] [PubMed] [Google Scholar]