Abstract
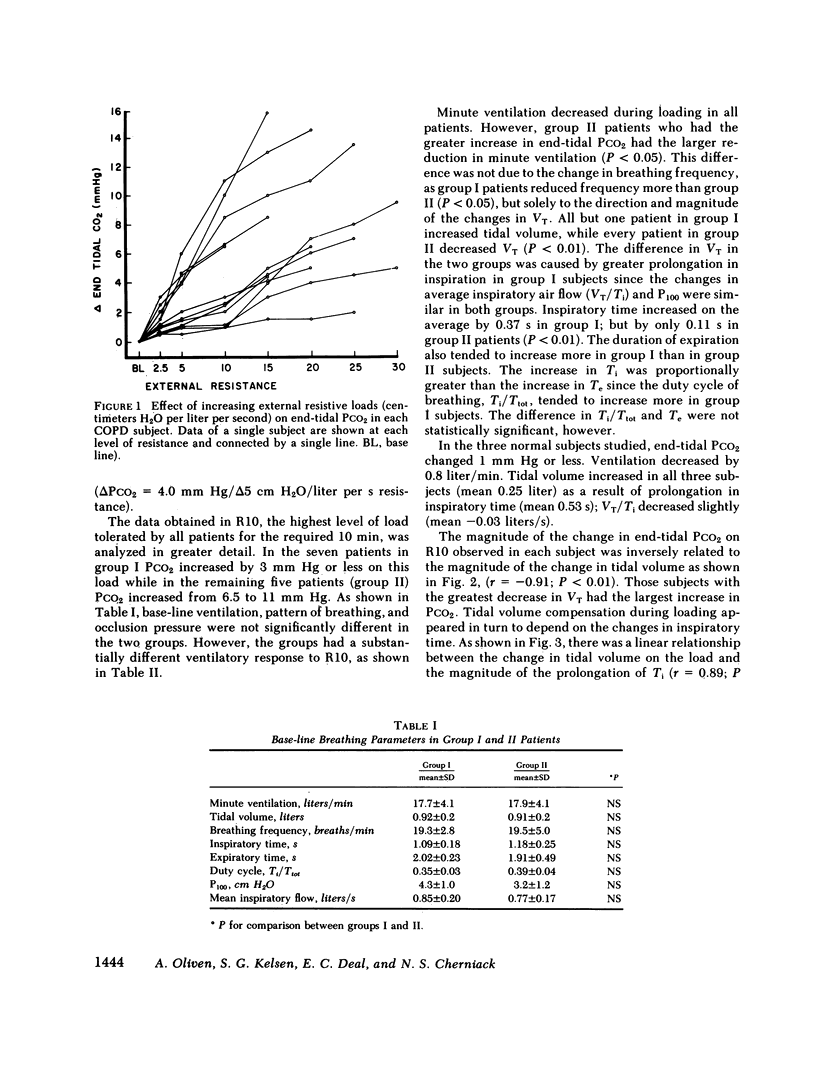
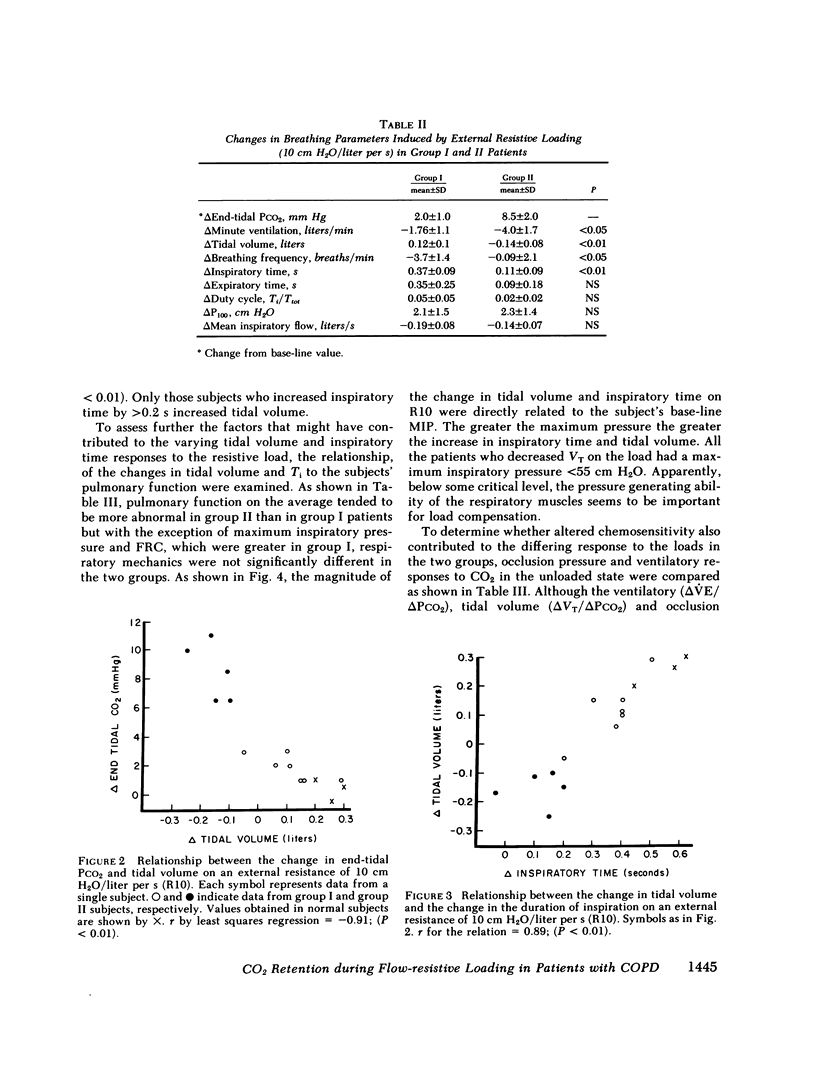
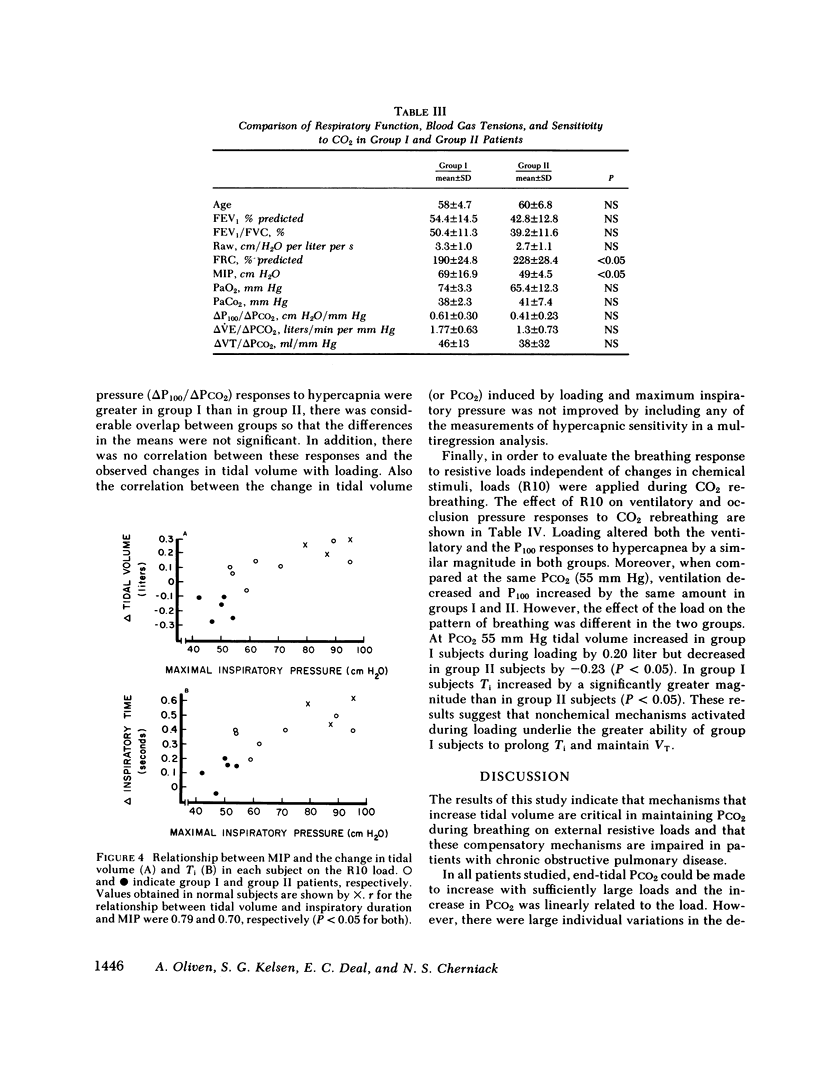
The present study examined the respiratory responses involved in the maintenance of eucapnea during acute airway obstruction in 12 patients with chronic obstructive disease (COPD) and 3 age-matched normal subjects. Acute airway obstruction was produced by application of external flow-resistive loads (2.5 to 30 cm H2O/liter per s) throughout inspiration and expiration while subjects breathed 100% O2. Application of loads of increasing severity caused progressive increases in PCO2 in the patients, but the magnitude of the increase in PCO2 varied substantially between subjects. On a resistance of 10 cm H2O/liter per s, the highest load that could be tolerated by all COPD patients, the increase in PCO2 ranged from 1 to 11 mm Hg, while none of the normal subjects retained CO2. Based on the magnitude of the increase in PCO2 the patients could be divided into two groups: seven subjects whose PCO2 increased by less than or equal to 3 mm Hg (group I) and five subjects whose PCO2 increased by greater than 6 mm Hg (group II). Base-line ventilation and the pattern of breathing were similar in the two groups. During loading group I subjects maintained or increased tidal volume while all group II patients decreased tidal volume (VT). The smaller tidal volume in group II subjects was mainly the result of their shorter inspiratory time as the changes in mean inspiratory flow were similar in the two groups. The magnitude of CO2 retention during loading was inversely related to the magnitude of the change in VT (r = -0.91) and inspiratory time (Ti) (r = -0.87) but only weakly related to the change in ventilation (r = -0.53). The changes in PCO2, VT, and Ti during loading correlated with the subjects' maximum static inspiratory pressure, which was significantly lower in group II as compared with group I patients. These results indicate that the tidal volume and respiratory timing responses to flow loads are impaired in some patients with COPD. This impairment, presumably due to poor inspiratory muscle function, appears to lead to CO2 retention during loaded breathing.
Full text
PDF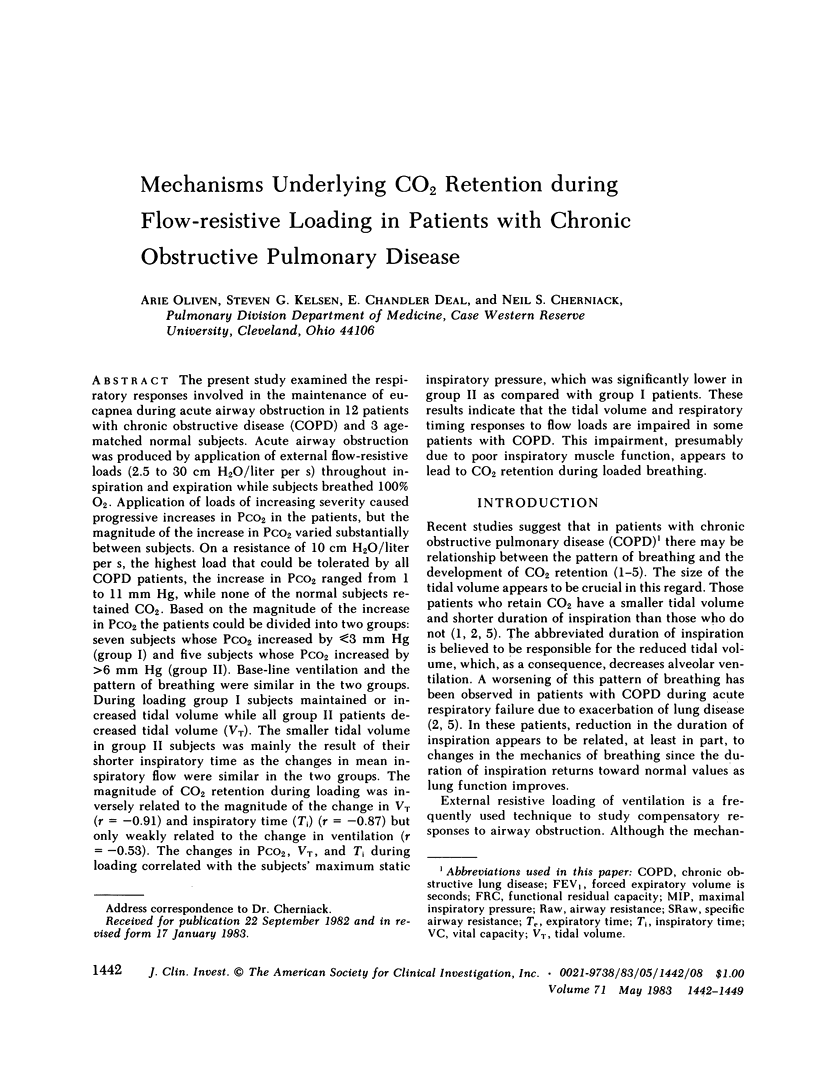


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Altose M. D., McCauley W. C., Kelsen S. G., Cherniack N. S. Effects of hypercapnia and inspiratory flow-resistive loading on respiratory activity in chronic airways obstruction. J Clin Invest. 1977 Mar;59(3):500–507. doi: 10.1172/JCI108665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora N. S., Rochester D. F. Respiratory muscle strength and maximal voluntary ventilation in undernourished patients. Am Rev Respir Dis. 1982 Jul;126(1):5–8. doi: 10.1164/arrd.1982.126.1.5. [DOI] [PubMed] [Google Scholar]
- Aubier M., Murciano D., Fournier M., Milic-Emili J., Pariente R., Derenne J. P. Central respiratory drive in acute respiratory failure of patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1980 Aug;122(2):191–199. doi: 10.1164/arrd.1980.122.2.191. [DOI] [PubMed] [Google Scholar]
- Campbell E. J., Gandevia S. C., Killian K. J., Mahutte C. K., Rigg J. R. Changes in the perception of inspiratory resistive loads during partial curarization. J Physiol. 1980 Dec;309:93–100. doi: 10.1113/jphysiol.1980.sp013496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman S. O. Editorial: Circulating antibodies in pulmonary tuberculosis. Chest. 1976 Jul;70(1):1–2. doi: 10.1378/chest.70.1.1. [DOI] [PubMed] [Google Scholar]
- Homma I. Inspiratory inhibitory reflex caused by the chest wall vibration in man. Respir Physiol. 1980 Mar;39(3):345–353. doi: 10.1016/0034-5687(80)90065-1. [DOI] [PubMed] [Google Scholar]
- Iber C., Berssenbrugge A., Skatrud J. B., Dempsey J. A. Ventilatory adaptations to resistive loading during wakefulness and non-REM sleep. J Appl Physiol Respir Environ Exerc Physiol. 1982 Mar;52(3):607–614. doi: 10.1152/jappl.1982.52.3.607. [DOI] [PubMed] [Google Scholar]
- Isaza G. D., Posner J. D., Altose M. D., Kelsen S. G., Cherniack N. S. Airway occlusion pressures in awake and anesthetized goats. Respir Physiol. 1976 Jul;27(1):87–98. doi: 10.1016/0034-5687(76)90020-7. [DOI] [PubMed] [Google Scholar]
- Javaheri S., Blum J., Kazemi H. Pattern of breathing and carbon dioxide retention in chronic obstructive lung disease. Am J Med. 1981 Aug;71(2):228–234. doi: 10.1016/0002-9343(81)90116-9. [DOI] [PubMed] [Google Scholar]
- Kelsen S. G., Fleegler B., Altose M. D. The respiratory neuromuscular response to hypoxia, hypercapnia, and obstruction to airflow in asthma. Am Rev Respir Dis. 1979 Sep;120(3):517–527. doi: 10.1164/arrd.1979.120.3.517. [DOI] [PubMed] [Google Scholar]
- Kelsen S. G., Nochomovitz M. L. Fatigue of the mammalian diaphragm in vitro. J Appl Physiol Respir Environ Exerc Physiol. 1982 Aug;53(2):440–447. doi: 10.1152/jappl.1982.53.2.440. [DOI] [PubMed] [Google Scholar]
- Killian K. J., Bucens D. D., Campbell E. J. Effect of breathing patterns on the perceived magnitude of added loads to breathing. J Appl Physiol Respir Environ Exerc Physiol. 1982 Mar;52(3):578–584. doi: 10.1152/jappl.1982.52.3.578. [DOI] [PubMed] [Google Scholar]
- MARSHALL R., MCILROY M. B. The mechanical properties of the lungs in asthma. Clin Sci. 1956 May;15(2):345–351. [PubMed] [Google Scholar]
- Macklem P. T., Roussos C. S. Respiratory muscle fatigue: a cause of respiratory failure? Clin Sci Mol Med. 1977 Nov;53(5):419–422. doi: 10.1042/cs0530419. [DOI] [PubMed] [Google Scholar]
- McCloskey D. I. Kinesthetic sensibility. Physiol Rev. 1978 Oct;58(4):763–820. doi: 10.1152/physrev.1978.58.4.763. [DOI] [PubMed] [Google Scholar]
- Murciano D., Aubier M., Viau F., Bussi S., Milic-Emili J., Pariente R., Derenne J. P. Effects of airway anesthesia on pattern of breathing and blood gases in patients with chronic obstructive pulmonary disease during acute respiratory failure. Am Rev Respir Dis. 1982 Jul;126(1):113–117. doi: 10.1164/arrd.1982.126.1.113. [DOI] [PubMed] [Google Scholar]
- Pardy R. L., Rivington R. N., Milic-Emili J., Mortola J. P. Control of breathing in chronic obstructive pulmonary disease. The effect of histamine inhalation. Am Rev Respir Dis. 1982 Jan;125(1):6–11. doi: 10.1164/arrd.1982.125.1.6. [DOI] [PubMed] [Google Scholar]
- Read D. J., Freedman S., Kafer E. R. Pressures developed by loaded inspiratory muscles in conscious and anesthetized man. J Appl Physiol. 1974 Aug;37(2):207–218. doi: 10.1152/jappl.1974.37.2.207. [DOI] [PubMed] [Google Scholar]
- Remmers J. E., Marttila I. Action of intercostal muscle afferents on the respiratory rhythm of anesthetized cats. Respir Physiol. 1975 Jun;24(1):31–41. doi: 10.1016/0034-5687(75)90119-x. [DOI] [PubMed] [Google Scholar]
- Roussos C. The failing ventilatory pump. Lung. 1982;160(2):59–84. doi: 10.1007/BF02719275. [DOI] [PubMed] [Google Scholar]
- Shannon R. Intercostal and abdominal muscle afferent influence on medullary dorsal respiratory group neurons. Respir Physiol. 1980 Jan;39(1):73–94. doi: 10.1016/0034-5687(80)90015-8. [DOI] [PubMed] [Google Scholar]
- Skatrud J. B., Dempsey J. A., Bhansali P., Irvin C. Determinants of chronic carbon dioxide retention and its correction in humans. J Clin Invest. 1980 Apr;65(4):813–821. doi: 10.1172/JCI109732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorli J., Grassino A., Lorange G., Milic-Emili J. Control of breathing in patients with chronic obstructive lung disease. Clin Sci Mol Med. 1978 Mar;54(3):295–304. doi: 10.1042/cs0540295. [DOI] [PubMed] [Google Scholar]
- Thurlbeck W. M. Diaphragm and body weight in emphysema. Thorax. 1978 Aug;33(4):483–487. doi: 10.1136/thx.33.4.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitelaw W. A., Derenne J. P., Couture J., Milic-Emili J. Adaptation of anesthetized men to breathing through an inspiratory resistor. J Appl Physiol. 1976 Sep;41(3):285–291. doi: 10.1152/jappl.1976.41.3.285. [DOI] [PubMed] [Google Scholar]
- ZECHMAN F., HALL F. G., HULL W. E. Effects of graded resistance to tracheal air flow in man. J Appl Physiol. 1957 May;10(3):356–362. doi: 10.1152/jappl.1957.10.3.356. [DOI] [PubMed] [Google Scholar]


