Abstract
Background
The fourth Millennium Development Goals targets reduction by 2/3 the mortality rate of under-fives by 2015. This reduction starts with that of neonatal mortality representing 40% of childhood mortality. In Cameroon neonatal mortality was 31‰ in 2011.
Objectives
We assessed the trends, associated factors and causes of neonatal deaths at the Yaounde Gynaeco-Obstetric and Pediatric Hospital.
Methods
The study was a retrospective chart review. Data was collected from the hospital records, and included both maternal and neonatal variables from 1st January 2004 to 31st December 2010.
Results
The neonatal mortality was 10%. Out-borns represented 49.3% of the deceased neonates with 11.3% born at home. The neonatal mortality rate followed a downward trend dropping from 12.4% in 2004 to 7.2% in 2010. The major causes of deaths were: neonatal sepsis (37.85%), prematurity (31.26%), birth asphyxia (16%), and congenital malformations (10.54%). Most (74.2%) of the deaths occurred within the first week with 35% occurring within 24hours of life. Mortality was higher in neonates with birth weight less than 2500g and a gestational age of less than 37 weeks. In the mothers, it was high in single parenthood , primiparous and in housewives and students.
Conclusion
There has been a steady decline of neonatal mortality since 2004.
Neonatal sepsis, prematurity, birth asphyxia and congenital malformations were the major causes of neonatal deaths. Neonatal sepsis remained constant although at lower rates over the study period.
Keywords: mortality, neonates, referral hospital, Cameroon
Introduction
Every year nearly 40% of all under-five child deaths are newborn babies in their first 28 days of life or the neonatal period. Three quarters of all newborn deaths occur in the first week of life, and between 25% and 45% occur within the first 24 hours1. One of the eight millennium development goals (MDGs) fixed by the United Nations in 2005, was to reduce the mortality rate of children under five by 2/3 by the year 2015.2 Such reduction can only be possible through the reduction of neonatal mortality which represents up to 40% of infantile deaths. The majority of newborn deaths occur in developing countries where access to health care is low. Most of these newborns die at home, without skilled care that could greatly increase their chances for survival3,4.
The gap between developed and developing countries as concerns neonatal mortality remains large. A child born in a developing country is 14 times more likely to die during the first 28 days of life than a baby born in a developed country; with sub-Saharan Africa and South.East Asia carrying the heaviest portions in terms of global neonatal mortality rates5. According to the Demographic Health Surveys of 2004,6 and 20117, the neonatal mortality rates in Cameroon were 29 per 1000 live births, and 31 per 1000 live births respectively.
The neonatal mortality rate being an indicator of the quality of the obstetrical and neonatal care in a setting, its evaluation permits the estimation of the quality of care4,5. The evaluation of the efficacy of preventive measures put into place for the reduction of infant mortality can be done through the evaluation of the neonatal mortality rate over a period of time4. Considering that neonatal mortality rates reflect the quality of obstetrical and neonatal care given to patients in a setting we found it necessary to study this mortality in the Yaounde Gynaeco-Obstetric and Pediatric Hospital (a tertiary hospital in Cameroon, and a reference centre for mother and child care) over a seven year period from 2004 to 2010. The aim of this study was to assess the trends, associated factors and causes of these deaths which will guide interventions to improve outcome.
Methods
Study setting: It was a retrospective, descriptive study covering a period of seven years extending from January 2004 to December 2010 at the neonatology unit of the Yaounde Gynaeco-Obstetric and Pediatric Hospital (YGOPH), which is one of the reference health facilities for mother and child health care in Yaounde, the political capital of Cameroon. It receives patients from Yaounde and other parts of Cameroon, and admissions have increased over the years with the extension of the unit.
The neonatology unit is divided into two sections; one section for preterm infants with 12 incubators and the other section for term neonates with a capacity of 16 cots. The service is taken care of by 2 pediatricians, 1 general practitioner, and 22 nurses together with about 4 auxiliary staff. It receives patients from all over the national territory and the center region in particular.
Inclusion and exclusion criteria: The admission files of all new borns (in-borns and out- borns) who were hospitalized and died in the unit during the study period were studied. The following data was noted: Sex, gestational age, birth weight, place of birth, postnatal age at the time of death, and the final diagnosis retained at the time of death. The maternal variables studied were: age, marital status, parity and prenatal visits.
All neonates who died on arrival or with empty or incomplete files were excluded from the study. We defined in-hospital neonatal mortality rate as the number of deaths occurring among admitted sick neonates over a given period expressed as a percentage4.
Specific mortality rate was defined as the number of neonates who died from a particular pathology divided by the number of neonates admitted for that pathology over a given period4.
Data analysis: The data obtained was analyzed with the SPSS17.0 and Excel 2007 soft ware. The results were expressed as percentages and averages. The Chisquared test was used when necessary to assess significance and statistical significance was at a P value less than 0.05.
Ethical considerations: Authorization to carry out the study, and ethical clearance were obtained from the hospital authorities and the hospital ethics committee.
Results
Mothers' socio-demographic profile: Most of the mothers were at least 30 years of age; with a mean age of 25.38 years (extremes 14–45years); 70% were single, and about 78% were students and housewives (Table 1).
Table 1.
Socio–demographic factors of mothers
| Variables | Number | Percentage |
| Age | ||
| <20 years | 232 | 42.69 |
| 20–30 years | 232 | 43.69 |
| >30 years | 67 | 12.60 |
| Matrimonial status | ||
| Single | 369 | 70 |
| Married | 162 | 30 |
| Profession | ||
| Students/house wives | 413 | 77.8 |
| Liberal profession* | 70 | 13.2 |
| Income earners | 48 | 9.0 |
lawyers, traders, hair dressers, tailors etc
Parity: Mortality was higher in neonates born of primiparous women (54%) against 46% in multiparous women. Concerning prenatal visits, only 25.8% of the mothers had had at least 4 prenatal visits.
Characteristics of the neonates: There were 5828 neonates hospitalized in the neonatal care unit of the YGOPH over the study period; 583 died giving a mortality of 10%. Some 52 files of deceased neonates were excluded because they had incomplete information and could not be exploited, so we finally analyzed 531 records. Out-borns represented 49.3% of the deceased neonates with 11.3% born at home.
The sex distribution of the deceased neonates was 297 males and 232 females giving a sex ratio of 1.27. Concerning gestational ages, 62.43% were born at less than 37 weeks gestation; whereas 64.32% had low birth weights (<2500gms).
Neonates with birth weight less than 2500g and a gestational age less 37 weeks had a significantly higher mortality compared to those delivered at term and with normal birth weights. (Table 2).
Table 2.
Neonatal mortality as a function of birth weight and gestational age (N=527)
| Birth weight Cestational age |
<2500g | 2500–4000g | >4000g | Total | % |
| <37 weeks | 307 | 21 | 1 | 329 | 62.43 |
| >37 weeks | 32 | 156 | 10 | 198 | 37.57 |
| Total (%) | 339(64.32) | 177(33.59) | 11(2.09) | 527(100) | (100) |
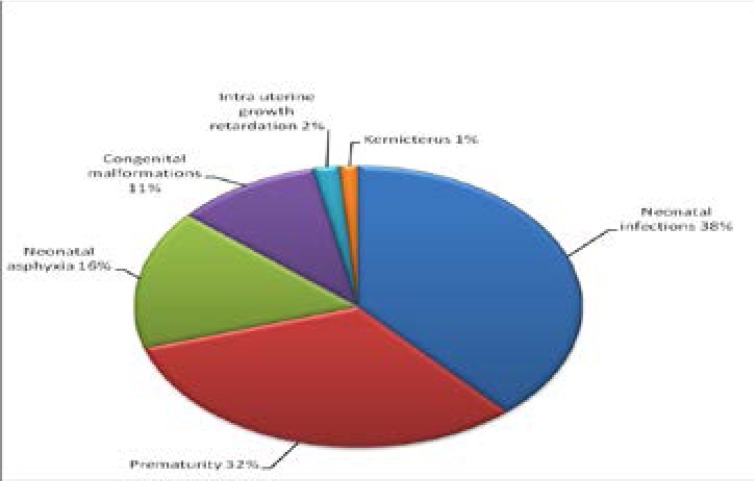
Causes of deaths: The main causes of deaths were: neonatal infections (37.85%), prematurity (31.56%), neonatal asphyxia (16%), and congenital malformations (10.54%) (Figure 1).
Figure 1.
Causes of deaths
Amongst the neonatal infections were 3 cases of neonatal tetanus.
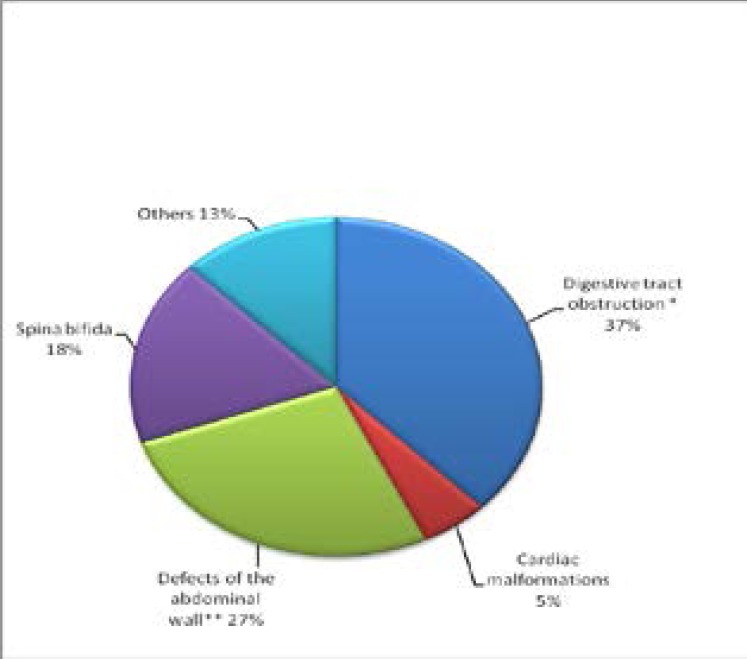
The most frequent congenital malformations were digestive tract obstruction, abdominal wall defects and spina bifida (Figure 2).
Figure 2.
Types of congenital malformations (N=56)
We noted that 74.2% of the deaths occurred within the first week, with 35% occurring within the first 24hours of life.
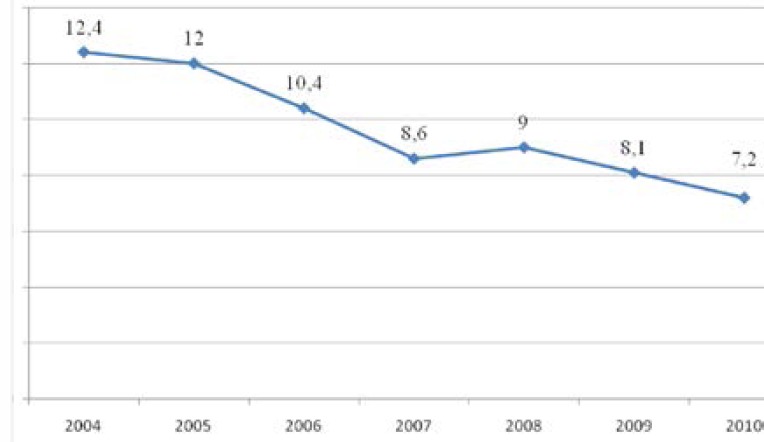
Mortality trends: The neonatal mortality rate followed a steady downward trend from 2004 to 2010 with a slight increase in 2008 (Figure 3).
Figure 3.
Evolution of hospital neonatal mortality from 2004 to 2010
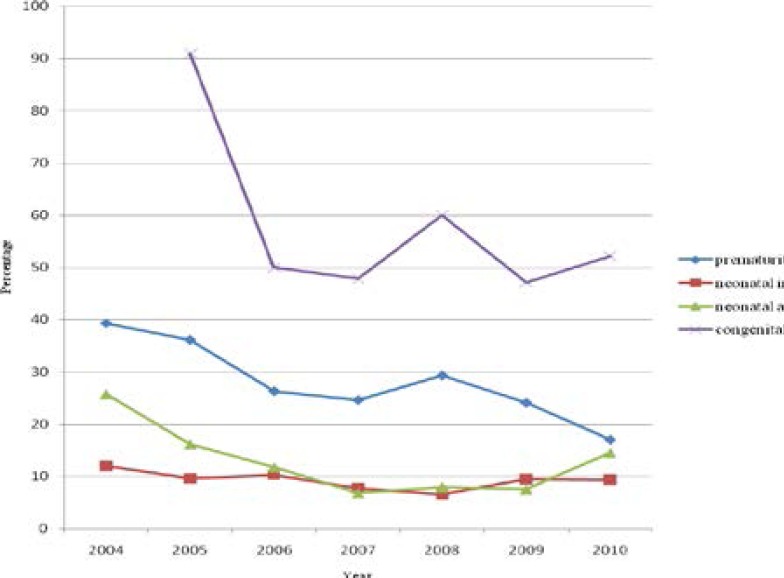
As concerns the trends in the causes of the deaths, we noted that congenital malformations were the most deadly, all through the study period; mortality from prematurity was on the decrease, whereas asphyxia and neonatal infections maintained comparatively low but constant frequencies all through (Figure 4).
Figure 4.
Evolution of mortality due to the principal pathologies from 2004 to 2010.
Discussion
The overall 10% hospital neonatal mortality over the seven year period was much lower than the 30.8% rate recorded by Oladokun et al in Ibadan in 20008, 20.5% recorded by Tietche et al in Yaounde in 19929, and the 17.3% recorded by Eloundou in the same Hospital in 200610. But this was much higher than the 2.25% recorded by Ekure et al in Lagos in 200511. However, Ekure's study involved only in-borns, while the other studies including ours involved both in-borns and out-borns.
The majority of the dead babies were of the male sex with a sex ratio of 1.27. Haon et al, and Ndiaye et al had similar results respectively 1.05 and 1.212,13. These authors found that the male sex was a risk factor for neonatal mortality unlike Chaman et al who did not find any significant difference in mortality rates in both sexes14.
Neonatal mortality was highest in mothers less than 30 years of age . Other authors observed that mortality was highest in neonates from mothers younger than 19 years and older than 35years14,15,16,17. The reasons for the difference are not very clear. In our study 70% of the women were single mothers. These results are in line with those obtained by Eloundou10. It can be hypothesized that the presence of a partner brings along financial, psychological and physical support to an expectant mother and her child. This could be a possible explanation for the more deaths of babies from single mothers. It was noticed that amongst all deceased neonates 74.2% were delivered of women from poorly followed- up pregnancies. This suggests that inadequate follow up of pregnancies is largely responsible for neonatal deaths. Our findings are in line with those of other studies15, 16. The irregular or poor follow up of pregnancies could be due to financial difficulties or simply ignorance and negligence on the part of these women. However it is thought that poverty directly contributes to neonatal mortality translated by the inability to carry out prenatal screening tests, necessary prophylactic measures and attend prenatal clinics.
The neonatal mortality from our study steadily dropped over the years from 12.4% in 2004 to7.2% in 2010. Balaka et al described increasing early neonatal mortality rates in the University Teaching Hospital in Lome Togo from 34,6% in 1981–1982 to 60,5% in 1991–199215, and the evolution has been irregular in the University Teaching Hospital in Dakar ranging from21,8% to 42%18. The steady drop in the mortality rate in our study could be attributed to improvement of the working conditions (increase in the number of personnel and working materials) and regular refresher courses for the personnel of the neonatology unit. The decrease could also be attributed to the fact that there is a minimum package of laboratory investigations for which the parents of the babies pay only on discharge from the hospital. This facilitates investigations (samples are taken from sick neonates and sent to the laboratory analysis, even if the parents are unable to pay on admission), and improves management of the sick neonates.
Most of the neonates (74.2%) died during the early neonatal period. Tietche et al at the Yaounde Central Hospital recorded similar rates 81.49% during the early neonatal period. Authors in other countries found even higher early neonatal mortality rates of up to 91%9,16,18. Thirty five percent of these early neonatal deaths occurred on the first day of life. Our results fall in line with WHO figures which stand between 25 and 45%. These results show that the early neonatal period as the most critical period in the life of a neonate. This is the period of extra uterine adaptation during which the neonate is most likely to develop complications. This therefore implies that neonatal care should be intensified during the first week of life if neonatal mortality is to be significantly reduced.
Neonatal infection was the principal direct cause of neonatal mortality in this hospital with a rate of 38.42%. Tietche et al in Cameroon,9 and Azoumah et al in Togo,19 found similar rates but ours was higher than those from other African authors ranging from 9% to 23.5%18,20,21,22. This is a signal for rigorous hygiene during the prenatal period, delivery and post natal periods for any reduction in infections to be achieved.
Prematurity was the second cause of death in our series. Our results show that, neonates with birth weights lower than 2.5kg and a gestational age of less than 37 weeks had a much higher mortality rate than those born at term with normal weights. Eloundou and Bobossi-Serengbe,10,20 had similar results with 38.9% and 30.7% mortality rates respectively. Many other African researchers have recorded rates ranging from 26% to 38.9%, 8,11,21,22 the highest rate (52.9%) was reported by Diallo17. Low birth weight and prematurity have been identified as risk factors for neonatal mortality by many other researchers9,11,12,21,23,24. Mendes et al in Brazil25 found that preterm neonates were fifty times more at risk of dying than term neonates. Satoshi et al in Japan26 and Velaphi et al in South Africa27 found that low birth weight was a risk factor for mortality. The premature neonate has multiple organ immaturity and therefore faced with difficulties in adaptation to extra uterine life; this coupled with the poor living and working conditions in our country expose the fragile neonate fatal complications like hypothermia, digestive intolerance, infections, bleeding etc..
Neonatal asphyxia was the third most common cause of death in this study. This was contrary to the results obtained by Diallo et al, Tietche et al and Bobossi et al8,9,20 who found asphyxia as the second cause of death after infections. The lower incidence of asphyxia in our series, could be the result of improved management of labour, delivery and early referrals of high- risk pregnancies, from the various refresher courses given to personnel in the delivery room in this context.
This hospital has more incubators than any other hospital in Yaounde and therefore receives premature neonates from all over the region, with most of them arriving in critical states due to poor and inadequate means of transportation. This can probably account for the increased deaths of preterms in this study.
Congenital malformations were responsible for 10.54% of all neonatal deaths in this hospital. Some authors observed lower rates16,18. The main congenital malformations were digestive tract malformations, spina bifida and abdominal wall defects. The very large number of malformations is thought to be due to the fact that the pediatric surgery unit of the hospital attracts referrals from all over the country, and most often late referrals making management more complicated. There is also insufficiency in trained staff in neonatal resuscitation and adequate surgical equipment to handle difficult cases. This further worsened the prognosis of neonates with congenital malformation needing immediate surgery.
Conclusion
Neonatal mortality rate in this health facility has registered a steady decrease from 2004 to 2010. Neonatal sepsis, prematurity, birth asphyxia and congenital malformations were the major causes of neonatal deaths. Health education to pregnant women on adequatefollow up of pregnancies should be reinforced. Health personnel in the delivery room and in the neonatology unit should be continuously trained on the management and prevention of the most frequent causes of deaths in this context, especially neonatal sepsis. The hospital technical platform needs to be reinforced in both material and human resources to manage complex cases with malformations.
Conflict of interest
None
References
- 1.United Nations, author. The Millennium Development Goals Report 2005. New York: 2005. [Google Scholar]
- 2.Organisation Mondiale de la Santé, author. Il faut améliorer les soins aux nouveau-nés pour réduire la mortalité infantile. 2010. [11th November 2010]. (Fre). disponible sur www.who.int.
- 3.Fonds des Nations Unies pour l'Enfance (UNICEF), author La situation des enfants dans le monde 2009-La santé maternelle et néonatale. New York (NY): UNICEF; 2008. (Fre). [Google Scholar]
- 4.WHO, author. Perinatal mortality: A listing of available information. 1996. WHO/FRH/MSM/96.7. p-4.
- 5.Wise PH. Infant mortality/neonatal disease in sexual and reproductive health: A public health perspective. Elservier INC; 2008. pp. 200–2006. [Google Scholar]
- 6.Institut National de la Statistique (INS) et ORC Macro 2004, author. Enquête Démographique et de Santé du Cameroun. Calverton Maryland, USA: INS et ORC Macro; 2004. (Fre). [Google Scholar]
- 7.Institut National de la Statistique (INS) et Macro 2011, author. Enquête Démographique et de Santé et Indicateurs Multiples. EDS-MICS Cameroun; 2011. (Fre). [Google Scholar]
- 8.Oladokun RE, Orimadegun AE, Olodou JA. A ten year review of neonatal deaaths in the special care baby unit at the university college hospital, Ibadan. Niger J Ped. 2004;31(4):119–125. [Google Scholar]
- 9.Tietche F, Kago I, Njimoke A, Mbonda E, Ndombo PK, Tetanye E. Mortalité hospitalière des nouveau-nés eutrophiques à terme à Yaoundé (Cameroun): Aspects étiologiques. Méd Afr Noire. 1998;45:193–195. (Fre). [Google Scholar]
- 10.Eloundou OE. Etiologies et facteurs aggravant la morbidité et la mortalité néonatales à l'Hopital Gynéco- Obstétrique et Pédiatrique de Yaoundé (HGOPY) Thèse de Médecine Faculté de Médecine et de Sciences Biomédicales-Université de Yaoundé I; 2007. (Fre). [Google Scholar]
- 11.Ekure EN, Ezeaka VC, Iroha EO, Egri-Okwaji MTC. Neonatal mortality of In-borns in the neonatal unit of a tertiary centre in Lagos, Nigeria. Nig Quart J Hosp Med. 2005;15(2):55–58. [Google Scholar]
- 12.Haon PT, Bao TV, Phong DN, Huong NT, Lazare M, Boelaert M. Mortalité néonatale précoce à l'Hopital de gynécologie-obstétrique de Hanoi,Vietnam. Bull Soc Pathol Exot. 2000;93:62–65. (Fre). [PubMed] [Google Scholar]
- 13.Ndiaye O, Sall G, Diagne I, Diouf S, Kuakuvi N. morbidité et mortalité néonatales au centre hospitalier Abass Ndao de Dakar (Senegal) Arch Pediatr. 2001;8:1019–1022. [Google Scholar]
- 14.Chaman R, Naieni KH, Golestan B, Nabavizadeh H, Yunesian M. Neonatal mortality risk factors in a rural part of Iran: a nested case-control study. Iran J Publ Health. 2009;38:48–52. [Google Scholar]
- 15.Balaka B, Agbere A, Kpemissi E, Baeta S, Kessie K, Assimadi K. Evolution de la mortalité neonatale précoce en dix ans (1981-82 & 1991-92) au CHU de lome : quelle politique de santé néonatale pour demain? Méd Afr Noire. 1998;45:430–434. (Fre). [Google Scholar]
- 16.Diallo S, Kourouma S, Camara Y. Mortalité neonatale à l'institut de nutrition et de santé de l'enfant (INSE) Méd Afr Noire. 1998;45:326–329. (Fre). [Google Scholar]
- 17.World Health Organisation, author. Neonatal and Perinatal Mortality: Country, regional and global estimates 2004. WHO library cataloguing-in-publication data; 2007. [Google Scholar]
- 18.Cissé CT, Yacoubou Y, Ndiaye O, Diop-Mbengue R, Moreau J-C. Evolution de la mortalité néonatale précoce entre 1994 et 2003 au CHU de Dakar. J Gynecol Obstet Biol Reprod. 2006;35:46–52. doi: 10.1016/s0368-2315(06)76371-2. [DOI] [PubMed] [Google Scholar]
- 19.Azoumah KD, Balaka B, Aboubakari AS, Matey K, Youlou A, Agbere AD. Morbidité et mortalité néonatales au CHU Kara (Togo) Méd Afr Noire. 2010;57:109–112. [Google Scholar]
- 20.Bobossi-serengbe G, Deyamissi TSS, Diemer HC, Gaudueille A, Gresenguet G, Mandaba JL, et al. Morbidité et mortalité néonatales au complexe pédiatrique de Bangui (Centrafrique) Méd Afr Noire. 2004;5103:159–163. (Fre). [Google Scholar]
- 21.Simiyu DE. morbidity and mortality of neonates admitted in general pediatric wards at the Kenyatta national hospital. E Afr Med J. 2003;80(12):661–666. doi: 10.4314/eamj.v80i12.8776. [DOI] [PubMed] [Google Scholar]
- 22.Ogunlesi TA, Ogufowora OB, Adekanmbi AF, Fetuga MB, Runsewe-Abiodun TL, Oyundeyi MM. Neonatal mortality at the Olabussi Onabanjo Hospital Sagamu. Niger J Ped. 2006;33(2):40–46. [Google Scholar]
- 23.Djadou K-E, Azouma D, Yable G, Dakey G, Sanda P, Dokounor D, et al. Mortalité néonatale au centre hospitalier régional de Tsévié (Togo) Arch Pediatr. 2006;13:1156–1159. doi: 10.1016/j.arcped.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 24.Monebenimp F, Tchiro R, Nana AD. Morbidité et mortalité des naissances intra- hospitalières du Centre Hospitalier Universitaire de Yaoundé, Cameroun. Clin Mother Child Heath. 2005;2:355–358. [Google Scholar]
- 25.Mendes KG, Anselmo Olinto MT, DiasdaCosta JS. Case-control study on infant mortality in Southern Brazil. Rev Saúde Pública. 2006;40(2):240–248. doi: 10.1590/s0034-89102006000200009. (Fre). [DOI] [PubMed] [Google Scholar]
- 26.Satoshi K, Masanori F, Izumi S, Hiofumi A, Kazuhiko K, Yasufumi H, et al. Morbidity and mortality of infants with very low birth weight in Japan: Center variation. Pediatrics. 2006;118:e 1130. doi: 10.1542/peds.2005-2724. [DOI] [PubMed] [Google Scholar]
- 27.Velaphi SC, Mokhachane M, Mphahlele RM, Beckh-Arnold E, Kuwanda ML, Cooper PA. Survival of very low birh weight infants according to birth weight and gestational age in a public hospital. S Afr Med J. 2005;95:504–509. [PubMed] [Google Scholar]