Abstract
Pulmonary hypertension is associated with advanced chronic obstructive pulmonary disease (COPD), although pulmonary vascular changes occur early in the course of the disease. Pulmonary artery (PA) enlargement (PAE) measured by computed tomography correlates with pulmonary hypertension and COPD exacerbation frequency. Genome-wide association studies of PAE in subjects with COPD have not been reported. To investigate whether genetic variants are associated with PAE within subjects with COPD, we investigated data from current and former smokers from the COPDGene Study and the Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints study. The ratio of the diameter of the PA to the diameter of the aorta (A) was measured using computed tomography. PAE was defined as PA/A greater than 1. A genome-wide association study for COPD with PAE was performed using subjects with COPD without PAE (PA/A ≤ 1) as a control group. A secondary analysis used smokers with normal spirometry as a control group. Genotyping was performed on Illumina platforms. The results were summarized using fixed-effect meta-analysis. Both meta-analyses revealed a genome-wide significant locus on chromosome 15q25.1 in IREB2 (COPD with versus without PAE, rs7181486; odds ratio [OR] = 1.32; P = 2.10 × 10−8; versus smoking control subjects, rs2009746; OR = 1.42; P = 1.32 × 10−9). PAE was also associated with a region on 14q31.3 near the GALC gene (rs7140285; OR = 1.55; P = 3.75 × 10−8). Genetic variants near IREB2 and GALC likely contribute to genetic susceptibility to PAE associated with COPD. This study provides evidence for genetic heterogeneity associated with a clinically important COPD vascular subtype.
Keywords: chronic obstructive pulmonary disease, genome-wide association, pulmonary hypertension, subtyping
Clinical Relevance
Our study is the first genome-wide association study of pulmonary artery enlargement (PAE) associated with chronic obstructive pulmonary disease (COPD). PAE is usually observed in advanced COPD, and it is also a significant predictor of COPD exacerbations. We have found that genetic variants near IREB2 and GALC are associated with susceptibility to PAE within subjects with COPD. This study suggests that a clinically important vascular subtype of COPD is closely linked to genetic heterogeneity.
Chronic obstructive pulmonary disease (COPD) is characterized by the progressive development of airflow limitation that is not fully reversible and marked phenotypic heterogeneity. COPD was the third leading cause of mortality in the United States in 2010 (1). Although COPD susceptibility is mainly attributable to cigarette smoking, not all heavy smokers develop COPD for reasons that are still unclear, but likely involve differences in genetic backgrounds (2–5).
Pulmonary hypertension (PH), a well established complication of COPD, is one of the most common forms of secondary PH (6). Typically, PH is associated with severe airflow limitation and chronic hypoxemia. However, there is a poor correlation between lung function parameters and pulmonary artery (PA) pressures, suggesting that factors other than airway obstruction may play a role in its etiology. Recent studies have reported that a proportion of patients with only moderate airflow limitation have severe PH (7, 8), which has been termed “disproportionate” PH. This subgroup has been suggested as a distinct phenotype, which may benefit from a different therapeutic approach, such as selective vasodilators (6–8). Furthermore, pulmonary vascular changes occur early in the course of COPD (9), and patients with COPD without resting PH frequently have exercise-induced PH (10). PH in COPD is associated with decreased survival (11–14). The ratio of the diameter of the PA to the diameter of the aorta (A) can be measured by computed tomography (CT), which correlates with PA pressure gauged by right heart catheterization (15–18). Recently, Wells and colleagues (19) demonstrated that PA/A greater than 1 was associated with COPD exacerbation frequency.
Although variants in several genes have been identified in association with Mendelian or near-Mendelian forms of PA hypertension, genetic risk factors for PH in COPD have not been well studied. A genome-wide association study (GWAS) of PA enlargement (PAE) within subjects with COPD has not been reported. We hypothesized that genetic susceptibility to PAE would differ among subjects with COPD. We addressed this hypothesis by comparing subjects with COPD with PA/A greater than 1 measured by CT to subjects with COPD with PA/A of 1 or less as a control group, as well as to smoking control subjects.
Materials and Methods
Study Cohorts
Subjects were current and former smokers from two studies: the COPDGene (Genetic Epidemiology of COPD) Study (NCT00608764, www.copdgene.org), and ECLIPSE (Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints; NCT00292552; www.eclipse-copd.com). Study design and details of each study have been previously published (20, 21). Subjects in COPDGene were either self-identified non-Hispanic white (NHW) or African American (AA), and those included from ECLIPSE were of white European ancestry.
Measurement of the Diameters of the PA and Aorta
An investigator who was unaware of the subjects’ clinical or genetic characteristics measured vascular diameters from axial images of baseline chest CT scans in the COPDGene and ECLIPSE cohorts by using inspiratory acquisitions with Digital Imaging and Communications in Medicine software (OsiriX DICOM Viewer, version 4.0, 32-bit; www.osirix-viewer.com), as previously described (19). The interpreter measured the diameter of the main PA at the level of its bifurcation and the diameter of the ascending aorta (A) by averaging two measurements taken 90° apart in its maximum dimension using the same images, and then a ratio of PA to A (PA/A) was calculated. The interobserver κ was 0.75 (95% confidence interval = 0.67–0.82) and intraobserver κ was 0.92 (95% confidence interval = 0.83–1.0) (19).
Variable Definitions
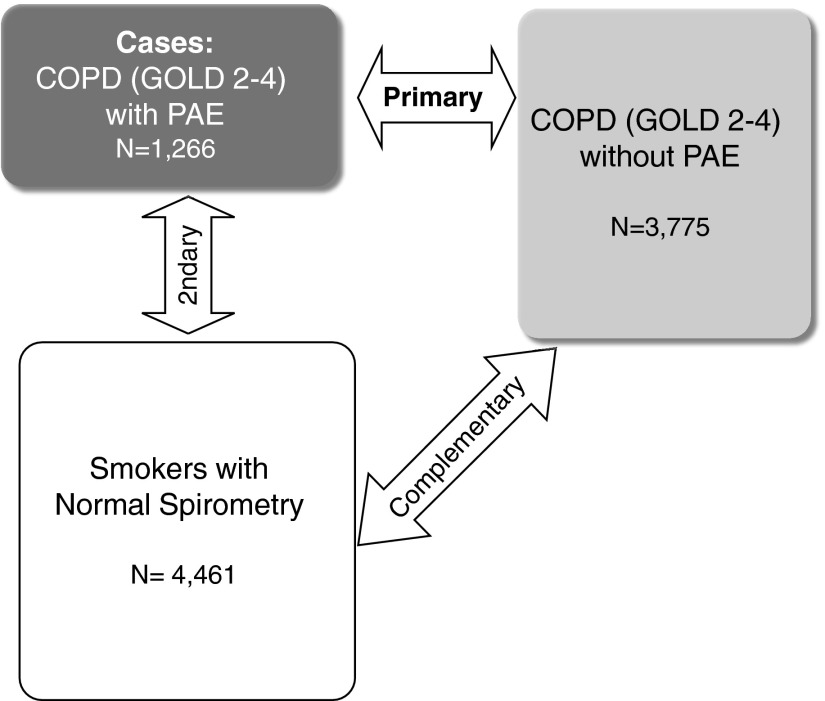
PAE was defined as PA/A measured by CT greater than 1. COPD cases with PAE were defined as having both PA/A greater than 1 and COPD severity of at least spirometry grade 2 (post-bronchodilator forced expiratory volume at 1 s [FEV1]/forced vital capacity < 0.7 and FEV1 < 80% predicted), defined by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) (22). For COPD cases with PAE, primary analysis was performed using subjects with COPD (GOLD 2–4) but no PAE (PA/A ≤ 1) as control subjects to explore genetic heterogeneity within subjects with COPD. The secondary analyses used current or former smokers with normal spirometry (post-bronchodilator FEV1/forced vital capacity ≥ 0.7 and FEV1 ≥ 80% predicted) as a control group. In addition, we performed GWAS of subjects with COPD without PAE relative to smoking control subjects for comparison to our results in subjects with COPD with PAE (Figure 1).
Figure 1.
Genome-wide association study design for subjects with chronic obstructive pulmonary disease (COPD) with a ratio of pulmonary artery (PA) diameter to aorta (A) diameter greater than 1. GOLD (Global Initiative for Chronic Obstructive Lung Disease) 2–4 was defined as having a post-bronchodilator forced expiratory volume at 1 second (FEV1)/forced vital capacity (FVC) less than 0.7 and FEV1 less than 80% predicted. Normal spirometry was defined as a post-bronchodilator FEV1/FVC of 0.7 or greater and an FEV1 of 80% predicted or greater. PAE, PA enlargement.
Genotyping Quality Control and Imputation
Illumina platforms (HumanOmniExpress for the COPDGene cohort and HumanHap 550V3 for the ECLIPSE cohort; Illumina, Inc., San Diego, CA) were used for genotyping. Details of genotyping and imputation quality control have been previously published (23) and are described in the online supplement. Briefly, we performed imputation on the COPDGene cohorts using MaCH (24) and minimac (25) using 1,000 Genomes (26) Phase I v3 European and cosmopolitan reference panels for the NHWs and AAs, respectively (23). Previous studies have described details on genotyping quality control and imputation for the ECLIPSE cohort (27–29). Variants passing genotyping or imputation quality control in all cohorts were included for analysis.
Statistical Analysis
We performed logistic regression analysis of single-nucleotide polymorphisms (SNPs) under an additive model of inheritance with affection status in each cohort with adjustment for age, sex, pack-years of cigarette smoking, and genetic ancestry–based principal components using PLINK 1.07 (30), as previously described (27, 29). Complementary analysis included post-bronchodilator FEV1 % predicted and/or exacerbation frequency as adjustment variables. Imputed genotypes were analyzed in a similar manner using SNP dosage data in PLINK 1.07 (30). Separate analyses were performed in COPDGene NHWs, COPDGene AAs, and ECLIPSE European ancestry subjects. Fixed-effects meta-analysis (31) was undertaken using METAL (version 2011-3-25) (32) and R 2.15.1 (www.r-project.org) with the meta-package. We evaluated heterogeneity by calculating both I2 (33) and P values for Cochran’s Q. I2 describes the percentage of total variation across studies that is due to heterogeneity rather than chance. I2 = 100%×(Q − df)/Q, where Q is Cochran's heterogeneity statistic and df the degrees of freedom. Genomic inflation factors (34) were calculated using GenABEL (35). Regional association plots were generated using LocusZoom (36), with linkage disequilibrium (LD) calculated using the 1,000 Genomes European reference data.
To evaluate differences of odds ratios (ORs) for previously known genome-wide significant SNPs between two different meta-analyses, permutation testing was performed. For each cohort, we randomly reassigned the phenotypes (COPD with or without PAE) of each individual to another individual in the dataset. Each random reassignment of the data represented one possible sampling of individuals under the null hypothesis, and this process was repeated a predefined number of times (N) to generate an empirical distribution with resolution N. Logistic regression was performed, and the results were combined using meta-analysis. We repeated this procedure 10,000 times to obtain the null distribution of differences of effect sizes. Our baseline difference of effect size for each SNP between two meta-analyses was compared with the permutation results, which was described by the null distribution to obtain a P value.
To search other SNPs independently associated with COPD with PAE, we also performed region-based conditional analyses using logistic regression, adjusting for the most significant (lead) SNP in each genome-wide significant region using genotyped or dosage data, as appropriate. All SNPs within a 250-kb window on either side of the lead SNP were tested for association with COPD with PAE. For region-based analyses conditional on the top SNP, a threshold of P less than 5 × 10−4 was considered significant to reflect an approximate adjustment for a 500-kb interval (23, 29).
Results
A total of 1,266 subjects with COPD with PAE, 3,775 subjects with COPD without PAE, and 4,461 smokers with normal spirometry from the combined COPDGene and ECLIPSE cohorts passed quality control and were not outliers by genetic ancestry. Table 1 shows baseline characteristics for these subjects.
Table 1.
Baseline Characteristics of Subjects with Chronic Obstructive Pulmonary Disease, Stratified by Pulmonary Artery:Ascending Aorta Ratio Values, and Smokers with Normal Spirometry
| COPDGene NHWs |
COPDGene AAs |
ECLIPSE |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| COPD |
COPD |
COPD |
|||||||
| Characteristics | PA/A > 1 | PA/A ≤ 1 | Control Subjects | PA/A > 1 | PA/A ≤ 1 | Control Subjects | PA/A > 1 | PA/A ≤ 1 | Control Subjects |
| n | 535 | 2,128 | 2,534 | 260 | 494 | 1,749 | 471 | 1,153 | 178 |
| Age, yr | 64.2 (8.4) | 64.8 (8.1) | 59.5 (8.7) | 59.3 (8.1) | 58.7 (8.1) | 52.8 (6.0) | 63.7 (7.2) | 63.7 (7.0) | 57.5 (9.4) |
| Sex, % male | 42.1 | 59.1 | 49.3 | 40.0 | 62.6 | 58.1 | 62.2 | 67.1 | 57.9 |
| Pack-years | 54.6 (25.1) | 56.8 (28.6) | 37.8 (20.3) | 41.0 (22.3) | 43.3 (23.0) | 36.4 (20.1) | 47.8 (24.4) | 51.9 (28.6) | 32.1 (24.8) |
| Current smoker, % | 27.3 | 36.7 | 39.6 | 52.3 | 65.8 | 87.4 | 31.4 | 36.4 | 40.1 |
| FEV1 % predicted | 45.5 (17.4) | 50.8 (17.9) | 96.8 (11.0) | 47.1 (18.0) | 55.1 (16.7) | 98.4 (12.2) | 43.2 (14.8) | 49.5 (15.6) | 107.9 (13.7) |
| Spirometry grade, %* | |||||||||
| GOLD 2 | 41.3 | 53.5 | 46.2 | 62.8 | 29.8 | 46.8 | |||
| GOLD 3 | 37.2 | 30.7 | 33.1 | 28.1 | 50.0 | 41.3 | |||
| GOLD 4 | 21.5 | 15.8 | 20.8 | 9.1 | 20.2 | 11.9 | |||
| PA, cm | 3.3 (0.4) | 2.7 (0.4) | — | 3.3 (0.4) | 2.8 (0.4) | — | 3.5 (0.5) | 2.9 (0.4) | — |
| A, cm | 3.1 (0.3) | 3.3 (0.4) | — | 3.1 (0.4) | 3.2 (0.4) | — | 3.2 (0.4) | 3.4 (0.4) | — |
| PA/A | 1.07 (0.08) | 0.84 (0.10) | — | 1.09 (0.10) | 0.88 (0.09) | — | 1.10 (0.10) | 0.85 (0.10) | — |
| Exacerbation frequency per year | 1.32 (1.52) | 0.61 (1.10) | 1.06 (1.41) | 0.47 (1.04) | 1.14 (1.34) | 0.73 (1.16) | |||
Definition of abbreviations: AA, African American; COPD, chronic obstructive pulmonary disease; COPDGene, Genetic Epidemiology of COPD Study; ECLIPSE, Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints; FEV1, forced expiratory volume at 1 second; GOLD, Global Initiative for Chronic Obstructive Lung Disease; NHW, non-Hispanic white; PA/A, ratio of the diameter of the main pulmonary artery (PA) at the level of its bifurcation and the diameter of the ascending aorta (A) in its maximum dimension measured by computed tomography.
Data are presented as mean (SD) or percentage, as appropriate.
For subjects with post-bronchodilator FEV1/forced vital capacity < 0.7; GOLD 2 = FEV1 ≥ 50% predicted and <80% predicted; GOLD 3 = FEV1 ≥ 30% predicted and <50% predicted; GOLD 4 = FEV1 < 30% predicted.
GWAS of Subjects with COPD with PAE Relative to Those without PAE
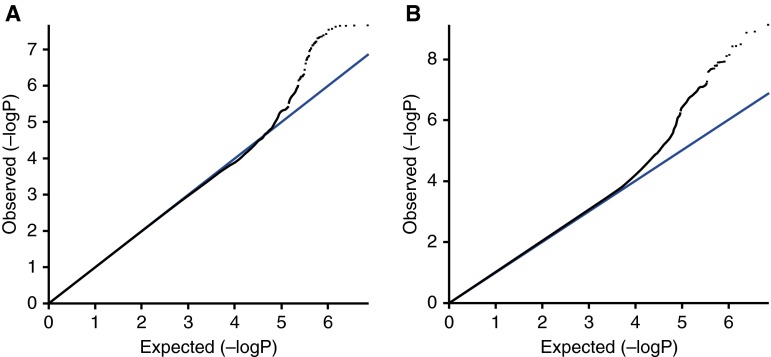
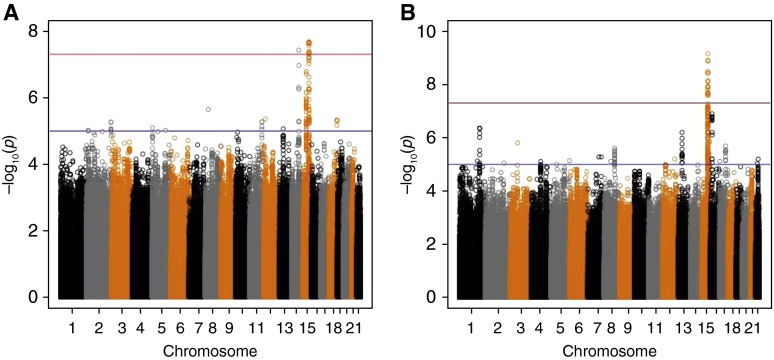
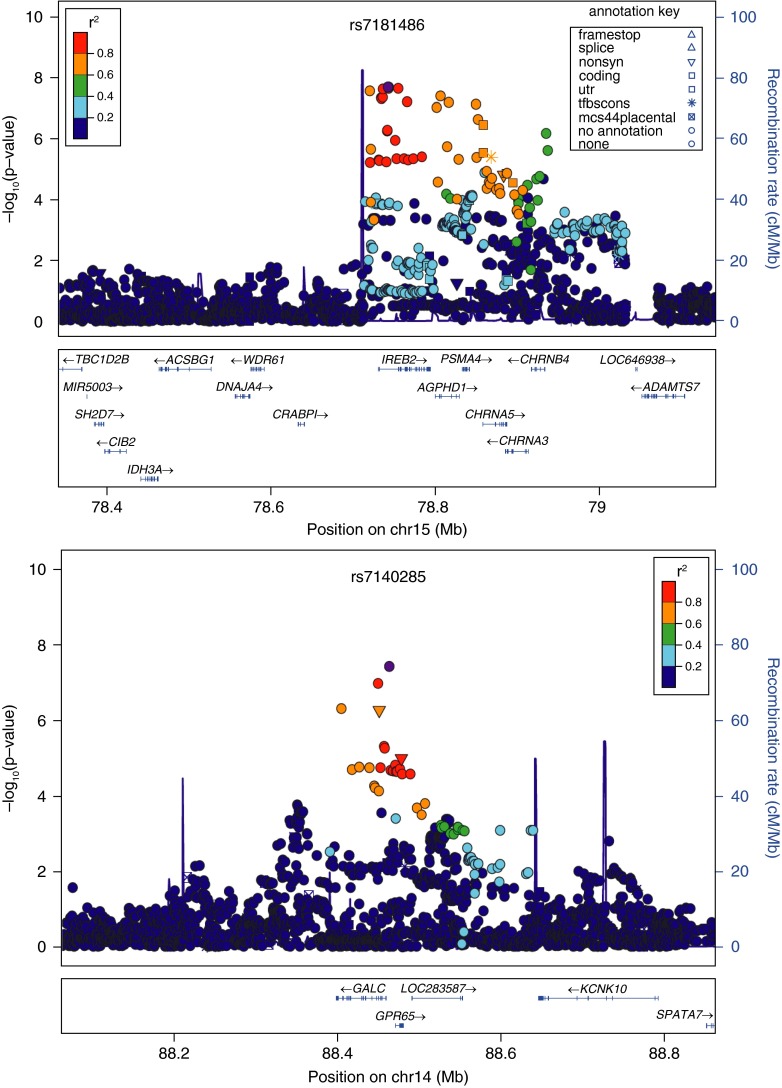
Our primary association analysis on the presence or absence of PAE (defined by CT measurement of PA/A > 1 versus ≤1) included 1,266 subjects with COPD with PAE and 3,775 subjects with COPD without PAE. The quantile–quantile plot showed no evidence of significant population stratification (Figure 2A; λ = 1.00). Figure 3A shows genome-wide significant associations on chromosomes 15q25.1 and 14q31.3. The most significantly associated SNP was rs7181486 on 15q25.1 with a meta-analysis P value of 2.10 × 10−8 and OR of 1.32, located within the iron-responsive element–binding protein 2 gene (IREB2). (Table 2 and Figure 4). All of the genome-wide significant SNPs on 15q25.1 were in strong LD (r2 > 0.6) with the previously described lead COPD risk SNP, rs11858836, near IREB2 (29).
Figure 2.
The quantile–quantile plots (black) for the meta-analysis including 1,000 Genomes project imputed data of (A) subjects with COPD with PAE (PA/A > 1) versus those without PAE (PA/A ≤ 1), and (B) subjects with COPD with PAE versus smokers with normal spirometry, after adjustment for age, sex, pack-years of cigarette smoking, and genetic ancestry using principal components. The reference lines (blue) show the values where the observed (−logP) is equal to the expected (−logP).
Figure 3.
Manhattan plots of –log10 P for the meta-analysis including 1,000 Genomes project imputed data of (A) subjects with COPD with PAE (PA/A > 1) versus those without PAE (PA/A ≤ 1), and (B) subjects with COPD with PAE versus smokers with normal spirometry, after adjustment for age, sex, pack-years of cigarette smoking, and genetic ancestry using principal components.
Table 2.
Top Results of the Genome-Wide Association Study for Subjects with Chronic Obstructive Pulmonary Disease with a Pulmonary Artery:Ascending Aorta Ratio Greater Than 1 versus Those with a Pulmonary Artery:Ascending Aorta Ratio of 1 or Less in the Cohorts of COPDGene Non-Hispanic Whites, COPDGene African Americans, and ECLIPSE Studies*
| Locus | Nearest Gene | SNP | Risk Allele | FRQ |
COPDGene NHW |
COPDGene AA |
ECLIPSE |
Overall |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EUR† | AA | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | I2 | Q | ||||
| 15q25.1 | IREB2 | rs7181486 | C | 0.39 | 0.24 | 1.22‡ (1.06–1.40) | 5.62 × 10−3 | 1.58‡ (1.23–2.04) | 3.53 × 10−4 | 1.36‡ (1.16–1.60) | 1.40 × 10−4 | 1.32 (1.20–1.45) | 2.10 × 10−8 | 43.6 | 0.17 |
| 15q25.1 | IREB2 | rs56219465 | G | 0.39 | 0.24 | 1.22‡ (1.06–1.40) | 5.64 × 10−3 | 1.59‡ (1.23–2.04) | 3.55 × 10−4 | 1.36‡ (1.16–1.60) | 1.40 × 10−4 | 1.32 (1.20–1.45) | 2.12 × 10−8 | 43.6 | 0.17 |
| 15q25.1 | IREB2 | rs17483929 | A | 0.38 | 0.23 | 1.21 (1.06–1.39) | 5.85 × 10−3 | 1.59 (1.23–2.04) | 3.51 × 10−4 | 1.36‡ (1.16–1.60) | 1.40 × 10−4 | 1.32 (1.20–1.45) | 2.24 × 10−8 | 44.2 | 0.17 |
| 15q25.1 | IREB2 | rs2009746 | G | 0.39 | 0.22 | 1.21‡ (1.06–1.39) | 6.15 × 10−3 | 1.62‡ (1.25–2.10) | 2.58 × 10−4 | 1.36‡ (1.16–1.60) | 1.49 × 10−4 | 1.32 (1.20–1.45) | 2.25 × 10−8 | 49.9 | 0.14 |
| 15q25.1 | IREB2 | rs72738718 | C | 0.39 | 0.24 | 1.22‡ (1.06–1.40) | 5.90 × 10−3 | 1.57‡ (1.22–2.02) | 4.37 × 10−4 | 1.37‡ (1.16–1.60) | 1.33 × 10−4 | 1.32 (1.20–1.45) | 2.37 × 10−8 | 41.1 | 0.18 |
| 15q25.1 | IREB2 | rs72736802 | T | 0.39 | 0.48 | 1.25‡ (1.08–1.45) | 3.52 × 10−3 | 1.38‡ (1.10–1.72) | 5.67 × 10−3 | 1.44‡ (1.20–1.71) | 5.77 × 10−5 | 1.34 (1.21–1.48) | 2.72 × 10−8 | 0 | 0.48 |
| 14q31.3 | GALC | rs7140285 | T | 0.08 | 0.12 | 1.51‡ (1.20–1.89) | 4.20 × 10−4 | 1.68‡ (1.19–2.37) | 3.12 × 10−3 | 1.53‡ (1.17–2.01) | 2.21 × 10−3 | 1.55 (1.33–1.81) | 3.75 × 10−8 | 0 | 0.87 |
| 15q25.1 | AGPHD1 | rs8034191 | C | 0.39 | 0.17 | 1.23 (1.08–1.41) | 2.70 × 10−3 | 1.66 (1.25–2.20) | 4.60 × 10−4 | 1.33 (1.13–1.56) | 4.49 × 10−4 | 1.31 (1.19–1.45) | 4.06 × 10−8 | 42.2 | 0.18 |
| 15q25.1 | IREB2 | rs55983731 | T | 0.39 | 0.24 | 1.21‡ (1.06–1.39) | 6.47 × 10−3 | 1.54‡ (1.19–1.98) | 9.01 × 10−4 | 1.36‡ (1.16–1.60) | 1.38 × 10−4 | 1.31 (1.19–1.44) | 4.39 × 10−8 | 33.1 | 0.22 |
| 15q25.1 | IREB2 | rs17483686 | T | 0.39 | 0.24 | 1.21‡ (1.05–1.39) | 6.72 × 10−3 | 1.53‡ (1.19–1.98) | 9.50 × 10−4 | 1.36‡ (1.16–1.60) | 1.38 × 10−4 | 1.31 (1.19–1.44) | 4.74 × 10−8 | 33.0 | 0.22 |
| 15q25.1 | IREB2 | rs17483721 | C | 0.38 | 0.23 | 1.21 (1.05–1.39) | 6.74 × 10−3 | 1.53 (1.19–1.97) | 9.81 × 10−4 | 1.36‡ (1.16–1.60) | 1.38 × 10−4 | 1.31 (1.19–1.44) | 4.90 × 10−8 | 32.7 | 0.23 |
Definition of abbreviations: AA, African American; CI, confidence interval; COPDGene, Genetic Epidemiology of COPD Study; ECLIPSE, Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints; EUR, European white; FRQ, risk allele frequency; I2, percentage of the variability in effect estimates due to heterogeneity; NHW, non-Hispanic white; OR, odds ratio; Q, P values for Cochran's Q test; SNP, single-nucleotide polymorphism.
Adjusted for age, sex, pack-years of cigarette smoking, and genetic ancestry, as summarized in the principal components.
EUR frequency data are from the meta-analysis of COPDGene NHW and ECLIPSE.
Imputed genotypes.
Figure 4.
Local association plots for genome-wide significant loci in the meta-analysis of subjects with COPD with PA/A greater than 1 versus subjects with COPD with PA/A of 1 or lower in COPDGene (Genetic Epidemiology of COPD) non-Hispanic whites (NHWs), African Americans (AAs), and ECLIPSE (Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints). The x axis is chromosomal position, and the y axis shows the –log10 P value. The most significant single-nucleotide polymorphism (SNP) at each locus is labeled in purple, with other SNPs colored by degree of linkage disequilibrium (LD; r2). Plots were created using LocusZoom.
We identified one novel additional locus on 14q31.3 near the GALC gene encoding galactosylceramidase; the top SNP at this locus was rs7140285, with a P value of 3.75 × 10−8. It was in strong LD (r2 = 0.68) with rs1805078, which is a missense SNP of GALC (P = 5.49 × 10−7).
Because of a significant difference of mean FEV1 % predicted between subjects with COPD with PAE and those without PAE (Table 1), we performed an additional meta-analysis including FEV1 % predicted as an adjustment variable (see Figure E1 in the online supplement). The results of the top SNPs (P < 1 × 10−6) are shown in Table E1. The significance of rs7181486 was reduced to 5.58 × 10−7 and the significance of rs7140285 was reduced to 1.50 × 10−7. Thus, adjustment for COPD severity, as captured by FEV1, attenuated but did not remove the IREB2 and GALC associations with PAE.
Because subjects with COPD with PAE and those without PAE showed different exacerbation frequency (Table 1), an additional meta-analysis including exacerbation frequency per year as an adjustment variable was performed (Figure E2). Although the significance of rs7181486 was increased to 6.68 × 10−9, rs7140285 was reduced to 1.87 × 10−7 (Table E2). An additional meta-analysis including adjustment for both FEV1 and exacerbation frequency showed slightly reduced significance of these two SNPs, rs718146 (P = 9.20 × 10−8) and rs7140285 (P = 5.33 × 10−7) (Figure E3 and Table E3).
GWAS of Subjects with COPD with PAE Relative to Smokers with Normal Spirometry
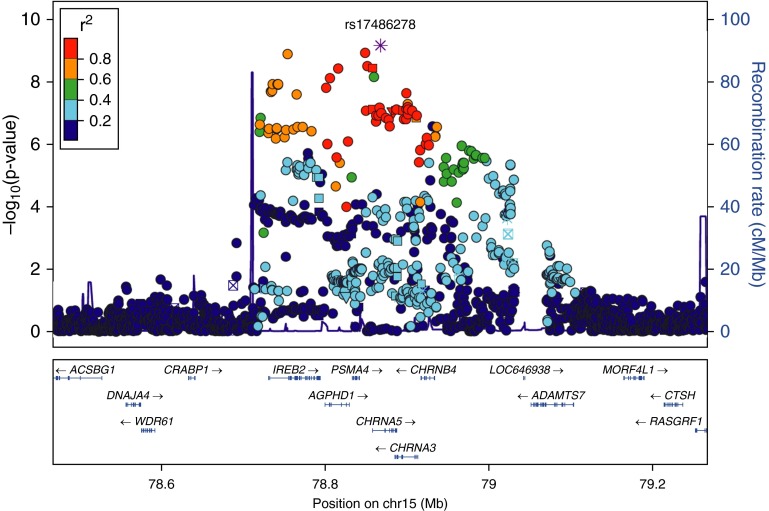
A GWAS of PAE associated with COPD (GOLD 2–4) included the same number of cases and 4,461 smokers with normal spirometry as a control group (Table 1). Figure 2B shows a corresponding quantile–quantile plot (lambda = 1.02). A genome-wide significant locus was identified on chromosome 15q25.1 (Figure 3B), and this locus includes five genes, which were cholinergic receptor, nicotinic, α 5 (neuronal) (CHRNA5), proteasome (prosome, macropain) subunit, α type, 4 (PSMA4), IREB2, aminoglycoside phosphotransferase domain containing 1 (AGPHD1), and cholinergic receptor, nicotinic, α 3 (neuronal) (CHRNA3) (Table 3 and Figure 5). The top SNP was rs17486278 (OR = 1.42; P = 6.93 × 10−10) and located within CHRNA5. These genome-wide significant SNPs were either identical to, or in strong LD (r2 ≥ 0.80) with, SNPs previously discovered in GWASs of COPD susceptibility (23, 37, 38).
Table 3.
Top Results of the Genome-Wide Association Study for Subjects with Chronic Obstructive Pulmonary Disease with a Pulmonary Artery:Ascending Aorta Ratio Greater Than 1 versus Smokers with Normal Spirometry in the Cohorts of COPDGene Non-Hispanic Whites, COPDGene African Americans, and ECLIPSE Studies*
| Locus | Nearest Gene | SNP | Risk Allele | FRQ |
COPDGene NHW |
COPDGene AA |
ECLIPSE |
Overall |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EUR† | AA | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | I2 | Q | ||||
| 15q25.1 | CHRNA5 | rs17486278 | C | 0.37 | 0.29 | 1.43‡ (1.23–1.65) | 2.05 × 10−6 | 1.54‡ (1.24–1.91) | 9.26 × 10−5 | 1.22‡ (0.92–1.62) | 1.69 × 10−1 | 1.42 (1.27–1.59) | 6.93 × 10−10 | 0 | 0.43 |
| 15q25.1 | PSMA4 | rs58365910 | C | 0.38 | 0.26 | 1.43‡ (1.24–1.66) | 1.82 × 10−6 | 1.51‡ (1.20–1.88) | 3.55 × 10−4 | 1.25‡ (0.94–1.67) | 1.21 × 10−1 | 1.42 (1.27–1.59) | 1.21 × 10−9 | 0 | 0.61 |
| 15q25.1 | IREB2 | rs2009746 | G | 0.37 | 0.21 | 1.38‡ (1.20–1.60) | 1.30 × 10−5 | 1.59‡ (1.26–2.00) | 8.33 × 10−5 | 1.32‡ (0.99–1.75) | 5.82 × 10−2 | 1.42 (1.27–1.59) | 1.32 × 10−9 | 0 | 0.52 |
| 15q25.1 | CHRNA5 | rs2036527 | A | 0.38 | 0.23 | 1.44 (1.24–1.67) | 1.05 × 10−6 | 1.43 (1.14–1.79) | 1.93 × 10−3 | 1.25‡ (0.94–1.67) | 1.23 × 10−1 | 1.41 (1.26–1.57) | 3.15 × 10−9 | 0 | 0.69 |
| 15q25.1 | CHRNA5 | rs55781567 | G | 0.37 | 0.28 | 1.44‡ (1.24–1.67) | 1.22 × 10−6 | 1.42‡ (1.14–1.78) | 1.94 × 10−3 | 1.25‡ (0.94–1.66) | 1.25 × 10−1 | 1.40 (1.25–1.57) | 3.68 × 10−9 | 0 | 0.69 |
| 15q25.1 | AGPHD1 | rs8031948 | T | 0.38 | 0.17 | 1.43‡ (1.23–1.65) | 1.89 × 10−6 | 1.51‡ (1.17–1.94) | 1.36 × 10−3 | 1.27‡ (0.95–1.68) | 1.03 × 10−1 | 1.42 (1.26–1.59) | 3.74 × 10−9 | 0 | 0.65 |
| 15q25.1 | CHRNA5 | rs190065944 | A | 0.29 | 0.23 | 1.67‡ (1.35–2.07) | 2.05 × 10−6 | 1.57‡ (1.18–2.09) | 1.96 × 10−3 | 1.36‡ (0.90–2.06) | 1.41 × 10−1 | 1.59 (1.36–1.86) | 7.04 × 10−9 | 0 | 0.69 |
| 15q25.1 | AGPHD1 | rs8034191 | C | 0.38 | 0.17 | 1.43 (1.24–1.66) | 1.75 × 10−6 | 1.44 (1.13–1.84) | 3.49 × 10−3 | 1.26 (0.95–1.67) | 1.09 × 10−1 | 1.40 (1.25–1.57) | 7.80 × 10−9 | 0 | 0.72 |
| 15q25.1 | IREB2 | rs56219465 | G | 0.37 | 0.23 | 1.39‡ (1.20–1.60) | 1.19 × 10−5 | 1.43‡ (1.15–1.79) | 1.59 × 10−3 | 1.31‡ (0.99–1.75) | 5.89 × 10−2 | 1.39 (1.24–1.55) | 1.20 × 10−8 | 0 | 0.90 |
| 15q25.1 | IREB2 | rs72738718 | C | 0.37 | 0.23 | 1.39‡ (1.20–1.61) | 1.16 × 10−5 | 1.43‡ (1.14–1.79) | 1.65 × 10−3 | 1.31‡ (0.99–1.75) | 6.01 × 10−2 | 1.39 (1.24–1.55) | 1.21 × 10−8 | 0 | 0.90 |
| 15q25.1 | IREB2 | rs7181486 | C | 0.37 | 0.23 | 1.39‡ (1.20–1.60) | 1.18 × 10−5 | 1.43‡ (1.15–1.79) | 1.61 × 10−3 | 1.31‡ (0.99–1.75) | 5.88 × 10−2 | 1.39 (1.24–1.55) | 1.21 × 10−8 | 0 | 0.90 |
| 15q25.1 | IREB2 | rs17483929 | A | 0.38 | 0.23 | 1.39 (1.20–1.60) | 1.19 × 10−5 | 1.43 (1.14–1.79) | 1.68 × 10−3 | 1.31‡ (0.99–1.75) | 5.89 × 10−2 | 1.39 (1.24–1.55) | 1.25 × 10−8 | 0 | 0.90 |
| 15q25.1 | AGPHD1 | rs11852372 | C | 0.35 | 0.17 | 1.45‡ (1.25–1.70) | 2.03 × 10−6 | 1.42‡ (1.10–1.82) | 6.25 × 10−3 | 1.27‡ (0.94–1.72) | 1.14 × 10−1 | 1.41 (1.25–1.59) | 1.57 × 10−8 | 0 | 0.75 |
| 15q25.1 | IREB2 | rs55983731 | T | 0.37 | 0.23 | 1.39‡ (1.20–1.60) | 1.18 × 10−5 | 1.41‡ (1.12–1.76) | 2.97 × 10−3 | 1.31‡ (0.99–1.75) | 5.87 × 10−2 | 1.38 (1.23–1.54) | 2.01 × 10−8 | 0 | 0.93 |
| 15q25.1 | IREB2 | rs17483686 | T | 0.37 | 0.23 | 1.39‡ (1.20–1.60) | 1.19 × 10−5 | 1.41‡ (1.12–1.76) | 2.98 × 10−3 | 1.31‡ (0.99–1.75) | 5.87 × 10−2 | 1.38 (1.23–1.54) | 2.06 × 10−8 | 0 | 0.93 |
| 15q25.1 | IREB2 | rs17483721 | C | 0.61 | 0.77 | 1.39 (1.20–1.60) | 1.21 × 10−5 | 1.40 (1.12–1.76) | 3.01 × 10−3 | 1.31‡ (0.99–1.75) | 5.87 × 10−2 | 1.38 (1.23–1.54) | 2.16 × 10−8 | 0 | 0.93 |
| 15q25.1 | CHRNA3 | rs56077333 | A | 0.35 | 0.17 | 1.46‡ (1.25–1.70) | 1.63 × 10−6 | 1.41‡ (1.09–1.83) | 7.98 × 10−3 | 1.24‡ (0.92–1.68) | 1.58 × 10−1 | 1.41 (1.25–1.59) | 2.38 × 10−8 | 0 | 0.65 |
| 15q25.1 | IREB2 | rs72738736 | T | 0.37 | 0.23 | 1.38‡ (1.19–1.59) | 1.79 × 10−5 | 1.42‡ (1.13–1.77) | 2.50 × 10−3 | 1.32‡ (0.99–1.75) | 5.72 × 10−2 | 1.38 (1.23–1.54) | 2.54 × 10−8 | 0 | 0.93 |
Definition of abbreviations: AA, African American; CI, confidence interval; COPDGene, Genetic Epidemiology of COPD Study; ECLIPSE, Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints; EUR, European white; FRQ, risk allele frequency; I2, percentage of the variability in effect estimates due to heterogeneity; NHW, non-Hispanic white; OR, odds ratio; Q, P values for Cochran’s Q test; SNP, single-nucleotide polymorphism.
Adjusted for age, sex, pack-years of cigarette smoking and genetic ancestry, as summarized in the principal components.
EUR frequency data is from the meta-analysis of COPDGene NHW and ECLIPSE.
Imputed genotypes.
Figure 5.
Local association plots for significant loci in the meta-analysis of subjects with COPD with PA/A greater than 1 versus smoking control subjects in COPDGene NHWs, AAs, and ECLIPSE. The x axis is chromosomal position, and the y axis shows the –log10 P value. The most significant SNP at each locus is labeled in purple (denoted by asterisk, as it is located in a transcription factor binding site conserved in a multiple-species alignment), with other SNPs colored by degree of LD (r2). Plots were created using LocusZoom.
Complementary Analyses
Because the meta-analysis of subjects with COPD with PAE relative to smoking control subjects showed 15q25.1 as the only genome-wide significant locus, we performed additional analyses to ascertain whether previously implicated genome-wide significant COPD risk loci had different effects between COPD with PAE and COPD without PAE. A meta-analysis of GWASs for subjects with COPD without PAE relative to smoking control subjects identified FAM13A on 4q22.1 as the top gene, which was followed by HHIP-AS1 on 4q31.21 and CHRNA3 (Table E4 and Figure E4). ORs and P values of previously known COPD risk SNPs among our results from meta-analyses for COPD with PAE or without PAE are summarized in Table E3. Permutation testing demonstrated that the effect estimates in the meta-analysis of subjects with COPD with PAE were stronger compared with those without PAE at three SNPs on 15q25 (P < 0.0001 for rs12914385, rs8034191, and rs11858836; Table 4).
Table 4.
Genome-Wide Association Study Meta-Analysis Results of Subjects with Chronic Obstructive Pulmonary Disease with a Pulmonary Artery:Ascending Aorta Ratio Greater Than 1 versus Smoking Control Subjects Compared with Those of Subjects with Chronic Obstructive Pulmonary Disease with a Pulmonary Artery:Ascending Aorta Ratio of 1 or Less versus Smoking Control Subjects for Previously Identified COPD Risk Alleles
| Locus | Gene | SNP | Risk Allele | COPD with PA/A > 1 versus Smoking Control Subjects |
COPD with PA/A ≤ 1 versus Smoking Control Subjects |
Permutation Testing to Assess Difference of OR between Two Meta-Analyses, 10,000 Times | ||
|---|---|---|---|---|---|---|---|---|
| OR | P Value | OR | P Value | P Value | ||||
| 4q22 | FAM13A | rs2869967* | C | 1.25 | 9.14 × 10−5 | 1.28 | 8.73 × 10−10 | NS |
| 4q22 | FAM13A | rs4416442† | C | 1.27 | 1.66 × 10−5 | 1.28 | 1.74 × 10−10 | NS |
| 4q22 | FAM13A | rs7671167*,‡ | T | 1.25 | 7.39 × 10−5 | 1.22 | 2.32 × 10−7 | NS |
| 4q22 | FAM13A | rs1964516‡ | T | 1.17 | 6.32 × 10−3 | 1.23 | 2.38 × 10−7 | 0.015 |
| 4q31 | HHIP | rs13141641†,‡ | T | 1.28 | 5.68 × 10−5 | 1.23 | 7.94 × 10−7 | 0.013 |
| 4q31 | HHIP | rs13118928‡ | A | 1.22 | 9.25 × 10−4 | 1.21 | 4.25 × 10−6 | NS |
| 15q25 | CHRNA3 | rs12914385† | T | 1.36 | 1.61 × 10−7 | 1.23 | 5.98 × 10−7 | <0.0001 |
| 15q25 | AGPHD1 | rs8034191§ | C | 1.40 | 7.80 × 10−9 | 1.12 | 7.97 × 10−3 | <0.0001 |
| 15q25 | IREB2 | rs11858836‡ | A | 1.38 | 3.90 × 10−7 | 1.16 | 1.32 × 10−3 | <0.0001 |
| 19q13 | RAB4B | rs2604894‡ | G | 1.16 | 1.01 × 10−2 | 1.10 | 1.53 × 10−2 | 0.010 |
| 14q32 | RIN3 | rs754388† | C | 1.38 | 3.49 × 10−5 | 1.29 | 1.19 × 10−6 | 0.007 |
| 14q32 | RIN3 | rs17184313† | C | 1.27 | 2.15 × 10−3 | 1.27 | 8.53 × 10−6 | NS |
Definition of abbreviations: COPD, chronic obstructive pulmonary disease; NS, not significant; OR, odds ratio; PA/A, ratio of the diameter of the main pulmonary artery (PA) at the level of its bifurcation and the diameter of the ascending aorta (A) in its maximum dimension measured by computed tomography; SNP, single-nucleotide polymorphism.
Cho and colleagues (Ref. 27).
Cho and colleagues (Ref. 23).
Cho and colleagues (Ref. 29).
Pillai and colleagues (Ref. 37).
To determine whether there is likely to be more than one functional variant located within the genome-wide significant regions, we performed analyses conditioning on the top (lead) SNP in these meta-analysis. All SNPs present in 250-kb flanks around the top signal were examined. Although no evidence suggestive of secondary associations (P < 5 × 10−4) existed in the meta-analyses of COPD with PAE relative to COPD without PAE on 15q25 (conditioning on rs7181486) and 14q31.3 (conditioning on rs7140285), we found evidence suggestive of secondary associations in the meta-analysis of COPD with PAE relative to smoking control subjects on 15q25 (conditioning on rs17486278) in two SNPs (rs9920506, P = 2.17 × 10−4; rs3813567, P = 4.43 × 10−4) located within CHRNB4, coding neuronal acetylcholine receptor subunit β-4.
Discussion
This study is the first GWAS of PAE in COPD, and the first reported genetic association analysis of an important vascular subtype using PA/A. Our most significant finding was at the IREB2 locus with the presence of PAE, which has been previously implicated as a predictor for severe exacerbations and total exacerbation frequency of COPD using the same case subjects as our current study (19).
A genomic region on chromosome 15q25.1 including CHRNA5/3, AGPHD1, and IREB2 is a well established locus for COPD susceptibility (37). Although this region clearly contains genetic determinants for nicotine addiction, mediation analysis suggested that there may be two COPD genetic determinants in that region—one related to smoking, and one independent of smoking (39). A study of sputum gene expression also demonstrated that expression quantitative trait loci for IREB2 and CHRNA5 are not in LD, suggesting two susceptibility genes in this region (40). Our meta-analysis of three GWASs for subjects with COPD with PAE versus smoking control subjects showed the same locus with SNPs in multiple genes reaching the genome-wide significant threshold, whereas the meta-analysis for subjects with COPD with PAE versus those without PAE revealed only IREB2 and AGPHD1 as genes that contained genome-wide significant SNPs. A recent meta-analysis for severe COPD including our subjects identified 15q25 as the most genome-wide significant region (23). Considering the relatively low mean FEV1 % predicted in our subjects with COPD with PAE, the most strongly associated genomic region in our current analysis of subjects with COPD with PAE relative to smoking control subjects seemed to be consistent with the previous locus for severe COPD. On the other hand, PA/A data in smoking control subjects were not available, and it is possible that some subjects could have PAE in this group, which may affect our results. The significance of the top SNP, rs17486278, located within CHRNA5, in the analysis of COPD with PAE relative to smoking control subjects was reduced to 4.08 × 10−6 in the analysis of PAE versus no PAE within subjects with COPD. Although the association of the CHRNA3 locus with COPD has been reported to be significantly mediated by smoking-related phenotypes, IREB2 appears to affect COPD independently of smoking (39, 41). IREB2 may have a different role for COPD pathogenesis from the other genes on 15q25.1, and our study provides additional evidence for this hypothesis.
The protein product of IREB2, also known as iron-regulatory protein 2 (IRP2), is an RNA-binding protein that, together with IREB1, participates in maintaining human cellular iron metabolism. Even though iron is a vital element, it is toxic at high concentrations. Therefore, iron acquisition and storage are strictly controlled. Translation and/or stability of mRNAs encoding proteins required for iron storage, acquisition, and utilization are regulated through the binding of IRPs. According to body iron amount, IRPs modulate the expression of those proteins relevant to iron uptake, export, and sequestration (42). When systemic iron is too low, IRPs decrease iron storage and increase iron uptake (43). Hypoxemia is commonly associated with COPD progression; post-translational regulation of IREB2 is dependent on oxygen as well as iron (44). Two recent papers (45, 46) have identified a mechanism for iron and oxygen sensing for IRP2-mediated post-transcriptional regulation of iron metabolism; IRP2 does not directly sense iron, but rather the iron/oxygen sensor is the enzyme that effects IRP2 degradation.
Chronic alveolar hypoxia may play an important mechanistic role; however, pulmonary vascular remodeling has been observed in lung specimens from patients with mild-to-moderate COPD without chronic hypoxemia (9). Even those without resting hypoxemia and/or PH could have hypoxemia or PH during exertion. Genetic variants of IREB2 may determine individual variability of pulmonary vascular response to exertional or resting hypoxemia, influencing PA pressures independently of the severity of airflow limitation.
One of the genome-wide significant SNPs for PAE in subjects with COPD was rs7140285 on 14q31.3 near GALC, which encodes galactosylceramidase, which was the most significant SNP in the analysis of COPD with PAE relative to those without PAE with adjustment for FEV1 % predicted. Mutations in GALC have been associated with Krabbe disease, also known as globoid cell leukodystrophy or galactosylceramide lipidosis. It is a rare, often fatal degenerative disorder that affects the myelin sheath of the nervous system, and involves dysfunctional metabolism of sphingolipids (47). This disorder is inherited in an autosomal recessive pattern. Recently, a study demonstrated that galactosylceramidase deficiency inhibits angiogenesis in murine aortic endothelial cells (48). It was also shown that small interfering RNA GALC knockdown inhibits human umbilical vein endothelial cell proliferation and migration, suggesting a pivotal role of GALC in endothelial neovascular responses. In addition, ceramides have been implicated in both COPD pathogenesis and vascular endothelial cell death through alterations in cellular apoptosis (49, 50). Even though a case report suggested lung involvement of Krabbe disease (51), it needs to be determined whether there is any role of GALC in the development of PH associated with COPD.
Our study has several limitations. First, although our strongest genetic associations with COPD with PAE were found with SNPs near IREB2, there are multiple other genes in the chromosome 15q25.1 region that could be responsible for the PAE associations. We have not determined which genetic variants in or near IREB2 are functional variants for the development of PH in COPD. Although IREB2 protein and mRNA were increased in lung tissue samples from subjects with COPD in comparison to control subjects (52), the specific role of IREB2 in the pathogenesis of PH associated with COPD and functional differences according to IREB2 variants will need to be evaluated. Second, a replication analysis has not been explored, even though this was a meta-analysis of three GWASs using the largest COPD cohorts to date. Third, PA/A of our smoking control subjects was not included, although the prevalence of PAE in control subjects was lower than that in subjects with GOLD 2–4 (J.M.W., unpublished data). Because age-associated increases in PA systolic pressure in the general population have been reported (53), a portion of our smoking control subjects might have PA/A greater than 1, considering their mean age. Fourth, PA pressures were not measured, although the ratio of PA/A has been shown to correlate with hemodynamically gauged PA pressure (15–17) even better than echocardiography in severe COPD (18), and PA/A greater than 1 has been proven to be a predictor of severe exacerbation of COPD (19). It is also possible that PAE, at least in some subjects, could be caused by COPD-related factors unrelated to hypoxemia. PAE could be caused by not only resting PH, but also peripheral vascular pruning with centralization of blood flow, undiagnosed cardiovascular disease, or a combination of these mechanisms (10, 54–56). Despite these limitations, we emphasize that our phenotype was recently validated in a well designed study including a large number of subjects with COPD, longitudinal follow up, and replication (19), and that we examined our hypothesis in the same set of well phenotyped subjects. Finally, our study did not address whether IREB2 is responsible for “disproportionate” PH associated with relatively mild airway limitation. Although some subjects with COPD with PAE had moderate airflow limitation (GOLD 2), mean FEV1 % predicted was lower than among those without PAE. However, our complementary analysis including adjustment for FEV1 % predicted revealed that rs7181486 in IREB2 was one of the most significant SNPs, but was not significant genome wide. Moreover, the results from the meta-analysis for COPD with PAE relative to smoking control subjects were somewhat different from a recent meta-analysis of subjects with severe COPD relative to smoking control subjects, including our subjects, which demonstrated MMP3/12, RIN3, and TGFB2, as well as four previously described genome-wide significant loci, as the most significant associations (23). These results suggest that our genome-wide significant region, particularly IREB2, is likely to be from a vascular subtype, not purely an indicator of the severity of airflow limitation.
We have reported the first GWAS of subjects with COPD with PAE relative to those without PAE as well as to smoking control subjects, and identified IREB2 and GALC as potential susceptibility genes associated with PH in COPD. This study strongly supports that phenotypic heterogeneity of COPD is closely linked to genetic heterogeneity. Additional GWASs for specific COPD subtypes are likely to provide further insight into different roles of genetic variants contributing to COPD heterogeneity.
Acknowledgments
Acknowledgments
The authors acknowledge and thank the COPDGene Core Teams, the COPDGene investigators from the participating clinical centers, and the ECLIPSE (Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints) investigators.
The Members of the COPDGene Core Teams Are:
Administrative Core: James D. Crapo, M.D. (Principal Investigator [PI]); Edwin K. Silverman, M.D., Ph.D. (PI); Barry J. Make, M.D.; Elizabeth A. Regan, M.D., Ph.D.; Stephanie Bratschie, M.P.H.; Rochelle Lantz; Sandra Melanson, M.S.W., L.C.S.W.; Lori Stepp.
Executive Committee: Terri Beaty, Ph.D.; Russell P. Bowler, M.D., Ph.D.; James D. Crapo, M.D.; Jeffrey L. Curtis, M.D.; Douglas Everett, Ph.D.; MeiLan K. Han, M.D., M.S.; John E. Hokanson, M.P.H., Ph.D.; David Lynch, M.B.; Barry J. Make, M.D.; Elizabeth A. Regan, M.D., Ph.D.; Edwin K. Silverman, M.D., Ph.D.; E. Rand Sutherland, M.D.
External Advisory Committee: Eugene R. Bleecker, M.D.; Harvey O. Coxson, Ph.D.; Ronald G. Crystal, M.D.; James C. Hogg, M.D.; Michael A. Province, Ph.D.; Stephen I. Rennard, M.D.; Duncan C. Thomas, Ph.D.
National Heart, Lung, and Blood Institute: Thomas Croxton, M.D., Ph.D.; Weiniu Gan, Ph.D.; Lisa Postow, Ph.D.
COPD Foundation: John W. Walsh; Randel Plant; Delia Prieto
Biorepository Visit 1 (Baltimore, MD): Homayoon Farzadegan, Ph.D.; Samantha Bragan; Stacey Cayetano
Biorepository Visit 2 (Boston, MA): Daniel Cossette; Roxanne K. Kelly, M.B.A.
Data Coordinating Center: Douglas Everett, Ph.D.; Andre Williams, Ph.D.; Ruthie Knowles; Carla Wilson, M.S.
Epidemiology Core: John Hokanson, M.P.H., Ph.D.; Jennifer Black-Shinn, M.P.H.; Gregory Kinney, M.P.H.
Genetic Analysis Core: Terri Beaty, Ph.D.; Peter J. Castaldi, M.D., M.Sc.; Michael Cho, M.D.; Dawn L. DeMeo, M.D., M.P.H.; Marilyn G. Foreman, M.D., M.S.; Nadia N. Hansel, M.D., M.P.H.; Megan E. Hardin, M.D.; Craig Hersh, M.D., M.P.H.; Jacqueline Hetmanski, M.S.; John E. Hokanson, M.P.H., Ph.D.; Nan Laird, Ph.D.; Christoph Lange, Ph.D.; Sharon M. Lutz, M.P.H., Ph.D.; Manuel Mattheisen, M.D.; Merry-Lynn McDonald, M.Sc., Ph.D.; Margaret M. Parker, MHS; Elizabeth A. Regan, M.D., Ph.D.; Stephanie Santorico, Ph.D.; Edwin K. Silverman, M.D., Ph.D.; Emily S. Wan, M.D.; Jin Zhou, Ph.D.
Genotyping Cores: Genome-Wide Core: Terri Beaty, Ph.D.; Candidate Genotyping Core: Craig P. Hersh, M.D., M.P.H.; Edwin K. Silverman, M.D., Ph.D.
Imaging Core: David Lynch, M.B.; Mustafa Al Qaisi, M.D.; Jaleh Akhavan; Christian W. Cox, M.D.; Harvey O. Coxson, Ph.D.; Deanna Cusick; Jennifer G. Dy, Ph.D.; Shoshana Ginsburg, M.S.; Eric A. Hoffman, Ph.D.; Philip F. Judy, Ph.D.; Alex Kluiber; Alexander McKenzie; John D. Newell, Jr., M.D.; John J. Reilly, Jr., M.D.; James Ross, M.Sc.; Raul San Jose Estepar, Ph.D.; Joyce D. Schroeder, M.D.; Jered Sieren; Arkadiusz Sitek, Ph.D.; Douglas Stinson; Edwin van Beek, M.D., Ph.D., MEd; George R. Washko, M.D.; Jordan Zach
PFT QA Core: Robert Jensen, Ph.D.; E. Rand Sutherland, M.D.
Biological Repository, Johns Hopkins University, Baltimore, Maryland: Homayoon Farzadegan, Ph.D.; Samantha Bragan; Stacey Cayetano
The COPDGene Investigators from the Participating Clinical Centers Are:
Ann Arbor Department of Veterans Affairs, Ann Arbor, Michigan: Jeffrey Curtis, M.D.; Ella Kazerooni, M.D.
Baylor College of Medicine, Houston, Texas: Nicola Hanania, M.D., M.S.; Philip Alapat, M.D.; Venkata Bandi, M.D.; Kalpalatha Guntupalli, M.D.; Elizabeth Guy, M.D.; Antara Mallampalli, M.D.; Charles Trinh, M.D.; Mustafa Atik, M.D.; Hasan Al-Azzawi, M.D.; Marc Willis, DO; Susan Pinero, M.D.; Linda Fahr, M.D.; Arun Nachiappan, M.D.; Collin Bray, M.D.; L. Alexander Frigini, M.D.; Carlos Farinas, M.D.; David Katz, M.D.; Jose Freytes, M.D.; Anne Marie Marciel, M.D.
Brigham and Women’s Hospital, Boston, Massachusetts: Dawn DeMeo, M.D., M.P.H.; Craig Hersh, M.D., M.P.H.; George Washko, M.D.; Francine Jacobson, M.D., M.P.H.; Hiroto Hatabu, M.D., Ph.D.; Peter Clarke, M.D.; Ritu Gill, M.D.; Andetta Hunsaker, M.D.; Beatrice Trotman-Dickenson, M.B.B.S.; Rachna Madan, M.D.
Columbia University, New York, New York: R. Graham Barr, M.D., Dr.P.H.; Byron Thomashow, M.D.; John Austin, M.D.; Belinda D’Souza, M.D.
Duke University Medical Center, Durham, North Carolina: Neil MacIntyre, Jr., M.D.; Lacey Washington, M.D.; H Page McAdams, M.D.
Fallon Clinic, Worcester, Massachusetts: Richard Rosiello, M.D.; Timothy Bresnahan, M.D.; Joseph Bradley, M.D.; Sharon Kuong, M.D.; Steven Meller, M.D.; Suzanne Roland, M.D.
Health Partners Research Foundation, Minneapolis, Minnesota: Charlene McEvoy, M.D., M.P.H.; Joseph Tashjian, M.D.
Johns Hopkins University, Baltimore, Maryland: Robert Wise, M.D.; Nadia Hansel, M.D., M.P.H.; Robert Brown, M.D.; Gregory Diette, M.D.; Karen Horton, M.D.
Los Angeles Biomedical Research Institute at Harbor University of California Los Angeles Medical Center, Los Angeles, California: Richard Casaburi, M.D.; Janos Porszasz, M.D., Ph.D.; Hans Fischer, M.D., Ph.D.; Matt Budoff, M.D.; Mehdi Rambod, M.D.
Michael E. DeBakey Veterans Affairs Medical Center, Houston, Texas: Amir Sharafkhaneh, M.D.; Charles Trinh, M.D.; Hirani Kamal, M.D.; Roham Darvishi, M.D.; Marc Willis, DO; Susan Pinero, M.D.; Linda Fahr, M.D.; Arun Nachiappan, M.D.; Collin Bray, M.D.; L. Alexander Frigini, M.D.; Carlos Farinas, M.D.; David Katz, M.D.; Jose Freytes, M.D.; Anne Marie Marciel, M.D.
Minneapolis Department of Veterans Affairs, Minneapolis, Minnesota: Dennis Niewoehner, M.D.; Quentin Anderson, M.D.; Kathryn Rice, M.D.; Audrey Caine, M.D.
Morehouse School of Medicine, Atlanta, Georgia: Marilyn Foreman, M.D., M.S.; Gloria Westney, M.D., M.S.; Eugene Berkowitz, M.D., Ph.D.
National Jewish Health, Denver, Colorado: Russell Bowler, M.D., Ph.D.; David Lynch, M.B.; Joyce Schroeder, M.D.; Valerie Hale, M.D.; John Armstrong II, M.D.; Debra Dyer, M.D.; Jonathan Chung, M.D.; Christian Cox, M.D.
Temple University, Philadelphia, Pennsylvania: Gerard Criner, M.D.; Victor Kim, M.D.; Nathaniel Marchetti, DO; Aditi Satti, M.D.; A. James Mamary, M.D.; Robert Steiner, M.D.; Chandra Dass, M.D.; Libby Cone, M.D.
University of Alabama, Birmingham, Alabama: William Bailey, M.D.; Mark Dransfield, M.D.; Michael Wells, M.D.; Surya Bhatt, M.D.; Hrudaya Nath, M.D.; Satinder Singh, M.D.
University of California, San Diego, California: Joe Ramsdell, M.D.; Paul Friedman, M.D.
University of Iowa, Iowa City, Iowa: Alejandro Cornellas, M.D.; John Newell, Jr., M.D.; Edwin JR van Beek, M.D., Ph.D.
University of Michigan, Ann Arbor, Michigan: Fernando Martinez, M.D.; MeiLan Han, M.D.; Ella Kazerooni, M.D.
University of Minnesota, Minneapolis, Minnesota: Christine Wendt, M.D.; Tadashi Allen, M.D.
University of Pittsburgh, Pittsburgh, Pennsylvania: Frank Sciurba, M.D.; Joel Weissfeld, M.D., M.P.H.; Carl Fuhrman, M.D.; Jessica Bon, M.D.; Danielle Hooper, M.D.
University of Texas Health Science Center at San Antonio, San Antonio, Texas: Antonio Anzueto, M.D.; Sandra Adams, M.D.; Carlos Orozco, M.D.; Mario Ruiz, M.D.; Amy Mumbower, M.D.; Ariel Kruger, M.D.; Carlos Restrepo, M.D.; Michael Lane, M.D.
The Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints Investigators Are:
Investigators: Bulgaria: Y. Ivanov, Pleven; K. Kostov, Sofia. Canada: J. Bourbeau, Montreal; M. Fitzgerald, Vancouver, BC; P. Hernandez, Halifax, NS; K. Killian, Hamilton, ON; R. Levy, Vancouver, BC; F. Maltais, Montreal; D. O'Donnell, Kingston, ON. Czech Republic: J. Krepelka, Prague. Denmark: J. Vestbo, Hvidovre. The Netherlands: E. Wouters, Horn-Maastricht. New Zealand: D. Quinn, Wellington. Norway: P. Bakke, Bergen. Slovenia: M. Kosnik, Golnik. Spain: A. Agusti, J. Sauleda, P. de Mallorca. Ukraine: Y. Feschenko, V. Gavrisyuk, L. Yashina, Kiev; N. Monogarova, Donetsk. United Kingdom: P. Calverley, Liverpool; D. Lomas, Cambridge; W. MacNee, Edinburgh; D. Singh, Manchester; J. Wedzicha, London. United States: A. Anzueto, San Antonio, Texas; S. Braman, Providence, Rhode Island; R. Casaburi, Torrance, California; B. Celli, Boston; G. Giessel, Richmond, Virginia; M. Gotfried, Phoenix, Arizona; G. Greenwald, Rancho Mirage, California; N. Hanania, Houston, Texas; D. Mahler, Lebanon, New Hampshire; B. Make, Denver, Colorado; S. Rennard, Omaha, Nebraska; C. Rochester, New Haven, Connecticut; P. Scanlon, Rochester, Minnesota; D. Schuller, Omaha, Nebraska; F. Sciurba, Pittsburgh, Pennsylvania; A. Sharafkhaneh, Houston, Texas; T. Siler, St. Charles, Missouri; E. Silverman, Boston, Massachusetts; A. Wanner, Miami, Florida; R. Wise, Baltimore, Maryland; R. ZuWallack, Hartford, Connecticut.
Steering Committee: H. Coxson (Canada), C. Crim (GlaxoSmithKline, USA), L. Edwards (GlaxoSmithKline, USA), D. Lomas (UK), W. MacNee (UK), E. Silverman (USA), R. Tal Singer (Co-chair, GlaxoSmithKline, USA), J. Vestbo (Co-chair, Denmark), J. Yates (GlaxoSmithKline, USA).
Scientific Committee: A. Agusti (Spain), P. Calverley (UK), B. Celli (USA), C. Crim (GlaxoSmithKline, USA), B. Miller (GlaxoSmithKline, USA), W. MacNee (Chair, UK), S. Rennard (USA), R. Tal-Singer (GlaxoSmithKline, USA), E. Wouters (The Netherlands), J. Yates (GlaxoSmithKline, USA).
Footnotes
This work was supported by National Institutes of Health grants R01 HL089856 (E.K.S.), R01 HL075478 (E.K.S), R01HL089897 (J.D.C.), P01 HL105339 (E.K.S.), K08 HL097029 (M.H.C), and R01 HL113264 (M.H.C.). The COPDGene study (NCT00608764) is also supported by the COPD Foundation through contributions made to an industry advisory board comprised of AstraZeneca, Boehringer Ingelheim, Novartis, Pfizer, Siemens, Sunovion and GlaxoSmithKline (GSK). The Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints study (NCT00292552; GSK code SCO104960) was sponsored by GSK.
Author Contributions: study concept and design—E.K.S. and J.H.L.; data acquisition and quality control—M.H.C., C.P.H, J.M.W., M.T.D., R.P.B., D. A. Lynch, D. A. Lomas, J.D.C., and E.K.S; analysis and interpretation—J.H.L., M.H.C., M.-L.N.M, C.P.H, and E.K.S; critical revision of manuscript—all authors.
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1165/rcmb.2014-0210OC on August 7, 2014
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.US Burden of Disease Collaborators. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel BD, Coxson HO, Pillai SG, Agustí AG, Calverley PM, Donner CF, Make BJ, Müller NL, Rennard SI, Vestbo J, et al. International COPD Genetics Network. Airway wall thickening and emphysema show independent familial aggregation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2008;178:500–505. doi: 10.1164/rccm.200801-059OC. [DOI] [PubMed] [Google Scholar]
- 3.McCloskey SC, Patel BD, Hinchliffe SJ, Reid ED, Wareham NJ, Lomas DA. Siblings of patients with severe chronic obstructive pulmonary disease have a significant risk of airflow obstruction. Am J Respir Crit Care Med. 2001;164:1419–1424. doi: 10.1164/ajrccm.164.8.2105002. [DOI] [PubMed] [Google Scholar]
- 4.Silverman EK, Mosley JD, Palmer LJ, Barth M, Senter JM, Brown A, Drazen JM, Kwiatkowski DJ, Chapman HA, Campbell EJ, et al. Genome-wide linkage analysis of severe, early-onset chronic obstructive pulmonary disease: airflow obstruction and chronic bronchitis phenotypes. Hum Mol Genet. 2002;11:623–632. doi: 10.1093/hmg/11.6.623. [DOI] [PubMed] [Google Scholar]
- 5.Hallberg J, Dominicus A, Eriksson UK, Gerhardsson de Verdier M, Pedersen NL, Dahlbäck M, Nihlén U, Higenbottam T, Svartengren M. Interaction between smoking and genetic factors in the development of chronic bronchitis. Am J Respir Crit Care Med. 2008;177:486–490. doi: 10.1164/rccm.200704-565OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Minai OA, Chaouat A, Adnot S. Pulmonary hypertension in COPD: epidemiology, significance, and management: pulmonary vascular disease: the global perspective. Chest. 2010;137(6 suppl):39S–51S. doi: 10.1378/chest.10-0087. [DOI] [PubMed] [Google Scholar]
- 7.Thabut G, Dauriat G, Stern JB, Logeart D, Lévy A, Marrash-Chahla R, Mal H. Pulmonary hemodynamics in advanced COPD candidates for lung volume reduction surgery or lung transplantation. Chest. 2005;127:1531–1536. doi: 10.1378/chest.127.5.1531. [DOI] [PubMed] [Google Scholar]
- 8.Chaouat A, Bugnet AS, Kadaoui N, Schott R, Enache I, Ducoloné A, Ehrhart M, Kessler R, Weitzenblum E. Severe pulmonary hypertension and chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;172:189–194. doi: 10.1164/rccm.200401-006OC. [DOI] [PubMed] [Google Scholar]
- 9.Santos S, Peinado VI, Ramírez J, Melgosa T, Roca J, Rodriguez-Roisin R, Barberà JA. Characterization of pulmonary vascular remodelling in smokers and patients with mild COPD. Eur Respir J. 2002;19:632–638. doi: 10.1183/09031936.02.00245902. [DOI] [PubMed] [Google Scholar]
- 10.Christensen CC, Ryg MS, Edvardsen A, Skjønsberg OH. Relationship between exercise desaturation and pulmonary haemodynamics in COPD patients. Eur Respir J. 2004;24:580–586. doi: 10.1183/09031936.04.00118303. [DOI] [PubMed] [Google Scholar]
- 11.McGhan R, Radcliff T, Fish R, Sutherland ER, Welsh C, Make B. Predictors of rehospitalization and death after a severe exacerbation of COPD. Chest. 2007;132:1748–1755. doi: 10.1378/chest.06-3018. [DOI] [PubMed] [Google Scholar]
- 12.Burrows B, Kettel LJ, Niden AH, Rabinowitz M, Diener CF. Patterns of cardiovascular dysfunction in chronic obstructive lung disease. N Engl J Med. 1972;286:912–918. doi: 10.1056/NEJM197204272861703. [DOI] [PubMed] [Google Scholar]
- 13.Traver GA, Cline MG, Burrows B. Predictors of mortality in chronic obstructive pulmonary disease: a 15-year follow-up study. Am Rev Respir Dis. 1979;119:895–902. doi: 10.1164/arrd.1979.119.6.895. [DOI] [PubMed] [Google Scholar]
- 14.Oswald-Mammosser M, Weitzenblum E, Quoix E, Moser G, Chaouat A, Charpentier C, Kessler R. Prognostic factors in COPD patients receiving long-term oxygen therapy: importance of pulmonary artery pressure. Chest. 1995;107:1193–1198. doi: 10.1378/chest.107.5.1193. [DOI] [PubMed] [Google Scholar]
- 15.Devaraj A, Wells AU, Meister MG, Corte TJ, Wort SJ, Hansell DM. Detection of pulmonary hypertension with multidetector CT and echocardiography alone and in combination. Radiology. 2010;254:609–616. doi: 10.1148/radiol.09090548. [DOI] [PubMed] [Google Scholar]
- 16.Pérez-Enguix D, Morales P, Tomás JM, Vera F, Lloret RM. Computed tomographic screening of pulmonary arterial hypertension in candidates for lung transplantation. Transplant Proc. 2007;39:2405–2408. doi: 10.1016/j.transproceed.2007.07.055. [DOI] [PubMed] [Google Scholar]
- 17.Ng CS, Wells AU, Padley SP. A CT sign of chronic pulmonary arterial hypertension: the ratio of main pulmonary artery to aortic diameter. J Thorac Imaging. 1999;14:270–278. doi: 10.1097/00005382-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Iyer AS, Wells JM, Vishin S, Bhatt SP, Wille KM, Dransfield MTCT. CT scan–measured pulmonary artery to aorta ratio and echocardiography for detecting pulmonary hypertension in severe COPD. Chest. 2014;145:824–832. doi: 10.1378/chest.13-1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wells JM, Washko GR, Han MK, Abbas N, Nath H, Mamary AJ, Regan E, Bailey WC, Martinez FJ, Westfall E, et al. COPDGene Investigators; ECLIPSE Study Investigators. Pulmonary arterial enlargement and acute exacerbations of COPD. N Engl J Med. 2012;367:913–921. doi: 10.1056/NEJMoa1203830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vestbo J, Anderson W, Coxson HO, Crim C, Dawber F, Edwards L, Hagan G, Knobil K, Lomas DA, MacNee W, et al. ECLIPSE investigators. Evaluation of COPD Longitudinally to Identify Predictive Surrogate End-points (ECLIPSE) Eur Respir J. 2008;31:869–873. doi: 10.1183/09031936.00111707. [DOI] [PubMed] [Google Scholar]
- 21.Regan EA, Hokanson JE, Murphy JR, Make B, Lynch DA, Beaty TH, Curran-Everett D, Silverman EK, Crapo JD. Genetic Epidemiology of COPD (COPDGene) study design. COPD. 2010;7:32–43. doi: 10.3109/15412550903499522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, Barnes PJ, Fabbri LM, Martinez FJ, Nishimura M, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–365. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 23.Cho MH, McDonald ML, Zhou X, Mattheisen M, Castaldi PJ, Hersh CP, Demeo DL, Sylvia JS, Ziniti J, Laird NM, et al. NETT Genetics, ICGN, ECLIPSE and COPDGene Investigators. Risk loci for chronic obstructive pulmonary disease: a genome-wide association study and meta-analysis. Lancet Respir Med. 2014;2:214–225. doi: 10.1016/S2213-2600(14)70002-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li Y, Willer CJ, Ding J, Scheet P, Abecasis GR. MaCH: using sequence and genotype data to estimate haplotypes and unobserved genotypes. Genet Epidemiol. 2010;34:816–834. doi: 10.1002/gepi.20533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Howie B, Fuchsberger C, Stephens M, Marchini J, Abecasis GR. Fast and accurate genotype imputation in genome-wide association studies through pre-phasing. Nat Genet. 2012;44:955–959. doi: 10.1038/ng.2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abecasis GR, Auton A, Brooks LD, DePristo MA, Durbin RM, Handsaker RE, Kang HM, Marth GT, McVean GA 1,000 Genomes Project Consortium. An integrated map of genetic variation from 1,092 human genomes. Nature. 2012;491:56–65. doi: 10.1038/nature11632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cho MH, Boutaoui N, Klanderman BJ, Sylvia JS, Ziniti JP, Hersh CP, DeMeo DL, Hunninghake GM, Litonjua AA, Sparrow D, et al. Variants in FAM13A are associated with chronic obstructive pulmonary disease. Nat Genet. 2010;42:200–202. doi: 10.1038/ng.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kong X, Cho MH, Anderson W, Coxson HO, Muller N, Washko G, Hoffman EA, Bakke P, Gulsvik A, Lomas DA, et al. ECLIPSE Study NETT Investigators. Genome-wide association study identifies BICD1 as a susceptibility gene for emphysema. Am J Respir Crit Care Med. 2011;183:43–49. doi: 10.1164/rccm.201004-0541OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cho MH, Castaldi PJ, Wan ES, Siedlinski M, Hersh CP, Demeo DL, Himes BE, Sylvia JS, Klanderman BJ, Ziniti JP, et al. ICGN Investigators; ECLIPSE Investigators; COPDGene Investigators. A genome-wide association study of COPD identifies a susceptibility locus on chromosome 19q13. Hum Mol Genet. 2012;21:947–957. doi: 10.1093/hmg/ddr524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, Maller J, Sklar P, de Bakker PI, Daly MJ, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81:559–575. doi: 10.1086/519795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Bakker PI, Ferreira MA, Jia X, Neale BM, Raychaudhuri S, Voight BF. Practical aspects of imputation-driven meta-analysis of genome-wide association studies. Hum Mol Genet. 2008;17:R122–R128. doi: 10.1093/hmg/ddn288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Willer CJ, Li Y, Abecasis GR. METAL: fast and efficient meta-analysis of genomewide association scans. Bioinformatics. 2010;26:2190–2191. doi: 10.1093/bioinformatics/btq340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Devlin B, Roeder K. Genomic control for association studies. Biometrics. 1999;55:997–1004. doi: 10.1111/j.0006-341x.1999.00997.x. [DOI] [PubMed] [Google Scholar]
- 35.Aulchenko YS, Ripke S, Isaacs A, van Duijn CM. GenABEL: an R library for genome-wide association analysis. Bioinformatics. 2007;23:1294–1296. doi: 10.1093/bioinformatics/btm108. [DOI] [PubMed] [Google Scholar]
- 36.Pruim RJ, Welch RP, Sanna S, Teslovich TM, Chines PS, Gliedt TP, Boehnke M, Abecasis GR, Willer CJ. LocusZoom: regional visualization of genome-wide association scan results. Bioinformatics. 2010;26:2336–2337. doi: 10.1093/bioinformatics/btq419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pillai SG, Ge D, Zhu G, Kong X, Shianna KV, Need AC, Feng S, Hersh CP, Bakke P, Gulsvik A, et al. ICGN Investigators. A genome-wide association study in chronic obstructive pulmonary disease (COPD): identification of two major susceptibility loci. PLoS Genet. 2009;5:e1000421. doi: 10.1371/journal.pgen.1000421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wilk JB, Shrine NR, Loehr LR, Zhao JH, Manichaikul A, Lopez LM, Smith AV, Heckbert SR, Smolonska J, Tang W, et al. Genome-wide association studies identify CHRNA5/3 and HTR4 in the development of airflow obstruction. Am J Respir Crit Care Med. 2012;186:622–632. doi: 10.1164/rccm.201202-0366OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Siedlinski M, Tingley D, Lipman PJ, Cho MH, Litonjua AA, Sparrow D, Bakke P, Gulsvik A, Lomas DA, Anderson W, et al. COPDGene and ECLIPSE Investigators. Dissecting direct and indirect genetic effects on chronic obstructive pulmonary disease (COPD) susceptibility. Hum Genet. 2013;132:431–441. doi: 10.1007/s00439-012-1262-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Qiu W, Cho MH, Riley JH, Anderson WH, Singh D, Bakke P, Gulsvik A, Litonjua AA, Lomas DA, Crapo JD, et al. ECLIPSE Investigators. Genetics of sputum gene expression in chronic obstructive pulmonary disease. PLoS One. 2011;6:e24395. doi: 10.1371/journal.pone.0024395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhou H, Yang J, Li D, Xiao J, Wang B, Wang L, Ma C, Xu S, Ou X, Feng Y. Association of IREB2 and CHRNA3/5 polymorphisms with COPD and COPD-related phenotypes in a Chinese Han population. J Hum Genet. 2012;57:738–746. doi: 10.1038/jhg.2012.104. [DOI] [PubMed] [Google Scholar]
- 42.Rouault TA. The role of iron regulatory proteins in mammalian iron homeostasis and disease. Nat Chem Biol. 2006;2:406–414. doi: 10.1038/nchembio807. [DOI] [PubMed] [Google Scholar]
- 43.Rouault T, Klausner R. Regulation of iron metabolism in eukaryotes. Curr Top Cell Regul. 1997;35:1–19. doi: 10.1016/s0070-2137(97)80001-5. [DOI] [PubMed] [Google Scholar]
- 44.Hanson ES, Foot LM, Leibold EA. Hypoxia post-translationally activates iron-regulatory protein 2. J Biol Chem. 1999;274:5047–5052. doi: 10.1074/jbc.274.8.5047. [DOI] [PubMed] [Google Scholar]
- 45.Vashisht AA, Zumbrennen KB, Huang X, Powers DN, Durazo A, Sun D, Bhaskaran N, Persson A, Uhlen M, Sangfelt O, et al. Control of iron homeostasis by an iron-regulated ubiquitin ligase. Science. 2009;326:718–721. doi: 10.1126/science.1176333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Salahudeen AA, Thompson JW, Ruiz JC, Ma HW, Kinch LN, Li Q, Grishin NV, Bruick RK. An E3 ligase possessing an iron-responsive hemerythrin domain is a regulator of iron homeostasis. Science. 2009;326:722–726. doi: 10.1126/science.1176326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Debs R, Froissart R, Aubourg P, Papeix C, Douillard C, Degos B, Fontaine B, Audoin B, Lacour A, Said G, et al. Krabbe disease in adults: phenotypic and genotypic update from a series of 11 cases and a review. J Inherit Metab Dis. 2013;36:859–868. doi: 10.1007/s10545-012-9560-4. [DOI] [PubMed] [Google Scholar]
- 48.Belleri M, Ronca R, Coltrini D, Nico B, Ribatti D, Poliani PL, Giacomini A, Alessi P, Marchesini S, Santos MB, et al. Inhibition of angiogenesis by β-galactosylceramidase deficiency in globoid cell leukodystrophy. Brain. 2013;136:2859–2875. doi: 10.1093/brain/awt215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Petrache I, Natarajan V, Zhen L, Medler TR, Richter AT, Cho C, Hubbard WC, Berdyshev EV, Tuder RM. Ceramide upregulation causes pulmonary cell apoptosis and emphysema-like disease in mice. Nat Med. 2005;11:491–498. doi: 10.1038/nm1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Petrache I, Petrusca DN, Bowler RP, Kamocki K. Involvement of ceramide in cell death responses in the pulmonary circulation. Proc Am Thorac Soc. 2011;8:492–496. doi: 10.1513/pats.201104-034MW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clarke JT, Ozere RL, Krause VW. Early infantile variant of Krabbe globoid cell leucodystrophy with lung involvement. Arch Dis Child. 1981;56:640–642. doi: 10.1136/adc.56.8.640-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.DeMeo DL, Mariani T, Bhattacharya S, Srisuma S, Lange C, Litonjua A, Bueno R, Pillai SG, Lomas DA, Sparrow D, et al. Integration of genomic and genetic approaches implicates IREB2 as a COPD susceptibility gene. Am J Hum Genet. 2009;85:493–502. doi: 10.1016/j.ajhg.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lam CS, Borlaug BA, Kane GC, Enders FT, Rodeheffer RJ, Redfield MM. Age-associated increases in pulmonary artery systolic pressure in the general population. Circulation. 2009;119:2663–2670. doi: 10.1161/CIRCULATIONAHA.108.838698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Barberà JA, Riverola A, Roca J, Ramirez J, Wagner PD, Ros D, Wiggs BR, Rodriguez-Roisin R. Pulmonary vascular abnormalities and ventilation-perfusion relationships in mild chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1994;149:423–429. doi: 10.1164/ajrccm.149.2.8306040. [DOI] [PubMed] [Google Scholar]
- 55.Barr RG, Bluemke DA, Ahmed FS, Carr JJ, Enright PL, Hoffman EA, Jiang R, Kawut SM, Kronmal RA, Lima JA, et al. Percent emphysema, airflow obstruction, and impaired left ventricular filling. N Engl J Med. 2010;362:217–227. doi: 10.1056/NEJMoa0808836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Matsuoka S, Washko GR, Yamashiro T, Estepar RS, Diaz A, Silverman EK, Hoffman E, Fessler HE, Criner GJ, Marchetti N, et al. National Emphysema Treatment Trial Research Group. Pulmonary hypertension and computed tomography measurement of small pulmonary vessels in severe emphysema. Am J Respir Crit Care Med. 2010;181:218–225. doi: 10.1164/rccm.200908-1189OC. [DOI] [PMC free article] [PubMed] [Google Scholar]