Abstract
Background
Previous IONM studies have demonstrated modest-to-no benefit and did not include a nationwide sample of hospitals representative of broad thyroidectomy practices. This national study was designed to compare vocal cord paralysis (VCP) rates between thyroidectomy with IONM and without monitoring (Conventional).
Study Design
We performed a retrospective analysis of 243,527 thyroidectomies during 2008-2011 using the Nationwide Inpatient Sample.
Results
IONM utilization increased throughout the study period (2.6%, 5.6%, 6.1%, 6.9%) and during this time, VCP rates in the IONM group initially increased year-over-year [0.9%(2008), 2.4%(2009), 2.5%(2010), 1.4%(2011)]. In unadjusted analyses, IONM was associated with significantly higher VCP rates (Conventional 1.4% vs IONM 1.9%, p<0.001). After propensity score matching, IONM remained associated with higher VCP rates in partial thyroidectomy and lower VCP rates for total thyroidectomy with neck dissection. Hospital-level analysis revealed that VCP rates were not explained by differential laryngoscopy rates, decreasing the likelihood of ascertainment bias. Additionally, for hospitals where IONM was applied to >50% of thyroidectomies, lower VCP rates were observed (1.1%) compared to hospitals that applied IONM to <50% (1.6%,p=0.016). Higher hospital volume correlated with lower VCP rates in both groups (<75, 75-299, >300 thyroidectomies/year: IONM-2.1%, 1.7%, 1.7%, conventional-1.5%, 1.3%, 1.0%).
Conclusions
According to this study, IONM has not been broadly adopted into practice. Overall, IONM was associated with a higher rate of VCP even after correction for numerous confounders. In particular, low institutional utilization of IONM and use in partial thyroidectomies is associated with higher rates of VCP. Further studies are warranted to support the broader application of IONM in patients where benefit can be reliably achieved.
Introduction
Thyroidectomy is largely a straightforward, safe and effective surgery for benign and malignant thyroid disease. As such, thyroidectomy is performed by surgeons with varying levels of expertise. In the past two decades several technological advances have altered the approach to thyroid surgery including the introduction of intraoperative nerve monitoring (IONM) to prevent recurrent laryngeal nerve injury1, a shift to ambulatory surgery2, and more recently robotic approaches for cosmetic reasons3.
The evidence to support IONM of the recurrent laryngeal nerve during thyroidectomy remains controversial and describes only modest 4-6 or no benefit 7, 8. Yet, the adoption of IONM was reportedly as high as 29% among surveyed otolaryngologists in 20079 and 37% among surveyed endocrine surgeons in 200610. The prevailing notion today is that IONM is a safe adjunct to thyroidectomy. However, the evidence remains limited and nearly all studies involve a single medical center with high-volume surgeons. Given the breadth of surgeons performing thyroidectomy, national databases can provide further insight into the effect of broad IONM adoption on VCP rates.
As complications following thyroidectomy are low, national databases with high volume and case diversity present an opportunity for robust sub-group analysis. Databases such as the Nationwide Inpatient Sample can yield broad generalizable results in a field with substantial variability among surgeons. In this light, the objective of this study is to measure the nationwide outcomes of thyroidectomy with and without IONM.
Methods
The Nationwide Inpatient Sample is a national database funded by the United States Agency for Healthcare Research and Quality (AHRQ). It is the largest all-payer inpatient health care database in the United States and collects data from a 20% stratified sample of the hospitals around the country. Weight coefficients for each hospital are provided to yield national estimates of inpatient stays. Data from admission to discharge are included for each patient in this database including charge and cost data. Cases that were performed in an outpatient or ambulatory setting are not included in the NIS. Financial data were inflation-adjusted to reflect 2013 equivalents11. Nationwide Inpatient Sample data were obtained according to the Agency for Healthcare Research and Quality (AHRQ) guidelines. The years 2008 to 2011 were selected due to the introduction of the International Classification of Diseases-9th Revision, Clinical Modification (ICD-9-CM) code for intraoperative nerve monitoring (00.94) in 2007. It should be noted that ICD-9-CM does not distinguish between intermittent or continuous IONM.
A listing of ICD-9-CM codes utilized for this study can be found in Table 1. Patients were identified by ICD-9-CM procedure codes for thyroidectomy. Presence of a neck dissection code was designated for each patient. The primary endpoint of this study was a diagnosis of same admission vocal cord paralysis. While diagnoses of partial and complete vocal cord paralysis were included in our outcome, the distinction between transient and permanent VCP is not captured within the ICD-9-CM coding scheme. It should be noted, however, that the codes used are distinct from dysphonia (784.42) which was not included in our analysis. Hospital-level analysis was performed for thyroidectomy case volume and laryngoscopy utilization. Surgeon-level analysis could not be performed because the AHRQ removed surgeon-level data from 2009 onward.
Table 1.
Study Definitions and Associated ICD-9-CM Descriptions and Codes
| Primary procedure | |
|
| |
| Partial thyroidectomy | Unilateral thyroid lobectomy (06.2) |
| Excision of lesion of thyroid (06.31) | |
| Other partial thyroidectomy (06.39) | |
|
| |
| Complete thyroidectomy | Complete thyroidectomy (06.4) |
|
| |
| Adjunctive procedures | |
|
| |
| Intraoperative nerve monitoring | Intraoperative neurophysiologic monitoring (00.94) |
|
| |
| Neck dissection | Regional lymph node excision (40.3) |
| Radical neck dissection NOS (40.40) | |
| Radical neck dissection, unilateral (40.41) | |
| Radical neck dissection, bilateral (40.42) | |
|
| |
| Laryngoscopy | Laryngoscopy or other tracheoscopy (31.42) |
|
| |
| Outcomes | |
|
| |
| Vocal cord paralysis | Vocal cord paralysis NOS (478.30) |
| Vocal cord paralysis, unilateral, partial (478.31) | |
| Vocal cord paralysis, unilateral, complete (478.32) | |
| Vocal cord paralysis, bilateral, partial (478.33) | |
| Vocal cord paralysis, bilateral, complete (478.34) | |
Propensity-score analysis was performed first by identifying pre-operative variables that significantly differed by a p-value of less than 0.001 between conventional and intraoperative nerve monitoring (IONM) groups. These variables were entered into a binary logistic regression and the logit was stored as the propensity score. Nearest neighbor one-to-one matching then was performed for each thyroidectomy type. Propensity score quartile analysis was also performed utilizing the same propensity score as above. Statistical analysis was performed with SPSS version 21. Institutional IRB approval was obtained for this study.
Results
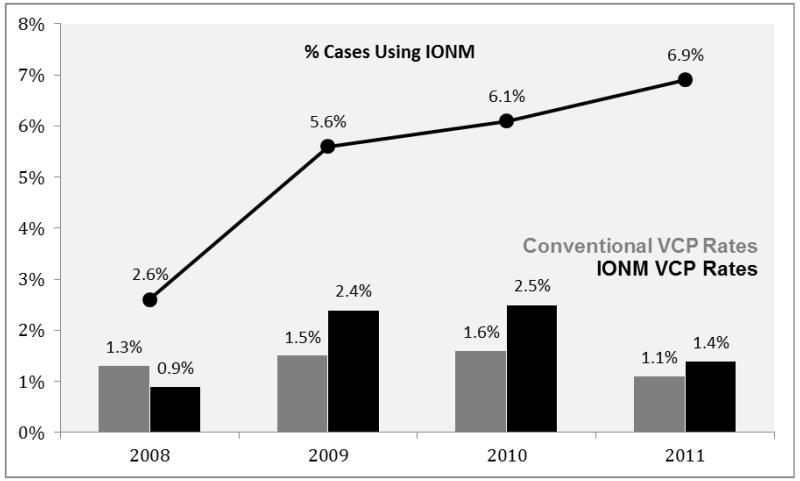
Between 2008 to 2011, 243,527 thyroidectomies were accrued in the Nationwide Inpatient Sample database. Patient demographics are listed by treatment group in Table 2. Patients who received IONM were younger with more chronic conditions, thyroid malignancy, concurrent neck dissection, and were more frequently treated at hospitals that were smaller, urban, and teaching hospitals. Conventional cases predominated (94.7%) with a yearly increase in intraoperative nerve monitoring (IONM) utilization [Figure 1]. As IONM utilization increased throughout the study period, overall VCP rates in the IONM group initially increased year-over-year [0.9%(2008), 2.4%(2009), 2.5%(2010)], but were lower in the last year 1.4%(2011). Overall, conventional VCP rates (1.4%) were significantly lower than IONM VCP rates (1.9%, p<0.001).
Table 2.
Patient Demographics by Treatment Group
| Conventional | IONM | p Value | |
|---|---|---|---|
|
| |||
| Age, y | 52.7 ± 15.8 | 52.3 ± 15.7 | <0.001 |
|
| |||
| No. chronic conditions | 3.3 ± 2.3 [0-19] | 3.6 ± 2.4 [0-16] | <0.001 |
|
| |||
| No. diagnoses for stay | 5.08 ± 3.89 | 5.66 ± 4.08 [1-30]; {5} | <0.001 |
|
| |||
| Length of stay, d | 2.35 ± 5.6 [0-239]; {1} | 2.04 ± 3.02 [0-66]; {1} | <0.001 |
|
| |||
| Race | |||
|
| |||
| White | 67.9% (134521/198161) | 70.6% (8098/11470) | <0.001 |
| Black | 14.1% (27884/198/161) | 12.4% (1422/11470) | |
| Hispanic | 9.7% (19188/198161) | 9.4% (1078/11470) | |
| Asian | 4.4% (8758/198161) | 3.8% (435/11470) | |
| Native American | 0.4% (777/198161) | 0.4% (48/11470) | |
| Other | 3.5% (7033/198161) | 3.4% (389/11470) | |
|
| |||
| Graves disease | 4.4% (10136/230781) | 4.0% (506/12746) | 0.024 |
|
| |||
| Thyroid malignancy | 34.5% (79639/230781) | 39.8% (5072/12746) | <0.001 |
|
| |||
| Same-stay neck dissection | 8.5% (19635/230781) | 14.1% (1792/12746) | <0.001 |
|
| |||
| Insurance | |||
|
| |||
| Medicare | 27.0% (62124/230433) | 25.4% (3241/12742) | <0.001 |
|
| |||
| Medicaid | 9.3% (21480/230433) | 8.2% (1046/12742) | |
|
| |||
| Private | 57.1% (131649/230433) | 60.4% (7695/12742) | |
|
| |||
| Self-Pay | 2.5% (5749/230433) | 2.4% (302/12742) | |
|
| |||
| No Charge | 0.5% (1200/230433) | 0.7% (87/12742) | |
|
| |||
| Other | 3.6% (8231/230433) | 2.9% (371/12742) | |
|
| |||
| Teaching hospital | 61.4% (140317/228416) | 64.5% (8105/12562) | <0.001 |
|
| |||
| Bed size of hospital | |||
|
| |||
| Small | 10.1% (23180/228417) | 11.8% (1480/12563) | <0.001 |
| Medium | 20.3% (46290/228417) | 20.3% (2553/12563) | |
| Large | 69.6% (158947/228417) | 67.9% (8530/12563) | |
|
| |||
| Urban hospital | 92.9% (212242/228416) | 96.45 (12113/12562) | <0.001 |
|
| |||
| Region of hospital | |||
|
| |||
| Northeast | 29.5% (68190/230781) | 24.8% (3167/12746) | <0.001 |
| Midwest | 17.5% (40394/230781) | 20.1% (2562/12746) | |
| South | 30.1% (69455/230781) | 25.8% (3289/12746) | |
| West | 22.9% (52743/230781) | 29.3% (3729/12746) | |
|
| |||
| Year | |||
|
| |||
| 2008 | 28.0% (64622/230781) | 13.3% (1695/12746) | <0.001 |
| 2009 | 22.2% (51330/230781) | 23.9% (3045/12746) | |
| 2010 | 25.7% (59213/230781) | 30.2% (3854/12746) | |
| 2011 | 24.1% (55616/230781) | 32.6% (4152/12746) | |
|
| |||
| Total charge ($) | 34,748 ± 63,400 [125-3,216,183]; {22,934} |
36,275 ± 39,712 [3,027-900,714]; {28,738} |
0.007 |
|
| |||
| Total cost ($) | 11,200 ± 17,856 [39-794,278]; {7,820} |
11,409 ± 11,591 [834-264,686]; {8,933} |
0.228 |
Figure 1.
Vocal cord paralysis rates by treatment group and year with utilization rates. IONM, intraoperative nerve monitoring; VCP, vocal cord paralysis.
Comparisons within each thyroidectomy type demonstrated mostly similar results. Conventional partial thyroidectomy had fewer VCP events (1%) compared with IONM (1.6%, p<0.001). Similarly, conventional total thyroidectomy without neck dissection had a VCP rate of 1.3% versus 1.8% in IONM cases (p<0.001). However, IONM did demonstrate a significant benefit within total thyroidectomies with neck dissection (2.9% versus conventional 4.2%, p=0.01). Given the preoperative differences between treatment groups, a propensity score was calculated for each patient in order to control for treatment bias. Following one-to-one nearest neighbor matching, IONM continued to be associated with higher VCP rates in partial thyroidectomy and lower VCP rates for total thyroidectomy with neck dissection (Table 3). Propensity scores were also examined by quartile. Interestingly, patients in the lowest propensity score quartile (e.g. patients least likely to receive IONM) appeared to contribute most to the differential VCP rates between IONM (2.5%) and conventional cases (1.2%, p=0.03).
Table 3.
Propensity-Score Analysis Comparing Conventional and IONM Groups
| Unadjusted | Propensity Score Matched 1:1 | |||||
|---|---|---|---|---|---|---|
| Conventional | IONM | p Value | Conventional | IONM | p Value | |
| All thyroids (P+T) | 1.4% (3115/228416) | 1.9% (235/12562) | <0.001 | 1.3% (144/11418) | 1.8% (203/11286) | 0.001 |
| Partial thyroid | 1.0% (987/101684) | 1.6% (76/4710) | <0.001 | 1.2% (49/4246) | 1.7% (72/4168) | 0.028 |
| Total thyroid | 1.7% (2129/127514) | 2.0% (160/7873) | 0.016 | 1.4% (103/7229) | 1.8% (131/7138) | 0.056 |
| Total thyroid without ND | 1.3% (1440/111296) | 1.8% (116/6366) | <0.001 | 1.2% (73/5913) | 1.6% (93/5804) | 0.101 |
| Total thyroid with ND | 4.2% (688/16217) | 2.9% (43/1506) | 0.010 | 4.5% (60/1340) | 2.8% (38/1334) | 0.030 |
We examined hospital-level rates of laryngoscopy in order to identify whether the increase in VCP rates was due to an increased surveillance for complications. Overall, 29% of patients diagnosed with VCP also had a documented laryngoscopy. In hospitals that did not use laryngoscopy in any of their thyroidectomy admissions, VCP rates were the same between conventional and IONM cases (0.8% vs 0.9% respectively). For hospitals that utilized laryngoscopy in less than 50% of inpatient stays, IONM continued to have increased VCP rates (2.2% versus conventional 1.8%, p=0.002). Similarly, within hospitals that utilized laryngoscopy more than 50% of the time, IONM cases continued to have more VCP (4.2% versus conventional 1.8%, p=0.009). Mean laryngoscopy rates by hospital were similar in both groups.
To ensure that coding practices did not confound the association of treatment group and VCP rates, we repeated the analysis excluding hospitals that never coded for IONM. VCP rates in IONM remained significantly higher in all thyroidectomy types except for significantly lower VCP in total thyroidectomy with neck dissection. To examine the effect of government payers that do not reimburse IONM, we restricted the analysis to patients within Medicare, Medicaid, and all other insurance types as primary insurance. IONM remained associated with higher VCP rates.
To investigate the effect of selective versus routine use of IONM, we compared hospitals that used IONM in less than and greater than 50% of cases. Hospitals where IONM was applied to >50% of thyroidectomies had lower VCP rates (1.1%) compared to hospitals where IONM was applied to <50% (1.6%,p=0.016). Subgroup analysis by thyroidectomy type revealed that VCP rates for partial thyroidectomy were lowest in hospitals using only conventional surgery, while VCP rates after total thyroidectomy favored hospitals routinely using IONM (Table 4). Higher hospital volume correlated with lower VCP rates in both treatment groups (Table 5). In the conventional group, VCP rates decreased as hospital case volume increased. This relationship was largely true in the IONM group with the exception of partial thyroidectomy, which demonstrated an increased VCP rate as volume increased.
Table 4.
VCP Rates by Hospital IONM Usage Rate
| Hospitals that do not use IONM, % |
Hospitals with Selective (<50%) IONM use, % |
Hospitals with Routine (>50%) IONM use |
p Value |
|
|---|---|---|---|---|
| All thyroids | 1.2 | 1.6 | 1.1% | <0.001 |
| Partial thyroidectomy | 0.8 | 1.3 | 1.4% | <0.001 |
| Total thyroid without neck dissection | 1.3 | 1.3 | 0.8% | 0.213 |
| Total thyroid with neck dissection | 4.8 | 3.9 | 0 | <0.001 |
Table 5.
Annual Hospital Volume By Thyroidectomy Type and IONM
| All thyroidectomies | Partial thyroidectomy | Total thyroid without neck dissection |
Total thyroid with neck dissection |
|||||
|---|---|---|---|---|---|---|---|---|
| Conventional | IONM | Conventional | IONM | Conventional | IONM | Conventional | IONM | |
| <75 | 1.5% | 2.1%** | 1.0% | 1.3% | 1.5% | 2.1%* | 5.3% | 5.4% |
| 75-299 | 1.3% | 1.7%* | 0.9% | 2.1%** | 1.2% | 1.6% | 3.8% | 0.8%** |
| >300 | 1.0% | 1.7%* | 0.8% | 3.5%** | 0.7% | 1.4% | 2.4% | 0* |
p < 0.05.
p<0.001
Discussion
Our results demonstrate that IONM was associated with higher VCP even after controlling for treatment, ascertainment and reimbursement biases. Furthermore, utilization of IONM and complications both increased from 2008 to 2010, then complications decreased in 2011. Sub-analysis demonstrated that less frequent institutional IONM use or use in partial thyroidectomy is associated with higher VCP rates. Moreover, VCP decreased as case volume increased in the IONM group. These findings suggest that there may be a learning curve to realize the benefits of IONM.
It stands to reason that such a learning curve for IONM may exist12. Recent international guidelines for IONM use highlight the complexity in optimizing IONM 13 including proper endotracheal tube and electrode placement, collaboration with anesthesiologist and monitor settings. Any anomaly within the IONM circuit could lead to misrecognition of the recurrent laryngeal nerve. Perhaps another plausible explanation is that IONM may be used as a substitute for, rather than an adjunct to, recurrent laryngeal nerve visualization thereby increasing VCP rates.
Our results do support the use of IONM for total thyroidectomy with neck dissection. This benefit may be due to the increased likelihood for aberrant anatomy, whether from the disease process itself or from prior neck intervention. Indeed, this coincides with studies that demonstrate a more pronounced benefit with IONM in cases with more extensive surgery and in cases of thyroid malignancy5, 6, 14, 15. Taken together, the evidence does support the ongoing use of IONM in total thyroidectomy with neck dissection.
The finding that partial thyroidectomy with IONM has higher VCP with increasing hospital volume is counterintuitive. One possible contributor to this sub-cohort is planned total thyroidectomies that are aborted due to a loss of continuous IONM signal, as has been recommended by recent studies16. In these instances, these cases will result in a partial thyroidectomy despite carrying the pre-operative risks of a total thyroidectomy. This may also explain the decreased VCP in total thyroidectomy. However, our results do not fully corroborate this hypothesis as complete unilateral VCP represents only 6% of all VCP cases. Given that this database cannot distinguish between intermittent recurrent laryngeal nerve monitoring or continuous IONM, further subanalysis is not possible at this time.
Estimations of IONM adoption have been restricted to surveys sent through professional society mailing lists, possibly biasing utilization rates. This study reports a significantly lower IONM utilization rate. It is not clear whether this number is underestimated or prior estimates overestimate utilization due to selection bias of surveys. It is possible that cases involving government-funded insurance that do not reimburse IONM may lead to under-coded IONM cases. Insurance type, however, does not appear to confound our results. Overall, adoption of IONM does not appear to be widespread nationally.
The association of volume and improved outcomes is again corroborated17, 18. This relationship appears to extend to the routine use of IONM. For surgeons who are able to reliably achieve improved results with IONM, this study supports its routine use.
There are notable limitations to this study. The NIS database does not allow for longitudinal tracking of patients following discharge. As such, VCP rates for both treatment groups are underestimated. In addition, a relevant proportion of thyroidectomies occur in ambulatory settings and therefore are not captured in this series. Furthermore, important confounders such as prior neck surgery or prior neck irradiation are not reliably captured in the NIS. These risk factors would affect the complexity of the case, the clinical value of IONM and ultimately the expected rate of VCP. Finally, retrospective analysis is limited by the potential for bias from unmeasured confounding. However, given the increased patient volume and the control of treatment, ascertainment, and coding biases, these results do not support broad adoption of IONM. Further study remains the best option in identifying a causal relationship between IONM and increased VCP.
Conclusion
We found that IONM has not been broadly adopted into practice. Overall, IONM was associated with a higher rate of VCP even after correction for numerous confounders. In particular, less frequent IONM utilization and use in partial thyroidectomies were associated with higher rates of VCP. However, IONM demonstrates a significant benefit in total thyroidectomies with neck dissection. Further studies with longitudinal data are necessary to corroborate these findings.
Acknowledgments
Financial Support: NIH 5T32CA091078-12.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Information: Nothing to disclose.
References
- 1.Eisele DW. Intraoperative electrophysiologic monitoring of the recurrent laryngeal nerve. Laryngoscope. 1996;106:443–449. doi: 10.1097/00005537-199604000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Sun GH, DeMonner S, Davis MM. Epidemiological and economic trends in inpatient and outpatient thyroidectomy in the United States, 1996-2006. Thyroid. 2013;23:727–733. doi: 10.1089/thy.2012.0218. [DOI] [PubMed] [Google Scholar]
- 3.Kang SW, Lee SC, Lee SH, et al. Robotic thyroid surgery using a gasless, transaxillary approach and the da Vinci S system: the operative outcomes of 338 consecutive patients. Surgery. 2009;146:1048–1055. doi: 10.1016/j.surg.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 4.Thomusch O, Sekulla C, Walls G, et al. Intraoperative neuromonitoring of surgery for benign goiter. Am J Surg. 2002;183:673–678. doi: 10.1016/s0002-9610(02)00856-5. [DOI] [PubMed] [Google Scholar]
- 5.Barczynski M, Konturek A, Cichon S. Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg. 2009;96:240–246. doi: 10.1002/bjs.6417. [DOI] [PubMed] [Google Scholar]
- 6.Chan WF, Lang BH, Lo CY. The role of intraoperative neuromonitoring of recurrent laryngeal nerve during thyroidectomy: a comparative study on 1000 nerves at risk. Surgery. 2006;140:866–872. doi: 10.1016/j.surg.2006.07.017. discussion 872-863. [DOI] [PubMed] [Google Scholar]
- 7.Dralle H, Sekulla C, Haerting J, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery. 2004;136:1310–1322. doi: 10.1016/j.surg.2004.07.018. [DOI] [PubMed] [Google Scholar]
- 8.Higgins TS, Gupta R, Ketcham AS, et al. Recurrent laryngeal nerve monitoring versus identification alone on post-thyroidectomy true vocal fold palsy: a meta-analysis. Laryngoscope. 2011;121:1009–1017. doi: 10.1002/lary.21578. [DOI] [PubMed] [Google Scholar]
- 9.Horne SK, Gal TJ, Brennan JA. Prevalence and patterns of intraoperative nerve monitoring for thyroidectomy. Otolaryngol Head Neck Surg. 2007;136:952–956. doi: 10.1016/j.otohns.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 10.Sturgeon C, Sturgeon T, Angelos P. Neuromonitoring in thyroid surgery: attitudes, usage patterns, and predictors of use among endocrine surgeons. World J Surg. 2009;33:417–425. doi: 10.1007/s00268-008-9724-4. [DOI] [PubMed] [Google Scholar]
- 11. [Accessed January 18, 2014]; http://www.bls.gov/cpi.
- 12.Snyder SK, Sigmond BR, Lairmore TC, et al. The long-term impact of routine intraoperative nerve monitoring during thyroid and parathyroid surgery. Surgery. 2013;154:704–711. doi: 10.1016/j.surg.2013.06.039. discussion 711-703. [DOI] [PubMed] [Google Scholar]
- 13.Randolph GW, Dralle H, Abdullah H, et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope. 2011;121:S1–16. doi: 10.1002/lary.21119. [DOI] [PubMed] [Google Scholar]
- 14.Shindo M, Chheda NN. Incidence of vocal cord paralysis with and without recurrent laryngeal nerve monitoring during thyroidectomy. Arch Otolaryngol Head Neck Surg. 2007;133:481–485. doi: 10.1001/archotol.133.5.481. [DOI] [PubMed] [Google Scholar]
- 15.Chan WF, Lo CY. Pitfalls of intraoperative neuromonitoring for predicting postoperative recurrent laryngeal nerve function during thyroidectomy. World J Surg. 2006;30:806–812. doi: 10.1007/s00268-005-0355-8. [DOI] [PubMed] [Google Scholar]
- 16.Schneider R, Randolph GW, Sekulla C, et al. Continuous intraoperative vagus nerve stimulation for identification of imminent recurrent laryngeal nerve injury. Head Neck. 2013;35:1591–1598. doi: 10.1002/hed.23187. [DOI] [PubMed] [Google Scholar]
- 17.Sosa JA, Bowman HM, Tielsch JM, et al. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg. 1998;228:320–330. doi: 10.1097/00000658-199809000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gourin CG, Tufano RP, Forastiere AA, et al. Volume-based trends in thyroid surgery. Arch Otolaryngol Head Neck Surg. 2010;136:1191–1198. doi: 10.1001/archoto.2010.212. [DOI] [PubMed] [Google Scholar]