Abstract
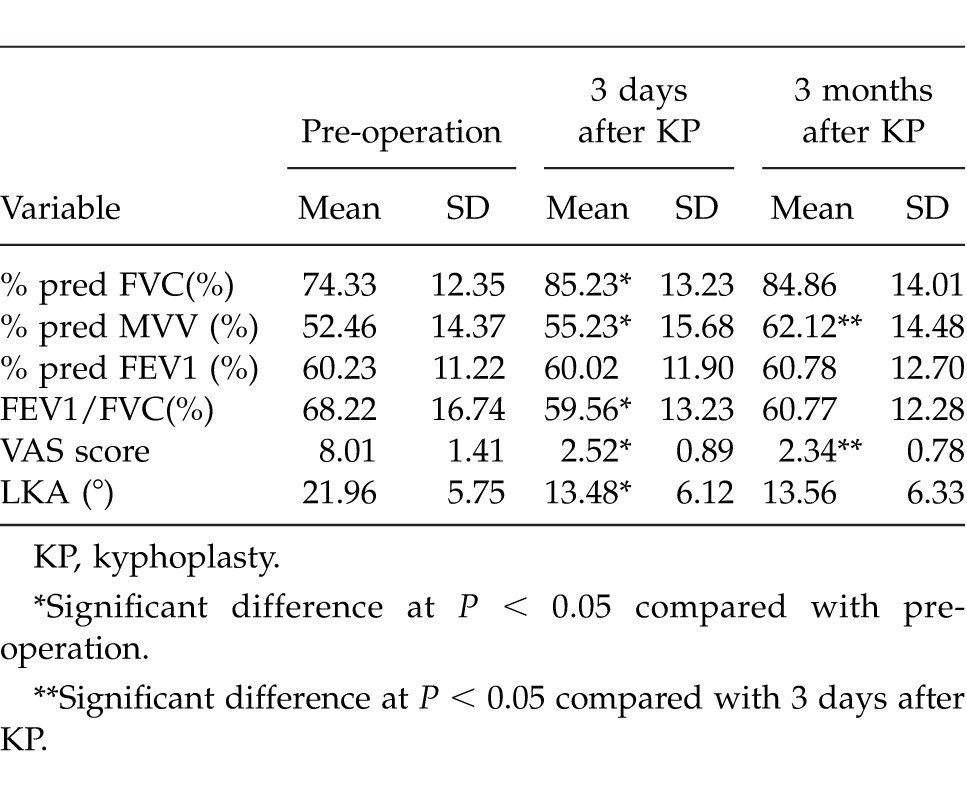
To investigate the changes in respiratory function of COPD patients with osteoporotic vertebral compression fractures (OVCFs) after kyphoplasty (KP). Pain scores, pulmonary function parameters (PFT), and local kyphotic angle (LKA) were measured in 31 older patients (25 women, 6 men) with OVCFs before, 3 days after and 3 months after kyphoplasty. The preoperative and postoperative (3 days, 3 months) PFT parameters were as follows: % pred FVC, 74.33 ± 12.35, 85.23.8 ± 13.23, and 84.86 ± 14.01; % pred FEV1, 60.23 ± 11.2, 60.02 ± 11.90, and 60.78 ± 12.70; FEV1/FVC ratio (%), 68.22 ± 16.74, 59.56 ± 13.23, and 60.77 ±12.28, % pred MVV 52.46 ± 14.37, 55.23 ± 15.68, and 62.12 ± 14.48, respectively. The preoperative mean VAS score was 8.01 ± 1.41 and significantly decreased to 2.52 ± 0.89 and 2.34 ± 0.78 at 3 days, 3 months after kyphoplasty, respectively. The preoperative local kyphotic angle degree was 21.96 ± 5.75°, significantly decreased to 13.48 ± 6.12° 3 days after KP, and maintained 3 month after KP. The decrease in the VAS scores correlated with the PFT parameters; however, there were no significant correlations between the PFT parameters and the LKA, the VAS scores and the LKA. Kyphoplasty under local anesthesia is a safety treatment for the COPD patients with OVCFS, and is able to improve the lung function impaired by OVCFs.
Key words: Chronic obstructive pulmonary disease, Osteoporotic vertebral compression fractures, Kyphoplasty, Pain, Kyphosis, Pulmonary function
Osteoporotic vertebral compression fractures (OVCFs), which are the most common complication of osteoporosis, especially in older women, are steadily increasing due to the aging population. Patients with OVCFs often suffer back pain and the collapse of the fractured vertebral body can lead to spinal kyphosis. Kyphosis has been linked to poor pulmonary function and an increased risk of mortality. Schlaich et al1 reported that pulmonary function is reduced in patients with spinal osteoporotic fractures in that both their vital capacity (VC) and forced expiratory volume were significantly diminished. Harrison et al2 reported reductions in vital capacity (VC) in OVCFs patients, with values ranging from 68% to 94% of predicted values. And the declines in pulmonary function were correlated with the degree of kyphosis.
The prevalence of osteoporosis in older patients with chronic obstructive pulmonary disease (COPD) is reported to be much higher than that in the age-matched elderly patients.3,4 The mechanisms of osteoporosis in COPD remain controversial. Less improvements in functional exercise capacity due to poor pulmonary function is associated with osteoporosis,5 and the pathogenic mechanisms in COPD is strongly interact with vitamin D deficiency.6
Kyphoplasty is a minimally invasive procedure to restore vertebral body anatomy, and internally stabilize OVCFs.7 Unlike vertebroplasty (VP), before the injection of PMMA a balloon is inserted into the vertebral body, leading to compression of cancellous bone, creation of a cavity, and if possible, realignment of the endplate of the vertebral body. After removal of the bone tamp, the injected PMMA fixes and stabilizes the fracture. Kyphoplasty not only has the advantage of improving or restoring vertebral height and kyphotic deformities, but can also decrease cement leakage and reduce the occurrence of new fracture.8 In a latest research, 45 patients who suffered osteoporotic fractures with middle column compromise were treated by BKP, the mean VAS improved significantly from pre- to postoperation (P < 0.05), and this improvement was sustained at the final follow-up which the mean follow-up period was 20.2 months.9 Maestretti et al10 reported a long follow-up about 10 years of kyphoplasty showing very good clinical and radiologic results.
Yang et al11 reported KP could partially improve the impaired lung function in patients with OVCFS, Dong et al12 reported an improvement of pulmonary function after both VP and KP. VP could improve restrictive ventilatory impairment in patients with moderate and severe COPD affected by OVCFs.13 There are few studies that evaluate the effect of deformity correction on the changes of respiratory function in COPD patients after KP. This study investigated the changes of respiratory function, spinal deformity, and pain scores in COPD patients with OVCFs after KP. It also attempted to find if the changes of pulmonary function are related to the spinal deformity correction and pain scores.
Materials and Methods
Patients
Thirty-one older patients affected by COPD [according the definition by The Global Initiative for Chronic Obstructive Lung Disease (GOLD)]14 with a total of 34 OVCFs in the thoracolumbar segment (T9:5; T11:7; T12:9; L1:9; L2:4) were studied. All fractures led to severe back pain that was resistant to conservative treatment. Potential subjects were excluded from participation if they had radicular pain or neurologic disorders.
Procedures
We explained fully to all patients about the purpose and procedures and obtained their consent for the operation. After routine operation preparations, each patient was given conscious sedation by intravenous analgesics. Then the patients were placed in the prone position on a carbon fiber radiolucent C-arm table. All operations were performed with the help of fluoroscopy using the C-arm percutaneously and under local anesthesia. KP procedures were performed by standard techniques. No operation was stopped because of the patient's intolerance of the procedure. The duration of the whole procedure was approximately 25–30 minutes. Each patient was mobilized 4 hours after the operation and all the patients were discharged on the next day (some of them were transferred to the physiotherapy departments).
Evaluation of pain
Pain intensity was evaluated on a visual analog scale (VAS) of 0 = no pain to 10 = severe pain. This test was done before kyphoplasty, 3 days after kyphoplasty, and 3 months after kyphoplasty.
Radiographic measures
The patients were tested 3 times—preoperatively and postoperatively after 3 days and 3 months after kyphoplasty—to obtain radiographs. All X-ray films were taken using standard radiographic techniques with the subject standing with her hands resting on a bar in front of the subject at shoulder level. The kyphosis were described by local kyphosis angle (LKA) in our study, the LKA was determined by the Cobb angle method on lateral radiographs, as the angle between the upper endplate of the uninvolved vertebra above the fractured level and the lower endplate of the uninvolved vertebra below the fractured level. The collapse of the fractured vertebral body can lead to an increase in LKA (Fig. 1; Fig 2).15
Fig. 1.
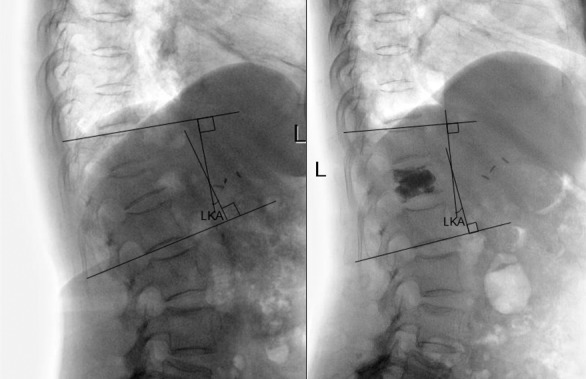
The LKA was measured from the upper endplate of the uninvolved vertebra above the fractured level to the lower endplate of the uninvolved vertebra below the fractured level.
Fig. 2.
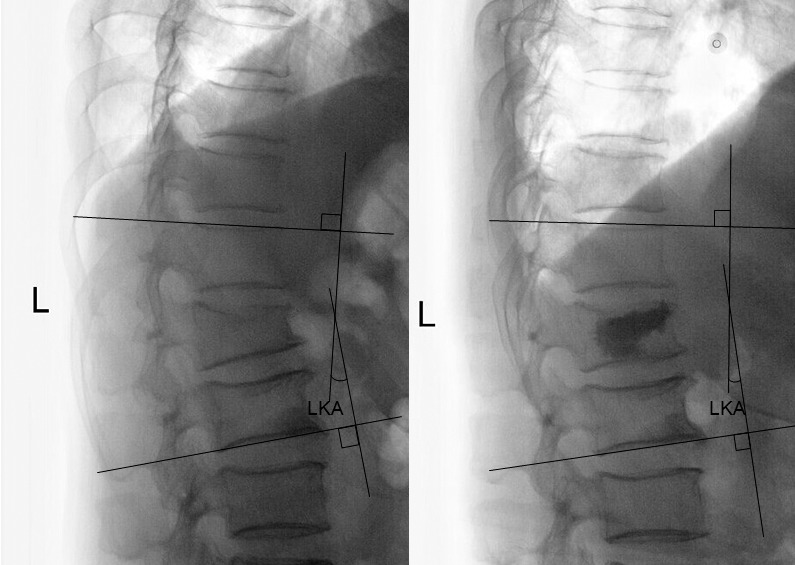
The LKA was improved and the height of the vertebra was restored after KP.
Pulmonary function tests
Percent predicted forced expiratory volume in 1 second (% pred FEV1), % predicted forced vital capacity (% pred FVC), % predicted maximum voluntary ventilation (% pred MVV), FEV1/FVC ratio were selected as the parameters of pulmonary function. The parameters of each patient were measured 3 times during different periods—before, 3 days after, and 3 months after operation by the same pulmonary function laboratory technician.
Statistical analysis
All data were expressed as mean ± standard deviation (SD). Paired t tests were used to compare parameters of patients before and after KP. The correlations between the decreased values of VAS score and the improvement of respiratory function, the local kyphotic angle, and the parameters of pulmonary function were evaluated by Pearson correlation test. The results were considered significant when a P value was less than 0.05. All statistics were performed using SPSS 19.0 software (SPSS Inc, Chicago, Illinois).
Results
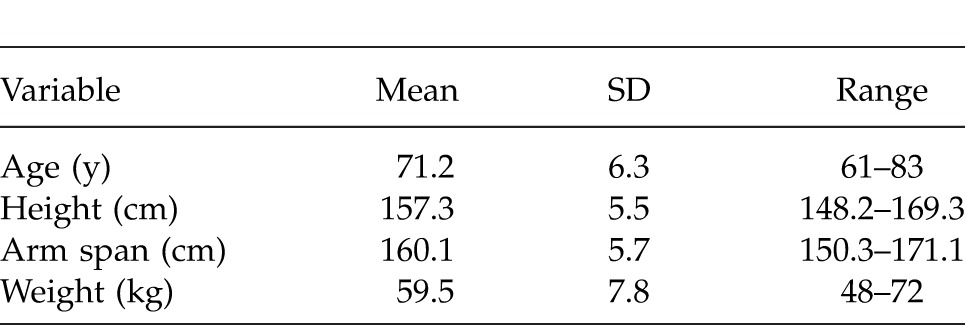
Characteristics of patients
Three months of follow-up were completed for all 31 patients. Mean values of age, height, arm span, and weight of the patients are presented in Table 1. The mean measured height of subjects was 156.7 cm and the mean arm span was 158.7 cm, representing, on average, a 2.0-cm reduction of height in patients.
Table 1.
Characteristics of patients
Pain and radiographic measures
According to the measurements 3 days after operation, pain evaluation, and spinal sagittal alignment improved significantly. Mean improvement in LKA was 8.19°. The mean vertebral body height restorations of the anterior, middle, and posterior portions of the vertebral body were 4.20, 4.61, and 1.1 mm after KP. Three months after the procedures, the kyphosis restored had not changed. All patients experienced pain relief after the operations. The preoperative mean pain score was 8.26, whereas it decreased to 2.77 after 3 days after KP. Three months after KP, the mean pain score continued to improve compared with the 3 days postoperative recording (P < 0.05).
Changes of pulmonary function
There was a statistically significant difference in the mean values of FVC and MVV between before and 3 days after operation. Additionally, there was a significant difference in the mean value of % pred MVV between 3 days and 3 months after KP, whereas there was no difference in % pred FVC. The % pred FEV1 did not change significantly throughout the follow-up. The results of the respiratory function measures are presented in Table 2.
Table 2.
Changes of pulmonary function, pain score and LKA degree
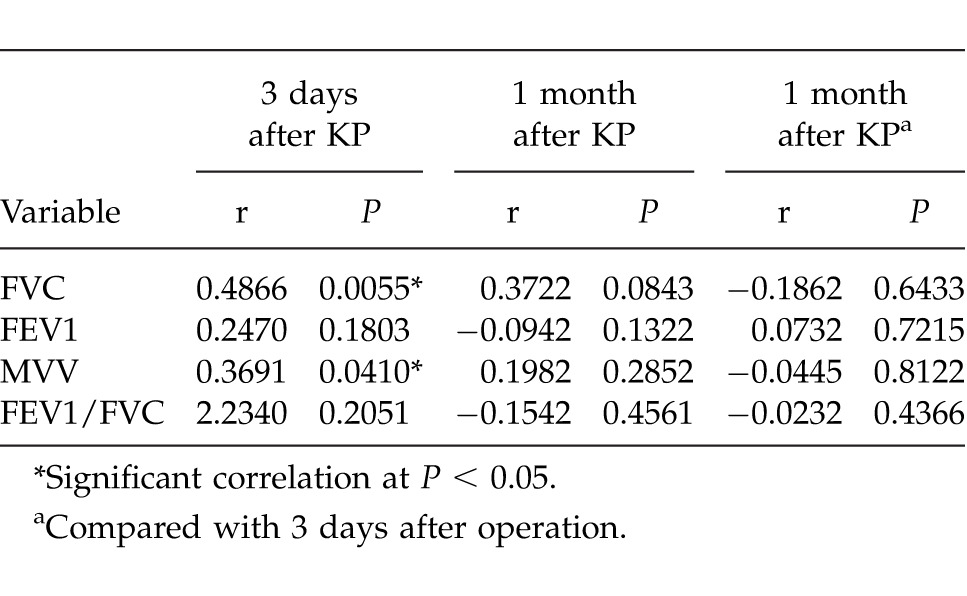
Correlation analysis of pulmonary function
Pearson correlation analysis revealed that the decrease in the VAS score correlated with the improvement of % pred FVC and % pred MVV 3 days after KP. However, 3 months later, the correlation between the decrease in VAS score and the changes in lung function parameters was no longer significant (Table 3). The VAS values had no significant correlation with the LKA. LKA did not have a significant correlation with any parameters of pulmonary function.
Table 3.
Correlation of the decreased values of pain scores and the improvement of pulmonary function
Discussion
Previous studies confirmed that the patients with COPD are often more likely to suffer from osteoporosis and subsequent vertebral fracture.3 Kyphosis and back pain due to OVCFs may reduce the patient's chest cavity, and respiratory muscle strength, further compromising lung function.4 Prevention of OVCFs can delay COPD progression reducing mortality in elderly patients with COPD.
Rapid regression of pain, restoration of vertebral kyphosis and less cement leakage are especially important advantages of KP.8 BKP improves patient quality of life and results in a significantly reduction in LKA.11,12,16 Although KP poses low surgical risk, the elderly patient population presents substantial anesthetic risk because of multiple comorbidities. COPD is one of the most common and severe comorbidities that require careful preoperative medical assessment and optimization.17 Some authors have used general anesthesia pointed out that this form of anesthesia was chosen because it was felt that the elderly patient would not tolerate prone positioning.18,19 Imani et al20 reported a cardiorespiratory compromised patient suffering painful vertebral compression fracture, after kyphoplasty under local anesthesia made by lidocaine 1%, the pain was decreased quickly the patient was discharged next day with overall good condition and without any neurologic complications. Cagli et al21 studied 91 patients with a mean age of 67 who underwent kyphoplasty or vertebroplasty under local anesthesia, they pointed out that elderly patients can therefore be protected from the complications of general anesthesia and mobilized and discharged earlier and KP may be performed on an outpatient basis under local anesthesia with minimal sedation. In our study, all operations were completed under local anesthesia without any intolerance of the patients. No complications of anesthesia were occurred during the follow-up.
In accordance with these studies,12,22 our study has shown that KP could deliver a good result of pain reduction with a significantly decrease of VAS score and LKA degree 3 days after the operation, and without further significant modification 3 months later. Three days after the procedures FVC and MVV were significantly increased, and MVV went on to improve remarkably 3 months after the procedures. VC and FEV1 values did not change significantly over the whole follow-up period. It is known that MVV is partially dependent on respiratory muscle strength and endurance. In another trial of COPD patients, Masala et al13 observed a progressive improvement of spirometric parameters such as VC and FVC 1 week after VTP, with further gradual improvement over the entire follow-up period.
Obviously, pain relief and improvement of mobility and function after KP is immediate.22 In our study the improvement in pulmonary function was related to the decrease of VAS values significantly. Three days after KP, the relative pulmonary parameters were FVC and MVV. Yang et al11 also showed that the improvement in pulmonary function was affected by pain reduction. They pointed out that back pain was relieved after KP, which could have helped improve the strength and endurance of the respiratory pump. In our viewpoint, the FEV1 and FVC values reflect the respiratory muscle strength while the MVV values reflect the respiratory muscle endurance.23 Because of back pain, all patients in our study were unable to change their positions even in bed by themselves and to take a deep breath. According to a recent study of the relationship between the pain and the voluntary control of respiration, pain ratings were significantly lower during inspiration compared with expiration.24 When asked to do deep breathing, COPD patients with severe back pain still can take the forced expiration in 1 second, which may be normal as usual, but had a limited respiration function throughout the whole process due to the pain. So, the limitation could be treated by the pain relief. That may explain that the FEV1 did not change significantly during the follow-up, and the improvement of FEV and MVV were related to the decrease of pain significantly after 3 days. After 3 months, although both MVV and pain values improved compared with 3 days, the correction between the decrease of VAS score and the improvement of MVV is not significant. Patients were encouraged to have more activity, which may play a more important role in the enhancement of respiratory muscle endurance than pain relief 3 months later. Although the FEV1/FVC decreased immediately after the kyphoplasty, it suggested that the mechanism leading to an improvement in pulmonary function is more likely to be a correction process of restrictive lung disease.25
The radiographic outcomes showed a restoration the height of the vertebral body and a decrease of kyphosis after KP. There is an argument about the relationship between the back pain and the severity of the kyphosis.11,12,26 Our study supported that LKA did not have a significant correlation with the VAS score. Meanwhile, the decrease of LKA did not have a significant correlation with any parameter of pulmonary function. In another trial of 72 patients (85 vertebrae) who underwent percutaneous vertebroplasty for thoracic osteoporotic compression fractures,21 pulmonary function was improved and pain was relieved immediately after vertebroplasty although the kyphotic deformity was not corrected. Some studies27,28 also supported that the reduction of pulmonary function is not related to the spine deformity.
Regarding the use of KP, in addition to the considerations listed above, KP procedure could improve the quality of life compared with conservative therapy, and has a further advantage in terms of height restoration and decrease of cement leakage, but has a higher overall coat compared with VP.29 Although the correction of kyphosis seemed to be irrelevant with the pulmonary function, patients with less kyphosis could obtain more benefit such as increased activity and lower incidence of other complications.30,31
In conclusion, although the most important goal of KP is to alleviate pain, this study clarified that KP also improve the impaired lung function which is directly related to the mortality and the quality of life of the COPD patients. KP effectively improved back pain and the improvement of pulmonary function correlated with pain relief. And the correction of kyphosis after KP is immediate and sustained, it is considered an irrelevant factor or of the improvement in pulmonary function and pain condition.
References
- 1.Schlaich C, Minne HW, Bruckner T, Wagner G, Gebest HJ, Grunze M, et al. Reduced pulmonary function in patients with spinal osteoporotic fractures. Osteoporos Int. 1998;8(3):261–267. doi: 10.1007/s001980050063. [DOI] [PubMed] [Google Scholar]
- 2.Harrison RA, Siminoski K, Vethanayagam D, Majumdar SR. Osteoporosis-related kyphosis and impairments in pulmonary function: a systematic review. J Bone Miner Res. 2007;22(3):447–457. doi: 10.1359/jbmr.061202. [DOI] [PubMed] [Google Scholar]
- 3.Graat-Verboom L, Smeenk FW, van den Borne BE, Spruit MA, Jansen FH, van Enschot JW, et al. Progression of osteoporosis in patients with COPD: A 3-year follow up study. Respir Med. 2012;106(6):861–870. doi: 10.1016/j.rmed.2011.12.020. [DOI] [PubMed] [Google Scholar]
- 4.Xiaomei W, Hang X, Lingling L, Xuejun L. Bone metabolism status and associated risk factors in elderly patients with chronic obstructive pulmonary disease (COPD) Cell Biochem Biophys. 2014;70(1):129–134. doi: 10.1007/s12013-014-9868-9. [DOI] [PubMed] [Google Scholar]
- 5.Hornikx M, Van Remoortel H, Demeyer H. Marcal Camillo CA, Decramer M, Janssens W et al. The influence of comorbidities on outcomes of pulmonary rehabilitation programs in patients with COPD: a systematic review. Biomed Res Int. 2013;2013:146148. doi: 10.1155/2013/146148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Janssens W, Mathieu C, Boonen S, Decramer M. Vitamin D deficiency and chronic obstructive pulmonary disease: a vicious circle. Am J Respir Crit Care Med. 2009;179(8):630–663. doi: 10.1164/rccm.200810-1576PP. [DOI] [PubMed] [Google Scholar]
- 7.Papanastassiou ID, Filis A, Gerochristou MA, Vrionis FD. Controversial issues in kyphoplasty and vertebroplasty in osteoporotic vertebral fractures. Biomed Res Int. 2014;2014:934206. doi: 10.1155/2014/934206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsieh MK, Chen LH, Chen WJ. Current concepts of percutaneous balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures: evidence-based review. Biomed J. 2013;36(4):154–161. doi: 10.4103/2319-4170.112544. [DOI] [PubMed] [Google Scholar]
- 9.Gan M, Zou J, Zhu X, Wang G, Yang H. Balloon kyphoplasty for osteoporotic spinal fractures with middle column compromise. Injury. 2014;45(10):1539–1544. doi: 10.1016/j.injury.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 10.Maestretti G, Sutter P, Monnard E, Ciarpaglini R, Wahl P, Hoogewoud H, et al. A prospective study of percutaneous balloon kyphoplasty with calcium phosphate cement in traumatic vertebral fractures: 10-year results. Eur Spine J. 2014;23(6):1354–1360. doi: 10.1007/s00586-014-3206-1. [DOI] [PubMed] [Google Scholar]
- 11.Yang HL, Zhao L, Liu J, Sanford CG, Jr, Chen L, Tang T, et al. Changes of pulmonary function for patients with osteoporotic vertebral compression fractures after kyphoplasty. J Spinal Disord Tech. 2007;20(3):221–225. doi: 10.1097/01.bsd.0000211273.74238.0e. [DOI] [PubMed] [Google Scholar]
- 12.Dong R, Chen L, Gu Y, Han G, Yang H, Tang T, et al. Improvement in respiratory function after vertebroplasty and kyphoplasty. Int Orthop. 2009;33(6):1689–1694. doi: 10.1007/s00264-008-0680-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Masala S, Magrini A, Taglieri A, Nano G, Chiaravalloti A, Calabria E, et al. Chronic obstructive pulmonary disease (COPD) patients with osteoporotic vertebral compression fractures (OVCFs): improvement of pulmonary function after percutaneous vertebroplasty (VTP) Eur Radiol. 2014;24(7):1577–1585. doi: 10.1007/s00330-014-3165-2. [DOI] [PubMed] [Google Scholar]
- 14.Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. 2011 (revised. Available at: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2011_Feb21_pdf. Accessed September 16, 2012. [Google Scholar]
- 15.Phillips FM, Ho E, Campbell-Hupp M, McNally T. Todd Wetzel F, Gupta P. Early radiographic and clinical results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Spine. 2003;28(19):2260–2265. doi: 10.1097/01.BRS.0000085092.84097.7B. [DOI] [PubMed] [Google Scholar]
- 16.Meirhaeghe JV, Bastian L, Boonen S, Ranstam J, Tillman JB, Wardlaw D. A randomized trial of balloon kyphoplasty and nonsurgical management for treating acute vertebral compression fractures. Spine. 2013;38(12):971–983. doi: 10.1097/BRS.0b013e31828e8e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dronkers JJ, Chorus AM, van Meeteren NL, Hopman-Rock M. The association of pre-operative physical fitness and physical activity with outcome after scheduled major abdominal surgery. Anaesthesia. 2013;68(1):67–73. doi: 10.1111/anae.12066. [DOI] [PubMed] [Google Scholar]
- 18.Luginbühl M. Percutaneous vertebroplasty, kyphoplasty and lordoplasty: implications for the anesthesiologist. Curr Opin Anaesthesiol. 2008;21(4):504–513. doi: 10.1097/ACO.0b013e328303be62. [DOI] [PubMed] [Google Scholar]
- 19.Health Quality Ontario. Balloon kyphoplasty: an evidence-based analysis. Ont Health Technol Assess Ser. 2004;4(12):1–45. [PMC free article] [PubMed] [Google Scholar]
- 20.Imani F, Gharaei H, Rahimzadeh P, Saffarian Z. Management of painful vertebral compression fracture with kyphoplasty in a sever cardio-respiratory compromised patient. Anesth Pain Med. 2012;2(1):42–45. doi: 10.5812/aapm.5030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cagli S, Isik HS, Zılelı M. Vertebroplasty and kyphoplasty under local anesthesia: review of 91 patients. Turk Neurosurg. 2010;20(4):464–469. doi: 10.5137/1019-5149.JTN.2954-10.0. [DOI] [PubMed] [Google Scholar]
- 22.Civelek E, Cansever T, Yilmaz C, Kabatas S, Gülşen S, Aydemir F, et al. The retrospective analysis of the effect of balloon kyphoplasty to the adjacent-segment fracture in 171 patients. J Spinal Disord Tech. 2014;27(2):98–104. doi: 10.1097/bsd.0b013e31824e9b98. [DOI] [PubMed] [Google Scholar]
- 23.Vieira PJ, Chiappa AM, Cipriano G, Jr, Umpierre D, Arena R, Chiappa GR. Neuromuscular electrical stimulation improves clinical and physiological function in COPD patients. Respir Med. 2014;108(4):609–620. doi: 10.1016/j.rmed.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 24.Arsenault M, Ladouceur A, Lehmann A, Rainville P, Piché M. Pain modulation induced by respiration: phase and frequency effects. Neuroscience. 2013;252:501–511. doi: 10.1016/j.neuroscience.2013.07.048. [DOI] [PubMed] [Google Scholar]
- 25.Lee JS, Kim KW, Ha KY. The effect of vertebroplasty on pulmonary function in patients with osteoporotic compression fractures of the thoracic spine. J Spinal Disord Tech. 2011;24(2):E11–E15. doi: 10.1097/BSD.0b013e3181dd812f. [DOI] [PubMed] [Google Scholar]
- 26.Ryan PJ, Blake G, Herd R, Fogelman I. A clinical profile of back pain and disability in patients with spinal osteoporosis. Bone. 1994;15:27–30. doi: 10.1016/8756-3282(94)90887-7. [DOI] [PubMed] [Google Scholar]
- 27.Patel J, Walker JL, Talwalkar VR, Iwinski HJ, Milbrandt TA. Correlation of spine deformity, lung function, and seat pressure in spina bifida. Clin Orthop Relat Res. 2011;469(5):1302–1307. doi: 10.1007/s11999-010-1687-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tanigawa N, Kariya S, Komemushi A, Nakatani M, Yagi R, Sawada S. Added value of percutaneous vertebroplasty: effects on respiratory function. AJR Am J Roentgenol. 2012;198(1):51–54. doi: 10.2214/AJR.11.6730. [DOI] [PubMed] [Google Scholar]
- 29.Eck JC, Nachtigall D, Humphreys SC, Hodges SD. Comparison of vertebroplasty and balloon kyphoplasty for treatment of vertebral compression fractures: a meta-analysis of the literature. Spine J. 2008;8(3):488–497. doi: 10.1016/j.spinee.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 30.Kim WJ, Kang JW, Kang SI, Sung HI, Park KY, Park JG. Factors affecting clinical results after corrective osteotomy for lumbar degenerative kyphosis. Asian Spine J. 2010;4(1):7–14. doi: 10.4184/asj.2010.4.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tsuchie H, Fukata C, Takahashi K, Miyakoshi N, Kobayashi A, Kasukawa Y, et al. Impact of lumbar kyphosis on gastric myoelectrical activity and heart rate variability in a model using flexion posture in healthy young adults. Biomed Res. 2011;32(4):271–278. doi: 10.2220/biomedres.32.271. [DOI] [PubMed] [Google Scholar]


