Abstract
We herein describe the case of an adult with a complicated huge lymphangioma of the small bowel mesentery. Computed tomography (CT) confirmed a 45 × 30 × 14 cm multiple and separate, mixed and solid cystic tumor without enhancement by contrast medium in the abdominal cavity. Mesenteric CT angiography with three-dimensional (3D) reconstruction showed that the tumor did not involve the first jejunal artery, although the tumor did involve the subsequent jejunal and ileal arteries and the corresponding segment of the small bowel. Under anatomic guidance based on mesenteric CT angiography with 3D reconstruction, we were able to successfully excise the tumor. Mesenteric lymphangioma should be excised even when the tumor is asymptomatic. Mesenteric CT angiography with 3D reconstruction is useful for the surgical treatment of huge mesenteric tumors.
Key words: Mesenteric lymphangioma, CT angiography
Lymphangioma occurs mainly in children, with 80% to 90% of cases being diagnosed in the first year of life, and more than 95% of lymphangiomas are found in the head, neck, and axillary region.1,2 On the other hand, intra-abdominal mesenteric lymphangioma is an uncommon tumor, but of the intraperitoneal sites, the small bowel mesentery is the most common site (70% of cases).2 On occasion, mesenteric lymphangioma has been reported to grow to an enormous size and to behave aggressively in an invasive manner.2–8
We herein describe the case of an adult with a huge lymphangioma of the small bowel mesentery—the largest one reported thus far—that was complicated with intestinal obstruction and infection.2–8 This report emphasizes the fact that the primary treatment for lymphangioma is radical surgical excision, even when the tumor is asymptomatic. In addition, mesenteric computed tomography (CT) angiography with three-dimensional (3D) reconstruction was useful in investigating the spread of the involved small bowel mesentery and in planning the surgical procedure in our case. We therefore discuss the role of mesenteric CT angiography with 3D reconstruction when planning and performing surgery for a huge abdominal tumor.
Case Report
A 34-year-old man presented to a previous hospital with abdominal pain and fever, and he was transferred to our hospital for the treatment of intestinal obstruction and sepsis caused by a huge lymphangioma. He had a medical history of Batter syndrome, and a huge abdominal tumor had been pointed out when he was age 18 years, which had been diagnosed as a lymphangioma by needle aspiration of the lymphatic fluid contained within it.
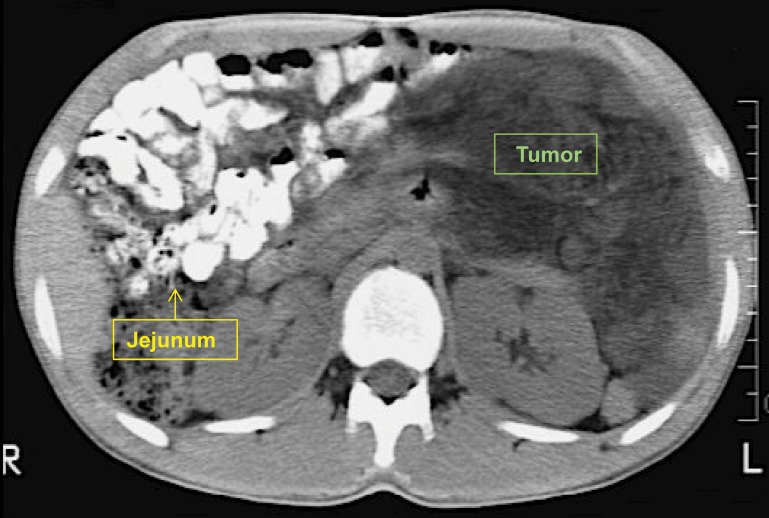
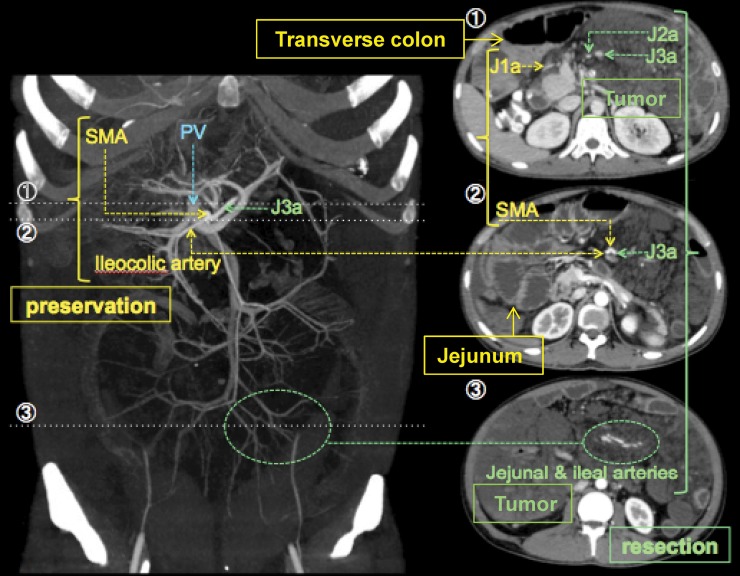
He presented with some abdominal swelling that was not severe, and the previous doctor did not recommend that he undergo a surgical excision, so he had been followed up until his current presentation. A physical examination following his transfer to our hospital revealed distension and tenderness of the whole abdomen, and no bowel sounds were audible. Laboratory data showed a high C-reactive protein value of 38 mg/dL and a prolonged coagulation time; thus, we diagnosed sepsis and disseminated intravascular coagulopathy caused by intestinal obstruction and ischemia. CT confirmed the presence of a large 45 × 30 × 14 cm multiple and separate, mixed and solid cystic tumor without enhancement by contrast medium in the abdominal cavity (Fig. 1). The tumor compressed some segments of the small intestine, which were not involved by the tumor, to the right upper quadrant of the peritoneal cavity, but we could not identify the range of normal small intestine (Fig. 2). Mesenteric CT angiography and processing of the images with a rendering software program to reconstruct a 3D model of the mesenteric vessels helped us understand that the tumor did not involve the first jejunal artery, although the tumor did involve the subsequent jejunal and ileal arteries and the corresponding segment of the small bowel (Fig. 3). In addition, these studies showed that the ileocolic artery and colic arteries diverging from the superior and inferior mesenteric arteries were not involved. Thus, under the guidance of mesenteric CT angiography with 3D reconstruction, we were able to plan a surgical procedure for radical excision of the tumor and the corresponding segment of the small intestine.
Fig. 1.
CT demonstrated that a huge multi-separate mixed solid and cystic tumor without enhancement by contrast medium occupied the peritoneal cavity.
Fig. 2.
The tumor compressed some segments of the small intestine, which were not involved by the tumor, to the right upper quadrant of the peritoneal cavity.
Fig. 3.
Mesenteric CT angiography with 3D reconstruction clearly demonstrated that the first jejunal artery and ileocolic artery were not involved by the tumor.
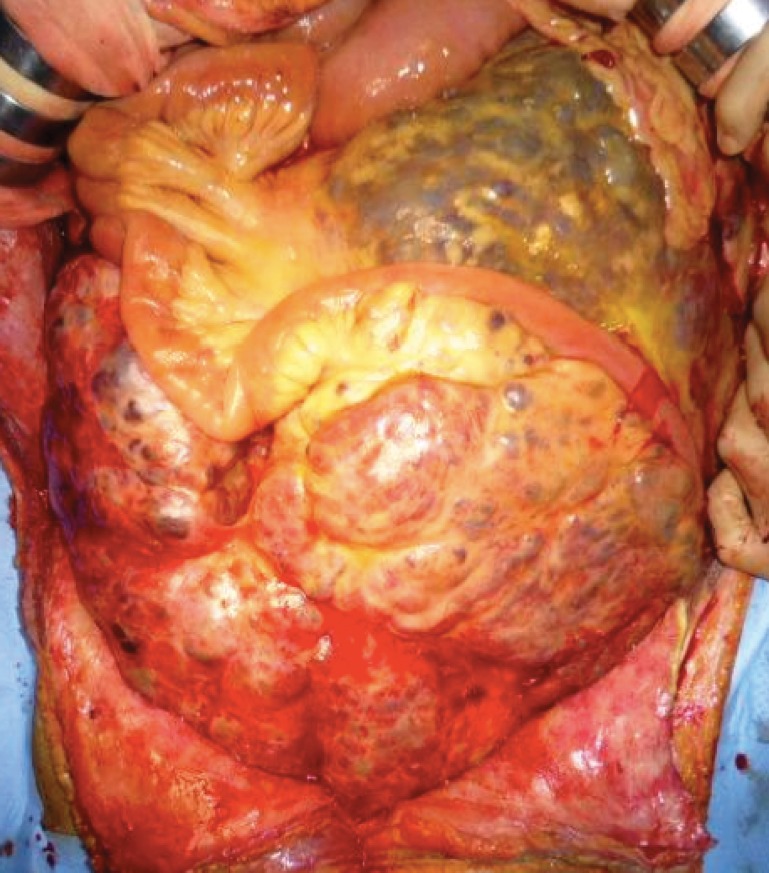
The patient was listed for an elective surgical intervention after 13 days of treatment for sepsis and disseminated intravascular coagulopathy. Upon opening the peritoneal cavity, a huge, yellowish cystic tumor of soft consistency, measuring 40 cm in diameter, was found (Fig. 4). Abscess formation was found in the tumor, the jejunum, and its corresponding mesenteric tissue. The tumor was very close to the superior mesenteric artery and vein, but we could dissect among them. Based on the preoperative plan developed using the guidance of mesenteric CT angiography with 3D reconstruction, we were able to successfully excise the tumor while preserving the first jejunal artery and ileocolic artery with the segments of corresponding small intestine. Approximately 30 cm of the ileum from the Treitz ligament, as well as 120 cm of the ileum from the ileocecal valve, could be preserved, and a jejunoileal anastomosis was required for intestinal continuity.
Fig. 4.
A huge, yellowish cystic tumor of soft consistency occupied the peritoneal cavity.
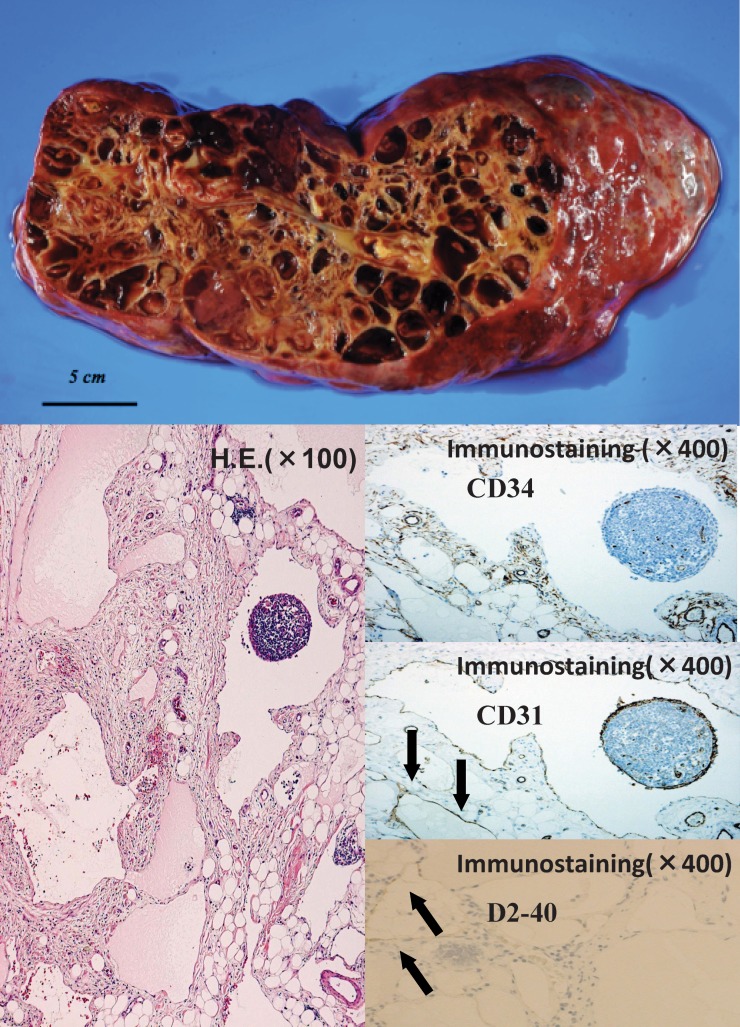
Macroscopically, the mucosal surface of the small intestine was intact, and the cystic tumor, which was 45 × 30 × 14 cm in size and weighed 9800 g, had many septa and contained yellowish, transparent fluid (Fig. 5). A histologic examination revealed variably sized, markedly dilated lymphatic channels in the mesentery, and all parts of the intestinal mucosa were covered with a single, flat layer of endothelial cells. These endothelial cells were positive for CD31 and D2-40 but not for CD34, and the findings were consistent with lymphangioma.
Fig. 5.
Macroscopically, the cystic tumor had many septa and contained yellowish, transparent fluid. A histologic examination revealed variably sized, markedly dilated lymphatic channels in the mesentery, and all parts of the intestinal mucosa were covered with a single, flat layer of endothelial cells. These endothelial cells were positive for CD31 and D2-40, but not for CD34.
The patient made an uneventful recovery and was discharged home on the 14th postoperative day. A follow-up examination at 15 months revealed that he was fit and healthy and completely symptom-free.
Discussion
The primary treatment for mesenteric lymphangioma is radical surgical excision, even when asymptomatic, because of its potential to grow enormously and to cause significant mortality.2–8 Our case also presented with a life-threatening complication of intestinal obstruction and sepsis associated with disseminated intravascular coagulopathy after the patient had been followed up for 16 years without any symptoms. Intestinal obstruction and ischemia related to mesenteric lymphangioma can be induced by compression or traction by the mass. Thus, this report also emphasizes the fact that mesenteric lymphangioma can grow to a huge size and lead to life-threatening complications. It is also necessary to consider the fact that mesenteric lymphangioma may exist even when patients are asymptomatic.
As mentioned above, the optimal treatment for mesenteric lymphangioma is radical complete excision, because incomplete resection may lead to recurrence.5,9,10 If mesenteric lymphangioma infiltrates the intestine, en bloc resection of the involved intestine is required. CT can give precise information about the size, anatomic location, extent of cysts, and involved structures for the surgical intervention.4,11 In this case, the tumor was huge, it occupied the abdominal cavity, and it was very difficult to judge the spread of the involved segment of the mesentery and corresponding small intestine. Although standard CT has always allowed the identification of the mesenteric arteries and veins, it is limited in its ability to adequately image small branches and complex anatomy. Therefore, we performed mesenteric CT angiography with 3D reconstruction for the present case. It clearly demonstrated the involved segment, and we could plan a radical excision of the tumor with the segments of corresponding small intestine. CT angiography with 3D reconstruction of the mesenteric vasculature is widely used in vascular surgery and interventional radiology for diagnosing and planning the treatment of median arcuate ligament syndrome, as well as for mesenteric ischemia, aneurysms, and vasculitis.12,13 Recently, in the field of gastrointestinal surgery, prior knowledge of the mesenteric vascular anatomy obtained using mesenteric CT angiography with 3D reconstruction helped surgeons to accurately plan the surgical strategy for laparoscopic colorectal surgery, which led to a reduced risk of complications when surgeons were faced with anatomic anomalies.14 In addition, magnetic resonance angiography also provided an excellent noninvasive screening technique for the anatomic evaluation of the mesenteric arteries, and CT angiography has higher spatial resolution and faster acquisition times, allowing for the assessment of the peripheral visceral branches of mesenteric arteries with greater accuracy than MR angiography.15 Thus, we believe that mesenteric CT angiography with 3D reconstruction is useful for planning the surgical procedure for a huge mesenteric tumor, as was observed in our case.
In conclusion, mesenteric lymphangioma should be existed even when it is asymptomatic because of its potential for massive and invasive growth. Mesenteric CT angiography with 3D reconstruction is useful for planning the surgical treatment of a huge mesenteric tumor, as demonstrated by our case.
References
- 1.Roisman I, Manny J, Fields S, Shiloni E. Intra-abdominal lymphangioma. Br J Surg. 1989;76(5):485–489. doi: 10.1002/bjs.1800760519. [DOI] [PubMed] [Google Scholar]
- 2.Rieker RJ, Quentmeier A, Weiss C, Kretzschmar U, Amann K, Mechtersheimer G, et al. Cystic lymphangioma of the small-bowel mesentery: case report and review of the literature. Pathol Oncol Res. 2000;6(2):146–148. doi: 10.1007/BF03032366. [DOI] [PubMed] [Google Scholar]
- 3.Tsukada H, Takaori S, Ishiguro S, Tsuda T, Ota S, Yamamoto T. Giant cystic lymphangioma of the small bowel mesentery: report of a case. Surg Today. 2002;32(8):734–737. doi: 10.1007/s005950200138. [DOI] [PubMed] [Google Scholar]
- 4.Jang JH, Lee SL, Ku YM, An CH, Chang ED. Small bowel volvulus induced by mesenteric lymphangioma in an adult: a case report. Korean J Radiol. 2009;10(3):319–322. doi: 10.3348/kjr.2009.10.3.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wani I. Mesenteric lymphangioma in adult: a case series with a review of the literature. Dig Dis Sci. 2009;54(12):2758–2762. doi: 10.1007/s10620-008-0674-3. [DOI] [PubMed] [Google Scholar]
- 6.Siddique K, Bhandari S, Basu S. Giant mesenteric lymphangioma: a rare cause of a life-threatening complication in an adult. BMJ Case Rep. 2010;pii:bcr0420102896. doi: 10.1136/bcr.04.2010.2896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Limdi JK, Mehdi S, Sapundzieski M, Manu M, Abbasi AM. Cystic lymphangioma of the mesocolon. J Gastrointest Surg. 2010;14(9):1459–1461. doi: 10.1007/s11605-010-1176-0. [DOI] [PubMed] [Google Scholar]
- 8.Eisawi A, Otter M, Asha M, Al-Temimi A. A case of a giant cystic lymphangioma mimicking acute appendicitis. Am R Coll Surg Engl. 2012;94(1):e24–e25. doi: 10.1308/003588412X13171221499144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poon MCM, Lee DWH, Wong PK, Chan ACW. Mesenteric cystic lymphangioma presented with small bowel volvulus. Ann Coll Surg Hong Kong. 2001;5(2):127–128. [Google Scholar]
- 10.Su CM, Yu MC, Chen HY, Tseng JH, Jan YY, Chen MF. Single-centre results of treatment of retroperitoneal and mesenteric cystic lymphangioma. Dig Surg. 2007;24(3):181–185. doi: 10.1159/000102896. [DOI] [PubMed] [Google Scholar]
- 11.Munechika H, Honda M, Kushihashi T, Koizumi K, Gokan T. Computed tomography of retroperitoneal cystic lymphangiomas. J Comput Assist Tomogr. 1987;11(1):116–119. doi: 10.1097/00004728-198701000-00023. [DOI] [PubMed] [Google Scholar]
- 12.Horton KM, Elliot K. Volume-rendered 3D CT of the mesenteric vasculature: normal anatomy, anatomic variants, and pathologic conditions. RadioGraphics. 2002;22(1):161–172. doi: 10.1148/radiographics.22.1.g02ja30161. [DOI] [PubMed] [Google Scholar]
- 13.Smith CL, Horton KM, Fishman EK. Mesenteric CT angiography: a discussion of techniques and selected applications. Tech Vasc Interventional Rad. 2006;9(4):150–155. doi: 10.1053/j.tvir.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Mari FS, Nigri G, Pancaldi A, De Cecco CN, Gasparrini M. Role of CT angiography with three-dimensional reconstruction of mesenteric vessels in laparoscopic colorectal resections: a randomized controlled trial. Surg Endosc. 2013;27(6):2058–2067. doi: 10.1007/s00464-012-2710-9. [DOI] [PubMed] [Google Scholar]
- 15.Shih MC, Hagspiel KD. CTA and MRA in mesenteric ischemia: part 1, role in diagnosis and differential diagnosis. AJR Am J Roentgenol. 2007;188(2):452–461. doi: 10.2214/AJR.05.1167. [DOI] [PubMed] [Google Scholar]