Abstract
Purpose
This multi-institutional phase II trial assessed the activity and tolerability of the anti-metastatic A6 peptide that binds CD44 in patients with persistent or recurrent epithelial ovarian, fallopian tube, or primary peritoneal carcinoma (EOC/FTC/PPC).
Patients and Methods
Women with persistent or recurrent EOC/FTC/PPC were eligible for participation if they had measurable disease defined by RECIST criteria, good performance status, and good overall organ function. Patients must have received one prior platinum-based chemotherapeutic regimen and were allowed to have received one additional cytotoxic regimen for the management of recurrent or persistent disease. Women received a 150 mg twice daily subcutaneous dose of A6 and continued on treatment until disease progression or unacceptable toxicity. Primary measures of clinical efficacy were objective tumor response and progression-free survival (PFS) at 6 months. The association of CD44 in archival tissue specimens with clinical outcome was investigated.
Results
Thirty-one eligible patients were evaluated. No responses were observed. Two patients (6.5%) were progression free for at least 6 months. The median PFS was 2.0 months, and median overall survival has not yet been reached. One patient died of hemorrhage which was possibly study related. There were no grade 4 toxicities. The most common grade 3 toxicities were constitutional (2/31; 6.5%). Archival specimens were available for 27 patients, and 5 (18.5%) were CD44 positive by immunohistochemistry. CD44 expression was not associated with the 6-month PFS (p=0.342).
Conclusion
A6 was well tolerated but had minimal activity in patients with persistent or recurrent EOC/FTC/PPC.
INTRODUCTION
Ovarian cancer is the fifth leading cause of cancer related death in women in the United States [1]. The majority of those with advanced stage disease will recur and virtually all of those will die of their disease. Front-line chemotherapy with a platinum and taxane is standard, but a wide variety of agents are commonly used for second and subsequent lines of chemotherapy. Response to these agents can be predicted by prior response to platinum, with response rates in platinum resistant patients being only 10–20%. This has led investigators to explore new and novel agents in this patient population.
A6 is an 8 amino-acid peptide derived from single chain urokinase plasminogen activator (scuPA), with the following sequence: Acetyl-Lys-Pro-Ser-Ser-Pro-Pro-Glu-Glu-NH2. The molecular formula is C39H62N10O15, with a molecular weight of approximately 911. A6 has been manufactured as the acetate salt. The finished drug product is a sterile aqueous solution in phosphate buffer (pH 5.5) in pre-filled syringes, each intended to deliver 150 mg of A6. A6 Injection contains 100 mg/mL of A6 as free peptide. A dose of 150 mg is therefore delivered subcutaneously in a volume of 1.5 mL.
Preclinical studies have shown that A6 has anti-angiogenic, anti-migratory, anti-invasive, and anti-metastatic properties, but is not anti-proliferative [2,3]. Å6 prevents the soluble complex of scuPA and soluble uPAR from activating plasminogen and thereby from mediating clot lysis [2]. Even a brief exposure to A6 produces paralysis of some types of ovarian cancer cells and prevents their migration in response to chemotactic signals. There is substantial heterogeneity among different human ovarian cancer cell lines in their sensitivity to this paralytic effect, but in susceptible lines that effect is observed at nanomolar concentrations. In vitro biological effects of A6 have generally been observed at concentrations in the micromolar range. A6 is active in a model of basic fibroblast growth factor (bFGF)-induced angiogenesis in a 7-day-old chick chorioallantoic membrane (CAM) model. A6 binds to and activates signaling from CD44, a stem cell marker commonly expressed in ovarian cancers [4]. A6 inhibits the invasion of several human (PC-3, MDA-MB-231) and non-human (3LL, Mat B-III) tumor cell lines through Matrigel™. Inhibitions of 75% at an A6 concentration of 50 micromolar were typically seen, without any in vitro cytotoxicity at concentrations up to 100 micromolar. Results from anti-tumor experiments in animals show that in addition to inhibiting major vessel formation, A6 also inhibits branching morphogenesis. In vivo results have shown that A6 has therapeutic activity in models of prostate cancer [5], glioblastoma multiforme (with cisplatin) [6], and breast cancer (with or without tamoxifen) [3]. In animal models, increased tumor necrosis is observed, probably due to increased apoptosis [3]. A6 has substantial anti-metastatic activity in the B16 lung metastasis model where it was found to reduce the number of metastases by 50% [4].
CD44 is a heavily glycosylated membrane protein important for cell-cell and cell-matrix adhesions [10]. The amino acid sequence of A6 exhibits homology to a linear sequence of the HA-binding domain of CD44 [11]. Recent studies have demonstrated that A6 binds to and activates CD44 on ovarian carcinoma cells, and that the anti-migratory activity of A6 correlated with CD44 expression suggesting that this activity may be due to modulation of CD44-dependent activities [4]. The ability of A6 to reduce the binding of an anti-CD44 antibody suggests that it alters CD44 structure. The changes produced by A6 represent an activation of CD44 as A6 increased cell adhesion to the CD44 ligand hyaluronic acid but only in CD44-positive cells. Relevant to its effect on migration, A6 elevates the activity of focal adhesion kinase (FAK) as reflected by phosphorylation at Y397, Y576/577 and Y925) but only in A6-responsive cell lines. FAK has a major role in reorganizing the cytoskeleton [12]. It is activated by auto-phosphorylation in response to integrin clustering [13, 14] following which it binds Src with high affinity at a single site on the cytoplasmic domain of CD44. This results in the subsequent Ras-dependent activation of the MAP kinase cascade, including MEK phosphorylation [15]. Similar to the effect of hyaluronic acid, the natural ligand for CD44, A6 produced not only phosphorylation of FAK but also activation of MEK [4]. This study was therefore undertaken in order to determine the activity of A6 in patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal carcinoma and to compare that activity to CD44 expression.
PATIENTS AND METHODS
Patients and Treatment
Eligibility
Eligible patients had a diagnosis of epithelial ovarian, fallopian tube, or primary peritoneal carcinoma. Histological documentation of the original primary tumor was required via the pathology report. Tumors were not screened for CD44 expression before enrollment. Patients were required to have measurable disease as defined by Response Evaluation Criteria in Solid Tumors (RECIST). Eligible patients must have received one prior platinum-based chemotherapeutic regimen for the management of their primary disease, including high-dose therapy, consolidation, non-cytotoxic agents, or extended therapy administered after surgical or non-surgical assessment. They were allowed to have received, but were not required to have received, one additional cytotoxic regimen for the management of persistent or recurrent disease. They were not permitted to have received any non-cytotoxic therapy for the management of persistent or recurrent disease. Patients who had received only one prior cytotoxic regimen must have had a platinum-free interval of less than 12 months, including those patients who progressed during or had persistent disease after platinum-based therapy. Patients who had received only one prior cytotoxic regimen were allowed to have a GOG performance status of 0 to 2, while those who had received two prior cytotoxic regimens were required to have a GOG performance status of 0 or 1. Patients were required to have adequate bone marrow (absolute neutrophil count ≥ 1,500/mcl, platelet count ≥ 100,000/mcl), renal (serum creatinine ≤ 1.5 × the upper limit normal), and hepatic function (total bilirubin ≤ 1.5 × the upper limit of normal, transaminases and alkaline phosphatase ≤ 2.5 × the upper limit of normal).
Patients provided written informed consent consistent with federal, state, and local institutional requirements. The protocol was also approved by the institutional review board at each participating GOG institution and performed in accordance with assurances filed with and approved by the Department of Health and Human Services.
Treatment plan
A6 (Angstrom Pharmaceuticals, Inc, San Diego, California) was self administered as a 300 mg daily dose consisting of two subcutaneous injections of 150 mg each. A cycle equaled 28 days. A6 was to be continued until progressive disease or adverse effects prohibited further therapy with this agent.
Toxicity was graded using the National Cancer Institute Common Toxicity Criteria version 3.0. From prior experience with A6 [8, 9], no significant toxicity was anticipated, so there were no allowable dose reductions. Patients experiencing persistent grade 3 (or greater) nausea, emesis, diarrhea, or constipation in spite of optimal medical management required a delay in subsequent therapy for a maximum of 2 weeks until recovered to grade 1. Similarly, patients experiencing non-hematologic toxicities with an impact on organ function of grade 2 (or greater) required a delay in subsequent therapy for a maximum of 2 weeks until recovered to grade 1, or pre-therapy baseline. Treatment delays of more than 2 weeks required removal from protocol treatment.
Response assessment
Patients were evaluated clinically every 4 weeks and radiologically every 8 weeks. The same evaluation modality was used throughout for each patient on study. Response criteria used were as defined by RECIST.
Translational Methodologies
If the patient agreed to participate in the translational portion of the study, archived formalin-fixed, paraffin-embedded tissue was obtained from the primary tumor in order to examine immunohistochemical (IHC) expression of CD44.
Statistical Methods
A6 was expected to be primarily cytostatic, but since a cytotoxic effect could not be excluded, the primary endpoint of this study included both progression-free survival at 6 months and objective tumor response. Time at risk was assessed from the date of study registration and included all eligible patients who received the drug. Progression-free survival (PFS) was defined as the period from study entry until disease progression, death or date of last contact and Overall survival (Survival) from entry until death or the date of last contact. The null hypothesis relating to uninteresting levels of activity was determined from an analysis of a historical GOG dataset based on a similar population of patients where the levels of activity were believed to be inactive to modestly active. The null hypothesis jointly specified the probability of a patient experiencing a tumor response to ≤10% and the probability of a patient being alive and progression free at 6 months to ≤15%. Increases to 25% for tumor response and to 35% for 6-month PFS were considered clinically significant. The two-stage, bivariate, flexible method of Sill and Yothers [7] was used with a goal of limiting patient exposure to inactive agents while restricting the probabilities of type I and type II errors to about 10%. If the regimen were to demonstrate sufficient activity in the first stage (with 31 patients, this required >3 objective tumor responses or >6 patients with PFS≥6 months), then the study would have targeted a total of 53 patients (cumulatively) in stage 2. Overall survival and progression-free survival were characterized with Kaplan-Meier plots and estimates of the median time until death or progression. Two-sided exact (Clopper-Pearson) 90% confidence intervals were calculated for 6-month PFS and tumor response. To assess the potential relationship between CD44 expression and clinical outcome, Fisher’s Exact Test was performed.
RESULTS
Patients and Eligibility
Thirty-one patients were enrolled onto the trial. All patients were both eligible and evaluable. Patient characteristics are listed in Table 1. All had a GOG performance status of either 0 or 1. Twenty-six patients had ovarian cancer, two fallopian tube cancer, and three primary peritoneal cancer. Serous carcinoma was the most common cell type (24/31; 77.4%). Fifteen patients had received only one prior chemotherapeutic regimen while sixteen patients had received two. Twenty patients were considered to have platinum-resistant disease (platinum-free interval < 6 months), whereas the platinum-free interval was between 6- 12 months in 4 patients and greater than 12 months in 7 patients (of whom, six patients were considered to be secondarily platinum resistant). All patients had previously undergone surgery for their cancer and none had received radiation therapy nor immunotherapy.
Table 1.
Patient Characteristics
| Characteristic | Number of Cases |
% |
|---|---|---|
| Age | ||
| 40–49 | 1 | 3.2 |
| 50–59 | 11 | 35.5 |
| 60–69 | 17 | 54.8 |
| 70–79 | 2 | 6.5 |
| Race | ||
| African American | 2 | 6.5 |
| White | 29 | 93.5 |
| Performance Status | ||
| 0 | 22 | 71.0 |
| 1 | 9 | 29.0 |
| Site of Disease | ||
| Ovary | 26 | 83.9 |
| Fallopian tube | 2 | 6.5 |
| Primary peritoneal | 3 | 9.7 |
| Cell Type | ||
| Clear Cell Carcinoma | 2 | 6.5 |
| Endometrioid Adenocarcinoma | 2 | 6.5 |
| Unclassified Carcinoma | 1 | 3.2 |
| Mixed Epithelial Carcinoma | 2 | 6.5 |
| Serous Adenocarcinoma | 24 | 77.4 |
| Grade | ||
| 1 | 4 | 12.9 |
| 2 | 3 | 9.7 |
| 3 | 24 | 77.4 |
| Prior Chemotherapy | ||
| 1 Regimen | 15 | 48.4 |
| 2 Regimens | 16 | 51.6 |
Treatment Response
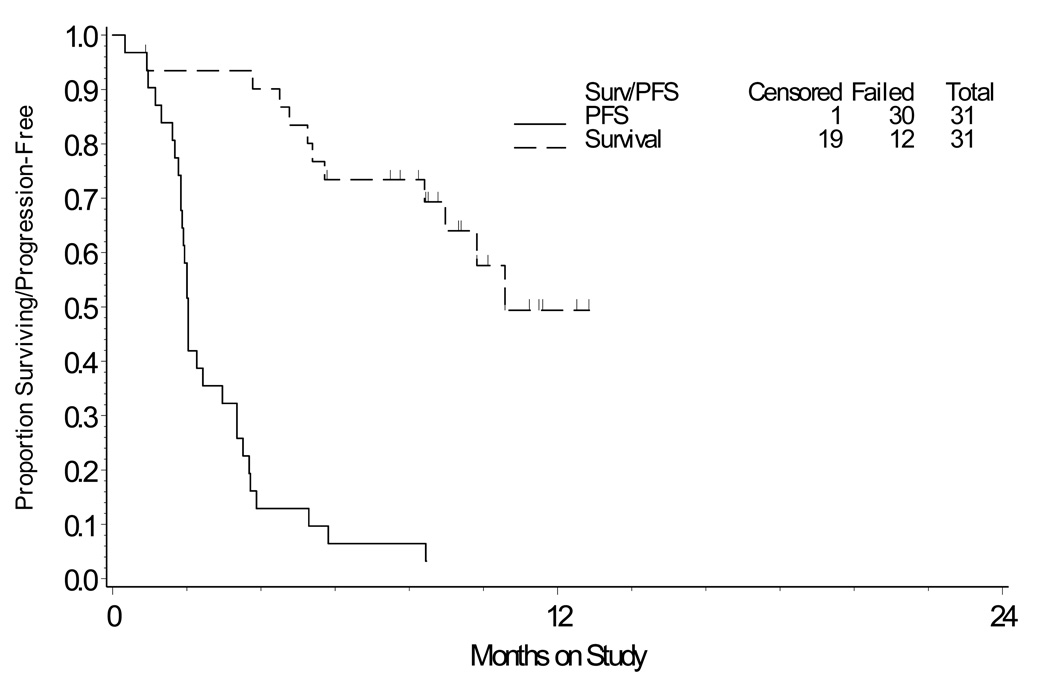
Patients received a median of two cycles (range one to 14). There were no objective responses (either complete or partial) (90% confidence interval [CI]: 0%, 9.2%). Two patients (6.5%) achieved PFS > 6 months (90% CI: 1.2%, 18.9%). The median PFS for the whole group was 2.0 months (first and third quartiles, 1.8 and 3.5 months, respectively). The median overall survival has not yet been reached (Figure 1).
Figure 1.
Plot of the Kaplan-Meier estimates of overall and progression free survival.
Toxicity
There were 2 deaths on study. One occurred after only 2 days of treatment and was determined to be due to disease progression. The other occurred during the first cycle of treatment in a woman receiving anticoagulation treatment for deep vein thrombosis and was due to hemorrhage which was felt to be possibly drug- related. There were no grade 4 toxicities. The most common grade 3 toxicities were constitutional (2/31; 6.5%) (Table 2).
Table 2.
Adverse Events (N=31)
| Grade | ||||||
|---|---|---|---|---|---|---|
| Adverse Events | 0 | 1 | 2 | 3 | 4 | 5 |
| Leukopenia | 27 | 2 | 2 | 0 | 0 | 0 |
| Thrombocytopenia | 28 | 3 | 0 | 0 | 0 | 0 |
| Neutropenia | 27 | 3 | 1 | 0 | 0 | 0 |
| Anemia | 21 | 5 | 5 | 0 | 0 | 0 |
| Other Hematologic | 30 | 0 | 1 | 0 | 0 | 0 |
| Constitutional | 18 | 10 | 1 | 2 | 0 | 0 |
| Dermatologic | 23 | 8 | 0 | 0 | 0 | 0 |
| Gastrointestinal | 23 | 3 | 4 | 1 | 0 | 0 |
| Hemorrhage | 29 | 1 | 0 | 0 | 0 | 1 |
| Lymphatics | 30 | 1 | 0 | 0 | 0 | 0 |
| Metabolic | 28 | 2 | 1 | 0 | 0 | 0 |
| Neurosensory | 30 | 1 | 0 | 0 | 0 | 0 |
| Other Neurological | 30 | 1 | 0 | 0 | 0 | 0 |
| Pain | 21 | 9 | 1 | 0 | 0 | 0 |
| Pulmonary | 30 | 1 | 0 | 0 | 0 | 0 |
Translational Endpoints
A total of 27 patients agreed to participate in the translational portion of the study and had available archived formalin-fixed, paraffin-embedded tissue from the primary tumor for analysis of immunohistochemical (IHC) expression of CD44. Five patients (18.5%) were positive for CD44 expression. Of the two patients achieving progression free survival ≥ six months, one was positive and one was negative for CD44 expression (p=0.342).
DISCUSSION
In a phase I trial [8], A6 was administered to 16 patients at doses escalating from 150 mg daily for 14 consecutive days every 29 days to 300 mg daily without interruption. Five patients had stable tumor measurements for at least 4 cycles, one of whom stayed on study for 12 months. One patient had a confirmed CA-125 response (decrease in CA-125 of > 50%) with stable disease on CT scan after 14 cycles. A phase II randomized double blind, placebo controlled trial of A6 in patients with asymptomatic CA-125 progression of epithelial ovarian cancer was then conducted [9], in which 24 patients were accrued, randomized, treated, and followed for up to 9 months. Despite early study termination due to slow accrual and small sample size, A6 therapy was associated with a statistically significant progression-free survival (PFS) (log rank p value = 0.01) with a median PFS of 100 days (95% CI 64,168) compared to 49 days (95% CI 29,67) in patients who received the placebo. The results of the current multi-institutional study of A6 for recurrent or persistent ovarian, peritoneal, and fallopian tube carcinoma do not confirm these results. Minimal activity was demonstrated, and the second phase of accrual was not opened. The current population, by design, had established, recurrent, measurable disease by RECIST criteria, which differs significantly from the population studied in the phase II trial who, by definition, had no evidence of disease on imaging. If, as previously noted [2..3], A6 inhibits formation of tumor metastases rather than acting as an anti proliferative agent, the population included in this current study may not have allowed for detection of A6 activity
CD44 expression has been reported in 23–100% of specimens of ovarian adenocarcinoma [16–24]. Serous ovarian adenocarcinoma is the predominant histology studied, however a single report documents expression in 86% of clear cell ovarian cancers studied [25]. The 18.5% CD44 expression in the current study is unexpectedly low, but not statistically different from the lower limit of reported expression [24], and limits evaluation of the utility of CD44 as a predictive marker for A6 activity.
Only 27 patients who agreed to participate in the translational portion of the study had available archived formalin-fixed, paraffin-embedded tissue from the primary tumor for analysis of immunohistochemical (IHC) expression of CD44. Five patients (18.5%) were positive for CD44 expression, and one of the two patients achieving progression free survival ≥ six months was positive for CD44 expression. This was, unfortunately, too few to comment on the utility of CD44 as a predictive marker for A6 activity.
Previous studies [8, 9] of A6 have demonstrated it to be well tolerated, with the only serious drug-related adverse events being transient nausea and dyspnea, which were considered possibly drug related. No dose-limiting toxicity was seen. Other A6-related toxicities were limited to grades 1 and 2 adverse effects including local injection site reactions. In this present study, two deaths occurred. One occurred after only 2 days of treatment and was determined to be due to disease progression. The other occurred during the first cycle of treatment in a woman receiving anticoagulation treatment for deep vein thrombosis and was due to hemorrhage which was felt to be possibly drug- related. No effect on parameters of coagulation, including prothrombin time, partial thromboplastin time, D-dimer, and fibrin split products, have previously been reported [8]. Because A6 prevents the activation of plasminogen, thereby inhibiting clot lysis [2], it should not be expected to increase the risk of bleeding. Never-the-less, it should be used with caution in patients receiving anti-coagulation until further experience with the combination is obtained.
A6 at the studied dose and schedule was not effective in the treatment of patients with recurrent or persistent ovarian, peritoneal, or fallopian tube carcinomas.
RESEARCH HIGHLIGHTS.
A6 demonstrated minimal activity in this study of recurrent or persistent epithelial ovarian, primary peritoneal, and fallopian tube carcinoma patients.
We were unable to associate CD44 expression with progression free survival at six months.
ACKNOWLEDGEMENTS
This study was supported in part by National Cancer Institute grants to the Gynecologic Oncology Group Administrative Office (CA 27469) and the Gynecologic Oncology Group Statistical and Data Center (CA 37517) and by Angstrom Pharmaceuticals.
The following Gynecologic Oncology Group member institutions participated in this study: Abington Memorial Hospital; University of Colorado-Anschutz Cancer Pavilion; University of Iowa Hospitals and Clinics; Rush University Medical Center; Magee Women’s Hospital; Cleveland Clinic Foundation; Columbus Cancer Council/Ohio State; University of Oklahoma; Case Western Reserve University; Women and Infants Hospital; and the Community Clinical Oncology Program.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST STATEMENT
William Brady reports that he received an Angstrom Honorarium for serving on their Advisory Board of $50. Additionally, Dr. Stephen Howell reports that he is a Member of the Board of Directors of Angstrom Pharmaceuticals which is the company that provided the drug for this study. Dr. Howell further reports that his laboratory has received gifts in support of research on the drug used in this study. There are no other conflicts to disclose.
REFERENCES
- 1.American Cancer Society. Cancer Facts & Figures 2011. Atlanta: American Cancer Society; 2011. [Google Scholar]
- 2.Guo Y, Higazi AA, Arakelian A, Sachais BS, Cines D, Goldfarb RH, et al. A peptide derived from the nonreceptor binding region of urokinase plasminogen activator (uPA) inhibits tumor progression and angiogenesis and induces tumor cell death in vivo. FASEB J. 2000;14:1400–1410. doi: 10.1096/fj.14.10.1400. [DOI] [PubMed] [Google Scholar]
- 3.Guo Y, Mazar AP, Lebrun JJ, Rabbani SA. An antiangiogenic urokinase-derived peptide combined with tamoxifen decreases tumor growth and metastasis in a syngeneic model of breast cancer. Cancer Res. 2002;62:4678–4684. [PubMed] [Google Scholar]
- 4.Piotrowicz RS, Damaj B, Hachicha M, Incardonna F, Howell SB, Finlayson F. A6 peptide Activates CD44 Adhesive Activity, Induces FAK and MEK Phosphorylation and Inhibits the Migration and Metastasis of CD44-Expressing Cells. Mol Cancer Therap, Published Online. 2011 Sep 1; doi: 10.1158/1535-7163.MCT-11-0351. [DOI] [PubMed] [Google Scholar]
- 5.Boyd DD, Kim SJ, Wang H, Jones TR, Gallick GE. A urokinase-derived peptide (Å6) increases survival of mice bearing orthotopically grown prostate cancer and reduces lymph node metastasis. Am J Pathol. 2003;162:619–626. doi: 10.1016/S0002-9440(10)63855-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mishima K, Mazar AP, Gown A, Skelly M, Xiang-Dong Ji, Wang X-D, et al. A peptide derived from the non-receptor-binding region of urokinase plasminogen activator inhibits glioblastoma growth and angiogenesis in vivo in combination with cisplatin. Proc Nat Acad Sci. 2000;97:8484–8489. doi: 10.1073/pnas.150239497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sill MW, Yothers G. Department of Biostatistics, University at Buffalo; A method for utilizing bivariate efficacy outcome measures to screen agents for activity in 2-stage phase II clinical trials, Technical Report 06–08. Website: http://sphhp.buffalo.edu/biostat/research/techreports/index.php. [Google Scholar]
- 8.Berkenblit A, Matulonis UA, Kroener JF, Dezube BJ, Lam GN, Cuasay LC, et al. A6, a urokinase plasminogen activator (uPA)-derived peptide in patients with advanced gynecologic cancer: A phase I trial. Gynecol Oncol. 2005;99:50–57. doi: 10.1016/j.ygyno.2005.05.023. [DOI] [PubMed] [Google Scholar]
- 9.Ghamande SA, Silverman MH, Huh W, Behbakht K, Ball G, Cuasay L, et al. A phase 2, randomized, double-blind, placebo-controlled trial of clinical activity and safety of subcutaneous A6 in women with asymptomatic CA125 progression after first-line chemotherapy of epithelial ovarian cancer. Gynecol Oncol. 2008;111:89–94. doi: 10.1016/j.ygyno.2008.06.028. [DOI] [PubMed] [Google Scholar]
- 10.Goodison S, Urquidi V, Tarin D. CD44 cell adhesion molecules. J Clin Pathol. 1999;52:189–196. doi: 10.1136/mp.52.4.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teriete P, Banerji S, Noble M, Blundell CD, Wright AJ, Pickford AR, et al. Structure of the regulatory hyaluronan binding domain in the inflammatory leukocyte homing receptor CD44. Mol Cell. 2004;13:483–496. doi: 10.1016/s1097-2765(04)00080-2. [DOI] [PubMed] [Google Scholar]
- 12.Schaller MD. Cellular functions of FAK kinases: insight into molecular mechanisms and novel functions. J Cell Sci. 2010;123:1007–1013. doi: 10.1242/jcs.045112. [DOI] [PubMed] [Google Scholar]
- 13.Schaller MD, Hildebrand JD, Shannon JD, Fox JW, Vines RR, Parsons JT. Autophosphorylation of the focal adhesion kinase, pp125FAK, directs SH2-dependent binding of pp60src. Mol Cell Biol. 1994;14:1680–1688. doi: 10.1128/mcb.14.3.1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cobb BS, Schaller MD, Leu TH, Parsons JT. Stable association of pp60src and pp59fyn with the focal adhesion-associated protein tyrosine kinase, pp125FAK. Mol Cell Biol. 1994;14:147–155. doi: 10.1128/mcb.14.1.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schlaepfer DD, Hanks SK, Hunter T, van der Gear P. Integrin-mediated signal transduction linked to Ras pathway by GRB2 binding to focal adhesion kinase. Nature. 1994;372:786–791. doi: 10.1038/372786a0. [DOI] [PubMed] [Google Scholar]
- 16.Hong SC, Song JY, Lee JK, et al. Significance of CD44v6 expression in gynecologic malignancies. J Obstet Gynaecol Res. 2006;32:379–386. doi: 10.1111/j.1447-0756.2006.00422.x. [DOI] [PubMed] [Google Scholar]
- 17.Bar JK, Grelewski P, Popiela A, Noga L, Rabczynski J. Type IV collagen and CD44v6 expression in benign, malignant primary and metastatic ovarian tumors: correlation with Ki-67 and p53 immunoreactivity. Gynecol Oncol. 2004;95:23–31. doi: 10.1016/j.ygyno.2004.06.046. [DOI] [PubMed] [Google Scholar]
- 18.Sillanpa S, Anttila MA, Voutilainen K, et al. CD44 expression indicates favorable prognosis in epithelial ovarian cancer. Clin Cancer Res. 2003;9:5318–5324. [PubMed] [Google Scholar]
- 19.Afify AM, Ferguson AW, Davila RM, Werness BA. Expression of CD44S and CD44v5 is more common in stage III than in stage I serous ovarian carcinomas. Applied Immunohistochem Molecular Morphology. 2001;9:309–314. doi: 10.1097/00129039-200112000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Kayastha S, Freedman AN, Piver MS, et al. Expression of the hyaluronan receptor, CD44S, in epithelial ovarian cancer is an independent predictor of survival. Clin Cancer Res. 1999;5:1073–1076. [PubMed] [Google Scholar]
- 21.Schroder W, Rudlowski C, Biesterfeld S, Knoblock C, Hauptman S, Rath W. Expression of CD44(v5–10) splicing variants in primary ovarian cancer and lymph n ode metastases. Anticancer Res. 1999;19:3901–3906. [PubMed] [Google Scholar]
- 22.Darai E, Walker-Combrouze F, Fauconnier A, Madelenat P, Potet F, Scoazec JY. Analysis of CD44 expression in serous and mucinous borderline tumours of the ovary: comparison with cystadenomas and over carcinomas. Histopath. 1998;32:151–159. doi: 10.1046/j.1365-2559.1998.00347.x. [DOI] [PubMed] [Google Scholar]
- 23.Rodriguez-Rodriguez L, Sancho-Torres I, Mesonero C, et al. The CD44 receptor is a molecular predictor of survival in ovarian cancer. Medical Oncol. 2003;20:255–263. doi: 10.1385/MO:20:3:255. [DOI] [PubMed] [Google Scholar]
- 24.Ross JS, Sheehan CE, Williams SS, Malfetano JH, Szyfelbein WM, Kallakury BVS. Decreased CD44 standard form expression correlates with prognostic variables in ovarian carcinomas. Am J Clin Pathol. 2001;116:122–128. doi: 10.1309/KUK0-1M3D-LGNE-THXR. [DOI] [PubMed] [Google Scholar]
- 25.Rodriguez-Rodriguez L, Sancho-Torres I, Leakey P, et al. CD44 splice variant expression in clear cell carcinoma of the ovary. Gynecol Oncol. 1998;71:223–229. doi: 10.1006/gyno.1998.5108. [DOI] [PubMed] [Google Scholar]