Abstract
eHealth, mHealth and “Web 2.0” social media strategies can effectively reach and engage key populations in HIV prevention across the testing, treatment, and care continuum. To assess how these tools are currently being used within the field of HIV prevention and care, we systematically reviewed recent (2013–2014) published literature, conference abstracts, and funded research. Our searches identified 23 published intervention studies and 32 funded projects underway. In this synthesis we describe the technology modes applied and the stages of the HIV care cascade addressed, including both primary and secondary prevention activities. Overall trends include use of new tools including social networking sites, provision of real-time assessment and feedback, gamification and virtual reality. While there has been increasing attention to use of technology to address the care continuum, gaps remain around linkage to care, retention in care, and initiation of antiretroviral therapy.
Keywords: mHealth, eHealth, Internet, HIV, Mobile phone, Smartphone, Social media, Intervention, Prevention
Introduction
In recent years, HIV prevention has been reframed by the dual, related concepts of the HIV care continuum – or treatment “cascade” [1, 2] – and “Treatment as Prevention” (TasP) [3, 4]. Both concepts draw on scientific advances that demonstrate the ability of antiretroviral therapies (ART) to prevent HIV acquisition in the form of Pre-Exposure Prophylaxis (PrEP), and reduce forward transmission via earlier initiation of ART among those who are HIV-positive [5–7]. In practice, the success of these biomedical strategies will depend on integrated prevention and care systems and sustained behavioral modification. To aid the rapid and cost-effective application of these new advances, researchers and health practitioners are testing a variety of technology-based approaches.
eHealth (using information and communication technologies for health), and more recently mHealth (using mobile devices for health), strategies provide opportunities to reach and engage key populations in HIV prevention across the testing, treatment, and care cascade [8•, 9, 10••]. Equivalent outcomes have been found comparing therapist and computer-based interventions (CBI) focused on the promotion of a range of health behaviors; two meta-analyses found that CBIs can change mediators of safer sex (e.g. HIV/AIDS knowledge condom use self-efficacy) as well as behavioral and biomedical outcomes (e.g. condom use, incident sexually transmitted infections (STIs) [11, 12]. Since the early 1990s, the range and complexity of tools available for CBIs have grown to include serious gaming (using gaming principles and mechanics to achieve a specific health or education outcome), interactivity, simulation, and virtual reality (VR). These tools are being leveraged to address the need for innovative and high-fidelity technologies within health-related interventions [13–21]. Given the rapid expansion of the mobile web, social media, and user-driven content—so called “Web 2.0”—these technologies are highly scalable and relatively cost-effective once developed.
Mobile phone ownership is widespread across the world. In the US, 90% of adults own a mobile phone and 58% own smartphones [22]. Usage statistics are variable in other parts of the world, but a recent Pew Internet Research survey found that over 50% of respondents in each of 24 included countries owned a mobile phone with rates as high as 91% in South Africa and 95% in Jordan and China [23].
Expanded access to smartphones has fundamentally changed how we engage with mobile technologies. Mobile applications, “apps”, are computer programs designed to run on smartphones, tablet computers and other mobile devices. While apps were originally offered for general productivity and information retrieval, they have expanded to include games, location-based services, and more recently, mobile medical apps, though use within HIV prevention and care is still in its infancy [24, 25, 26•].
A concurrent evolution of web technologies has transformed internet utilization. In contrast to static web sites where consumers are limited to passive viewing of content, a Web 2.0 site allows users to interact and collaborate via social media platforms as co-creators of user-generated content in virtual communities (e.g. Facebook, Twitter). The popularity of these new forms of engagement is evidenced in the exponential growth of social and sexual networking sites (sites where people explicitly seek others for sex) over the past decade. Seventy-three percent of online adults now use a social networking site of some kind, and 42% use multiple sites [27]. Thus, interventions delivered via social media have the potential to reach large numbers of participants “where they are”. Sexual networking sites like Grindr among men seeking men, and more recently Tinder for heterosexuals, are increasingly popular and create new opportunities for finding sex partners. Grindr boasts five million users in 192 countries [28] while Tinder is suspected to have as many as 10 million active daily users [29].
While social media sites may facilitate sexual risk behaviors in certain contexts, they also create opportunities for health promotion [30••]; interventions can be delivered at the times and places most relevant for individuals, utilizing technologies they already own and are familiar with. We conducted a review of recent advances and current trends in the use of electronic and mobile health technologies for primary and secondary HIV prevention. As technological development often out-paces academic research, we include emerging technologies and interventions that are still under development.
Methods
We searched PubMed, Web of Science, and NIH Reporter, using the dates 1/1/2013 to 9/1/2014 and the following key words in combination: HIV, eHealth, mHealth, smartphone, mobile phone, cell phone, mobile health, internet, online, app, application, social media, web, and Web 2.0. We also searched select conference databases for 2013 and 2014, including Conference on Retroviruses and Opportunistic Infections (CROI); International AIDS Society (IAS2013 and AIDS2014), US Conference on AIDS (USCA), STD Prevention Conference, and Youth+Tech+Health (YTH). Among articles and abstracts identified through these searches, we included for review those which reported the development, pilot test, or randomized controlled trial (RCT) of an HIV primary or secondary prevention intervention that utilized internet and/or smartphone-based technology as a primary component of the intervention. We excluded publications that: 1) did not include a clear intervention, 2) exclusively used text-based technologies such as mobile phone text messaging (SMS), or CD-ROM-based technologies (independent of internet connection), or 3) did not include an HIV-specific outcome (e.g. focused exclusively on other STIs).
We abstracted the following information into a Microsoft Excel database: author; publication/funding year(s); citation/grant number; institution; study population; sample size; study location; study description (intervention and control conditions) and primary and secondary outcomes. We categorized the technology mode(s) applied as: “web-only” (website-based, no explicit mobile phone component); “mobile web” (explicit design for use via a smartphone or tablet with internet connectivity); “app” (stand-alone application, able to operate on a mobile device independent of internet connectivity); “web+phone” (utilizes a combination of internet and mobile phone based elements); and “Web 2.0 “ (employs tools or platforms of social media in conjunction with internet or mobile phone, e.g. use of Facebook to spread HIV education).
Lastly, we categorized each included intervention by the stage(s) of the HIV cascade primarily addressed defined as: 1) preventing primary acquisition (e.g. condom promotion, STI care, pre-exposure prophylaxis); 2) increasing HIV testing; 3) supporting linkage to care; 4) supporting retention in care; 5) supporting initiation of ART; 6) supporting adherence to ART and/or increasing viral suppression; 7) preventing secondary transmission. We applied categorization 7 to interventions which focused on reducing risk behaviors among diagnosed HIV-infected persons (prevention for positives). ART-based strategies can also be considered as preventing secondary transmission; in this categorization model, these activities are captured by categories 3 through 6.
Results
We identified 26 relevant published articles and conference abstracts describing 21 intervention studies (Table 1) and 14 systematic reviews and meta-analysis studies (not presented in Table form). Searches within the NIH Reporter database identified an additional 31 studies currently underway (Table 2).
Table 1.
eHealth prevention interventions for HIV
| Author, publication year |
Population; sample size | Location | Study Description Intervention (I) vs.Control (C) |
Results | eHealth mode | Cascadestage |
|---|---|---|---|---|---|---|
| Miranda et al. 2013 [40] |
HIV+ MSM; n=60 | US | Study protocol: Internet-based intervention to increase condom use compared to list of websites with HIV prevention information |
Outcomes: improving condom use, self- efficacy, and intentions to use condoms. NOTE: study not yet conducted. |
web | Prevent secondary transmission |
| Ybarra et al. 2013, 2014 [32, 33] |
Secondary school students; n=366 |
Uganda | Pilot: CyberSenga five 1-hour online modules (+ booster module), tailored for gender and culture. Aim: to increase abstinence and/or condom use. |
3-month FU: Abstinence, I vs C: 81% vs. 74%, p=0.08); unprotected sex: no difference. 6-month FU: no significant differences in main outcomes. Abstinence, I booster group vs. I no booster vs. C: (80% vs. 57% vs. 55%). |
web | Prevent primary acquisition |
| Villegas et al. 2014 [34] |
Women, age 18–24; n=40 |
Chile | Pilot: I-STIPI, online adaptation of successful in-person interventions (Mano a Mano-Mujer & SEPA). Modules, quizzes, activities, 1 month. |
91.9%: very satisfied with website content and activities. 67.6%: information was easy-to-find on the site, 70.3%: website features were very good. |
web | Prevent primary acquisition |
| Bauermeister, 2014 YTH [36] |
MSM, age 15–24; n=130 |
Michigan, US | I: HIV education and HIV/STI test locator. Content tailored for demographics, values and prior HIV risk and testing behaviors. C: Test locator only. |
Intervention: more likely to visit HIV/STI testing clinic (past 30 days), and reported higher self-efficacy around testing behaviors. I and C: significantly reduced sex risk behaviors, no difference by treatment condition. |
web | Prevent primary acquisition Increase HIV testing |
| Fakhouri, 2014 YTH [35] |
“teens”; n=199 | US | I: PlayForward, 12-session (75–90 min each) online game to improve sexual health decision-making, 6 weeks. C: attention/time control games. |
Positive association trend between greater progress through the game and sexual health knowledge score at 6 months. |
web | Prevent primary acquisition |
| Milam et al. 2014 CROI [39] |
HIV+ MSM with recent UAI or STI; n=181 |
Southern California,US |
I: Monthly risk survey+tailored internet-based prevention messages targeting condoms, ART use, status disclosure, and reducing substance use. C: monthly behavioral risk survey. |
12-month follow-up: I vs C, at least one new STI: 27 (30%) vs. 22 (27%) (p=0.38). Similar non-significant results found in sensitivity analyses. |
web | Support ART initiation Improve ART adherence Prevent secondary transmission |
| Christensen et al. 2013 [31•] |
HIV-neg MSM, UAI, age 18–24; n=921 |
National online | I: Socially Optimized Learning in Virtual Environments (SOLVE): web-based modules to reduce UAI via reduced stigma. C: wait-list control. |
I vs C at 3 month follow-up: significant shame reduction, p<0.001; significant decrease in UAI: (point estimate −0.10, 95% CI [−0.01 to −0.23]. 6 month follow-up data (also significant) forthcoming. |
web | Prevent primary acquisition |
| Jones et al. 2013 [46] |
Urban African American women, age 18–29; n=238 |
New Jersey, US | I: “Love, Sex, & Choices” streaming 12-episode weekly soap opera video episodes to smartphones. C: weekly HIV prevention text messages |
Video was rated popular, relevant, and identifiable. Episodes of UVI, past 3 months dropped significantly in both study arms from 21–22 episodes to 5–6 episodes. No statistical differences in effect for text vs. video. |
mobile web | Prevent primary acquisition |
| Phillips et al. 2013 [47] |
Opioid-dependent drug users, age 18–75; n=24 |
Baltimore, US | Pilot: smartphone based intervention with 3 modules that each consisted of a 10-minute video on HIV risk reduction |
All 3 videos met a priori criteria for acceptability and feasibility. On average, participants answer 92% of HIV/STI knowledge questions correctly post-video (pre-post difference not measured). |
mobile web | Prevent primary acquisition |
| Bonnet Rivera et al. 2014 USCA [37] |
High-risk Latino young MSM |
Puerto Rico | Proyecto Nosotr@s: venue-based testing staff support linkage to care via SMS, email, calls, social media and apps. |
The project has identified 260 HIV positive MSM (159 ages 13 to 29). |
web+phone | Support linkage to care |
| Jones & Green. 2014 USCA [38], |
Providers and their HIV+ patients |
United States | A mobile app and four e-learning modules adapted from evidence- based CDC interventions: Project HEART (Helping Enhance Adherence to Anti-retroviral Therapy), SMART (Sharing Medical Adherence Responsibilities Together) Couples, Partnership for Health - Medication Adherence, and Peer Support. |
Outcomes: ART initiation, medication adherence among PLWH NOTE: study not yet conducted. |
Web+App | Support ART initiation Improve ART adherence |
| Danielson et al. 2013 [41•] |
African American women, age 13–18; n=41 |
Southeast, US | Pilot: web adaptation of CDC evidence- based intervention Sistas, Informing, Healing, Living, and Empowering. 4 one-hour modules: interactive video- based design, health educator, activities, “near peer”, real-time tailored feedback. |
63% completed all four modules. Pre-post study: significant increases in: HIV/STI risk knowledge and condom use self- efficacy. No significant change in: ethnic and gender pride, partner communication, healthy relationships and self-care, or self-esteem. |
web 2.0 | Prevent primary acquisition |
| Anand et al. 2013 IAS [51] |
MSM | Indonesia | TemanTeman.org: information on MSM- friendly healthcare and services in Indonesia. Over 40 expert advice videos on sexual health. Male fashion photography is linked to HTV/STI information and campaign is affiliated with an HIV/STI testing clinic in Jakarta and in Bali. |
Outcomes: HIV and STI testing. NOTE: Intervention not yet evaluated |
web 2.0/social media |
Prevent primary acquisition Increase HIV testing |
| Pachankis et al. 2013 [48] |
Adult MSM with recent UAI and substance use |
NYC, US | I: online adaptation of Young Men’s Health Project (using motivational interviewing in 4 one-hour sessions), specifically using the unique features of Facebook. |
Outcomes: reduce substance use and sexual risk-taking NOTE: Study not yet conducted |
web 2.0 | Prevent primary acquisition |
| Gaysynsky et al. 2014 [59] |
HIV+ participants in a Facebook support group, age 16–27; n=43 |
NYC, US | Evaluation of a private Facebook group established for members of an HIV clinic’s young adult program, 16 month study period. |
3838 posts and comments. Content analysis: 42% of content was classified as “administrative/engagement in group” and functioned to enhance the operations of the program as a whole. Positive interactions were common: socializing (25%), banter (20%), and offers of social support (15%). Emotional support most frequent type of support requested, esteem support most commonly provided form of support. |
web 2.0 | Support retention in care Support ART initiation Improve ART adherence |
| Lelutiu-Weinberger et al. 2014 [49] |
High-risk MSM, age 18–29; n=41 |
United States (online) |
I: 8 one-hour motivational interviewing and cognitive behavioral skills-based online live chat intervention sessions delivered on Facebook. Pre/post study design. |
Pre-post reductions in past 30 days: days of drug (5.52 vs. 3.30, p=0.073) and heavy alcohol use (10.7 vs. 8.52, p=0.082), and episodes of UAI (8.96 vs. 3.11, p=0.042), and UAI+substance use(6.89 vs. 0.81, p<0.001). Significant increases in HIV risk knowledge. |
web 2.0 | Prevent primary acquisition |
| Young et al. 2013,2014 [53–56, 57••] |
MSM (85% African American); n = 112 |
Los Angeles, US | Project HOPE: 16 peer leaders randomly assigned to (I) deliver HIV information and promote free home- based HIV tests or (C) provide general health information, via Facebook groups over 12 weeks. |
I vs. C: communication via the social platform: 95% vs 73%; requested home- based HIV testing kits: 44% vs. 20%; took and returned test kit: 36% vs. 18%. 12 week retention >93%, 1 year retention: 82%. |
web 2.0 | Prevent primary acquisition Increase HIV testing |
| Zou et al. 2013 [58] | MSM; n=3332 | China | I: two volunteers promoted VCT using active (instant messaging, chat rooms, mobile phones, email) and passive (website banner ads) methods. Those who came for testing completed a survey and HIV/ syphilis tests. |
12.9% of men contacted (n=429) were tested at designated VCT clinics. Instant messaging was most effective mode for promotion (1 out of 4 men). Email was least effective (1:140). Active recruitment yielded men who were significantly younger and more likely to have never tested for HIV or tested less frequently. |
web 2.0 | Increase HIV testing |
| Ko et al. 2013 [52] | MSM users of social media sites; n=1037 |
Taiwan | I: iPOL, online adaptation of CDC’s Popular Opinion Leader intervention. iPOLs are trained to disseminate information about HIV, risk reduction, behavior change; and ask and respond to questions and discussions via Facebook. C: informational website. |
369 iPOLs reached 959,088 persons on Facebook in 6 months. I vs. C: receive HIV-related information (25% vs 10%), discuss HIV issues with others (42% vs 24%), review articles about HIV (91% vs 80%), be asked about or discuss HIV- related questions (51% vs 32%), have HIV test within 6 months (44% vs 22%), no UAI with online sex partners (34% vs 26%). |
web 2.0 | Prevent primary acquisition Increase HIV testing |
| Marie, 2014 STD Prevention [50] |
Youth, age 15–25 | US | I: The STD Project (thestdproject.com) online storytelling to address STD stigma by advocating for awareness, education, and acceptance. Readers submit personal stories and engage via the forum or contact form. |
All participants had improvements (psychological improvements, safer sex practices and partner disclosure) after engaging with The STD Project. |
web 2.0 | Prevent primary acquisition Prevent secondary transmission |
| Marhefka et al. 2013 [60] |
HTV+ women; n=4 | US | Pilot study: video-conferencing based intervention, HR-VG: six two-hour sessions led by two facilitators, and used structured activities and video- clips to build HIV status disclosure and safer sex skills. |
Participants and facilitators reported feeling either “very comfortable” or “completely comfortable” with the technology and the overall intervention. Participants reported high levels of unity and togetherness among the group. |
web 2.0 | Prevent secondary transmission |
I intervention; C control; CDC Centers for Disease Control; VCT voluntary counseling and testing; UAI unprotected anal intercourse; MSM men who have sex with men; FU follow-up
Table 2.
Currently funded eHealth for HIV Prevention studies (NIH Reporter and conference abstracts)
| Primary Investigator Organization Name |
Funding period | Project Abstract | Target population | eHealth mode(s) | Cascade stage |
|---|---|---|---|---|---|
| Cohen MIRIAM HOSPITAL |
2011–13 | Vigorous Mind 4.0 uses a computerized system to promote treatment adherence for those with substance use disorders via enhanced cognitive functioning (cognitive exercises, organizational tools) training. 3 month pilot study (n=50) will compare intervention with standard of care control. |
HIV+ with substance use disorders |
Web | ART adherence |
| Boyer UNIV OF MASSACHUSETTS MED SCH WORCESTER |
2011–15 | iHAART delivers personalized adherence interventions with content and “dose” that adapt in real time to variable medication adherence in HIV+ stimulant users (methamphetamine, cocaine, MDMA). 3 month pilot study to test functionality and acceptability. |
HIV+ stimulant users | Smartphone App | ART adherence |
| Brown RHODE ISLAND HOSPITAL |
2012–15 | Medication monitoring device (Vitality Cap) integrated with an interactive app/game. Opening the medication bottle gives access to the app game. The game integrates health information (knowledge about HIV treatment), motivation, and skill-building. Intervention will be tested in a pilot RCT (n=60). Primary outcomes: medication adherence and biological measures. |
HIV+ youth | Smartphone App, gaming |
ART adherence |
| Gonzalez CUNY GRADUATE SCH AND UNIV CTR |
2012–15 | Pilot testing of a smartphone app for sexual and reproductive health information and push messages versus self-directed app use for increasing dose. Primary outcomes: increased knowledge and utilization of services such as PEP, Plan B, HIV, STD, and pregnancy testing, and to other social services, such as substance abuse treatment. |
Black and Latina women, age 18–25 |
Smartphone App | Primary acquisition HIV testing |
| Kirk JOHNS HOPKINS UNIVERSITY |
2012–15 | eMOCHA: (electronic Mobile Open-source Comprehensive Health Application) app assists peer navigators (former IDUs currently in HIV care) to deliver individually-tailored interventions to HIV+ IDUs out of care for >1 year. Ecologic momentary analysis assesses clinic attendance, adherence, drug cravings, and stress then triggers either: phone call/visit from a peer navigator or automated, context- specific text message |
HIV+ IDU, out-of-care | Smartphone App | Linkage to care Retention in care ART adherence |
| Himelhoch UNIVERSITY OF MARYLAND |
2013–15 | HEART to HAART (Helping Enhance Adherence to Retroviral therapy using Technology): provides real-time information on adherence, periodic assessment of medication side effects, depressive symptoms and drug use and tailored education, recommendation and encouragement. Participant and adherence team jointly adherence in real-time. 6 month pilot test planned (n=50) comparing intervention with smartphone control. |
HIV+ drug users | Smartphone | ART adherence |
| Reback COG ANALYTICS, LLC |
2013–15 | Project aims to translate “Getting Off: A Behavioral Treatment Intervention for Gay and Bisexual Male Methamphetamine Users” into a computerized app to reduce methamphetamine use and HIV sexual risk behaviors and increase antiretroviral therapy (ART) medication adherence. Study will pilot test the intervention prototypes |
Gay and Bisexual Male Methamphetamine Users |
Smartphone App | Primary acquisition ART adherence Secondary transmission |
| Horvath UNIVERSITY OF MINNESOTA |
2013–16 | ART adherence intervention app: tailored informational messages, a motivational personal intervention guide, medication reminders, ART and drug use self-monitoring, self-reflection and strategy rehearsal. Pilot RCT testing (n=76) with primary outcomes: app component use, percent of ART doses taken, rating of suggested strategies to overcome adherence barriers, experiences of drug cravings and use of stimulants. |
HIV-positive stimulant- using MSM |
Smartphone App | ART adherence |
| Horvath UNIVERSITY OF MINNESOTA |
2014–17 | App to facilitate regular HIV testing through: regular assessment of risk behaviors via personal profile, recommended HIV test frequency based on individual’s risk patterns and profile, GPS- enabled HIV testing location finder, and motivational messages addressing critical barriers to testing. Pilot RCT test (n= 120) to assess primary outcome: increased HIV testing. |
HIV-negative/unknown MSM |
Smartphone App | HIV testing |
| Pillai CAPITAL TECHNOLOGY INFORMATION SERVICES |
2014–15 | Smartphone app to promote HIV care and prevention services. Will be pilot tested with target population in Baltimore. |
Urban young MSM | Smartphone App | (unclear) Mentions all stages of the cascade |
| McNulty CAKTUS CONSULTING |
2014–16 | “Epic Allies” is a mobile phone app that utilizes game mechanics and social networking features to improve and optimize linkage to HIV care and ART uptake and adherence. App will be tested in a RCT through 14 sites of the Adolescent Trials Network (n=300). Outcome measures: engagement with medical providers, medical appointment consistency, ART uptake, adherence, viral suppression, CD4 count. |
HIV+MSM, age 18–30 | Smartphone App, interactive gaming, social networking |
Retention in care ART initiation ART adherence |
| Cruess UNIVERSITY OF CONNECTICUT STORRS |
2010–14 | This study will develop and pilot RCT test an internet-delivered risk reduction intervention for HIV-positive MSM who use the Internet to meet potential sex partners. Primary outcomes: behavioral risk and Internet use outcomes. |
HIV+ MSM | Web | Secondary transmission |
| Mustanski NORTHWESTERN UNIVERSITY AT CHICAGO |
2012–17 | Keep It Up! (KIU!), an online HIV prevention program tailored to ethnically diverse YMSM. KIU! is based on the Information- Motivation-Behavior Skills model of HIV risk behavior change and informed by principals of E-learning. Pilot RCT had high retention and a significant 44% decrease in UAI. This study will test KIU! in a multisite RCT (n=750) for primary outcomes: UAI and STD incidence. |
Young MSM | Web | Primary acquisition |
| Hirshfield PUBLIC HEALTH SOLUTIONS |
2014–16 | Online videos for HIV prevention about UAI, HIV disclosure, and testing partnered with POZ.com. RCT found significantly reduced UAI and significant increases in HIV status disclosure. Current RCT (n= 1500) will edit the 3 HIV prevention videos into 10 short online sessions (including boosters), improve retention with incentives and a proven online platform, and conduct cost-effectiveness analyses for averted HIV infections. |
Virally unsuppressed HIV+ MSM |
Web | Secondary transmission |
| Hightow-Weidman UNIVERSITY OF NORTH CAROLINA |
2012–16 | “healthMpowerment.org”: a mobile phone and internet-based intervention that provides information, resources, tailored feedback, gamification, and platforms for social support. Currently undergoing a state-wide RCT in North Carolina (n=474). Outcomes: reduced UAI past 3 months (primary), depression, social support, viral load/CD4, adherence, testing, HIV knowledge, substance use. |
Black MSM and TW, age 18–30 |
Mobile optimized web, gaming, social networking |
All stages of cascade |
| Koblin NEW YORK BLOOD CENTER |
2013–17 | Internet-based testing intervention optimized for mobile devices to provide men with a tailored recommendation of their optimal HIV testing approach. Pilot RCT to assess primary outcome of increased HIV testing. |
Young, Black MSM | Mobile optimized web | HIV testing |
| Tulsky UNIVERSITY OF CALIFORNIA SAN FRANCISCO |
2011–16 | Teach and train newly diagnosed HIV infected individuals to utilize deployed internet and cellular technologies and develop novel applications to assist with linkages to care and improve treatment outcomes. Primary outcomes: referrals and follow through with appointments, retention in care and the initiation and sustaining of ART. |
Newly HIV diagnosed in safety net care settings |
Web+App | Linkage to care Retention in care ART initiation ART adherence |
| Mitchell UNIVERSITY OF MIAMI SCHOOL OF MEDICINE |
2014–16 | Web-based prevention toolkit: modules to guide creation of an explicit sexual agreement that integrates interval testing for HIV/STDs and prevention messaging, interactive website and smartphone app with GPS resources for HIV/STD testing and free safer sex supplies. Pilot RCT (n= 160) to assess primary outcomes of: forming and adhering to a sexual agreement, increased HIV/STD testing, decreased UAI with casual partners. |
HIV-negative male- male couples practicing UAI |
Web+App | Primary acquisition HIV testing |
| Sullivan EMORY UNIVERSITY |
2014–16 | Development of support for home-based HIV testing system in support of PrEP including specimen self-collection using mail-in kits; online smartphone or SMS assessment of medication adherence and sexual behavior risk; and video/telephone counseling support. |
MSM | Web+App | Primary acquisition HIV testing |
| Rosser UNIVERSITY OF MINNESOTA |
2010–15 | Men’s Internet Study - MINTS-III - aims to increase the long-term effectiveness of MINTS-II (Sexpulse, an online, HIV prevention intervention for Men who use the Internet to seek Sex with Men) by strengthening the dosage of Sexpulse via tailored feedback on individual risk behavior; integrated research surveys; and follow-up boosters and test Sexpulse 1.1 in two RCTs (n= 1000 high-risk MSM and n=500 no/low-risk MSM) |
Men who use the Internet to seek Sex with Men |
Web 2.0/social media | Primary acquisition |
| Young UNIVERSITY OF CALIFORNIA LOS ANGELES |
2010–15 | Intervention to test the use of online social networks to scale peer community leader models to increase HIV prevention. Pilot study primary outcomes: increased testing and HIV prevention behaviors. |
African-American and Latino MSM |
Web 2.0/social media | Primary acquisition HIV testing |
| Rhodes WAKE FOREST UNIVERSITY HEALTH SCIENCES |
2011–15 | “CyBER/testing” is a chat room intervention to increase HIV testing. Primary outcome: self-reported HIV testing at immediate post- intervention. |
MSM | Web 2.0/social media | HIV testing |
| Washington CALIFORNIA STATE UNIV. LONG BEACH |
2012–15 | Exploring an HIV Testing Intervention Model (TIM project): Facebook “like” site will feature videos to encourage HIV testing plus social networking features to host discussions among the intervention group about HIV testing uptake and testing sites, drug use and sexual risk behavior. Will be tested in a pilot RCT. |
Black MSM, age 18–30 | Web 2.0/social media | HIV testing |
| Clark UNIVERSITY OF CALIFORNIA LOS ANGELES |
2014–17 | “TransPrEP”: Social network intervention to promote PrEP adherence via individual counseling, group workshops, adherence support tools. Structured social media platforms to educate, motivate, and promote discussions of PrEP adherence, unstructured participant- generated interactions to reinforce new social norms within the network. Pilot RCT (n=8 social network-based clusters) primary outcome PrEP adherence. |
Transgender women in Lima, Peru |
Web 2.0/social media | Primary acquisition |
| Blacks tock ALBER EINSTEIN COLLEGE OF MEDICINE |
2014–19 | “Sisters-GPS”: intervention to improve ART adherence adapted from the group clinical visit model and incorporating social media. Pilot RCT with primary outcome of ART adherence; secondary outcomes HIV viral load and health care utilization. |
HIV+ African American and Latina women |
Web 2.0/social media | Retention in care ART adherence |
| Patel ALBERT EINSTEIN COLLEGE OF MEDICINE |
2014–19 | “E-PrEP”: a social media-based peer-led intervention to promote PrEP uptake via online messaging and discussions directed by peer leaders to provide education on PrEP, increase interest in PrEP use, and facilitate access to PrEP. Pilot RCT to assess feasibility and preliminary efficacy for increasing self-reported intention in and uptake of PrEP. |
Men of color who have sex with men, age 18–29 |
Web 2.0/social media | Primary acquisition |
| Merchant RHODE ISLAND HOSPITAL |
2014–16 | Study aims to evaluate use of a social-networking website to facilitate HIV testing and dissemination through an RCT. Primary outcomes: testing uptake, time to initiation of testing, and whether participants invite their ‘online’ or ‘offline’ contacts to use this new type of test. |
Black, Hispanic, and white MSM, age 18- 24 |
Web 2.0, social networking |
HIV testing |
| Miller UNIVERSITY OF SOUTHERN CALIFORNIA |
2008–15 | SOLVE (Socially Optimized Learning in Virtual Environments) integrates cognitive approaches with affect- based and reactive risky decision-making processes, providing experience with risk cues in a safe, virtual environment. RCT being conducted online: testing and risk situations using Intelligent Agent and Gaming technologies. Primary outcomes: UAI change with casual partners. Significant 3- and 6- month findings to date. |
MSM, age 18–24 | Virtual reality | Primary acquisition HIV testing |
| Fiellin YALE UNIVERSITY |
2009–15 | Retro-Warriors’ study will adapt existing software for an interactive video game designed to decrease HIV risk by teaching sex, drug and alcohol negotiation and refusal skills. Intervention will be tested in an RCT (n=330) with primary outcome: initiation of sexual activity; secondary outcomes: HIV risk behavior knowledge, social competency, self-efficacy, drug/alcohol use behaviors and overall risk-taking behaviors. |
Minority youth, age 9–14 | Interactive gaming | Primary acquisition |
| Enah UNIVERSITY OF ALABAMA AT BIRMINGHAM |
2012–15 | Study will develop a prototype for an individually tailored, electronic HIV prevention adventure game designed to improve decision- making and learn behavioral strategies that assist with avoiding sexual risk behaviors. Intervention prototype will be tested (n=40) for acceptability and relevance. |
African American rural youth, age 12–14 |
Interactive gaming | Primary acquisition |
| McLaughlin RADIANT CREATIVE GROUP, LLC |
2012–15 | It’s Your Game- Family’: online game intervention provides age- appropriate sexual health life skills education and training for children and to enhance parents’ skills in support of this training. Supports ongoing pregnancy and HIV/STD prevention education. Study will develop and test IYG-F in a pilot RCT in 80 homes. Primary outcomes: children: intentions for abstinence, psychosocial determinants of sexual behavior, adults: psychosocial determinants regarding parent-child sexual health communication and parental monitoring, beliefs about youth sexual behavior, both: increased sexual health communication. |
Children, age 11–14 and their parents |
Interactive gaming | Primary acquisition |
| McDaniel VIRTUALLY BETTER, INC. |
2014–16 | “Tough Talks” will be an internet-delivered software program with intelligent virtual character-driven scenarios focused on increasing skills associated with disclosure of HIV status. |
HIV+ young MSM | Virtual reality | Secondary transmission |
IDU Injection drug user; RCT randomized controlled trial; HIV+ HIV-infected; MSM men who have sex with men; STD sexually transmitted infections; UAI unprotected anal intercourse
For each prevention approach, we begin by highlighting evidence from randomized controlled trials (RCTs). In the absence of data from RCTs, we describe results from pilot trials and study protocols. Following the continuum of care framework, we organize the results in terms of mode of delivery (e.g. web based, mobile, smartphone app) and point of intervention along the care continuum. As noted throughout, and displayed in Table 3, a number of interventions target more than one area along the continuum and/or use multiple modes of technology.
Table 3.
eHealth interventions across the HIV continuum of prevention and care: published and under development
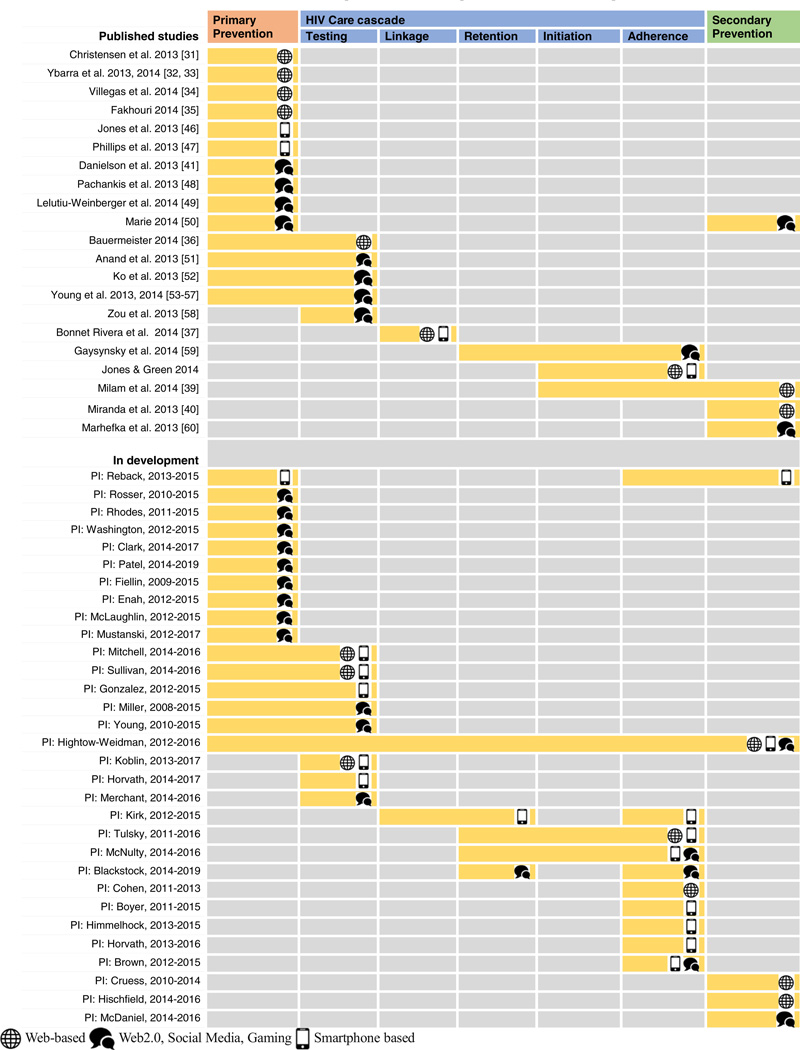 |
Note: Pillai 2014–15 excluded from Figure 1 as stage of cascade addressed in intervention is unclear
I. Web-Based Interventions
Within peer-reviewed published literature, the web continues to be the predominant mode for intervention delivery. Overall, ten published studies [31•, 32–40] and eight studies underway applied web-based interventions. Focus areas across the HIV continuum of prevention and care included eight primary prevention interventions, five testing interventions, two for linkage to care, two focused on retention, four focused on ART initiation, four focused on ART adherence, and five for secondary prevention (Table 3).
Prevention of Primary Acquisition and/or Secondary Transmission
The majority of the interventions completed in the last year have focused on prevention of primary HIV acquisition. Danielson et al. developed a web-based adaptation of the evidence-based intervention, Sistas, Informing, Healing, Living, and Empowering (SiHLE). The pilot study demonstrated increases in HIV/STI knowledge, risk reduction, and condom use self-efficacy [41•]. Ybarra et al. conducted a large pilot trial of CyberSenga, an internet-based intervention informed by the Information-Motivation-Behavior model for HIV prevention among 366 secondary school students in Uganda to increase abstinence and condom use, and teach about healthy relationships, communication and decision-making skills. While there was an increased level of abstinence at the three month follow-up between the intervention and control (81% vs. 74%, p=0.08), there were no significant differences in the main outcomes at 6 months [32, 33]. This type of intervention decay has been seen in other behavioral interventions delivered online and in person [42, 43].
Milam et al. presented results from their controlled trial of an internet-based risk reduction intervention in HIV-positive men who have sex with men (MSM) who reported recent unprotected sex or STIs. Participants at three US HIV clinics were randomized (1:1) to either a monthly behavioral risk survey instrument alone or combined with tailored internet-based prevention messages based on their self-reported risk of HIV transmission. Intervention arm messages targeted condom use, ART use, disclosure of HIV status, and reducing substance use. Syphilis, gonorrhea and Chlamydia were assessed at baseline and every 3 months. The internet-based risk reduction intervention showed no evidence for efficacy in reducing incident STIs among these subjects [39].
HIV Testing
Despite recommendations to increase and routinize HIV testing, an estimated 15% of persons in US [44] and 54.3% of persons worldwide [45] are unaware of their HIV-positive serostatus. Bauermeister et al. presented findings of an intervention designed to provide young MSM (age 15–24) with tailored, motivational content around HIV/STI testing alongside a testing locator. Those who received the intervention (compared to the testing locator only) were more likely to visit an HIV/STI testing clinic and report higher testing self-efficacy. The intervention also saw decreases in reports of the number of overall sex partners as well as the number of condomless anal sex partners in the prior 30 days [36].
II. Mobile Web/Smartphone Apps
Our review identified four published studies [37, 38, 46, 47] and 14 studies underway utilizing smartphone-based interventions for HIV prevention and care. These include seven interventions focused on primary prevention, six addressing testing, three for linkage to care, four for retention in care, four for initiation of ART, ten for ART adherence, and two for secondary prevention (Table 3). Of note, all interventions identified for retention in care and secondary prevention were still in the development phase.
Prevention of Primary Acquisition and/or Secondary Transmission
Jones et al. tested the use of smartphones for the delivery of HIV prevention messages to women in an RCT, comparing 12 weekly videos of the educational soap opera Love, Sex, and Choices to 12 weekly HIV prevention messages [46]. Baseline and follow-up interviews at 3 and 6 months were completed by an audio computer-assisted self-interview (ACASI). The primary study outcome measure of unprotected vaginal and anal sex with a high-risk partner was significantly lower at follow-up for both treatment arms (p<.001) compared to baseline. These reductions were dramatic with median risk behavior falling from about 21 to 22 unprotected vaginal sex act equivalents in the prior 3 months at pre-intervention to five to six such acts post intervention. The authors concluded that both smartphone interventions were viable for HIV prevention [46].
Phillips et al. evaluated the feasibility and acceptability of the Safe in the City intervention modified for “on-demand” delivery on a handheld device among opioid-dependent patients in methadone maintenance therapy [47]. The interactive mobile HIV Risk Reduction modules consisted of three components: videos, questions about videos’ acceptability, and questions about videos’ perceived effectiveness. All three videos met a priori criteria for acceptability and feasibility and participants answered 92% of HIV/STI knowledge questions correctly post-video [47].
III. Web 2.0/Social Media
Numerous studies employed innovative demonstration of Web 2.0 and social media website and apps including the use of Facebook, gamification, and interactive graphical interfaces (discussed in more detail in section IV, below). We found 10 published interventions [41•, 48–56, 57••, 58–60] and 17 studies underway utilizing Web 2.0 technologies. These include 19 focused on primary prevention, eight addressing testing, one for linkage to care, four for retention in care, three for initiation of ART, five for ART adherence, and four for secondary prevention (Table 3).
Prevention of Primary Acquisition and/or Secondary Transmission
Lelutiu-Weinberger et al. tested the feasibility, acceptability and preliminary efficacy of a live chat intervention delivered on Facebook for reducing condomless anal sex and substance use within a group of high risk young MSM (YMSM) in a pre-post-test design with no control group [49]. Participants (N= 41; 18–29 years old) completed up to eight one-hour motivational interviewing and cognitive behavioral skills-based online live chat intervention sessions. Analyses indicated that participation in the intervention (n=31) was associated with reductions of days of drug and alcohol use in the past month and instances of anal sex without a condom (including under the influence of substances), as well as increases in knowledge of HIV-related risks at three-month follow-up [49].
HIV Testing
Within Project Hope, 16 peer leaders were randomly assigned to deliver either HIV information and promote free home-based HIV tests (intervention) or general health information (control) over 12 weeks through closed Facebook groups [55]. The intervention was delivered to 112 MSM (85% African American). Compared to the control group, those in the intervention were more likely to request home-based HIV testing kits: 44% vs. 20%; and take and return test kits: 36% vs. 18% [57••]. Retention in this study was very high: 93% at 12 weeks and 82% at 12 months [61].
While Facebook has been the primary site of most Web 2.0 interventions to date, researchers in China used a combination of active (instant messaging, chat rooms, mobile phones, email) and passive (website banner ads) methods to promote voluntary counseling and testing (VCT) among 3332 MSM. Overall, 12.9% of men contacted (n = 429) were tested at designated VCT clinics. Instant messaging was the most effective mode for promotion: one of four men contacted went in for testing, while email was least effective (1:140). Compared to passive recruitment, active recruitment mechanisms yielded men who were significantly younger and more likely to have never tested for HIV or tested less frequently [58].
There have been a number of online interventions that resulted from adaptation of existing in-person evidence-based or evidence-informed interventions to be delivered online [34, 38, 41•, 52]. For example, Ko et al. adapted CDC’s Popular Opinion Leader (POL) intervention to develop an online version (iPOL) which trained peers to disseminate information about HIV, risk reduction, and behavior change; and to ask and respond to questions via Facebook [52]. 369 iPOLs reached 959, 088 persons on Facebook in 6 months. At six-month follow-up, those in the intervention arm were more likely than those in the information-only control to: receive HIV-related information (25.5% vs 10.5%, p<0.001), discuss HIV issues with others (41.9% vs 23.8%, p<0.001), review articles about HIV (90.6% vs 79.7%, p<0.001), be asked about or discuss HIV-related questions (51.1% vs 31.8%, p<0.001), have HIV tested within 6 months (43.9% vs 22.3, p<0.001%), and to avoid condomless anal intercourse with partners met online (34.2% vs 26.2%, p=0.004) [52].
Linkage and Retention in Care
Gaysynsky et al. describe the integration of Facebook into an HIV treatment program serving adolescents and young adults infected with HIV (Young Adult Program – YAP). Content analysis was applied to 3838 posts and comments that appeared on the YAP Facebook wall over a 15-month period (3/1/11 −7/1/12). Most of the interactions on the Facebook page during the course of the study period were positive, and a substantial amount of social support was observed. Of the 3838 posts and comments analyzed, 6.6 % (255) sought some kind of social support and 15.1% (578) provided (or offered to provide) some type of social support, demonstrating that social networking sites may offer effective ways for health organizations to communicate with young adults [59].
IV. New Trends and Developments in mHealth Interventions
The US National Institutes of Health (NIH) has recently funded a number of new HIV prevention and care interventions that apply mHealth and eHealth technologies (Table 2). While some employ established technologies, there is a noteworthy trend toward greater integration of individual user tailoring via interactive and role-playing elements. We highlight these interventions as examples of what the field can expect to see in the published literature over the next few years.
Provision of Real-time Feedback
Several interventions attempt to monitor behaviors over time and offer real-time feedback at key moments in order to influence positive behavior change (also called Ecological Momentary Assessment [28]) [41•]. One newer intervention under development, iHAART, delivers personalized adherence interventions with content and “dose” that adapt in real time to variable medication adherence in HIV-infected stimulant users (methamphetamine, cocaine, MDMA). A three-month pilot study is planned to test functionality and acceptability (PI: Boyer). In another example, eMOCHA (electronic Mobile Open-source Comprehensive Health Application), investigators are developing an app to assist peer navigators deliver individually-tailored interventions to HIV-infected injection drug users who are out of care. Ecologic momentary analysis is being used to trigger either phone call or visit from the peer navigator or automated, context-specific messages (PI: Kirk).
Gaming and Gamification
Gamification uses game-related design components and principles along with psychology in non-traditional gaming contexts and represents a unique opportunity for meaningful and sophisticated ways to engage participants in online health behavior interventions [62, 63]. Components of gamification may enhance the degree and depth of participant interaction, increase behavior change learning opportunities and improve intervention appeal for youth. We draw attention to two interventions focused on youth (ages 9–14) that address prevention of primary acquisition of HIV/STIs delivered using two popular gaming systems (e.g. Playstation, Wii). Retro-Warriors’ is an interactive video game in development designed to decrease HIV risk by teaching sex, drug and alcohol negotiation and refusal skills to youth, aged 9–14 (PI: Fiellin). In a second example, investigators at the University of Alabama are developing an unnamed individually tailored, electronic HIV prevention adventure game designed to improve decision-making and learn behavioral strategies that assist with avoiding sexual risk behaviors among African American rural adolescents, age 12–14 (PI: Enah).
Another intervention that uses game-based principles is healthMpowerment.org (HMP). HMP is a mobile-phone-optimized internet-based intervention for young black MSM that provides information, resources, tailored feedback, and social networking platforms for social support. As participants engage with material on the site (e.g. read articles, submit posts), they acquire points to spend on real items in the HMP store (e.g. water bottles, sweatshirts) and they move up status levels on the site. Pilot studies supported the feasibility and acceptability of this intervention [64–66]. A state-wide RCT is currently underway in North Carolina (n=474) and outcomes include reduced unprotected anal intercourse (UAI) in the past 3 months (primary), depression, social support, viral load/CD4, adherence, testing, HIV knowledge, and substance use (PI: Hightow-Weidman).
We also highlight two interventions in development that focus on increasing medication adherence through gamification. Epic Allies™ is a mobile phone app that utilizes game mechanics and social networking features to improve and optimize ART uptake and adherence among YMSM. This app will be tested in an RCT (n=300) through 14 sites of the Adolescent Trials Network. Outcome measures include engagement with medical providers, medical appointment consistency, ART uptake, medication adherence, viral suppression, and CD4 count (PI: McNulty).
In an intervention being developed by Brown, participants will gain smartphone access to an engaging and immersive gaming app each time they open their medication bottle (via wireless connection between the pill bottle cap and participant’s smartphone). While gaming, participants will gain information about their health, improve motivation for ART and medical appointment adherence, and practice healthy behaviors. The intervention will be tested in a pilot RCT (n=60) with medication adherence and viral load measures as primary outcomes.
Virtual Reality
Virtual Reality (VR) scenarios are computerized, interactive role-playing games that can yield engaging, ecologically valid, and user-centric content. Within the field of HIV, these interventions are designed to increase mastery of important skills associated with sexual health promotion, effectively address affect management, and provide more robust situation-specific intervention techniques (e.g. practicing HIV status disclosure or condom negotiation skills). VR can supplement or take the place of traditional in-person role-playing exercises, which are limited by numerous factors including the prior relationship between the health provider and participant, appropriate ethical constraints, and scalability [67]. These limitations make for highly artificial “practice” that is unlikely to elicit the actual reactions, both emotional and physiological that individuals encounter in real life.
“Tough Talks” is a disclosure intervention for HIV-infected YMSM, which aims to create an internet-delivered software program that will offer intelligent virtual character-driven scenarios focused on increasing mastery of important skills associated with disclosure of HIV status. The intervention will address sexual health communication with sex partners in the context of disclosing HIV status using artificially intelligent technology (e.g. avatars) and natural language processing.
Another example, “SOLVE: Socially Optimized Learning in Virtual Environments (SOLVE)”, has created “virtual date” narratives based on extensive formative research with MSM. In a national online survey among HIV-uninfected MSM (n=921) they found significant shame reduction and decrease in UAI compared to a wait-list control group [31•]. Significant effects were maintained at 6 months follow-up (author personal communication).
Conclusion
The advantages of internet and mobile-based interventions include the potential to provide consistency in the delivery of an intervention, potential low cost once developed, and the ability to disseminate the intervention to a wider population. Advances in technology offer a wide range of approaches, from the most straightforward use of mobile phones to send reminders or track information to a full suite of capabilities within smartphones (e.g. GPS, sensors) and beyond. While there has been significant progress over the past year, there is still a lack of long term and large-scale efficacy outcome studies. Given the many pilot studies and studies in development, we can expect to see a substantial increase in available results in the coming years. Importantly, as shown in the bottom half of Table 3, the pipeline of interventions appears to acknowledge the importance of the HIV Care Continuum and the necessary combination of behavioral and biomedical interventions across the various stages. The middle of the care continuum (i.e. link, retain, initiate ART) remains an area open for further development.
Confirming what others have noted, our review identified a predominant number of completed and planned interventions conducted within the United States (U.S.) and focused on MSM [68•]. This leaning, in part, reflects the defined nature of this review which excluded text-based interventions, a number of which have been conducted in non-US settings (see [69–72] for recent reviews of SMS-based HIV/AIDS interventions). This pattern also reflects the unequal distribution of technology worldwide, the American HIV epidemic, and MSM’s early adoption of new technologies and social media, including geosocial smartphone apps to meet sex partners [73, 74].
Smartphone uptake is increasing globally and changing the way we access the internet. More than 1.75 billion people are expected to own and use smartphones by the end of 2014, up more than 25% over 2013 [75]. Users in Western Europe and the Asia-Pacific region make up the greatest number of users, with consumers in Asia-Pacific accounting for more than half of all smartphone users in 2014 [75]. Expansion of smartphone penetration in non-industrialized countries will impact our ability to affect HIV outcomes globally in a meaningful way. A critical first step requires local assessments to understand a target populations’ technology access and use (e.g. hardware ownership, development platforms, subscription plans, usage patterns and preferences). For example, while Android and iOS (Apple) continue to be the top two mobile operating systems globally (holding over 80% and 10% of market share in the second quarter of 2014, respectively) [76], usage among key demographics may favor one or the other. This information is a critical starting point for appropriately tailored app development and dissemination. Throughout intervention development and implementation, research teams need to continue monitoring the local market and have a flexible intervention approach that can adapt to changes in technology uptake and usage within diverse populations and geographies.
Working in developing countries, particularly among MSM, requires a high sensitivity and awareness of safety, security, and privacy issues. MSM face high levels of stigmatization in many settings: In five countries and in parts of two others, homosexuality is still punishable with the death penalty, while a further 70 countries may imprison citizens because of their sexual orientation [77]. In addition, government monitoring and restrictions on technology access can pose problems including lack of trust and the ability to design engaging, explicit and appealing content. For example, the Chinese government maintains strict control over the internet through a variety of censoring, blocking, and monitoring tactics [78, 79]. At the same time, web-based technologies may offer more discrete access to health information (as compared to clinic settings) in countries where sexuality, sexual behaviors and HIV/STI are highly stigmatized. Regardless of the setting, in-depth assessment and qualitative research are needed to ensure protection of individuals and position programs for better success [80].
There are a number of lessons we can learn from researchers who have tried to use smartphone and Web 2.0-based technologies for HIV prevention and care. First, future interventions will need to be mindful of eHealth literacy inequities in the population, as well as account for constant changes in the popularity and emergence of social media platforms and devices themselves. Second, challenges exist between different “languages” spoken and overall goals of programmers, researchers, and end-users. Aims of app development and definitions of success may differ between researchers and programmers, and each may be responding to different perceived needs of end users. Teams can address some of these differences through continuous formative research with the target population during intervention development and creating very explicit deliverables, timelines, and division of labor within the development team. These first and second points emphasize the importance of designing technology-based interventions with the end user constantly in mind to create something that is intuitive, useful, engaging and fun [80].
Lastly, a number of funding challenges are inherent to this research. Investigators may have difficulty devoting sufficient money to design, programming and/or dissemination either due to budget limitations, inexperience, or unexpected technology challenges. In addition, the required development process for technology projects is not necessarily well-aligned with standard federal funding mechanisms and timelines; The accelerated pace of technology evolution is driven by commercial markets, and is often at odds with the typical speed of funding application, review and reward cycles, as well as with typical research timelines. Technology interventions that are tested through this cycle run the risk of being outdated by the time intervention results are ready for dissemination. Additional funding may need to be explicitly earmarked to expedite the technology transfer pipeline from prototype to pilot trial and efficacy trial if we are to be responsive to the rapid changes in technology.
Going forward, we foresee HIV care and prevention intersecting with novel technology advances such as quantified self-movement and geolocation, self-monitoring of physiological and emotional states (e.g. mood, arousal), and performance (mental and physical) in the near future. These advances will be vital to ensure the success of integrated sustained, behavioral modification and biomedical strategies for prevention and care. Additionally, while establishing efficacy is of course critical, many of these studies have yet to demonstrate effectiveness through scale-up, a key issue in increasing access and dissemination for HIV prevention. As with biomedical interventions, we need to explore ways to ensure that “what works” within eHealth, mHealth, and Web 2.0 can be accessed and widely utilized by populations at risk for HIV.
Acknowledgments
Conflict of Interest Kathryn E. Muessig, Manali Nekkanti, Jose Bauermeister, and Sheana Bull report that they have NIH-funded grants.
Lisa B. Hightow-Weidman reports personal fees from Gilead Sciences and personal fees from Janssen Therapeutics.
Footnotes
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
Kathryn E. Muessig, Email: kmuessig@med.unc.edu, Department of Health Behavior, University of North Carolina at Chapel Hill, 306 Rosenau Hall, Campus Box 7440, Chapel Hill, NC 27599-7440, USA.
Manali Nekkanti, Email: nekkanti@live.unc.edu, Department of Health Behavior, University of North Carolina at Chapel Hill, 306 Rosenau Hall, Campus Box 7440, Chapel Hill, NC 27599-7440, USA.
Jose Bauermeister, Email: jbauerme@umich.edu, Department of Health Behavior and Health Education, School of Public Health, University of Michigan, 1415 Washington Heights, SPH I, Room 3822, Ann Arbor, MI 48109-2029, USA.
Sheana Bull, Email: Sheana.Bull@ucdenver.edu, Department of Community and Behavioral Health, University of, Colorado School of Public Health, 13001 E. 17th Place, Box B119, Aurora, CO 80045, USA.
Lisa B. Hightow-Weidman, Email: lisa_hightow@med.unc.edu, Department of Medicine, University of North Carolina at Chapel, Hill, 130 Mason Farm Road, Bioinformatics Building CB#7030, Chapel Hill, NC 27599, USA.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis. 2013;57:1164–1171. doi: 10.1093/cid/cit420. [DOI] [PubMed] [Google Scholar]
- 2.Greenberg AE, Hader SL, Masur H, Young AT, Skillicorn J, Dieffenbach CW. Fighting HIV/AIDS in Washington, D.C. Health Aff (Millwood) 2009;28:1677–1687. doi: 10.1377/hlthaff.28.6.1677. [DOI] [PubMed] [Google Scholar]
- 3.Cohen MS, McCauley M, Sugarman J. Establishing HIV treatment as prevention in the HIV Prevention Trials Network 052 randomized trial: an ethical odyssey. Clin Trials. 2012;9:340–347. doi: 10.1177/1740774512443594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen MS, Smith MK, Muessig KE, Hallett TB, Powers KA, Kashuba AD. Antiretroviral treatment of HIV-1 prevents transmission of HIV-1: where do we go from here? Lancet. 2013;382:1515–1524. doi: 10.1016/S0140-6736(13)61998-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grant RM, Anderson PL, McMahan V, Liu A, Amico KR, Mehrotra M, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14:820–829. doi: 10.1016/S1473-3099(14)70847-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Catalani C, Philbrick W, Fraser H, Mechael P, Israelski DM. mHealth for HIV Treatment & Prevention: A Systematic Review of the Literature. Open AIDS J. 2013;7:17–41. doi: 10.2174/1874613620130812003.. This article presents a detailed review of mHealth interventions to support HIV care (up to December 2011). See especially, the detailed assessment of these studies presented in the article’s Tables 1 and 2.
- 9.Sullivan PS, Grey JA, Simon Rosser BR. Emerging technologies for HIV prevention for MSM: what we have learned, and ways forward. J Acquir Immune Defic Syndr. 2013;63(Suppl 1):S102–S107. doi: 10.1097/QAI.0b013e3182949e85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Allison S, Bauermeister JA, Bull S, Lightfoot M, Mustanski B, Shegog R, et al. The intersection of youth, technology, and new media with sexual health: moving the research agenda forward. J Adolesc Health. 2012;51:207–212. doi: 10.1016/j.jadohealth.2012.06.012.. This article summarizes proceedings and key recommendations from a March 2011 joint meeting of the Internet Sexuality Information Services, National Institute of Mental Health, and the Ford Foundation. The meeting aimed to address the state and possibilities of using new forms of technology for sexual health promotion research. Successful case studies were presented as well as topical discussions around research-community partnerships, research ethics, use of theory, intervention approaches, recruitment methods, and measuring impact.
- 11.Noar SM, Pierce LB, Black HG. Can Computer-Mediated Interventions Change Theoretical Mediators of Safer Sex? A Meta-Analysis. Human Communication Research. 2010;36:261–297. [Google Scholar]
- 12.Noar SM, Black HG, Pierce LB. Efficacy of computer technology-based HIV prevention interventions: a meta-analysis. AIDS. 2009;23:107–115. doi: 10.1097/QAD.0b013e32831c5500. [DOI] [PubMed] [Google Scholar]
- 13.Selmi PM, Klein MH, Greist JH, Sorrell SP, Erdman HP. Computer-administered cognitive-behavioral therapy for depression. Am J Psychiatry. 1990;147:51–56. doi: 10.1176/ajp.147.1.51. [DOI] [PubMed] [Google Scholar]
- 14.Newman MG, Kenardy J, Herman S, Taylor CB. Comparison of palmtop-computer-assisted brief cognitive-behavioral treatment to cognitive-behavioral treatment for panic disorder. J Consult Clin Psychol. 1997;65:178–183. doi: 10.1037//0022-006x.65.1.178. [DOI] [PubMed] [Google Scholar]
- 15.Lenert L, Munoz RF, Stoddard J, Delucchi K, Bansod A, Skoczen S, et al. Design and pilot evaluation of an internet smoking cessation program. J Am Med Inform Assoc. 2003;10:16–20. doi: 10.1197/jamia.M1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feil EG, Noell J, Lichtenstein E, Boles SM, McKay HG. Evaluation of an Internet-based smoking cessation program: lessons learned from apilot study. Nicotine Tob Res. 2003;5:189–194. doi: 10.1080/1462220031000073694. [DOI] [PubMed] [Google Scholar]
- 17.Woodruff SI, Edwards CC, Conway TL, Elliott SP. Pilot test of an Internet virtual world chat room for rural teen smokers. J Adolesc Health. 2001;29:239–243. doi: 10.1016/s1054-139x(01)00262-2. [DOI] [PubMed] [Google Scholar]
- 18.Sciamanna CN, Lewis B, Tate D, Napolitano MA, Fotheringham M, Marcus BH. User attitudes toward a physical activity promotion website. Prev Med. 2002;35:612–615. doi: 10.1006/pmed.2002.1103. [DOI] [PubMed] [Google Scholar]
- 19.Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. JAMA. 2003;289:1833–1836. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- 20.Tate DF, Wing RR, Winett RA. Using Internet technology to deliver a behavioral weight loss program. JAMA. 2001;285:1172–1177. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- 21.Napolitano MA, Fotheringham M, Tate D, Sciamanna C, Leslie E, Owen N, et al. Evaluation of an internet-based physical activity intervention: a preliminary investigation. Ann Behav Med. 2003;25:92–99. doi: 10.1207/S15324796ABM2502_04. [DOI] [PubMed] [Google Scholar]
- 22.Pew Resesarch Center Internet Project. [Accessed 31 Oct 2014];“Cell Phone and Smartphone Ownership Demographics.”. 2014 Available at: http://www.pewinternet.org/data-trend/mobile/cell-phone-and-smartphone-ownership-demographics/.
- 23.Pew Research Center Global Attitudes Project. [Accessed 31 Oct 2014];“Emerging Nations Embrace Internet, Mobile Technology.”. 2014 Feb 13; Available at: http://www.pewglobal.org/2014/02/13/emerging-nations-embrace-internet-mobile-technology/.
- 24.Muessig KE, Pike EC, Legrand S, Hightow-Weidman LB. Mobile phone applications for the care and prevention of HIV and other sexually transmitted diseases: a review. J Med Internet Res. 2013;15:e1. doi: 10.2196/jmir.2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Horvath T, Azman H, Kennedy GE, Rutherford GW. Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection. Cochrane Database Syst Rev. 2012;3:Cd009756. doi: 10.1002/14651858.CD009756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Robustillo Cortes Mde L, Cantudo Cuenca MR, Morillo Verdugo R, Calvo Cidoncha E. High Quantity But Limited Quality in Healthcare Applications Intended for HIV-Infected Patients. Telemed J E Health. 2014;20:729–735. doi: 10.1089/tmj.2013.0262.. This article reviews available smartphone applications (up to May 2013) for HIV care. Specifically assesses the quality of information provided. Includes a novel weighted ranking system. Only 1 out of 41 apps received the highest score of “A”, while 27/41 (65.9%) scored in the lowest class, “F”, not even meeting minimal criteria. Includes Spanish-language apps.
- 27.Duggan M, Smith A. Pew Research Internet Project. Washington DC: 2013. Dec 30, [Accessed 31 Oct 2014]. Social Media Update 2013. Available at: http://www.pewinternet.org/2013/12/30/social-media-update-2013/. [Google Scholar]
- 28. [Accessed 31 Oct 2014];Grindr:The world’s biggest mobile network of guys. Available at: http://grindr.com/learn-more.
- 29.Lapowsky I. Tinder May Not Be Worth $5B, But It’s Way More Valuable Than You Think. [Accessed 31 Oct 14];Wired Magazine. 2014 Apr 11; published online Available at: http://www.wired.com/2014/04/tinder-valuation/.
- 30. Grov C, Breslow AS, Newcomb ME, Rosenberger JG, Bauermeister JA. Gay and bisexual men’s use of the Internet: research from the 1990s through 2013. J Sex Res. 2014;51:390–409. doi: 10.1080/00224499.2013.871626.. This article presents a thorough historical review of the role and evolution of the Internet and sex (and HIV research/intervention) for MSM. The review is divided and presented chronologically into the following periods: 1990s, 2000–2004, 2005–2009, and 2010–2014 – with this last period focused on the mobile web and social media.
- 31. Christensen JL, Miller LC, Appleby PR, Corsbie-Massay C, Godoy CG, Marsella SC, et al. Reducing shame in a game that predicts HIV risk reduction for young adult MSM: a randomized trial delivered nationally over the Web. JInt AIDS Soc. 2013;16:18716. doi: 10.7448/IAS.16.3.18716.. This article presents 3-month follow-up findings from SOLVE (Socially Optimized Learning in Virtual Environments), an online intervention aimed to reduce UAI indirectly via reduced stigma/shame. 3 month follow-up found significant shame reduction, p< 0.001; significant decrease in UAI: (point estimate −0.10, 95% CI[−0.01 to −0.23]. 6 month follow-up data is also significant and will be forthcoming in 2014–2015.
- 32.Ybarra ML, Bull SS, Prescott TL, Korchmaros JD, Bangsberg DR, Kiwanuka JP. Adolescent abstinence and unprotected sex in CyberSenga, an Internet-based HIV prevention program: randomized clinical trial of efficacy. PLoS One. 2013;8:e70083. doi: 10.1371/journal.pone.0070083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ybarra ML, Bull SS, Prescott TL, Birungi R. Acceptability and feasibility of CyberSenga: an Internet-based HIV-prevention program for adolescents in Mbarara, Uganda. AIDS Care. 2014;26:441–447. doi: 10.1080/09540121.2013.841837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Villegas N, Santisteban D, Cianelli R, Ferrer L, Ambrosia T, Peragallo N, et al. The development, feasibility and acceptability of an Internet-based STI-HIV prevention intervention for young Chilean women. Int Nurs Rev. 2014;61:55–63. doi: 10.1111/inr.12080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fakhouri T. Data collection in games for health. YTH Live Conference; April 6–8, 2014; San Francisco, CA. Available at: http://www.slideshare.net/isisinc/data-collection-in-games-for-health. [Google Scholar]
- 36.Bauermeister J. Get Connected: A Tailored web intervention for young MSM. YTH Live Conference; April 6–8, 2014; San Francisco, CA. Available at: http://www.slideshare.net/isisinc/get-connected-a-tailored-web-intervention-for-young-msm. [Google Scholar]
- 37.Bonnet Rivera AM, Garcia Perez WG. Innovative Strategies to Expand Access to HIV testing, Increase linkage to Care Among High-Risk Latino Young Men who Have Sex With Men (YMSM) in Puerto Rico. United States Conference on AIDS; October 2–5, 2014; San Diego, CA. p. 117. Abstract available at: http://www.nmac.org/pdf/Digital%20USCA%20Program%20Book%28Rev%209-29-2014%29.pdf. [Google Scholar]
- 38.Jones R, Green K. Every Dose Every Day: Innovative E-learning Toolkit Supporting Prevention with Positive Persons. United States Conference on AIDS; October 2–5, 2014; San Diego, CA. p. 74. Abstract available at: http://www.nmac.org/pdf/Digital%20USCA%20Program%20Book%28Rev%209-29-2014%29.pdf. [Google Scholar]
- 39.Milam J, Jain S, Daar E, Dube M, Seefreid E, Ellorin E, et al. Controlled Trial of an Internet-Based Risk Reduction Intervention in HIV+ Men Who Have Sex With Men. Conference on Retroviruses and Opportunistic Infections (CROI); March 3–6, 2014; Boston, MA. Poster #943, http://croi2014.org/sites/default/files/uploads/CROI2014_Final_Abstracts.pdf. [Google Scholar]
- 40.Miranda J, Cote J, Godin G, Blais M, Otis J, Gueheneuc YG, et al. An Internet-Based Intervention (Condom-Him) to Increase Condom Use Among HIV-Positive Men Who Have Sex With Men: Protocol for a Randomized Controlled Trial. JMIR Res Protoc. 2013;2:e39. doi: 10.2196/resprot.2723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Danielson CK, McCauley JL, Jones AM, Borkman AL, Miller S, Ruggiero KJ. Feasibility of delivering evidence-based HIV/STI prevention programming to a community sample of African American teen girls via the internet. AIDS Educ Prev. 2013;25:394–404. doi: 10.1521/aeap.2013.25.5.394.. This article presents a pilot study of a web adaptation of the CDC evidence-based intervention, Sistas, Informing, Healing, Living, and Empowering, among 41 African American women, age 13–18. Pre-post study, the authors found significant increases in HIV/STI risk knowledge and condom use self-efficacy.
- 42.Bull SS, Levine DK, Black SR, Schmiege SJ, Santelli J. Social media-delivered sexual health intervention: a cluster randomized controlled trial. Am J Prev Med. 2012;43:467–474. doi: 10.1016/j.amepre.2012.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Copenhaver MM, Lee IC. Examining the decay of HIV risk reduction outcomes following a community-friendly intervention targeting injection drug users in treatment. J Psychoactive Drugs. 2007;39:223–229. doi: 10.1080/02791072.2007.10400608. [DOI] [PubMed] [Google Scholar]
- 44.US Centers for Disease Control and Prevention. National HIV Prevention Progress Report, 2013. Atlanta, GA: 2013. Dec, [Accessed 31 Oct 14]. Available at: http://www.cdc.gov/hiv/pdf/policies_NationalProgressReport.pdf. [Google Scholar]
- 45.UNAIDS. The Gap Report. Geneva: 2014. [Accessed 31 Oct 14]. Available at: http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2014/UNAIDS_Gap_report_en.pdf. [Google Scholar]
- 46.Jones R, Hoover DR, Lacroix LJ. A randomized controlled trial of soap opera videos streamed to smartphones to reduce risk of sexually transmitted human immunodeficiency virus (HIV) in young urban African American women. Nurs Outlook. 2013;61:205–215. e203. doi: 10.1016/j.outlook.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Phillips KA, Epstein DH, Mezghanni M, Vahabzadeh M, Reamer D, Agage D, et al. Smartphone Delivery of Mobile HIV Risk Reduction Education. AIDS Res Treat. 2013;2013:231956. doi: 10.1155/2013/231956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pachankis JE, Lelutiu-Weinberger C, Golub SA, Parsons JT. Developing an online health intervention for young gay and bisexual men. AIDS Behav. 2013;17:2986–2998. doi: 10.1007/s10461-013-0499-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lelutiu-Weinberger C, Pachankis JE, Gamarel KE, Surace A, Golub SA, Parsons JT. Feasibility, Acceptability, and Preliminary Efficacy of a Live-Chat Social Media Intervention to Reduce HIV Risk Among Young Men Who Have Sex With Men. AIDS Behav. doi: 10.1007/s10461-014-0911-z. epub ahead of print 26 September 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marie J. How effectively eroding STD stigma facilitates prevention. STD Prevention Conference; June 9–12, 2014; Atlanta, GA. TP 51, Abstract available in Sex Transm Diseases 2014,41(S1):S53. [Google Scholar]
- 51.Anand T, Ananworanich J, Parwati Merati T, Yunihastuti E, Imran D, Nitpolprasert C, et al. A culturally sensitive online communication campaign to reach hidden men who have sex with men for HIV/STI prevention and testing in Indonesia: TemanTeman.org. 7th IAS Conference on HIV Pathogenesis, Treatment, and Prevention; June 30 – July 3, 2013; Kuala Lumpur, Malaysia. [Accessed 10/31/2014]. Abstract #WEPE590, avilable at: http://pag.ias2013.org/Abstracts.aspx?AID=969. [Google Scholar]
- 52.Ko NY, Hsieh CH, Wang MC, Lee C, Chen CL, Chung AC, et al. Effects of Internet popular opinion leaders (iPOL) among Internet-using men who have sex with men. J Med Internet Res. 2013;15:e40. doi: 10.2196/jmir.2264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Young SD, Zhao M, Teiu K, Kwok J, Gill H, Gill N. A social-media based HIV prevention intervention using peer leaders. J Consum Health Internet. 2013;17:353–361. doi: 10.1080/15398285.2013.833445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Young SD, Jaganath D. Online social networking for HIV education and prevention: a mixed-methods analysis. Sex Transm Dis. 2013;40:162–167. doi: 10.1097/OLQ.0b013e318278bd12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Young SD, Holloway I, Jaganath D, Rice E, Westmoreland D, Project CT, et al. Online Social Network Changes in an HIV Prevention Randomized Controlled Trial for African American and Latino Men Who Have Sex With Men. Am J Public Health. 2014;104:1707–1712. doi: 10.2105/AJPH.2014.301992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Young SD, Daniels J, Chiu CJ, Bolan RK, Flynn RP, Kwok J, et al. Acceptability of using electronic vending machines to deliver oral rapid HIV self-testing kits: a qualitative study. PLoS One. 2014;9:e103790. doi: 10.1371/journal.pone.0103790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Young SD, Cumberland WG, Lee SJ, Jaganath D, Szekeres G, Coates T. Social networking technologies as an emerging tool for HIV prevention: a cluster randomized trial. Ann Intern Med. 2013;159:318–324. doi: 10.7326/0003-4819-159-5-201309030-00005.. Study presents an innovated online peer-leader diffusion of innovation intervention for minority MSM in the US which successfully increased ordering (and returning) of HIV home testing kits. Demonstrates the feasibility of using a social networking platform (Facebook) to promote testing among a key population.
- 58.Zou H, Wu Z, Yu J, Li M, Ablimit M, Li F, et al. Internet-facilitated, voluntary counseling and testing (VCT) clinic-based HIV testing among men who have sex with men in China. PLoS One. 2013;8:e51919. doi: 10.1371/journal.pone.0051919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gaysynsky A, Romansky-Poulin K, Arpadi S. “My YAP Family”: Analysis of a Facebook Group for Young Adults Living with HIV. AIDS Behav. doi: 10.1007/s10461-014-0887-8. epub ahead of print, 5 September 2014. [DOI] [PubMed] [Google Scholar]
- 60.Marhefka SL, Iziduh S, Fuhrmann HJ, Lopez B, Glueckauf R, Lynn V, et al. Internet-based video-group delivery of Healthy Relationships-a “prevention with positives” intervention: report on a single group pilot test among women living with HIV. AIDS Care. 2013;25:904–909. doi: 10.1080/09540121.2013.793266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Young SD. Social media technologies for HIV prevention study retention among minority men who have sex with men (MSM) AIDS Behav. 2014;18:1625–1629. doi: 10.1007/s10461-013-0604-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Starks K. Cognitive behavioral game design: a unified model for designing serious games. Front Psychol. 2014;5:28. doi: 10.3389/fpsyg.2014.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brox E, Fernandez-Luque L, Tollefsen T. Healthy Gaming - Video Game Design to promote Health. Appl Clin Inform. 2011;2:128–142. doi: 10.4338/ACI-2010-10-R-0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Muessig KE, Pike EC, Fowler B, LeGrand S, Parsons JT, Bull SS, et al. Putting prevention in their pockets: developing mobile phone-based HIV interventions for black men who have sex with men. AIDS Patient Care STDS. 2013;27:211–222. doi: 10.1089/apc.2012.0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.LeGrand S, Muessig KE, Pike EC, Baltierra N, Hightow-Weidman LB. If you build it will they come? Addressing social isolation within a technology-based HIV intervention for young black men who have sex with men. AIDS Care. 2014;26:1194–1200. doi: 10.1080/09540121.2014.894608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Muessig K, Baltierra N, Pike E, LeGrand S, Hightow-Weidman L. Achieving HIV risk reduction through healthmpowerment.org, a user-driven eHealth intervention for young black men who have sex with men and transgender women who have sex with men. Digital Culture & Education. 2014;6:164–182. Available at: http://www.digitalcultureandeducation.com/volume-6/muessig_et_al/ [PMC free article] [PubMed] [Google Scholar]
- 67.Albarracin D, Gillette JC, Earl AN, Glasman LR, Durantini MR, Ho MH. A test of major assumptions about behavior change: a comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychol Bull. 2005;131:856–897. doi: 10.1037/0033-2909.131.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Schnall R, Travers J, Rojas M, Carballo-Dieguez A. eHealth interventions for HIV prevention in high-risk men who have sex with men: a systematic review. J Med Internet Res. 2014;16:e134. doi: 10.2196/jmir.3393.. This systematic review (up to April 2014) for HIV prevention among MSM identified 13 relevant eHealth interventions. The diversity of outcomes and formats prevented meta-analysis but the authors conclude that findings are promising on a whole and recommend testing longer intervention periods. See especially Table 2 for comparative results.
- 69.Deglise C, Suggs LS, Odermatt P. SMS for disease control in developing countries: a systematic review of mobile health applications. J Telemed Telecare. 2012;18:273–281. doi: 10.1258/jtt.2012.110810. [DOI] [PubMed] [Google Scholar]
- 70.Finitsis DJ, Pellowski JA, Johnson BT. Text message intervention designs to promote adherence to antiretroviral therapy (ART): a meta-analysis of randomized controlled trials. PLoS One. 2014;9:e88166. doi: 10.1371/journal.pone.0088166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gurman TA, Rubin SE, Roess AA. Effectiveness of mHealth behavior change communication interventions in developing countries: a systematic review of the literature. J Health Commun. 2012;17(Suppl 1):82–104. doi: 10.1080/10810730.2011.649160. [DOI] [PubMed] [Google Scholar]
- 72.van Velthoven MH, Brusamento S, Majeed A, Car J. Scope and effectiveness of mobile phone messaging for HIV/AIDS care: a systematic review. Psychol Health Med. 2013;18:182–202. doi: 10.1080/13548506.2012.701310. [DOI] [PubMed] [Google Scholar]
- 73.Winetrobe H, Rice E, Bauermeister J, Petering R, Holloway IW. Associations of unprotected anal intercourse with Grindr-met partners among Grindr-using young men who have sex with men in Los Angeles. AIDS Care. 2014;26:1303–1308. doi: 10.1080/09540121.2014.911811. [DOI] [PubMed] [Google Scholar]
- 74.Landovitz RJ, Tseng CH, Weissman M, Haymer M, Mendenhall B, Rogers K, et al. Epidemiology, sexual risk behavior, and HIV prevention practices of men who have sex with men using GRINDR in Los Angeles, California. J Urban Health. 2013;90:729–739. doi: 10.1007/s11524-012-9766-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.eMarketer. [Accessed 23 Nov 2014];Worldwide Smartphone Usage to Grow 25% in 2014: Nine countries to surpass 50% smartphone penetration this year. 2014 Jun 11; Published online Available at: http://www.emarketer.com/Article/Worldwide-Smartphone-Usage-Grow-25-2014/1010920.
- 76.International Data Corporation (IDC Corporate USA) [Accessed 23 Nov 2014];Smartphone OS Market Share, Q2. 2014 Oct; Published online Available at: http://www.idc.com/prodserv/smartphone-os-market-share.jsp.
- 77.Itaborahy LP, Zhu JS. State-sponsored Homophobia: A world survey of laws: Criminalisation, protection and recognition of same-sex love. [Accessed 23 Nov 2014];International Lesbian Gay Bisexual Trans and Intersex Association, May 2013 Edition. Available at: http://old.ilga.org/Statehomophobia/ILGA_State_Sponsored_Homophobia_2013.pdf.
- 78.BBC News, China. [Accessed 23 Nov 2014];China employs two million microblog monitors state media say. Published online. 2013 Oct 4; Available at: http://www.bbc.com/news/world-asia-china-24396957.
- 79.Reporters Without Borders for Freedom of Information. The Enemies of Internet, Special Edition: Surveillance. China: State Enemies; [Accessed 23 Nov 2014]. Available at http://surveillance.rsf.org/en/china/. [Google Scholar]
- 80.Goldenberg T, McDougal SJ, Sullivan PS, Stekler JD, Stephenson R. Preferences for a Mobile HIV Prevention Application for Men Who Have Sex With Men. J Med Internet Res mHealth uHealth. 2014;2:e47. doi: 10.2196/mhealth.3745. [DOI] [PMC free article] [PubMed] [Google Scholar]


