Abstract
Background
We know little about patient–physician communication during visits to discuss diagnosis and treatment of prostate cancer.
Objective
To examine the overall visit structure and how patients and physicians transition between communication activities during visits in which patients received new prostate cancer diagnoses.
Participants
Forty veterans and 18 urologists at one VA medical centre.
Methods
We coded 40 transcripts to identify major communication activities during visits and used empiric discourse analysis to analyse transitions between activities.
Results
We identified five communication activities that occurred in the following typical sequence: ‘diagnosis delivery’, ‘risk classification’, ‘options talk’, ‘decision talk’ and ‘next steps’. The first two activities were typically brief and involved minimal patient participation. Options talk was typically the longest activity; physicians explicitly announced the beginning of options talk and framed it as their professional responsibility. Some patients were unsure of the purpose of visit and/or who should make treatment decisions.
Conclusion
Visits to deliver the diagnosis of early stage prostate cancer follow a regular sequence of communication activities. Physicians focus on discussing treatment options and devote comparatively little time and attention to discussing the new cancer diagnosis. Towards the goal of promoting patient‐centred communication, physicians should consider eliciting patient reactions after diagnosis delivery and explaining the decision‐making process before describing treatment options.
Keywords: discourse analysis, patient‐centred communication, prostate cancer, qualitative research, structure, transitions, veterans
Introduction
Cancer care often begins with clinic visits during which patients receive their new diagnoses and discuss treatment options. Understanding how patients and physicians communicate during these visits is an important part of promoting patient‐centred communication and effective decision making in cancer care.1 Early stage prostate cancer provides the quintessential example of this kind of visit. Patients with this disease typically attend visits during which they learn their diagnosis and in most cases consider three main treatment options – active surveillance, radiation therapy and surgical removal of the prostate – with essentially equivalent survival rates.2, 3 Researchers have therefore used early stage prostate cancer to investigate many aspects of cancer communication (e.g., risk communication,4 shared decision making5) and have built decision aids to foster treatment decisions consistent with patients' preferences.6, 7
However, the overall structure of patient–physician communication during these types of visits has not been well described. By overall structure, we mean the sequential organization of communication activities that patients and physicians navigate during visits. Understanding the overall structure of visits in which patients discuss new diagnoses and treatment options for prostate cancer is important for several reasons. It fills a gap in knowledge about how patients and physicians communicate during a kind of visit that is very different from routine outpatient and primary care visits. Empirical data on overall structure will also provide an important foundation to advance research on the links between overall structure and other aspects of communication in this setting. Finally, data on overall structure are likely to have practical implications for other well‐studied aspects of prostate cancer communication and for promoting patient‐centred communication during these visits.
In contrast to visits about cancer diagnoses, the overall structure of routine outpatient visits has been well studied, starting with Byrne and Long's landmark monograph.8 Overall structure is fundamental to communication because it comprises the framework within which all other aspects of communication take place.
Researchers have shown that the overall visit structure of routine visits is related to other aspects of communication including the ratio of physician to patient talk,9 the tension between patients' everyday experience and the world of medicine,10, 11 and the timing of patient questions.12, 13 Many strategies for improving communication such as agenda setting,14, 15 the Four Habits model,16 and patient‐centred interviewing17 were developed using empiric data about the overall structure of routine outpatient visits.
In this study, we examined the overall structure of urology clinic visits involving veterans with newly diagnosed early stage prostate cancer recorded as part of a clinical trial comparing two decision aids. We characterized the sequential organization of communication activities during these visits and analysed patient–physician communication during transitions between activities. We focused on transitions because both patients and physicians have the opportunity to initiate new topics and/or control the flow of the discussion during transitions;18, 19 as a result, communication during transitions often reveals participants' stance on the overall visit purpose.20, 21
Methods
Study data
Audio recordings were collected as part of a multisite clinical trial comparing two prostate cancer decision aids.22 Patients undergoing prostate biopsies were recruited from urology clinics between September 2008 and May 2012. Patients' prostate specific antigen (PSA) level and Gleason score (a numerical rating of prostate cancer aggressiveness based on biopsy tissue histology) were abstracted from electronic health records. Patients with a diagnosis of early stage prostate cancer (i.e. PSA <20 ng/ml and Gleason score of 6 or 7) received one of two decision aids. They were then interviewed just before receiving their cancer diagnosis and were asked what treatment they might prefer if they were to have prostate cancer. Patients could either indicate a treatment preference or defer stating a preference until after they learned their diagnosis. Physician participants were urology residents and attending physicians. All participants provided demographic data at the time of recruitment.
The clinic visit during which each patient learned of their prostate cancer diagnosis and discussed treatment options was audio recorded. A research associate set up an audio recorder in the exam room at the start of each visit and then waited outside the exam room until the visit was finished.
Sampling strategy
Data for the current study were a subset of audio recordings from one VA medical centre in the parent study. We selected a stratified purposeful sample23 based on two clinical factors likely to influence the sequential organization of communication: patients' cancer recurrence risk and patients' pre‐visit treatment preference. We characterized patients as either low risk (Gleason score of 6 and a PSA <10 ng/ml) or intermediate risk (Gleason score of 7 or a PSA ≥10 and <20 ng/ml). These categories are congruent with National Comprehensive Cancer Network Prostate Cancer Treatment Guidelines.24 We also characterized patients according to their pre‐visit treatment preference (active surveillance, surgery, radiation, or defer). We selected five audio recordings from each possible two‐way combination of recurrence risk and treatment preference from all recordings at one VA medical centre. When more than five recordings were available, we selected recordings that maximized the number of different physicians in our overall sample to capture the broadest possible range of physician communication styles.
Audio recordings were stripped of spoken identifiers (e.g. names, dates) and transcribed verbatim. This study was approved by the VA Institutional Review Boards.
Coding and data analysis
Our coding and analysis were informed by the method of empiric discourse analysis, which analyses the functions and organization of language in action during face‐to‐face interactions.25 We carried out our coding process in two steps. First, we iteratively reviewed transcripts to identify major communication activities related to the diagnosis and treatment of prostate cancer during each visit (e.g. explaining biopsy results, discussing treatment options). We used Robinson's list of communication activities during primary care visits26 as a starting point and adapted this list to reflect the activities that emerged from our data. We identified communication activities based on communicative function and linguistic features rather than on length or who was speaking. For each visit, we also calculated the approximate time spent on each activity by multiplying the proportion of the transcript spent on an activity by the total visit time measured from the audio recording.
After we identified a complete list of major communication activities, we developed a coding system to identify transitions between activities (Table 1). We defined transitions as shifts from one communication activity to another. Transitions typically involved both topic shifts and linguistic features, such as discourse markers, (e.g. well, oh, you know27) that indicate a shift between activities (e.g. ‘okay, now let's talk about…’28). Transitions between communication activities require at least tacit co‐operation between patients and physicians. Therefore, we also coded “attempted transitions.” We defined attempted transitions as instances when one person suggests a shift between communication activities but the other person keeps the discussion focused on the previous activity (Table 1).
Table 1.
Definitions of major communication activities, transitions and attempted transitions
| Diagnosis delivery: Physician telling the patient that he has cancer. |
| Risk classification: Discussion of the patient's biopsy results and the patient's personal risk classification (i.e., low versus intermediate). Risk classification typically includes discussion of Gleason score, PSA levels, and biopsy cores. |
| Options talk: Discussion of the patient's treatment options. Options talk typically includes explanation of different treatment options as well as the prognosis, logistics and side‐effects related to each option. Options talk also includes physician recommendations for or against specific treatment options. |
| Decision talk: Discussion of treatment decisions. Decision talk typically includes patients' preferences for or against specific treatment options, factors patients should consider when making decisions and the decision‐making process. (e.g., statements that the patient must make his own decision). |
| Next steps: Discussion of future actions related to prostate cancer treatment. Next steps include discussion of what the physician and patient should or will do after the visit (e.g., plans to schedule a follow‐up appointment or consultation with radiation oncology). |
| Transitions: A shift from one main communication activity to another. Transitions typically include both a topic shift and linguistic features that suggest a shift between activities. Transitions can occur during a single speaking turn or involve several speaking turns. A successful transition requires both parties to accept or go along with the shift to a new activity. |
| Attempted transitions: An instance when one person suggests or attempts a shift from one communication task to another and the other person keeps the discussion focused on the previous activity rather than going along with the suggested shift. |
Five investigators independently applied the initial coding system to two transcripts and then discussed their results to resolve disagreements. Based on this discussion, we refined the coding system to better reflect the data and reduce ambiguity. Investigators applied the revised coding system to two additional transcripts, discussed their results and made further revisions to the coding system. We repeated this process until investigators could reliably code transcripts. The 40 transcripts were then distributed among the five coders so that two coders independently coded each transcript using the final coding system. A research assistant not involved in coding reviewed the coding for each transcript and identified disagreements between coders. Coders resolved disagreements by reviewing the codebook and discussing discrepancies until they reached consensus.29 During coding we discovered that the recording stopped before the end of the visit in four visits. We kept these visits in our sample because, in each case, the recording seemed to capture nearly the entire visit.
Results
Our sample comprised 40 visits involving 40 patients and 18 physicians (Table 2). The median number of visits per physician was 2 (mean 2.2; range 1–6). Median visit length was 21 min (mean 21; range 8–37). Eight visits included a patient companion (e.g. spouse or friend).
Table 2.
Participant demographics
| Patients (n = 40) | Physiciansa (n = 15) | |
|---|---|---|
| Mean age (years) (SD) | 63.6 (5.0) | 28.8 (2.0) |
| Men (%) | 100.0 | 73.3 |
| Race (%) | ||
| White | 82.5 | 60.0 |
| Black | 15.0 | 6.7 |
| Native American | 2.5 | 0 |
| Asian | 0 | 20.0 |
| Multi‐racial | 0 | 13.3 |
| Highest education (%) | ||
| Some high school | 2.5 | |
| High school diploma or GED | 30.0 | |
| Some college (no degree) | 27.5 | |
| Associate's degree | 22.5 | |
| Bachelor's degree | 15.0 | |
| Master's degree | 2.5 | |
| Companion present (%) | 20.0 | |
Information missing for 3 of the 18 physicians.
Sequential organization of communication activities
We identified five major communication activities in our sample that usually happened in the following sequence: First, the physician told the patient that his biopsy showed cancer (‘diagnosis delivery’); second, the physician explained the biopsy results and recurrence risk (‘risk classification’); third the physician explained the treatment options in detail (‘options talk’); fourth, the patient and physician discussed the patient's treatment preference and the decision‐making process (‘decision talk’); fifth the patient and physician agreed on a plan of action (‘next steps’). Fig. 1 shows this sequence and Table 1 gives detailed definitions. We found no evidence that the sequence differed based on patients' recurrence risk or pre‐visit treatment preference. All visits in our sample included all five of these main communication activities, except for two visits in which the recording stopped before the end of the visit. The mean time per visit spent on each activity was 1 min for diagnosis delivery, 2 min for risk classification, 10 min for options talk, 6 min for decision talk and 3 min for next steps.
Figure 1.
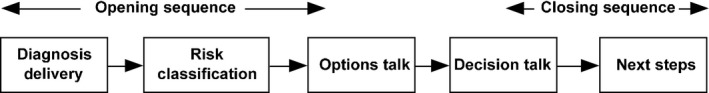
Typical organization of communication activities during visits.
Table 3 shows the prevalence of specific transitions and attempted transitions in our sample. The four transitions associated with the usual sequence (Fig. 1) were the most common transition types in our sample and comprised 72% of all coded transitions. Visit openings and closings showed the least variation across visits. Ninety percent of visits started with the same opening sequence: diagnosis delivery, then risk classification, then options talk. In addition, all visits that were completely recorded ended with the same closing sequence: decision talk, then next steps.
Table 3.
Prevalence of transitions and attempted transitions by typea
| Transition type | Number of visits | Number of codes |
|---|---|---|
| Diagnosis delivery to risk classification | 39 | 39 |
| Options talk to decision talk | 38 | 41 |
| Risk classification to options talk | 38 | 40 |
| Decision talk to next steps | 33 | 34 |
| Attempted decision talk to next steps | 14 | 19 |
| Attempted options talk to decision talk | 13 | 15 |
| Decision talk to options talk | 5 | 5 |
| Next steps to decision talk | 4 | 4 |
| Options talk to next steps | 4 | 4 |
| Options talk to risk classification | 3 | 3 |
| Risk classification to decision talk | 3 | 3 |
| Decision talk to options talk | 2 | 2 |
| Decision talk to risk classification | 2 | 2 |
| Next steps to options talk | 1 | 1 |
| Risk classification to diagnosis delivery | 1 | 1 |
| Risk classification to next steps | 1 | 1 |
| Attempted risk classification to options talk | 1 | 1 |
One visit can include multiple instances for the same transition type if, for example, participants transition back and forth several times between two communication activities.
Two types of attempted transitions – options talk to decision talk and decision talk to options talk – were each present in about one‐third of transcripts. Other types of attempted transitions and transitions that were inconsistent with the usual sequence were relatively rare. In the following sections, we discuss key findings from our analysis of patient–physician communication during transitions. Transcript excerpts are presented in Table 4 and referenced by number in the text.
Table 4.
Transcript excerpts
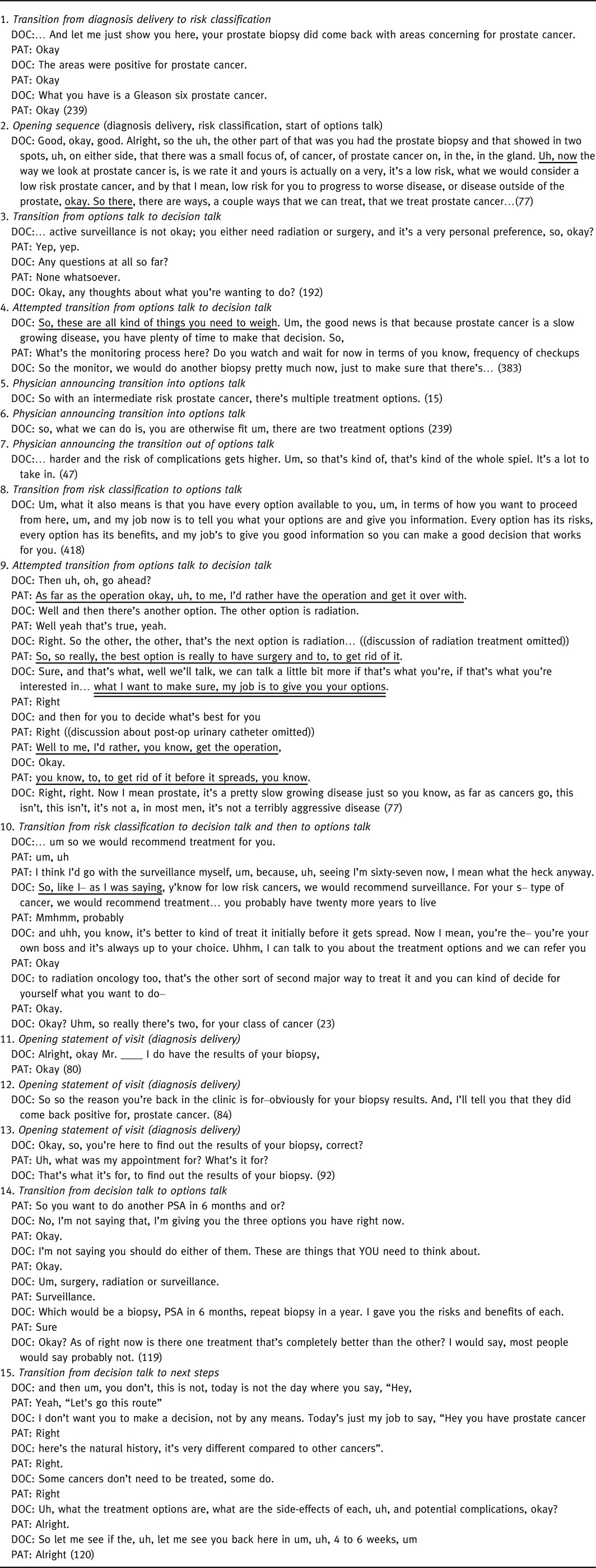
Opening sequences of visits are uniform and dominated by physicians
Activities and transitions during the opening sequence were usually brief, were similar across visits and involved minimal patient speech. Physicians initiated the majority of transitions in our sample, and patient‐initiated transitions were especially rare during the opening sequence. Patient speech during these transitions was mostly confined to backchannels (i.e. brief listener responses that indicate attention: ‘mm‐hmm,’ ‘okay’30). Physicians rarely elicited patient concerns or questions after delivering the cancer diagnosis. Excerpt 1 shows a typical transition from diagnosis delivery to risk classification. Physicians tended to accomplish these early transitions almost unilaterally, (i.e. with minimal patient involvement19) but we found no evidence that lack of patient speech was due to physicians interrupting patients. Excerpt 2 shows a physician completing the entire opening sequence during a single speaking turn (transitions are underlined). One logical consequence of physicians initiating most transitions is that the overall visit structure often emerges from physicians' priorities.
Patient speech increases notably after the opening sequence
Transitions after the opening sequence included much more patient speech; this increase was due to an increase in both physicians' eliciting patient talk and in patient questions. Physicians elicited patient questions and concerns during about one‐third of transitions from options talk to decision talk; eliciting questions was rare before this point. Excerpt 3 shows one example during a transition from options talk to decision talk.
Attempted transitions were fairly common after the opening sequence; most attempted transitions involved patient questions that delayed physicians' attempts to shift between communication activities. Eleven of the 13 attempted transitions from options talk to decision talk involved patient questions; most patients requested more information about treatment options. In excerpt 4, the physician signals that he has finished options talk (underlined), but the patient's question returns the discussion to options talk. Similarly, 10 of the 14 attempted transitions from decision talk to next steps involved patient questions.
Physicians talk about options talk
We found that physicians in our sample paid more attention to options talk than to other communication activities. During transitions into and out of options talk, physicians tended to explicitly reference discussion of treatment options as a communication activity. Physicians explicitly announced the transition into options talk in over 90% of visits using language that was very similar across visits. Excerpts 5 and 6 show announcements by two different physicians. Physicians also explicitly announced the end of options talk in about 25% of visits, as shown in excerpt 7. Several physicians described options talk as part of their professional responsibility, as shown in excerpt 8. Physicians did not explicitly reference any other communication activity in this way. We previously noted that most attempted transitions out of options talk included patient questions. Physicians almost always responded to these questions, suggesting a willingness to delay transitions to decision talk until patients' questions about treatment options had been addressed.
Atypical transitions reveal physicians' stance towards options talk
We found only two visits in which patients attempted to initiate transitions out of options talk. These atypical transitions or ‘deviant cases’23 provided insight about the role of options talk within the overall visit. In both visits, patients attempted transitions away from options talk, but physicians did not cooperate. Excerpt 9 is from one of these visits and shows how the patient attempts to transition into decision talk three times by stating a preference for surgery (underlined) before the physician has described the other options. Each time, the physician responds with pro‐forma agreement (i.e. ‘well,’ ‘sure,’ ‘right, right'31) but continues to discuss treatment options, which he identifies as his professional responsibility (double underline).
Transitions from decision talk back to options talk were also relatively rare (Table 3) and were not part of the usual sequence. These transitions also provided insight about the role of options talk. In two of these transitions, patients showed confusion about treatment options, and physicians transitioned back to options talk to address this confusion. In two other instances, patients transitioned to decision talk before the physician has a chance to start options talk. In both of these instances, the physician quickly steered the discussion back to options talk. For example, in excerpt 10, the physician transitions away from decision talk into options talk and treats the patient's statement of preference as an interruption of the opening sequence (‘So, like I— as I was saying…’). So, these ‘deviant cases’ show instances in which physicians (i) resist patient‐initiated transitions out of options talk before they have finished describing treatment options, (ii) indicate a willingness to return to options talk when patients are confused about treatment options and (iii) resist efforts to engage in decision talk prior to options talk.
Some patients do not understand the visit purpose or the decision‐making process
A few patients seemed unclear about the overall visit purpose and their role in the decision‐making process. One likely reason for patient confusion about the overall visit purpose is that physicians rarely established the visit purpose at the start of visits. Physicians almost always opened visits by telling patients that their biopsies showed cancer. Excerpt 11, in which the physician starts the visit by discussing the biopsy results but does not mention the visit purpose, is typical of most visits. When physicians did mention the visit purpose at the start of visits, they said the visit purpose was to discuss biopsy results, usually in a way that presumed this purpose was already obvious to patients (e.g. excerpt 12). Most patients gave only brief acknowledgements or backchannel responses after diagnosis delivery. Patients who gave substantive responses usually indicated agreement that the visit purpose related to biopsy results. However, two patients were confused about the visit purpose; excerpt 13 shows one of these patients. We have minimal data to evaluate whether patients were actually unclear about the overall visit purpose because most physicians did not mention the visit purpose and most patients did not give substantive responses after hearing their biopsy results. Physicians stated or implied that the visit purpose was to discuss biopsy results, but they spent much more time discussing treatment options than biopsy results. This discrepancy may have contributed to a few patients being unclear about the visit purpose.
In addition, some patients were confused about the decision‐making process. Physicians seemed to recognize this confusion; in more than 25% of visits, physicians gave patients some kind of anticipatory guidance about the decision‐making process during the transition from options talk to decision talk. Most of this advice involved telling patients that treatment decisions were not urgent or describing what patients should consider when making decisions. When physicians perceived that patients misunderstood the decision‐making process, they almost always responded by clarifying that the physician's role was to describe options and not to prescribe treatments. Excerpt 14 shows one example from a visit in which the patient repeatedly asks for treatment recommendations, and the physician repeatedly clarifies that the patient must decide.
In addition to these kinds of clarifications, some physicians referenced the decision‐making process when they described their professional responsibility related to options talk (e.g. excerpts 8 and 9). Excerpt 15, in which the physician summarizes the visit purpose before transitioning into next steps, shows the most extended example of this phenomenon. So, at least in some visits, communication during transitions suggested that either patients were confused about their role or that physicians perceived that patients were confused.
Discussion
In this study, we analysed the sequential organization of communication activities and the transitions between activities during visits dedicated to discussing diagnosis and treatment of early stage prostate cancer. We found that that communication during these visits comprised a regular sequence of five activities (Fig. 1). Most visits showed this same overall sequence, especially during the opening sequence. This overall structure differs markedly from that of routine outpatient visits in several ways. Visits in our sample rarely mentioned the visit purpose up front, whereas routine outpatient visits typically start by establishing the chief complaint. Visits in our sample also began with a short, physician‐dominated opening sequence rather than with patient‐centred activities.17, 26 Finally, visits in our sample typically ended with discussion of the decision‐making process rather than with physician‐directed treatment recommendations.
Our analysis of transitions revealed that physicians approach discussion of treatment options (options talk) rather than diagnosis delivery as the main visit purpose. The opening sequence was generally short, and physician‐initiated transitions provided minimal space for patient speech or reactions after diagnosis delivery. These findings suggest that physicians treat diagnosis delivery and risk classification as activities that are not central to the visit purpose and function primarily to set the stage for options talk.
In contrast, options talk took up a substantial proportion of most visits and was the central activity in the typical sequence (Fig. 1). Physicians frequently described options talk as both part of their professional responsibility and central to the overall visit purpose. Physicians in our sample performed considerable conversational work to inform patients about options and encourage patients to make treatment choices. Physicians showed a clear orientation to providing guidance while encouraging patients to make their own treatment decisions. This ethos likely reflects the especially complex nature of treatment decisions in prostate cancer, which involve choosing among three equally effective options. This explanation is consistent with a recent study that found 87% of men with early stage prostate cancer reported making either shared or patient‐driven (rather than physician‐driven) treatment decisions.32
Compared to physicians, patients spoke little during transitions. We found evidence that a few patients were confused about either the overall visit purpose or their role in the decision making process. This confusion was present in a minority of transcripts even though all patients in our sample received decision aids. Therefore, patient confusion is likely to be more prevalent when patients do not get decision aids. Factors that are likely contributing to patients' confusion include the unusual structure of these visits, the expectation that patients (rather than physicians) make decisions and patients' emotions and fears related to being told they have cancer.
Our study is the first to analyse the overall structure of actual visits about early stage prostate cancer and provides a foundation for research in this area. Efforts to improve communication are more likely to succeed if they are based on accurate knowledge about how patients and physicians actually communicate.33, 34 Our findings reflect patients' and physicians' stance towards communication activities (e.g. whether participants considered options talk to be complete) rather than communication content (e.g., whether physicians completely described treatment options). These findings support some broader conclusions related to patient‐centred cancer communication. In particular, the National Cancer Institute has identified six communication activities that are core components of patient‐centred communication.35, 36 Our findings relate to two of these activities: ‘recognizing and responding to emotion’ and ‘managing uncertainty.’
First, our analysis suggests that physicians may fall short when it comes to recognizing and responding to emotion during visits, especially during the opening sequence. Cancer is a frightening subject for most patients; being aware of and responsive to patient emotions is a well‐established principle of good cancer communication.37 To accomplish this component of patient‐centred communication, physicians should elicit or at least acknowledge patients' reactions immediately after telling patients they have cancer. Recognizing and addressing patients' perspectives will also likely help physicians to adjust their subsequent communication to meet patients' individual needs.
Second, physicians could better manage uncertainty by explicitly describing the main purpose of the visit (i.e. to discuss treatment options) and the decision‐making process (i.e. that physicians describe options but patients make decisions) before starting to discuss treatment options. Routinely explaining these aspects of the visit up front would alert patients as to how their current visit differs from routine outpatient visits and so would likely lead to more effective discussion of treatment options and decision making. This communication activity would serve a function analogous to agenda setting in routine outpatient visits. However, physicians must tell patients they have cancer before they can discuss treatment options and choices.
Our study has several limitations. Visits in our sample were collected at a single urology clinic, so our findings may not generalize to other settings. Our analysis also relied on transcripts from audio rather than video recordings, so we could not analyse non‐verbal communication (e.g. body language), which often serves important functions during transitions.20 However, we feel that audio recordings were adequate for this study because all visits in our sample dealt with the same clinical problem, making transitions more uniform and easier to identify across visits. Finally, analysing communication behaviours does not always provide reliable data about participants' thoughts and motives.38 This limitation is common to all discourse analysis studies, but it was mitigated in our study because physicians often talked explicitly about the communication activities they were performing.
Conflicts of interest
None.
Sources of Funding
This study was supported in part by grants from the Blue Cross Blue Shield of Michigan Foundation (1722.II; Detroit, MI) and the University of Michigan Robert Wood Johnson Foundation Health and Society Scholars program (Ann Arbor, MI) to Dr. Henry. The parent study was funded by an IIR Merit Award from the U.S. Department of Veterans Affairs (IIR 05‐283, Washington, DC) to Dr. Fagerlin.
Acknowledgements
The authors are grateful to Daniel Connochie for assistance with transcription and to Nicholas M. Moloci for assistance with data management.
References
- 1. Arora NK, Street RL Jr, Epstein RM, Butow PN. Facilitating patient‐centered cancer communication: a road map. Patient Education and Counseling, 2009; 77: 319–321. [DOI] [PubMed] [Google Scholar]
- 2. Wilt T, Shamliyan T, Taylor B et al Comparative Effectiveness of Therapies for Clinically Localized Prostate Cancer. Rockville, MD: Agency for Healthcare Research and Quality, February 2008. Report No.: 08‐EHC010‐EF. [PubMed]
- 3. Wilt TJ, Brawer MK, Jones KM et al Radical prostatectomy versus observation for localized prostate cancer. New England Journal of Medicine, 2012; 367: 203–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ilic D, Murphy K, Green S. Risk communication and prostate cancer: identifying which summary statistics are best understood by men. American Journal of Men's Health, 2012; 6: 497–504. [DOI] [PubMed] [Google Scholar]
- 5. Pieterse AH, Henselmans I, de Haes HCJM, Koning CCE, Geijsen ED, Smets EMA. Shared decision making: prostate cancer patients' appraisal of treatment alternatives and oncologists' eliciting and responding behavior, an explorative study. Patient Education and Counseling, 2011; 85: e251–e259. [DOI] [PubMed] [Google Scholar]
- 6. Hoffman RM. Improving the communication of benefits and harms of treatment strategies: decision AIDS for localized prostate cancer treatment decisions. Journal of the National Cancer Institute Monographs, 2012; 2012: 197–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Holmes‐Rovner M, Stableford S, Fagerlin A et al Evidence‐based patient choice: a prostate cancer decision aid in plain language. BMC Medical Informatics and Decision Making, 2005; 5: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Byrne JM, Long BEL. Doctors Talking to Patients. London: Her Majesty's Stationery Office, 1976. [Google Scholar]
- 9. Roter DL, Hall JA. Doctors Talking with Patients/Patients Talking with Doctors: Improving Communication in Medical Visits, 2nd edn Westport, CT: Praeger, 2006. [Google Scholar]
- 10. Mishler EG. The Discourse of Medicine: Dialectics of Medical Interviews. Norwood, NJ: Ablex Publishing Corporation, 1984. [Google Scholar]
- 11. Waitzkin H. The Politics of Medical Encounters: How Patients and Doctors Deal with Social Problems. New Haven: Yale University Press, 1991. [Google Scholar]
- 12. Frankel RM Talking in interviews: a dispreference for patient‐initiated questions in physician‐patient encounters In: Psathas G. (ed) Interaction Competence. Studies in Ethnomethodology and Conversation Analysis. Washington, DC: International Institute for Ethnomethodology and Conversation Analysis and University Press of America, 1990: 231–262. [Google Scholar]
- 13. Robinson JD. Closing medical encounters: two physician practices and their implications for the expression of patients' unstated concerns. Social Science and Medicine, 2001; 53: 639–656. [DOI] [PubMed] [Google Scholar]
- 14. Rodriguez HP, Anastario MP, Frankel RM et al Can teaching agenda‐setting skills to physicians improve clinical interaction quality? A controlled intervention BMC Medical Education, 2008; 8: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rodondi PY, Maillefer J, Suardi F, Rodondi N, Cornuz J, Vannotti M. Physician response to “by‐the‐way” syndrome in primary care. Journal of General Internal Medicine, 2009; 24: 739–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stein T, Krupat E, Frankel RM. Talking with Patients: Using the Four Habits Model. Oakland, CA: The Permanente Medical Group, 2011. [Google Scholar]
- 17. Fortin AH, Dwamena FC, Frankel RM, Smith RC Smith's Patient‐Centered Interviewing: An Evidence‐Based Method. 3rd edn New York: McGraw‐Hill Medical, 2012. [Google Scholar]
- 18. Ainsworth‐Vaughn N. Topic transitions in physician‐patient interviews: power, gender, and discourse change. Language in Society, 1992; 21: 409–426. [Google Scholar]
- 19. West C, Garcia A. Conversational shift work: a study of topical transitions between women and men. Social Problems, 1988; 35: 551–575. [Google Scholar]
- 20. Robinson JD, Stivers T. Achieving activity transitions in physician‐patient encounters from history taking to physical examination. Human Communication Research, 2001; 27: 253–298. [Google Scholar]
- 21. Heritage J. Conversation analysis and institutional talk: analyzing data In: Silverman D. (ed) Qualitative Research: Theory, Method, and Practice. London: Sage, 1997, 161–182. [Google Scholar]
- 22. United States Department of Veterans Affairs . Testing the helpfulness of two decision aids for prostate cancer. In: ClinicalTrials.gov [Internet]. Bethesda, Maryland: National Library of Medicine (US). 2000‐2013. Available from: http://clinicaltrials.gov/ct2/show/NCT00432601?term=NCT00432601&rank=1, accessed 28 September 2013.
- 23. Patton MQ Designing Qualitative Studies. Qualitative Research and Evaluation Methods. 3rd edn Thousand Oaks, CA: Sage Publications, 2002, 209–258. [Google Scholar]
- 24. NCCN Clinical Practice Guidelines in Oncology 2012 Prostate cancer: National Comprehensive Cancer Network; Available from: http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf, accessed 22 November 2012.
- 25. Hodges BD, Kuper A, Reeves S. Discourse analysis. British Medical Journal, 2008; 337: 570–572. [DOI] [PubMed] [Google Scholar]
- 26. Robinson JD. An interactional structure of medical activities during acute visits and its implications for patients' participation. Health Communication, 2003; 15: 27–57. [DOI] [PubMed] [Google Scholar]
- 27. Schiffrin D Discourse markers: language, meaning, and context In: Schiffrin D, Tannen D, Hamilton HE. (eds) The Handboook of Discourse Analysis. Blackwell Handbooks in Linguistics. Malden, Mass: Blackwell Publishing, 2003, 54–75. [Google Scholar]
- 28. Beach W Preserving and constraining options:”okays” and ‘official’ priorities in medical interviews In: Morris GH, Chenail RJ. (eds) The Talk of the Clinic. Hillsdale, NJ: Lawrence Erlbaum Associates, 1995, 259–289. [Google Scholar]
- 29. Waitzkin H. On studying the discourse of medical encounters: a critique of quantitative and qualitative methods and a proposal for reasonable compromise. Medical Care, 1990; 28: 473–488. [DOI] [PubMed] [Google Scholar]
- 30. Knapp ML, Hall JA Nonverbal Communication in Human Interaction. 7th edn Boston, MA: Wadsworth, Cengage Learning, 2009. xii, 496. [Google Scholar]
- 31. Sidnell J Conversation Analysis: An Introduction. Chichester, UK; Malden, MA: Wiley‐Blackwell, 2010. x, 283. [Google Scholar]
- 32. Song L, Chen RC, Bensen JT et al Who makes the decision regarding the treatment of clinically localized prostate cancer–the patient or physician?: results from a population‐based study. Cancer, 2013; 119: 421–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Maynard DW, Frankel RM. On diagnostic rationality: bad news, good news, and the symptom residue In: Heritage J, Maynard DW. (eds) Communication in Medical Care: Interaction Between Primary Care Physicians and Patients: New York: Cambridge University Press, 2006, 248–278. [Google Scholar]
- 34. Eggly S, Penner L, Albrecht TL et al Discussing bad news in the outpatient oncology clinic: rethinking current communication guidelines. Journal of Clinical Oncology, 2006; 24: 716–719. [DOI] [PubMed] [Google Scholar]
- 35. McCormack LA, Treiman K, Rupert D et al Measuring patient‐centered communication in cancer care: a literature review and the development of a systematic approach. Social Science and Medicine, 2011; 72: 1085–1095. [DOI] [PubMed] [Google Scholar]
- 36. Epstein R, Street RL Jr Patient‐centered communication in cancer care: Promoting healing and reducing suffering. Bethesda, MD: National Cancer Institute, 2007: NIH Publication No. 07‐6225.
- 37. Kissane DW, Bylund CL, Banerjee SC et al Communication skills training for oncology professionals. Journal of Clinical Oncology, 2012; 30: 1242–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hudak PL, Frankel RM, Braddock C III et al Do patients' communication behaviors provide insight into their preferences for participation in decision making? Medical Decision Making, 2008; 28: 385–393. [DOI] [PubMed] [Google Scholar]


