Abstract
Luminal acidity is a physiologic challenge in the foregut, and acidosis can occur throughout the gastrointestinal tract as a result of inflammation or ischemia. These conditions are surveyed by an elaborate network of acid-governed mechanisms to maintain homeostasis. Deviations from physiologic values of extracellular pH are monitored by multiple acid sensors expressed by epithelial cells and sensory neurons. Acid-sensing ion channels are activated by moderate acidification, whereas transient receptor potential ion channels of the vanilloid subtype are gated by severe acidosis. Some ionotropic purinoceptor ion channels and two-pore domain background K+ channels are also sensitive to alterations of extracellular pH.
Keywords: Acidosis, Acid-induced motor programs, Acid-sensing ion channels (ASICs), Gastric acid, Hyperalgesia, Inflammation, Ionotropic purinoceptor (P2X) ion channels, Ischemia, Mucosal protection, Pain, Transient receptor potential ion channels of the vanilloid subtype (TRPV), Two-pore domain potassium channels (KCNK)
Acidity and acidosis in the gastrointestinal tract
Acidity in the stomach and adjacent gut regions
Ever since the landmark paper “On the nature of acid and saline matters usually existing in the stomach of animals” was presented by William Prout to the Royal Society of London on December 11, 1823, has the stomach been known as a highly productive source of acid in the foregut. It is one of the most remarkable physiologic achievements that the parietal cells can secrete hydrochloric acid (HCl) to yield a proton (H+) concentration in the gastric lumen that is more than 6 orders of magnitude higher than in the interstitial space of the gastric lamina propria. Thus, the average diurnal pH in the empty human stomach is around 1.5 (25).
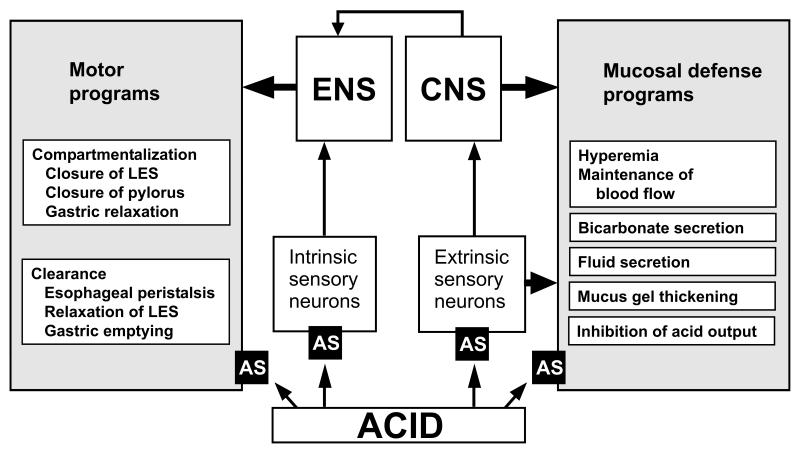
Most tissues would rapidly disintegrate if exposed to this concentration of HCl, yet gastric acid is essential for the digestive breakdown of food and elimination of ingested pathogens. The autoaggressive potential of HCl is kept in check by an elaborate network of mucosal defense mechanisms and the functional compartmentalization of the esophago-gastro-duodenal region (Figure 1). Both strategies require an acid surveillance system among which acid-sensitive afferent neurons play a particular role (10,11). If the pathophysiologic impact of gastric acid gets out of control, acid-related diseases including gastritis, gastroduodenal ulceration, dyspepsia and gastroesophageal reflux disease (GERD) may ensue.
Figure 1.
Two types of luminal acid-induced programs to ensure tissue homeostasis in the esophagus, stomach and duodenum. Either type of program is under the control of molecular acid sensors (AS) on sensory neurons. CNS, central nervous system; ENS, enteric nervous system; LES, lower esophageal sphincter.
Acidosis in the gastrointestinal tract
Importantly, acid sensors are not only relevant to control the secretion and actions of gastric acid but also to detect tissue acidosis resulting, e.g., from ischemia, inflammation, microbial activity, malignant tumor growth and gastrointestinal (GI) motor stasis (8,28). The pH profile in the GI lumen of healthy subjects shows a distinct shape (8,28), with peaks of acidity in the stomach and proximal large bowel (Table 1). While HCl and bicarbonate (HCO3−) secretion are the major determinants of luminal pH in the foregut, luminal pH in the colon depends on mucosal HCO3− and lactate production as well as on microbial transformation of carbohydrates to short chain fatty acids and formation of ammonia (28). This pH profile can be changed by surgical interventions and in inflammatory bowel disease (8,28). Thus, chronic pancreatitis and cystic fibrosis appear to decrease pH of the proximal small intestine (8), and inflammatory bowel disease has been reported to lower colonic pH values, although the pertinent data are conflicting (28).
Table 1.
Luminal pH profile along the human gastrointestinal tract
| Region | pH |
|---|---|
| Proximal esophagus | > 6.0 |
| Distal esophagus | > 5.0 |
| Stomach | 1.5 |
| Duodenum | 6.0 |
| Ileum | 7.4 |
| Caecum | 5.7 |
| Rectum | 6.7 |
GI acidosis due to splanchnic hypoperfusion can occur as a result of a variety of pathologic conditions including shock and sepsis. Taken all findings together, a fall of extracellular pH in the GI tract appears to be a surrogate marker of many pathophysiologic processes that are not limited to the adverse actions of gastric acid. Adequate acid sensing, therefore, is essential for the maintenance of homeostasis in the GI tract, whereas inappropriate acid sensing might contribute to inflammatory and ulcerative disturbances of the mucosa and to functional abdominal pain syndromes.
Acid sensing-dependent processes in the gastrointestinal tract
Feedback control of gastric acid secretion
The secretion of gastric acid at highly toxic concentrations requires a tight control of its production according to need. Acid sensing may be achieved directly through molecular acid sensors or indirectly via mediators that are formed in response to luminal acidification. The major inhibitory regulator of gastric acid secretion is an increase in intragastric acidity. A decrease of luminal pH below 3.0 has a concentration-dependent inhibitory influence on HCl and gastrin secretion, and at pH 1.0 further acid output is abolished (35). The major mediator of this feedback inhibition is somatostatin which via paracrine and endocrine pathways inhibits parietal cell function both directly and indirectly via reduction of gastrin secretion (35). It awaits to be examined in which way the somatostatin-producing endocrine D cells sense acidity in the gastric lumen. There is evidence that the activity of D cells is indirectly governed by acid-sensitive primary afferent neurons in the gastric mucosa. Luminal acidification excites their nerve terminals in the lamina propria and causes a local release of calcitonin gene-related peptide (CGRP). CGRP, in turn, stimulates D cells and inhibits acid secretion via the somatostatin pathway (10).
Esophago-gastro-duodenal mucosal function
Exposure of the esophageal, gastric and duodenal mucosa to excess acid elicits protective mechanisms including hyperemia (10). Focussing on the duodenum which is continuously exposed to gastric acid emptied from the stomach, recent studies have revealed that maintenance of mucosal integrity is critically dependent on acid sensing and appropriate initiation of protective measures. Unlike the gastric mucosa, the duodenal epithelium displays high permeability for water and ions. As a consequence, exposure of the duodenal mucosa to excess acid stimulates several defense mechanisms (Figure 1) including an increase in mucus gel thickness, HCO3− secretion and mucosal blood flow (26). In the stomach, fluid secretion is also enhanced (14). The mucosal acid sensors that alarm these epithelial and subepithelial defenses are not fully known. Besides the generation of mediators such as prostaglandins which augment HCO3− secretion, the epithelial cells are capable of directly responding to a drop of luminal pH (26).
One possibility of acid sensing is reflected by the ability of luminal acidification to decrease the intracellular pH (pHi) of the duodenal epithelium, possibly via inhibition of apical sodium-proton exchangers of type 2 or 3 (NHE2 or NHE3) (26). This change is followed by active uptake of HCO3− from the blood via a Na+/ HCO3− cotransporter and formation of HCO3− from ambient CO2 with the help of carbonic anhydrase. HCO3− is then exported via apical anion channels such as cystic fibrosis transmembrane conductance regulator (26).
There is emerging evidence, however, that the epithelial cells sense pCO2 rather than pH (1,2,26). This possibility accounts for the fact that active epithelial cells are normally not exposed to luminal acid because pH at the epithelial surface is kept at a neutral value owing to the pH gradient within the mucus gel layer adherent to the gastroduodenal mucosa (2). Excess luminal H+ combines with secreted HCO3− to yield CO2 and H2O. CO2 is much more membrane-permeant than H+ and can easily traverse the apical plasma membrane. Subsequently, CO2 is hydrated with the help of carbonic anhydrase to carbonic acid which dissociates into HCO3− and H+. HCO3−, in turn, exits through the plasma membrane via an anion exchange process (1,2,26).
Experimental evidence indicates that the transient receptor potential ion channel of vanilloid type 1 (TRPV1) plays a role as acid sensor for signaling mucosal hyperemia in the duodenum in response to luminal acidification. Since TRPV1, however, is located on sensory nerve terminals in the lamina propria behind the epithelium, the mucosal acid signal must be transduced across the epithelium. This transepithelial pathway likewise involves diffusion of CO2 into the epithelial cells, hydration to H+ and HCO3−, intracellular acidification and exit of H+ via the basolateral sodium-proton exchanger of type 1 (NHE1) (1,26). As a result, interstitial pH is lowered, which activates TRPV1-bearing sensory nerve terminals that release the potent vasodilator peptide CGRP.
Esophago-gastro-duodenal motility
The aggressive potential of gastric acid is kept in check not only by mucosal defense mechanisms but also by compartmentalization of the esophago-gastro-duodenal region (Figure 1). The latter strategy is to restrict the presence of high acid concentrations to the stomach, the mucosa of which is most resistant to intrusion by H+, and to precisely control H+ passage from the stomach to the duodenum through coordinated activity of the lower esophageal (LES) and pyloric sphincter. Both sphincters are under the control of neural reflexes involving acid-sensitive neurons which adjust the tone of the LES and pyloric sphincter to balance the levels of acid present in the esophagus, stomach and duodenum with the mucosal defense mechanisms in these compartments (11,14).
The pyloric sphincter controls gastric emptying and ensures that the acidified gastric contents are delivered to the duodenum at a rate that enables this most proximal region of the small intestine to cope with the imposed acid load. If too much gastric acid enters the duodenum, a duodeno-pyloro-gastric reflex is elicited, which leads to contraction of the pylorus and inhibition of gastric motor activity, effects which halt further gastric emptying. These coordinated motor reactions are governed by acid-sensitive neurons which, in turn, activate multiple neural circuits involving enteric, sympathetic and vagal nerve pathways (11,14).
The LES ensures that gastric acid does not reflux into the esophagus and cause damage of the esophageal mucosa. Contraction of the LES, on the one hand, prevents reflux of gastric acid whereas relaxation of the LES, on the other hand, is necessary to allow esophageal clearance. There is evidence that the activity of the LES is determined by two different motor programs initiated by the presence of acid in the esophagus (11). Acidification of the distal esophagus, mimicking reflux of gastric acid, causes contraction of the LES through an enteric neural reflex and thus prevents further acid reflux. In contrast, administration of acid into the more proximal esophagus triggers a motor program that facilitates the clearance of the esophagus. Thus, acid promotes esophageal peristalsis, accelerates its transport towards the stomach and leads to relaxation of the LES (11). Acid-induced esophagitis enhances this inhibitory pathway to the LES, and it is tempting to hypothesize that hypersensitivity of this inhibitory LES reflex mechanism is a pathogenetic factor in the impaired LES function associated with GERD (11).
Acid-induced pain and hyperalgesia
Investigations in somatic tissues have established that acidosis is extremely painful and, in addition, sensitizes afferent nerve fibers to mechanical stimulation (20). Similar observations have been made in the GI tract where acid causes sensitization of mechanosensitive afferent pathways from the esophagus and stomach (6,24). Acidosis is thought to be an important factor in inflammatory hyperalgesia (20), and exposure of the mouse colon to an acidic mixture of inflammatory mediators likewise enhances afferent nerve responses to stretch (17). While acid is known to contribute to the pain associated with GERD, dyspepsia and peptic ulcer, it is less well understood whether acid also plays a role in the pain associated with functional bowel disorders such as non-cardiac chest pain, functional dyspepsia, irritable bowel syndrome as well as in functional abdominal pain syndrome. Recent experimental studies have shed some light on the identity of the molecular acid sensors and neural pathways that underlie acid-evoked nociception particularly in the rodent foregut.
These studies indicate that HCl is a noxious stimulus that following penetration through the mucosal barrier contributes to pain arising from the esophagus, stomach and upper small intestine. Intramucosal acidosis can be induced by exposure of the rat or mouse gastric lumen to supraphysiologic HCl concentrations that create a transmucosal H+ gradient high enough to drive H+ into the lamina propria. Accordingly, intragastric administration of HCl at concentrations of 0.15 - 0.5 M to conscious rats elicits a visceromotor response indicative of pain (22) and causes many neurons in the nucleus of the solitary tract in the rat brainstem to express c-Fos, a marker of neuronal excitation (34). The gastric HCl-evoked visceromotor reaction and medullary c-Fos response are suppressed by vagotomy, but not transection of the sympathetic nerve supply to the stomach, which indicates that gastric HCl-evoked nociception depends critically on the integrity of the vagal afferent innervation (22,34).
Experimentally induced gastritis or gastric ulceration enhance the visceromotor response to intragastric administration of excess acid and gastric distension (22,38). Further analysis has shown that gastric ulceration increases the pH sensitivity and alters the kinetics of acid-induced currents in vagal and spinal afferent neurons innervating the stomach (38). These observations indicate that inflammation and injury of the rat gastric mucosa enhance the signaling and perception of acid-induced pain.
Clinically, it is well established that ischemia can be painful, and this is also true for colonic ischemia and ischemic colitis which are typically associated with abdominal pain (36). Transient clamping of mesenteric blood vessels in the anesthetized rat likewise gives rise to pseudoaffective blood pressure reactions indicative of pain (16). In this context it may be reasoned that pain due to extensive distension of hollow viscera may in part be due to ischemia. Transient distension of the rat stomach by intraluminal pressures in excess of 30 mm Hg triggers pseudoaffective pain responses in a pressure-dependent manner (22). The blood supply of the distended segment will be gradually interrupted once the intraluminal pressure becomes equal to the blood pressure in the blood vessels supplying the distended segment. Indirect support for a role of ischemia-induced acidosis in distension-evoked pain has come from the findings that genetic knockout of certain molecular acid sensors ameliorates mechanical nociception in the GI tract (17,30).
Molecular acid sensors
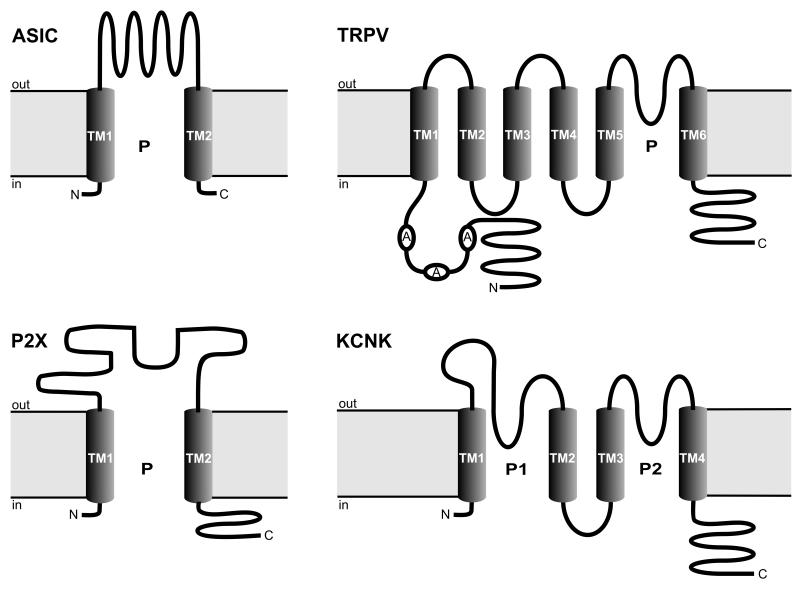
It has long been known that sensory neurons respond to acidification of their environment, and analysis of the acid-induced currents has provided an early hint at the existence of specific H+ receptors (20). Acid excites sensory neurons projecting to the GI tract, most probably by a direct action on the neurons (38), although an indirect action via neuroactive factors released by H+ in the tissue has not been ruled out. The former possibility is supported by the discovery that primary afferent neurons originating from the dorsal root (DRG; spinal afferents) and nodose ganglia (vagal afferents) express cation channels that can operate as molecular acid sensors (Figure 2). Apart from these extrinsic sensory neurons, there are also intrinsic primary afferent neurons that originate in the enteric nervous system and supply enteric nerve circuits with the information necessary for the physiologic control of digestion. Although intrinsic primary afferent neurons are sensitive to acidosis (3), the molecular acid sensors on enteric neurons have been much less studied than those expressed by extrinsic primary afferent neurons.
Figure 2.
Membrane topology of four classes of acid-sensitive ion channel subunits relevant to acid sensing in the GI tract: ASIC (acid-sensing ion channel), TRPV (transient receptor potential ion channel of the vanilloid subtype), P2X (ionotropic purinoceptor), and KCNK (two pore domain potassium channel). A, ankyrin; C, C-terminal; N, N-terminal; P, pore; TM, transmembrane domain.
From the pertinent studies it has become clear that no single molecular probe alone accounts for the acid sensitivity of afferent neurons. There is in fact a redundancy of molecular acid sensors, which signifies that homeostasis in the face of acidosis is physiologically so important that multiple mechanisms of acid sensing have evolved. Some of the acid-sensitive ion channels are upregulated in GI inflammation and hyperalgesia (12,13,23), which implies that neural acid sensors could be targets for novel therapies of chronic abdominal pain.
Acid-sensing ion channels (ASICs)
The ASICs belong to the voltage-insensitive, amiloride-sensitive epithelial Na+ channel/degenerin family of cation channels (12,19,21). The H+-gated members of this family are encoded by three different genes, ASIC1, ASIC2 and ASIC3, with ASIC1 and ASIC2 each having alternative splice variants termed ASIC1a, ASIC1b, ASIC2a and ASIC2b. Typical of the membrane topology of ASICs is the presence of two transmembrane domains and a large extracellular loop (Figure 2). Functional channels are made up of different ASIC subunits which form homo- or heteromultimeric channels that differ in their pH sensitivity and pharmacologic properties (21). ASIC3 is the subunit that displays the highest acid sensitivity and, when activated, generates a biphasic current that consists of a fast inactivating and a sustained component (21). ASIC2b which is inactive as a homomultimer forms functional heteromultimers with other ASIC subunits, particularly ASIC3, and the H+-gated current in DRG neurons most closely resembles that generated by activation of ASIC2b/ASIC3 heteromultimers (21).
While ASIC1 and ASIC2 are widely distributed in the nervous system, ASIC3 (previously termed DRASIC for dorsal root ASIC) is restricted to primary afferent neurons. Most ASIC subunits have been localized to both nodose ganglion and DRG neurons of the rat and mouse, although to different degrees (12,21,29,30,33,38). Retrograde tracing has revealed that 75 % of the nodose ganglion neurons and 82 % of the DRG neurons projecting to the rat stomach express ASIC3 (33).
The role of ASICs in acid sensing within the GI tract has not yet been extensively studied, with the exception of one study in the mouse stomach. Thus, the afferent input from the acid-threatened stomach to the brainstem, as visualized by c-Fos expression in the nucleus of the solitary tract, has been found unaltered in ASIC3 knockout mice, but significantly enhanced in ASIC2 knockout mice (15). It would appear, therefore, that ASIC3 does not contribute to the acid sensing of vagal afferent neurons in the normal stomach, probably because of a redundancy in the molecular acid sensors expressed by these neurons. ASIC3, however, plays a major role in the inflammatory hyperresponsiveness of the vagal afferent – brainstem axis, since the effect of gastritis to enhance the gastric acid-evoked expression of c-Fos in the brainstem is abolished in ASIC3 knockout mice but fully preserved in ASIC2 knockout mice (15). Thus, while ASIC3 is relevant to gastritis-evoked acid hypersensitivity, ASIC2 appears to dampen acid-evoked afferent input from the stomach to the brainstem.
The implication of ASIC3 in inflammatory hyperresponsiveness to acid challenge of the mouse stomach could be taken to hypothesize that the expression and/or function of ASICs is altered in inflammation and hyperalgesia. This is true for experimental ulceration in the rat stomach, which leads to changes in the kinetics of ASIC-like currents in both DRG and nodose ganglion neurons (38). Importantly, the expression of ASIC3, but not ASIC1 and ASIC2, is upregulated in the colonic mucosa of patients with inflammatory bowel disease (12). Antiinflammatory drugs such as aspirin, diclofenac and flurbiprofen counteract the upregulation of ASICs caused by experimental inflammation and inhibit ASIC currents in afferent neurons (12,21). The elucidation of ASIC function in health and disease will greatly depend on the availability of selective ASIC inhibitors which, in addition, could turn out to be novel therapeutics in pathologic conditions driven by ASIC overexpression or hyperactivity.
It is currently emerging that ASICs also play a role in GI mechanoreceptor function, because mechanotransduction in GI afferent neurons is differentially altered in ASIC1, ASIC2 and ASIC3 knockout mice. Deletion of ASIC1 increases mechanosensitivity in gastroesophageal vagal and colonic spinal afferent neurons, while ASIC2 knockout has variable effects on the different classes of GI mechanoreceptors, and ASIC3 deletion invariably reduces mechanosensitivity (17,29,30). In view of these reports it is tempting to speculate that subcellular acidosis is a link in the mechanotransduction process. A further issue that may be relevant to the outcome of in vivo studies with ASIC knockout mice is the possibility that mechanical stimulation (stretch, distension) induces ischemia and that ischemia-induced acidosis is a factor in the mechanotransduction process. This argument finds support in the experimental findings that lactate which is generated during ischemia sensitizes ASICs to acid and that ASIC3 contributes to ischemic heart and muscle pain (12,21).
Transient receptor potential ion channels of the vanilloid subtype (TRPVs)
TRP channels have evolved as an ancient sensory apparatus of the cell, responding to temperature, touch, sound, osmolarity, pH and various chemical messengers (5). Among the TRP channels it is particularly TRPV1, also known as the “capsaicin receptor”, and TRPV4 that respond to acidosis (12,13). Structurally they are typified by three ankyrin repeats in the N-terminus, six transmembrane domains and an extracellular re-entrant pore loop between transmembrane domain 5 and 6 (Figure 2). Like other TRP channels, functional TRPV channels are thought to be homo/hetero-tetramers that operate as non-selective cation channels with high permeability for Ca2+ (5).
Unlike ASIC3 which responds to mild acidosis, TRPV1 and TRPV4 are activated only if the extracellular pH is reduced to values below 6, in which case a sustained channel current is generated (4,12,13). Apart from H+, noxious heat, vanilloids such as capsaicin and resiniferatoxin, and some arachidonic acid-derived lipid mediators can also gate TRPV1 (4,12,13). Importantly, mild acidosis (pH 7-6) is able to sensitize TRPV1 to other stimuli such as capsaicin and heat and to lower its temperature threshold such that the channel becomes active at normal body temperature (39). Whereas H+ targets an extracellular domain of TRPV1, the vanilloid and arachidonic acid-derived agonists bind to an intracellular site of the channel (4,12,13).
TRPV1-positive nerve fibers occur in mucosa, musculature and enteric nerve plexuses of the rat, guinea-pig and mouse gut. Since enteric neurons usually do not stain for TRPV1, it follows that the TRPV1-positive nerve fibers in the GI tract represent processes of spinal afferents and, in the stomach, of some vagal afferents (13,33). Further analysis has revealed that the majority of nodose ganglion neurons projecting to the stomach and of DRG neurons projecting to the gut of rats express TRPV1 (13,33). It remains to be elucidated whether the TRPV1-like immunoreactivity which some investigators have seen in guinea-pig, porcine and human enteric neurons and rat gastric epithelial cells (13) is authentic TRPV1 or represents a nonfunctional protein such as TRPV1-β derived from alternative splicing of the trpv1 gene (40).
There is increasing evidence that TRPV1 and, to a much lesser extent, TRPV4 are acid sensors relevant to GI homeostasis and pain, although further work in this respect is needed. Whole-cell voltage-clamp recordings from DRG and nodose ganglion neurons innervating the rat stomach have shown that acidosis induces currents that can to a variable degree be attributed to the gating of ASICs and TRPV1 (38). The pH sensitivity and other parameters of these currents are distinctly altered after experimental induction of gastric ulcers (38). Genetic deletion of TRPV1 reduces the responsiveness of jejunal afferent neurons to acid and distension, similar effects being seen with the TRPV1 blocker capsazepine (32). The mechanosensitivity of muscular/mucosal afferents from the mouse colon is likewise reduced in TRPV1 knockout mice (17), and pharmacologic blockade of TRPV1 attenuates the visceromotor pain response to intraperitoneal administration of acetic acid (13).
TRPV1-expressing spinal afferent neurons play an important role in the rise of mucosal blood flow that occurs in response to acid backdiffusion in the rat stomach and duodenum (10). TRPV1 appears to be involved in the duodenal hyperemia since it is attenuated by the TRPV1 blocker capsazepine, whereas the gastric hyperemia is left unaltered by capsazepine (1,13). In contrast, the acid-evoked secretion of duodenal HCO3− is left unchanged by capsazepine (18), which is consistent with the concept that acid-stimulated production of HCO3− takes place within the epithelial cells (26).
Further studies indicate that TRPV1 contributes to the hypersensitivity of DRG neurons caused by administration of inflammatory mediators to the mouse colon. Thus, the 5-hydroxytryptamine (5-HT)-induced sensitization of these neurons to acid, capsaicin and heat is absent in TRPV1 knockout mice (37). The effect of 5-HT to sensitize colonic DRG neurons is mediated by metabotropic 5-HT2 and 5-HT4 receptors which appear to enhance TRPV1 activity by downstream phosphorylation pathways (37). Furthermore, TRPV1 contributes to the effect of an acidic inflammatory soup containing 5-HT, histamine, bradykinin and prostaglandin E2 to sensitize muscular afferent nerve fibers in the mouse colon to stretch, because this process is absent in TRPV1 knockout mice (17).
Taken together, these findings point to a role of TRPV1 in afferent neuron hypersensitivity, which is in keeping with the ability of many proalgesic mediators to enhance TRPV1 activity (4,13). This conjecture is further supported by the findings that TRPV1-like immunoreactivity is upregulated in esophagitis, painful inflammatory bowel disease as well as rectal hypersensitivity and fecal urgency (12,13,23). As a consequence, blockade of TRPV1 activity is currently explored as a strategy to treat abdominal hyperalgesia, and a large variety of TRPV1 blockers has been developed (13). However, a causal involvement of TRPV1 in abdominal hyperalgesia has not yet been proved nor is it known whether acidosis sensed by TRPV1 is a relevant factor in this instance.
Ionotropic purinoceptor ion channels
P2X purinoceptors are ligand-gated membrane cation channels that open when extracellular ATP is bound. They are assembled as homo- or heteromultimers of various subunits, seven of which (P2X1 - P2X7) have been identified at the gene and protein level (7,27). Structurally, all P2X subunits are characterized by a very long extracellular polypeptide loop between two transmembrane domains (Figure 2). The P2X receptors on nodose ganglion and DRG neurons supplying the gut comprise homomultimeric P2X2 and P2X3 as well as heteromultimeric P2X2/3 receptors (7). Since the time course and kinetics of the ATP-gated channel currents differ fundamentally between the various homo- and heteromultimeric P2X receptors, the P2X-mediated currents vary with the P2X subunit distribution in spinal and vagal sensory neurons.
The activity of most P2X subunits is modulated by alterations of the extracellular pH (12). While the potency of ATP to gate homomultimeric P2X1, P2X3, P2X4, P2X5 and P2X7 receptors is reduced by mild acidification, homomultimeric P2X2 receptors are sensitized to ATP (7,12,27). Since only P2X2 homomultimers and heteromultimers involving P2X2 (P2X1/2, P2X2/3 and P2X2/6) are sensitized by acid, it is primarily P2X2-containing purinoceptors that can function as indirect acid sensors in the presence of ATP (12). This scenario may be of pathophysiologic significance since ATP is liberated from a number of cellular sources in the gut in response to both physiologic and pathologic stimuli. Whether P2X receptors play a role in GI pain has not yet been ascertained, although ATP can excite vagal and mesenteric afferents and inflammatory bowel disease is associated with an increase in the number of P2X3 receptors on nerve fibers and myenteric neurons in the colon (7,12). Pharmacologic blockade of P2X3 and P2X2/3 receptors has been reported to suppress the nociceptive behavior provoked by interaperitoneal injection of acetic acid in mice (12).
Acid-sensitive two-pore domain potassium channels
Two-pore (or tandem-pore) domain potassium channels (KCNK) possess four transmembrane segments, two pore-forming loops and a large extracellular linker region between transmembrane domain 1 and the first pore-forming loop (Figure 2) (9,12,31). Acid modulates the activity of several KCNK family members including TWIK (tandem of pore domains in weak inward rectifier K+ channel), TREK (TWIK-related K+ channel), TASK (TWIK-related acid-sensitive K+ channel), TALK (TWIK-related alkaline pH-activated K+ channel) and TRAAK (TWIK-related arachidonic acid-stimulated K+ channel). All KCNK channels seem to be made up as dimers, primarily homodimers, although the formation of functional heterodimers (such as TASK-1/TASK-3) has also been reported (9,12,31). Many KCNK channels are thought to be background channels that are independent of membrane voltage, constitutively active and non-inactivating. The resulting ‘leak’ currents play a role in setting the resting membrane potential as well as membrane input resistance and, consequently, the excitability of neurons (9,12,31).
TASK channels are extremely sensitive to variations in the extracellular pH in a narrow physiologic range. The channels are blocked by very small increases in the extracellular concentration of H+ (9,12,31). Although TASK inhibition will not per se result in nerve traffic, it is likely to facilitate nerve activity evoked by other stimuli and hence indirectly encode the presence of acid. Other KCNK members such as TWIK-1, TWIK-2, TREK-1, TREK-2 and TRAAK respond to changes in intracellular pH (12,31). Although any functional implication of KCNK channels in the neural acid surveillance of the GI tract awaits to be proven, various levels of TASK-1, TASK-2, TASK-3, TWIK-1, TWIK-2, TREK-1, TREK-2 and TRAAK mRNA and protein have been localized to DRG neurons and the gut (12).
Conclusions
Acid sensing is of paramount importance to GI homeostasis, because there are huge variations in the intraluminal pH along the alimentary canal and the survival of epithelial cells requires maintenance of intracellular pH in a narrow physiologic range. This situation is met by an elaborate network of mechanisms controlling extra- and intracellular pH, in which a redundant array of molecular acid sensors plays a critical role. In the foregut, acid detectors on epithelial cells and sensory neurons govern mucosal defense and motor programs according to the intraluminal and interstitial pH. If there is any impending danger to tissue integrity, they signal for measures that seek to minimize any injury excess acid may cause. Throughout the GI tract acidosis may occur as a result of inflammation, ischemia, overdistension of the GI wall, malignant tumor growth or disturbances in the microbial flora.
To cope with these challenges, there is a multitude of molecular acid sensors that survey a wide pH range from acidic to alkaline environments. While ASICs and acid-sensitive TRP channels are directly gated by deviations from the physiologic pH in the extracellular space, pH-dependent alterations of P2X purinoceptor and KCNK channel activity modulate cell excitability, sensitivity and function. Nearly all of these acid sensors occur in primary sensory neurons supplying the gut, and there is good reason to hypothesize that they are relevant to GI function in health and disease.
Some acid sensors behave as polymodal nociceptors that are able to detect sensory modalities other than acidosis. Particularly worth noting is the property of ASICs and TRPV1 to play a role in mechanoreception, which raises the question whether subcellular acidosis plays a role in mechanotransduction. The finding that TRPV1, ASIC3 and P2X3 are upregulated in GI inflammation and hypersensitivity suggests that aberrant function of molecular acid sensors may contribute to abdominal hyperalgesia and pain. While this conjecture identifies molecular acid sensors as emerging drug targets for the management of functional bowel disorders, it must not be neglected that interference with the function of molecular acid sensors may have a deleterious impact on GI acid homeostasis.
Acknowledgements
Work in the author’s laboratory is supported by the Austrian Scientific Research Funds (FWF grant L25-B05) and the Zukunftsfonds Steiermark (grant 262). Evelin Painsipp’s artistry in drawing the figures is greatly appreciated.
References
- 1.Akiba Y, Ghayouri S, Takeuchi T, Mizumori M, Guth PH, Engel E, Swenson ER, Kaunitz JD. Carbonic anhydrases and mucosal vanilloid receptors help mediate the hyperemic response to luminal CO2 in rat duodenum. Gastroenterology. 2006;131:142–152. doi: 10.1053/j.gastro.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 2.Allen A, Flemström G. Gastroduodenal mucus bicarbonate barrier: protection against acid and pepsin. Am J Physiol Cell Physiol. 2005;288:C1–C19. doi: 10.1152/ajpcell.00102.2004. [DOI] [PubMed] [Google Scholar]
- 3.Bertrand PP, Kunze WA, Bornstein JC, Furness JB, Smith ML. Analysis of the responses of myenteric neurons in the small intestine to chemical stimulation of the mucosa. Am J Physiol Gastrointest Liver Physiol. 1997;273:G422–G435. doi: 10.1152/ajpgi.1997.273.2.G422. [DOI] [PubMed] [Google Scholar]
- 4.Caterina MJ, Julius D. The vanilloid receptor: a molecular gateway to the pain pathway. Annu Rev Neurosci. 2001;24:487–517. doi: 10.1146/annurev.neuro.24.1.487. [DOI] [PubMed] [Google Scholar]
- 5.Clapham DE. TRP channels as cellular sensors. Nature. 2003;426:517–524. doi: 10.1038/nature02196. [DOI] [PubMed] [Google Scholar]
- 6.Coffin B, Chollet R, Flourie B, Lemann M, Franchisseur C, Rambaud JC, Jian R. Intraluminal modulation of gastric sensitivity to distension: effects of hydrochloric acid and meal. Am J Physiol Gastrointest Liver Physiol. 2001;280:G904–G909. doi: 10.1152/ajpgi.2001.280.5.G904. [DOI] [PubMed] [Google Scholar]
- 7.Dunn PM, Zhong Y, Burnstock G. P2X receptors in peripheral neurons. Prog Neurobiol. 2001;65:107–134. doi: 10.1016/s0301-0082(01)00005-3. [DOI] [PubMed] [Google Scholar]
- 8.Fallingborg J. Intraluminal pH of the human gastrointestinal tract. Dan Med Bull. 1999;46:183–196. [PubMed] [Google Scholar]
- 9.Goldstein SA, Bockenhauer D, O’Kelly I, Zilberberg N. Potassium leak channels and the KCNK family of two-P-domain subunits. Nat Rev Neurosci. 2001;2:175–184. doi: 10.1038/35058574. [DOI] [PubMed] [Google Scholar]
- 10.Holzer P. Neural emergency system in the stomach. Gastroenterology. 1998;114:823–839. doi: 10.1016/s0016-5085(98)70597-9. [DOI] [PubMed] [Google Scholar]
- 11.Holzer P. Role of sensory neurons in mucosal protection from acid-induced lesions in the foregut. In: Dal Negro RW, Geppetti P, Morice AH, editors. Experimental and Clinical Pharmacology of Gastroesophageal Reflux-Induced Asthma. Pacini; Pisa: 2002. pp. 25–33. [Google Scholar]
- 12.Holzer P. Acid-sensitive ion channels in gastrointestinal function. Curr Opin Pharmacol. 2003;3:618–625. doi: 10.1016/j.coph.2003.06.008. [DOI] [PubMed] [Google Scholar]
- 13.Holzer P. TRPV1 and the gut: from a tasty receptor for a painful vanilloid to a key player in hyperalgesia. Eur J Pharmacol. 2004;500:231–241. doi: 10.1016/j.ejphar.2004.07.028. [DOI] [PubMed] [Google Scholar]
- 14.Holzer P, Painsipp E, Jocic M, Heinemann A. Acid challenge delays gastric pressure adaptation, blocks gastric emptying and stimulates gastric fluid secretion in the rat. Neurogastroenterol Motil. 2003;15:45–55. doi: 10.1046/j.1365-2982.2003.00382.x. [DOI] [PubMed] [Google Scholar]
- 15.Holzer P, Wultsch T, Painsipp E, Shahbazian A, Waldmann R. Involvement of the acid-sensing ion channel ASIC3, but not ASIC2, in acid hypersensitivity associated with gastritis in mice. Gastroenterology. 2006;130(Suppl 2):A-250. [Google Scholar]
- 16.Holzer-Petsche U, Brodacz B. Traction on the mesentery as a model of visceral nociception. Pain. 1999;80:319–328. doi: 10.1016/s0304-3959(98)00233-4. [DOI] [PubMed] [Google Scholar]
- 17.Jones RCW, Xu L, Gebhart GF. The mechanosensitivity of mouse colon afferent fibers and their sensitization by inflammatory mediators require transient receptor potential vanilloid 1 and acid-sensing ion channel 3. J Neurosci. 2005;25:10981–10989. doi: 10.1523/JNEUROSCI.0703-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kagawa S, Aoi M, Kubo Y, Kotani T, Takeuchi K. Stimulation by capsaicin of duodenal HCO3− secretion via afferent neurons and vanilloid receptors in rats: comparison with acid-induced HCO3− response. Dig Dis Sci. 2003;48:1850–1856. doi: 10.1023/a:1025480003388. [DOI] [PubMed] [Google Scholar]
- 19.Kellenberger S, Schild L. Epithelial sodium channel/degenerin family of ion channels: a variety of functions for a shared structure. Physiol Rev. 2002;82:735–767. doi: 10.1152/physrev.00007.2002. [DOI] [PubMed] [Google Scholar]
- 20.Kress M, Reeh PW. Molecular physiology of proton transduction in nociceptors. Curr Opin Pharmacol. 2001;1:45–51. doi: 10.1016/s1471-4892(01)00014-5. [DOI] [PubMed] [Google Scholar]
- 21.Kress M, Waldmann R. Acid sensing ionic channels. Curr Top Membranes. 2006;57:241–276. [Google Scholar]
- 22.Lamb K, Kang YM, Gebhart GF, Bielefeldt K. Gastric inflammation triggers hypersensitivity to acid in awake rats. Gastroenterology. 2003;125:1410–1418. doi: 10.1016/j.gastro.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 23.Matthews PJ, Aziz Q, Facer P, Davis JB, Thompson DG, Anand P. Increased capsaicin receptor TRPV1 nerve fibres in the inflamed human oesophagus. Eur J Gastroenterol Hepatol. 2004;16:897–902. doi: 10.1097/00042737-200409000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Medda BK, Sengupta JN, Lang IM, Shaker R. Response properties of the brainstem neurons of the cat following intra-esophageal acid-pepsin infusion. Neuroscience. 2005;135:1285–1294. doi: 10.1016/j.neuroscience.2005.07.016. [DOI] [PubMed] [Google Scholar]
- 25.Modlin IM, Sachs G. Biology and Treatment. Schnetztor-Verlag; Konstanz: 1998. Acid Related Diseases. [Google Scholar]
- 26.Montrose MH, Akiba Y, Takeuchi K, Kaunitz JD. Gastroduodenal mucosal defense. In: Johnson LR, editor. Physiology of the Gastrointestinal Tract. Fourth Edition Academic Press; San Diego: 2006. pp. 1259–1291. [Google Scholar]
- 27.North RA. Molecular physiology of P2X receptors. Physiol Rev. 2002;82:1013–1067. doi: 10.1152/physrev.00015.2002. [DOI] [PubMed] [Google Scholar]
- 28.Nugent SG, Kumar D, Rampton DS, Evans DF. Intestinal luminal pH in inflammatory bowel disease: possible determinants and implications for therapy with aminosalicylates and other drugs. Gut. 2001;48:571–577. doi: 10.1136/gut.48.4.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Page AJ, Brierley SM, Martin CM, Martinez-Salgado C, Wemmie JA, Brennan TJ, Symonds E, Omari T, Lewin GR, Welsh MJ, Blackshaw LA. The ion channel ASIC1 contributes to visceral but not cutaneous mechanoreceptor function. Gastroenterology. 2004;127:1739–1747. doi: 10.1053/j.gastro.2004.08.061. [DOI] [PubMed] [Google Scholar]
- 30.Page AJ, Brierley SM, Martin CM, Price MP, Symonds E, Butler R, Wemmie JA, Blackshaw LA. Different contributions of ASIC channels 1a, 2, and 3 in gastrointestinal mechanosensory function. Gut. 2005;54:1408–1415. doi: 10.1136/gut.2005.071084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patel AJ, Honoré E. Properties and modulation of mammalian 2P domain K+ channels. Trends Neurosci. 2001;24:339–346. doi: 10.1016/s0166-2236(00)01810-5. [DOI] [PubMed] [Google Scholar]
- 32.Rong W, Hillsley K, Davis JB, Hicks G, Winchester WJ, Grundy D. Jejunal afferent nerve sensitivity in wild-type and TRPV1 knockout mice. J Physiol. 2004;560:867–881. doi: 10.1113/jphysiol.2004.071746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schicho R, Florian W, Liebmann I, Holzer P, Lippe IT. Increased expression of TRPV1 receptor in dorsal root ganglia by acid insult of the rat gastric mucosa. Eur J Neurosci. 2004;19:1811–1818. doi: 10.1111/j.1460-9568.2004.03290.x. [DOI] [PubMed] [Google Scholar]
- 34.Schuligoi R, Jocic M, Heinemann A, Schöninkle E, Pabst MA, Holzer P. Gastric acid-evoked c-fos messenger RNA expression in rat brainstem is signaled by capsaicin-resistant vagal afferents. Gastroenterology. 1998;115:649–660. doi: 10.1016/s0016-5085(98)70144-1. [DOI] [PubMed] [Google Scholar]
- 35.Shulkes A, Baldwin GS, Giraud AS. Regulation of gastric acid secretion. In: Johnson LR, editor. Physiology of the Gastrointestinal Tract. Fourth Edition Academic Press; San Diego: 2006. pp. 1223–1258. [Google Scholar]
- 36.Sreenarasimhaiah J. Chronic mesenteric ischemia. Best Pract Res Clin Gastroenterol. 2005;19:283–295. doi: 10.1016/j.bpg.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 37.Sugiura T, Bielefeldt K, Gebhart GF. TRPV1 function in mouse colon sensory neurons is enhanced by metabotropic 5-hydroxytryptamine receptor activation. J Neurosci. 2004;24:9521–9530. doi: 10.1523/JNEUROSCI.2639-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sugiura T, Dang K, Lamb K, Bielefeldt K, Gebhart GF. Acid-sensing properties in rat gastric sensory neurons from normal and ulcerated stomach. J Neurosci. 2005;25:2617–2627. doi: 10.1523/JNEUROSCI.2894-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tominaga M, Caterina M, Malmberg AB, Rosen TA, Gilbert H, Skinner K, Raumann BE, Basbaum AI, Julius D. The cloned capsaicin receptor integrates multiple pain-producing stimuli. Neuron. 1998;21:531–543. doi: 10.1016/s0896-6273(00)80564-4. [DOI] [PubMed] [Google Scholar]
- 40.Wang C, Hu HZ, Colton CK, Wood JD, Zhu MX. An alternative splicing product of the murine trpv1 gene dominant negatively modulates the activity of TRPV1 channels. J Biol Chem. 2004;279:37423–37430. doi: 10.1074/jbc.M407205200. [DOI] [PubMed] [Google Scholar]