Abstract
Objective
The purpose of this study was to describe non-Hispanic blacks that use chiropractic health care to better understand this underserved demographic.
Methods
E-mail and telephone calls were used to recruit doctors of chiropractic (DCs) in Texas and Louisiana to distribute anonymous surveys to their non-Hispanic black patients. Twenty doctors volunteered to participate. Each was sent 10 surveys and self-addressed envelopes to distribute. All doctors were given at least 3 months to distribute surveys to as many non-Hispanic black patients that they had. The survey contained 20 questions designed to develop a profile of non-Hispanic black patients that used chiropractic care. Descriptive statistics were used to summarize demographic and other patient attributes.
Results
Two-hundred surveys were distributed and 44 were completed, yielding a response rate of 22%. Non-Hispanic black patients were more likely to be female (54.5%), be older than 50 years (56.8%), be a college graduate (59.1%), be employed (61.9%), report not receiving public assistance in the past 5 years (81.4%), report a household income of $20 000 to $60 000 a year (48.8%), and born in the United States (83.7%). Participants reported that there was a DC within 30 minutes of their address (81.4%), their DC always explained things to them in an easy-to-understand manner (81.8%), their DC always showed respect for what they had to say (88.6%), and their DC always cared about them as a person (86.4%).
Conclusions
In the sample surveyed, non-Hispanic black patients tended to be female, be older, be college educated, be employed, and have a positive viewpoint on their interactions with their DC.
Key Indexing Terms: African Americans, Black, Complementary medicine, Minority health, Chiropractic
Introduction
Existing research suggests that non-Hispanic blacks use Complementary and Alternative Medicine (CAM) treatments less often than whites,1 with the exception of using religion as a form of CAM.2, 3, 4, 5, 6, 7, 8, 9 In one study, for example, Barnes et al10 demonstrated that 43.1% of white adults sought out CAM treatments in comparison to 25.5% of blacks. Furthermore, there is minimal research that provides an explanation as to why blacks use CAM less often.10, 11, 12, 13 Some reasons for the differences observed have been that whites possess higher education and increased annual income, and that blacks lack access to conventional medicine and demonstrate dissatisfaction with it in general.10, 11, 12, 13, 14
Limited existing research appears to demonstrate that there are also some similarities between white and black CAM users. White CAM demographic studies show that most users are between the ages of 35 and 49 years, are married, possess some level of college education, and have a household income more than $50,000.13, 15, 16, 17, 18, 19 Studies specifically focusing on blacks have found that CAM users have an average age of 43.3 years; they are more likely to be female, have a college education, and possess insurance.14, 20, 21, 22, 23 Blacks who regularly use CAM report that it gives them a sense of power over their own health.14 A common reason for trying CAM among blacks is that they report having another family member use it.22
Most CAM use research does not break down the amount of use of each CAM subtype (eg, chiropractic, herbal medicine, acupuncture) by minorities.24 Because of the unique intrinsic cultural differences that minority groups possess,24 their reasons for using or not using different forms of CAM remain a gap in existing research.
Chiropractic is one form of CAM as defined by the National Center for Complementary and Alternative Medicine.25 All existing survey research studies demonstrate that blacks use chiropractic health care services less often than whites.2, 3, 4, 5, 6, 7, 9, 15, 16, 26, 27, 28, 29 In many instances, whites used chiropractic at least twice as often as blacks.2, 4, 6, 7, 9, 15, 16, 26, 29 Some have attributed this difference to the perception of discrepancies of health care treatment by blacks, lower average educational levels of blacks compared to whites, and the lack of accessibility to doctors of chiropractic (DCs) in black communities.2, 4, 20, 21, 30
Very little information currently exists in the literature that describes use of chiropractic by non-Hispanic black patients. Therefore, the purpose of this study was to develop a profile of and to gain insight to non-Hispanic black patients’ utilization of chiropractic services.
Methods
This study was approved by the Texas Chiropractic College (TCC) Institutional Review Board for human subjects. All subjects were provided a written explanation of the study purpose prior to participation in the survey. This trial was registered with the University hospital Medical Information Network Clinical Trials Registry: trial number UMIN000014669.
Study Design and Setting
This was an open descriptive study designed to develop a demographic profile of non-Hispanic blacks that use chiropractic health care. Typically, national studies analyzing CAM use have used telephone,13, 31 mail,17 and secondary analyses of national data sets.18, 29, 32, 33 This study chose to use mail-out surveys distributed through chiropractic doctors’ offices. Twenty chiropractic doctors were recruited for this research study. Each doctor was given 10 anonymous self-addressed stamped surveys to distribute to their non-Hispanic black chiropractic patients; thus, 200 surveys were distributed. Anonymous surveys were mailed back directly from survey participants to the primary investigator, and responses were tallied.
Instrument Development
The initial survey was 48 questions long. Researchers then chose to limit the survey to 20 questions. The intent was to shorten the survey to reduce the likelihood that participants would feel survey fatigue and answer questions inaccurately.14 A 3-DC panel reviewed existing survey research and developed this survey. The 2 initial authors of this manuscript wrote the questions; and a third DC, TCC’s Institutional Review Board chair, reviewed them and provided input on question clarity and value. Two of the members of the panel have already published a review article on non-Hispanic black use of CAM.1 Fifteen out of the 20 survey questions were modeled after existing questions that have been used in health care survey research. The initial 8 baseline demographic questions (#1-8) for this survey were developed to be almost identical to those generated by Kronenberg et al.6 The remaining 12 survey questions were predominantly adapted from the Consumer Assessment of Healthcare Providers and Systems—Cultural Competency instrument to provide categorically unique information about the population sampled.34, 35 From the Consumer Assessment of Healthcare Providers and Systems instrument, 4 questions (#14-17) were developed to address Domain 1: Doctor Communication-Positive Behaviors. Two questions (#18-19) were developed to address Domain 3: Doctor Communication-Health Promotion. One question (#20) was developed from Domain 6: Trust. The remaining 5 questions (#9-13) were constructed by study researchers to provide insightful information about non-Hispanic blacks that chose to use chiropractic services.
The 3-page survey was printed only on one side of the paper in an attempt to prevent participants from missing questions that might be printed on the back of any page. The survey was printed in Arial size 11 font. The beginning of the survey included identification of the researchers, identification of the college conducting the survey, a nonparticipation option statement, the purpose of the study, publication statement, instructions, and the actual survey questions. The nonparticipation option statement instructed participants to discard the survey in a trash receptacle if they did not wish to complete the survey.
Chiropractic Doctor Recruitment and Their Role
Chiropractic doctors in Texas and Louisiana were recruited for this study through mass e-mail from TCC’s alumni department. In addition, the Texas Chiropractic Association volunteered to contact their member doctors and encourage them to participate in this study. Sixteen DCs that responded were included in the survey. In addition, several phone calls were made to chiropractic offices in Texas and Louisiana to recruit the last 4 DCs. Surveys were distributed in urban areas. Table 1 lists the number of DCs per city that were recruited, their county, 2013 population estimate based on census data, mean household income per county, percentage below the poverty line per county, and overall percentage of blacks in the county.36, 37, 38, 39, 40, 41 Chiropractors that were contacted via e-mail were sent a copy of the survey for their review before they decided if they wished to participate in the study. They were not allowed to modify the survey in any way. They could only inform the researchers if they wished to participate. They were provided a copy of the survey in advance, as a professional courtesy, to help ensure that they felt comfortable distributing the survey through their office.
Table 1.
| # | City and State | County | 2013 Population Estimate | Mean Household Income | % Below Poverty Line | % Black |
|---|---|---|---|---|---|---|
| 12 | Houston, TX | Harris | 4 336 853 | $53 160 | 17.9 | 19.5 |
| 2 | Pearland, TX | Brazoria | 330 242 | $68 008 | 10.9 | 13.3 |
| 1 | San Antonio, TX | Bexar | 1 817 610 | $49 141 | 17.8 | 8.2 |
| 1 | Spring, TX | Harris | 4 336 853 | $53 160 | 17.9 | 19.5 |
| 1 | Sugarland, TX | Fort Bend | 652 365 | $84 211 | 8.3 | 21.2 |
| 1 | Tomball, TX | Harris | 4 336 853 | $53 160 | 17.9 | 19.5 |
| 1 | Waco, TX | McLennan | 241 481 | $41 589 | 21.8 | 15.0 |
| 1 | Lafayette, LA | Lafayette Parish | 230 845 | $49 705 | 16.6 | 26.1 |
Once a given doctor agreed to participate in the study, he or she was mailed a large 15ʺ × 12ʺ manila envelope with 10 smaller 8½ʺ × 11ʺ surveys and self-addressed, stamped envelopes inside. The envelopes used in this study were anonymous. They had the address line for the college conducting this study on the outgoing and return address already printed on return envelopes. All returned surveys were mailed directly to the study primary investigator. The surveys themselves were also anonymous. They had no blank for participant name or signature. Chiropractic doctors that were mailed surveys were instructed to distribute up to 10 anonymous surveys to their adult non-Hispanic black chiropractic patients over a 3-month data collection window. There was no attempt by researchers to define adult, as the legal definition of adult varies slightly state to state. All returned envelopes and data entry were processed by the primary investigator to ensure uniformity. Doctors were not required to mail back unused blank surveys.
Study Participant Implied Consent
All study applicants provided their implied consent if they filled out the survey, as per the instructions listed on the survey.
Inclusion/Nonresponder Criteria
Inclusion criteria were as follows: (1) participant had to classify themselves as non-Hispanic black, and (2) participant had to be an adult chiropractic patient. Nonresponder criteria were the participant failed to complete the survey or did not desire to participate.
Statistical Analysis
Data were analyzed in SPSS version 20.0 (IBM, Armonk, NY). Descriptive statistics were used to illustrate the number of responses and overall percentage of responses for each option of survey questions.
Results
Forty-four surveys out of 200 were returned, yielding a response rate of 22%. Table 2, Table 3 and Figure 1 list the demographic data, survey questions, and responses. Data in the “Results” section are listed as percentage followed by raw total response rate for that given question. Demographically, non-Hispanic black patients were most likely to be female (54.5%, 44), be older than 50 years (56.8%, 44), be a college graduate (59.1%, 44), be employed (61.9%, 42), report not receiving public assistance in the preceding 5 years (81.4%, 43), have a household income between $20 000 and $60 000 a year (48.8%, 41), state that they were born in the United States (83.7%, 43), and report their self-assessed health as good (59.5%, 42). For the final 12 questions, most participants lived within 30 minutes of their DC (81.4%, 43), drove less than 30 miles to see their DC (71.4%, 42), saw their DC for back pain (46.5%, 43), visited a DC because a friend referred them (33.3%, 42), stated that they never used chiropractic care before their current treatment (34.9%, 43), reported that their DC always explained things to them in an easy-to-understand manner (81.8%, 44), asserted that their DC always spent enough time with them (77.3%, 44), stated that their DC always showed respect for what they had to say (88.6%, 44), reported that their chiropractor always gave them easy-to-understand instructions about their health problems (79.5%, 44), asserted that their DC always instructed them on a healthy diet (38.7%, 44), stated that their DC always discussed physical activity with them (59.1%, 44), and reported that their DC always cared about them as a person (86.4%, 44).
Table 2.
Initial 8 Survey Questions That Focused on Sociodemographic Information
| Attribute | n | Subgroup | % of n |
|---|---|---|---|
| 1. Sex | 44 | ||
| Male | 20 | 45.5 | |
| Female | 24 | 54.5 | |
| Other | 0 | 0.0 | |
| 2. Age, y | 44 | ||
| 18-29 | 1 | 2.3 | |
| 30-49 | 18 | 40.9 | |
| ≥ 50 | 25 | 56.8 | |
| 3. Level of education completed | 44 | ||
| Less than high school | 0 | 0.0 | |
| Completed high school | 8 | 18.2 | |
| 2 y of college | 10 | 22.7 | |
| College graduate or more | 26 | 59.1 | |
| 4. Currently employed | 42 | ||
| Yes | 26 | 61.9 | |
| No | 16 | 38.1 | |
| 5. Received public assistance in past 5 y | 43 | ||
| Yes | 8 | 18.6 | |
| No | 35 | 81.4 | |
| 6. Current household income | 41 | ||
| <$20 000/y | 8 | 19.5 | |
| $20 000-$60 000/y | 20 | 48.8 | |
| > $60 000/y | 13 | 31.7 | |
| 7. Born in United States | 43 | ||
| Yes | 36 | 83.7 | |
| No | 7 | 16.3 | |
| 8. Self-assessed health status | 42 | ||
| Excellent | 2 | 4.8 | |
| Good | 25 | 59.5 | |
| Fair | 15 | 35.7 | |
| Poor | 0 | 0.0 |
These are not the exact questions asked, but they represent a bulleted summary of survey data similar to tables generated by Kronenberg et al.6
Table 3.
Remaining 12 Questions That Attempted to Gain Insight Into Why Non-Hispanic Blacks Choose to Use Chiropractic Care
| Question Asked of Survey Participants | n | Subgroup | % of n |
|---|---|---|---|
| 9. Is there a chiropractor's office within 30 min of your place of residence? | 43 | ||
| Yes | 35 | 81.4 | |
| No | 3 | 7.0 | |
| Unsure | 5 | 11.6 | |
| 10. Did you have to drive more than 30 min to see the chiropractor treating you now? | 42 | ||
| Yes | 12 | 28.6 | |
| No | 30 | 71.4 | |
| Unsure | 0 | 0.0 | |
| 11. What is the main reason for you seeking care by a chiropractor? | 43 | ||
| Neck pain | 8 | 18.6 | |
| Back pain | 20 | 46.5 | |
| Personal injury | 8 | 18.6 | |
| Referral from a friend/family member | 2 | 4.7 | |
| Other (please specify)______________ | 5 | 11.6 | |
| 12. Which of the following best describes the reason you first began using chiropractic treatment? | 42 | ||
| My first visit to the chiropractor was when a parent took me there. | 2 | 4.8 | |
| I first tried chiropractic care because a friend recommended it. | 14 | 33.3 | |
| I saw an advertisement (newspaper, billboard, mailer, etc) and decided to try it. | 1 | 2.4 | |
| I was referred there by another health care provider (MD, nurse, podiatrist, etc). | 12 | 28.5 | |
| Other (please specify)______________ | 13 | 31 | |
| 13. Which of these best describes your use of chiropractic health care (either for your current problem or other conditions)? | 43 | ||
| Never used chiropractic health care before this series of treatments. | 15 | 34.9 | |
| I have had problems treated before by chiropractors, probably on 1 or 2 occasions. | 11 | 25.6 | |
| I have had problems treated before by chiropractors on many occasions. | 9 | 20.9 | |
| I usually get regular chiropractic care, regardless of whether or not I have a problem. | 8 | 18.6 | |
| 14. During your visits, did the chiropractor explain things to you in a way that was easy to understand? | 44 | ||
| Never | 1 | 2.3 | |
| Sometimes | 0 | 0.0 | |
| Usually | 7 | 15.9 | |
| Always | 36 | 81.8 | |
| 15. During your visits, did you feel the chiropractor spent enough time with you? | 44 | ||
| Never | 1 | 2.3 | |
| Sometimes | 0 | 0.0 | |
| Usually | 9 | 20.4 | |
| Always | 34 | 77.3 | |
| 16. During your visits, did the chiropractor show respect for what you had to say? | 44 | ||
| Never | 0 | 0.0 | |
| Sometimes | 0 | 0.0 | |
| Usually | 5 | 11.4 | |
| Always | 39 | 88.6 | |
| 17. During your visits, did the chiropractor give you easy-to-understand instructions about taking care of your health problems or concerns? | 44 | ||
| Never | 0 | 0.0 | |
| Sometimes | 3 | 6.9 | |
| Usually | 6 | 13.6 | |
| Always | 35 | 79.5 | |
| 18. During your visits, did the chiropractor talk about a healthy diet and healthy eating habits? | 44 | ||
| Never | 7 | 15.9 | |
| Sometimes | 10 | 22.7 | |
| Usually | 10 | 22.7 | |
| Always | 17 | 38.7 | |
| 19. During your visits, did the chiropractor talk about exercise or physical activity with you? | 44 | ||
| Never | 1 | 2.3 | |
| Sometimes | 8 | 18.2 | |
| Usually | 9 | 20.4 | |
| Always | 26 | 59.1 | |
| 20. How often have you felt that the chiropractor really cared about you as a person? | 44 | ||
| Never | 0 | 0.0 | |
| Sometimes | 0 | 0.0 | |
| Usually | 6 | 13.6 | |
| Always | 38 | 86.4 |
These were the exact questions asked.
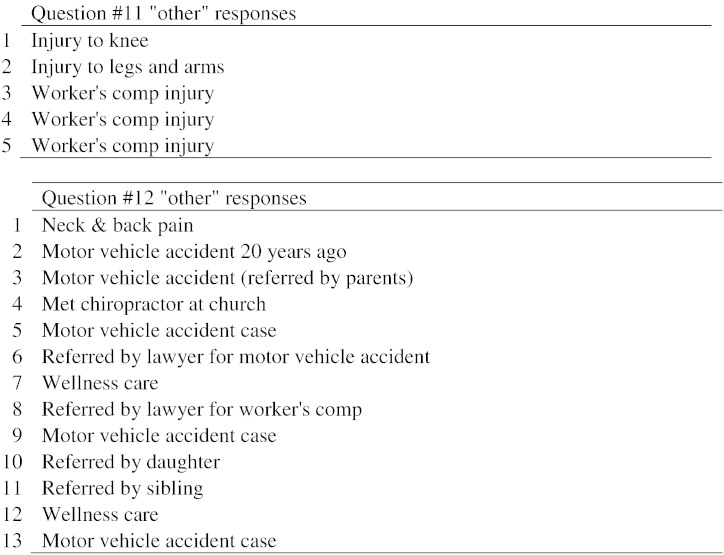
Figure 1.
Other category responses to questions 11 and 12.
Discussion
Existing survey research studies show that blacks use chiropractic health care services less often than whites.2, 3, 4, 5, 6, 7, 9, 15, 16, 26, 27, 28, 29 Some researchers have attributed this difference to the perception of discrepancies of health care treatment by blacks, lower average educational levels of blacks compared to whites, and the lack of accessibility to DC s in black communities.2, 4, 20, 21, 30 In this study, researchers found that non-Hispanic black patients that do use chiropractic services have a positive outlook on doctor-patient interactions with their DC, they often are college graduates, and they live within 30 minutes of their DC. In addition, researchers found that non-Hispanic black women marginally use chiropractic services more often than men, which is in congruence with existing CAM research overall.3
Studies have demonstrated that blacks trust the medical system less than whites42, 43 and that health disparities in their care exist.44, 45, 46, 47 For example, several articles have shown that blacks receive less care, less intensive treatment, and less follow-up care in general.48, 49 This is believed to result in them suffering from higher morbidity and mortality.49 For example, Schwamm et al48 performed a study where they found that blacks had lower odds compared to white patients of receiving intravenous thrombolysis, deep vein thrombosis prophylaxis, smoking cessation encouragement, discharge antithrombotics, or anticoagulants for atrial fibrillation upon presentation to a hospital with ischemic stroke. Similarly, Jacobs et al45 found that blacks with ischemic stroke were less likely to receive door-to-computed-tomography times of less than 25 minutes at emergency medicine centers when compared to whites. In addition, multiple other researchers have found a similar trend of blacks receiving appropriate intravenous medications following a stroke less often compared to whites at hospitals, to include academic hospitals.50, 51
One focus group study attempted to delve into some of the reasons for the mistrust. They found that blacks strongly perceived that allopathic doctors overprescribe medications to receive financial incentives from pharmaceutical companies and that they do not have the patient’s best interest in mind.42
Some researchers have suggested that the use of different forms of CAM may help decrease health disparities among ethnic minorities.52 Increased utilization of chiropractic health care may provide blacks with more diverse health care options, particularly with soft tissue injuries associated with neck and low back pain. Research demonstrates that spinal manipulation can have a positive impact on neck and low back pain.53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65 Future directions to engage in after this study that researchers intend to pursue shall be to (1) engage in a larger study to confirm trends observed with this survey and monitor health care disparities in a more in-depth manner and (2) develop a demographic profile of non-Hispanic blacks that do not use chiropractic health care for comparison purposes.
Researchers recommend that future chiropractic social scientists engaging in similar minority research use focus groups first to ensure that the survey questions are as clear as possible.14 Then, after the face validity of the survey instrument is established, they should distribute fewer surveys per DC than what was performed in this experiment. In this study, survey distribution was a limiting factor. Instead of distributing 10 surveys to each DC, researchers suggest that distributing 4 to 5 surveys per doctor may be a more effective use of resources that would yield a better overall return. Throughout the process of recruiting doctors to distribute the survey, approximately 6 doctors informed us via e-mail or over the phone that they only had 1 to 2 non-Hispanic black active patients, thus emphasizing the point that distributing fewer surveys per doctor might reach more of the intended minority population.
Limitations
The primary limitation of this study was the small sample size. As a result, a broader and larger study would be more informative of data trends within this population. Because of the limited distribution of this survey in cities in Texas and one in Louisiana, the results of this research are most representative of regional attributes of patients and not national attributes.
This is the first time that this survey has been distributed, and it is plausible to suggest that some of the questions researchers used were not as optimal as possible. For example, upon further analysis of questions #9 and #10, researchers felt that there likely was too much overlap in the information they provided to researchers. Researchers also failed to ask about marital status in the survey as some other CAM researchers have done.4, 24 Being married has been correlated with a significant increase in lifespan among non-Hispanic black men and the likelihood that they will engage in better health care choices.66 In addition, researchers regretted not asking patients about their viewpoint on conventional medicine.
Another area that future researchers could analyze is the link between visiting a DC, as a form of CAM, and visiting an allopathic physician in the same year. Some CAM research has shown a link between using CAM and visiting a physician in the preceding 6 months to 1 year.4, 8 This may indicate that a patient is more proactive in taking care of his or her own health or perhaps that he or she is sicker and is seeking out every avenue of care. This is also pertinent because studies have shown that non-Hispanic blacks have 63% to 72% nondisclosure rates of CAM use to their allopathic physician.4, 67 All of these retrospective observations may be used to enhance the quality of future CAM use surveys that focus on minorities.
In addition, participants did not have an opportunity to interact with researchers directly. This could be an issue if participants read a question and did not clearly understand what the question was asking or how to optimally answer a given question (eg, the questions that were left unanswered on the survey in Table 2, Table 3). Having researchers physically present at the geographically separated clinics was not possible because of the very limited budget for this study. Another possible improvement over this phenomenon could be to include a “does not apply” option to some of the survey questions.
Conclusions
The findings of this small survey study preliminarily suggest that non-Hispanic black patients in the United States appear to be older, be college educated, and have a positive viewpoint on their interactions with their DC.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
References
- 1.Ward J., Humphries K., Ramcharan M., Webb C. Review of the use of complementary and alternative medicine by non-Hispanic blacks. Top Integr Health Care. 2013;4 [ID 4.1004] [Google Scholar]
- 2.Cuellar N., Aycock T., Cahill B., Ford J. Complementary and alternative medicine (CAM) use by African American (AA) and Caucasian American (CA) older adults in a rural setting: a descriptive, comparative study. BMC Complement Altern Med. 2003;3:8. doi: 10.1186/1472-6882-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldstein M., Brown E., Ballard-Barbash R. The use of complementary and alternative medicine among California adults with and without cancer. Evid Based Complement Alternat Med. 2005;2:557–565. doi: 10.1093/ecam/neh138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Graham R., Ahn A., Davis R., O’Connor B., Eisenberg D., Phillips R. Use of complementary and alternative medical therapies among racial and ethnic minority adults: results from the 2002 National Health Interview Survey. J Natl Med Assoc. 2005;97:535–545. [PMC free article] [PubMed] [Google Scholar]
- 5.Hsiao A., Wong M., Goldstein M. Variation in complementary and alternative medicine (CAM) use across racial/ethnic groups and the development of ethnic-specific measures of CAM use. J Altern Complement Med. 2006;12:281–290. doi: 10.1089/acm.2006.12.281. [DOI] [PubMed] [Google Scholar]
- 6.Kronenberg F., Cushman L., Wade C., Kalmuss D., Chao M. Race/ethnicity and women’s use of complementary and alternative medicine in the United States: results of a national survey. Am J Public Health. 2006;96:1236–1242. doi: 10.2105/AJPH.2004.047688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu K., Farrell T. The complementarity and substitution between unconventional and mainstream medicine among racial and ethnic groups in the United States. Health Serv Res. 2007;42:811–826. doi: 10.1111/j.1475-6773.2006.00628.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilkinson J., Saper R., Rosen A., Welles S., Culpepper L. Prayer for health and primary care: results from the 2002 National Health Interview Survey. Fam Med. 2008;40:638–644. [PMC free article] [PubMed] [Google Scholar]
- 9.Upchurch D., Dye C., Chyu L., Gold E., Greendale G. Demographic, behavioral, and health correlates of complementary and alternative medicine and prayer use among midlife women: 2002. J Women's Health. 2010;19:23–30. doi: 10.1089/jwh.2008.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barnes P., Bloom B., Nahin R. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1–23. [PubMed] [Google Scholar]
- 11.Kessler R., Davis R., Foster D. Long-term trends in the use of complementary and alternative medical therapies in the United States. Ann Intern Med. 2001;135:262–268. doi: 10.7326/0003-4819-135-4-200108210-00011. [DOI] [PubMed] [Google Scholar]
- 12.Eisenberg D., Kessler R., Foster C., Norlock F., Calkins D., Delbanco T. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328:246–252. doi: 10.1056/NEJM199301283280406. [DOI] [PubMed] [Google Scholar]
- 13.Eisenberg D., Davis R., Ettner S. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. J Am Med Assoc. 1998;280:1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 14.Barnett M., Cotroneo M., Purnell J., Martin D., Mackenzie E., Fishman A. Use of CAM in local African-American communities: community-partnered research. J Natl Med Assoc. 2003;95:943–950. [PMC free article] [PubMed] [Google Scholar]
- 15.Ndetan H., Bae S., Evans M., Rupert R., Singh K. Characterization of health status and modifiable risk behavior among United States adults using chiropractic care as compared with general medical care. J Manipulative Physiol Ther. 2009;32:414–422. doi: 10.1016/j.jmpt.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 16.Conboy L., Patel S., Kaptchuk T., Gottlieb B., Eisenberg D., Acevedo-Garcia D. Sociodemographic determinants of the utilization of specific types of complementary and alternative medicine: an analysis based on a nationally representative survey sample. J Altern Complement Med. 2005;11:977–994. doi: 10.1089/acm.2005.11.977. [DOI] [PubMed] [Google Scholar]
- 17.Astin J. Why patients use alternative medicine: results of a national study. J Am Med Assoc. 1998;279:1548–1553. doi: 10.1001/jama.279.19.1548. [DOI] [PubMed] [Google Scholar]
- 18.Paramore L. Use of alternative therapies: estimates from the 1994 Robert Wood Johnson Foundation national access to care survey. J Pain Symptom Manage. 1997;13:83–89. doi: 10.1016/s0885-3924(96)00299-0. [DOI] [PubMed] [Google Scholar]
- 19.Gold E., Sternfeld B., Kelsey J. Relation of demographic and lifestyle factors to symptoms in a multi-racial/ethnic population of women 40-55 years of age. Am J Epidemiol. 2000;152:463–473. doi: 10.1093/aje/152.5.463. [DOI] [PubMed] [Google Scholar]
- 20.Brown C., Barner J., Richards K., Bohman T. Patterns of complementary and alternative medicine use in African Americans. J Altern Complement Med. 2007;13:751–758. doi: 10.1089/acm.2006.6392. [DOI] [PubMed] [Google Scholar]
- 21.Brown C., Barner J., Bohman T., Richards K. A multivariate test of an expanded Andersen Health Care Utilization Model for Complementary and Alternative Medicine (CAM) use in African Americans. J Altern Complement Med. 2009;15:911–919. doi: 10.1089/acm.2008.0561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chao M., Wade C., Kronenberg F., Kalmuss D., Cushman L. Women’s reasons for complementary and alternative medicine use: racial/ethnic differences. J Altern Complement Med. 2006;12:719–720. doi: 10.1089/acm.2006.12.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ni H., Simile C., Hardy A. Utilization of complementary and alternative medicine by United States adults: results from the 1999 national health interview survey. Med Care. 2002;40:353–358. doi: 10.1097/00005650-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Bair Y., Gold E., Greendale G. Ethnic differences in the use of complementary and alternative medicine at midlife: longitudinal results from SWAN participants. Am J Public Health. 2002;92:1832–1840. doi: 10.2105/ajph.92.11.1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lester M. National Center for Complementary and Alternative Medicine; Washington (DC): 2012. Chiropractic: an introduction [Internet] [cited 2014 Jul 29. Available from: http://www.nccam.nih.gov/health/chiropractic/introduction.htm] [Google Scholar]
- 26.Weigel P., Hockenberry J., Bentler S. A longitudinal study of chiropractic use among older adults in the United States. Chiropr Osteopat. 2010;18:34. doi: 10.1186/1746-1340-18-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wolinsky F., Liu L., Miller T. The use of chiropractors by older adults in the United States. Chiropr Osteopat. 2007;15:12. doi: 10.1186/1746-1340-15-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ness J., Cirillo D., Weir D., Nisly N., Wallace R. Use of complementary medicine in older Americans: results from the Health and Retirement Study. Gerontologist. 2005;45:516–524. doi: 10.1093/geront/45.4.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mackenzie E., Taylor L., Bloom B., Hufford D., Johnson J. Ethnic minority use of complementary and alternative medicine (CAM): a national probability survey of CAM utilizers. Altern Ther Health Med. 2003;9:50–56. [PubMed] [Google Scholar]
- 30.Barner J., Bohman T., Brown C., Richards K. Use of complementary and alternative medicine for treatment among African-Americans: a multivariate analysis. Res Social Adm Pharm. 2010;6:196–208. doi: 10.1016/j.sapharm.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blendon R., DesRoches C., Benson J., Brodie M., Altman D. Americans' views on the use and regulation of dietary supplements. Arch Intern Med. 2001;161:805–810. doi: 10.1001/archinte.161.6.805. [DOI] [PubMed] [Google Scholar]
- 32.Boyd E., Taylor S., Shimp L., Semler C. An assessment of home remedy use by African Americans. J Natl Med Assoc. 2000;92:341–353. [PMC free article] [PubMed] [Google Scholar]
- 33.Bausell R., Lee W., Berman B. Demographic and health-related correlates of visits to complementary and alternative medical providers. Med Care. 2001;39:190–196. doi: 10.1097/00005650-200102000-00009. [DOI] [PubMed] [Google Scholar]
- 34.Weech-Maldonado R., Carle A., Weidmer B., Hurtado M., Ngo-Metzger Q., Hays R. The Consumer Assessment of Healthcare Providers and Systems (CAHPS) cultural competence (CC) item set. Med Care. 2012;50:S22–S31. doi: 10.1097/MLR.0b013e318263134b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carle A., Weech-Maldonado R. Does the Consumer Assessment of Healthcare Providers and Systems Cultural Competence survey provide equivalent measurement across English and Spanish versions? Med Care. 2012;50:S37–S41. doi: 10.1097/MLR.0b013e3182665189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.United States Census Bureau . US Census Bureau; Washington, (DC): 2013. Harris County, Texas [Internet] [Available from: quickfacts.census.gov/qfd/states/48/48201.html] [Google Scholar]
- 37.United States Census Bureau . US Census Bureau; Washington, (DC): 2013. Brazoria County, Texas [Internet] [Available from: quickfacts.census.gov/qfd/states/48/48039.html] [Google Scholar]
- 38.United States Census Bureau . US Census Bureau; Washington, (DC): 2013. . Bexar County, Texas [Internet] [Available from: quickfacts.census.gov/qfd/states/48/48029.html] [Google Scholar]
- 39.United States Census Bureau . US Census Bureau; Washington, (DC): 2013. Fort Bend County, Texas [Internet] [Available from: quickfacts.census.gov/qfd/states/48/48157.html] [Google Scholar]
- 40.United States Census Bureau . US Census Bureau; Washington, (DC): 2013. McLennan County, Texas [Internet] [Available from: quickfacts.census.gov/qfd/states/48/48309.html] [Google Scholar]
- 41.United States Census Bureau . US Census Bureau; Washington, (DC): 2013. Lafayette Parish County, Texas [Internet] [Available from: quickfacts.census.gov/qfd/states/22/22055.html] [Google Scholar]
- 42.Sewell K., Andreae S., Luke E., Safford M. Perceptions of and barriers to use of generic medications in a rural African American population, Alabama, 2011. Prev Chronic Dis. 2012;9:120010. doi: 10.5888/pcd9.120010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thorburn S., Faith J., Keon K., Tippens K. Discrimination in health care and CAM use in a representative sample of U.S. adults. J Altern Complement Med. 2013;19:577–581. doi: 10.1089/acm.2012.0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Villarruel A. Introduction: eliminating health disparities among racial and ethnic minorities in the United States. Annu Rev Nurs Res. 2004;22:1–6. [PubMed] [Google Scholar]
- 45.Jacobs B., Birbeck G., Mullard J. Quality of hospital care in African American and white patients with ischemic stroke and TIA. Neurology. 2006;66:809–814. doi: 10.1212/01.wnl.0000203335.45804.72. [DOI] [PubMed] [Google Scholar]
- 46.Ravenell J., Johnson W., Jr., Whitaker E. African-American men’s perceptions of health: a focus group study. J Natl Med Assoc. 2006;98:544–550. [PMC free article] [PubMed] [Google Scholar]
- 47.Dunlop D., Manheim L., Song J., Chang R. Gender and ethnic/racial disparities in health care utilization among older adults. J Gerontol B Psychol Sci Soc Sci. 2002;57:S221–S233. doi: 10.1093/geronb/57.4.s221. [DOI] [PubMed] [Google Scholar]
- 48.Schwamm L., Reeves M., Pan W. Race/ethnicity, quality of care, and outcomes in ischemic stroke. Circulation. 2010;121:1492–1501. doi: 10.1161/CIRCULATIONAHA.109.881490. [DOI] [PubMed] [Google Scholar]
- 49.Betancourt J. Eliminating racial and ethnic disparities in health care: what is the role of academic medicine? Acad Med. 2006;81:788–792. doi: 10.1097/00001888-200609000-00004. [DOI] [PubMed] [Google Scholar]
- 50.Johnston S., Fung L., Gillum L. Utilization of intravenous tissue-type plasminogen activator for ischemic stroke at academic medical centers: the influence of ethnicity. Stroke. 2001;32:1061–1068. doi: 10.1161/01.str.32.5.1061. [DOI] [PubMed] [Google Scholar]
- 51.Reed S., Cramer S., Blough D., Meyer K., Jarvik J. Treatment with tissue plasminogen activator and inpatient mortality rates for patients with ischemic stroke treated in community hospitals. Stroke. 2001;32:1832–1840. doi: 10.1161/01.str.32.8.1832. [DOI] [PubMed] [Google Scholar]
- 52.Struthers R., Nichols L. Utilization of complementary and alternative medicine among racial and ethnic minority populations: implications for reducing health disparities. Annu Rev Nurs Res. 2004;22:285–313. [PubMed] [Google Scholar]
- 53.Goertz M., Thorson D., Bonsell J. Institute for Clinical Systems Improvement (US); Bloomington (MN): 2012. Adult acute and subacute low back pain. [92 p. Report No.: 15th ed.] [Google Scholar]
- 54.Assendelft W., Morton S., Yu E., Suttorp M., Shekelle P. Spinal manipulative therapy for low back pain. Cochrane Database Syst Rev. 2004;1:CD000447. doi: 10.1002/14651858.CD000447.pub2. [DOI] [PubMed] [Google Scholar]
- 55.Dagenais S., Tricco A., Haldeman S. Synthesis of recommendations for the assessment and management of low back pain from recent clinical practice guidelines. Spine J. 2010;10:514–529. doi: 10.1016/j.spinee.2010.03.032. [DOI] [PubMed] [Google Scholar]
- 56.Juni P., Battaglia M., Nuesch E. A randomised controlled trial of spinal manipulative therapy in acute low back pain. Ann Rheum Dis. 2009;68:1420–1427. doi: 10.1136/ard.2008.093757. [DOI] [PubMed] [Google Scholar]
- 57.Santilli V., Beghi E., Finucci S. Chiropractic manipulation in the treatment of acute back pain and sciatica with disc protrusion: a randomized double-blind clinical trial of active and simulated spinal manipulations. Spine J. 2006;6:131–137. doi: 10.1016/j.spinee.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 58.Walker B., French S., Grant W., Green S. Combined chiropractic interventions for low-back pain. Cochrane Database Syst Rev. 2010;4:CD005427. doi: 10.1002/14651858.CD005427.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Anderson-Peacock E., Blouin J., Bryans R. Chiropractic clinical practice guideline: evidence-based treatment of adult neck pain not due to whiplash. J Can Chiropr Assoc. 2005;49:158–209. [PMC free article] [PubMed] [Google Scholar]
- 60.Cassidy J., Quon J., LaFrance L., Yong-Hing K. The effect of manipulation on pain and range of motion in the cervical spine: a pilot study. J Manipulative Physiol Ther. 1992;15:495–500. [PubMed] [Google Scholar]
- 61.Vernon H., Aker P., Burns S., Viljakaanen S., Short L. Pressure pain threshold evaluation of the effect of spinal manipulation in the treatment of chronic neck pain: a pilot study. J Manipulative Physiol Ther. 1990;13:13–16. [PubMed] [Google Scholar]
- 62.Pikula J. The effect of spinal manipulative therapy (SMT) on pain reduction and range of motion in patients with acute unilateral neck pain: a pilot study. J Can Chiropr Assoc. 1999;43:111–119. [Google Scholar]
- 63.Yurkiw D., Mior S. Comparison of two chiropractic techniques on pain and lateral flexion in neck pain patients: a pilot study. Chiropr Tech. 1996;8:155–162. [Google Scholar]
- 64.Globe G., Morris C., Whalen W., Farabaugh R., Hawk C. Chiropractic management of low back disorders: report from a consensus process. J Manipulative Physiol Ther. 2008;31:651–658. doi: 10.1016/j.jmpt.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 65.Lawrence D., Meeker W., Branson R. Chiropractic management of low back pain and low back-related leg complaints: a literature synthesis. J Manipulative Physiol Ther. 2008;31:659–674. doi: 10.1016/j.jmpt.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 66.Haldane E., Mincy R., Miller D. Racial disparities in men’s health and the transition to marriage among unmarried fathers. J Fam Issues. 2010;31:1183–1210. doi: 10.1177/0192513X10365830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Eisenberg D., Kessler R., Van Rompay M. Perceptions about complementary therapies relative to conventional therapies among adults who use both: results from a national survey. Ann Intern Med. 2001;135:344–351. doi: 10.7326/0003-4819-135-5-200109040-00011. [DOI] [PubMed] [Google Scholar]