The authors observed reductions in hospital use for patients with cancer related to an observation unit in a comprehensive cancer center. Adoption of this approach could reduce hospital use, which is of interest to hospitals, payers, and patients.
Abstract
Purpose:
For patients with cancer, the impact of observation status on hospital and patient outcomes is not well understood. Our objective was to assess the impact that an observation unit had on hospital use for patients with cancer who presented to the Urgent Care Center at a comprehensive cancer center.
Methods:
We assessed the proportion of Urgent Care Center visits that resulted in an admission to the hospital at a comprehensive cancer center, before (July 9, 2012–December 31, 2012) versus after (July 9, 2013–December 31, 2013) implementation of the observation unit. We also assessed differences in length of stay and stratified the data by presenting complaint.
Results:
During each 6-month study interval, there were more than 10,000 patient visits to the Urgent Care Center, representing approximately 6,000 unique patients. Fewer visits resulted in an inpatient admission postimplementation (47%) compared with preimplementation (50%). The duration of hospital stay for admitted patients was higher in the post period (median 108 hours) than in the pre period (median 96 hours). Alternatively, the proportion of hospital admissions with a length of stay less than 24 hours was lower in the post period (pre: 7%; post: 5%). Lower admission rates postimplementation were observed for patients who presented with fluid and electrolyte disorders, nausea and vomiting, syncope, and chest pain.
Conclusion:
We observed reductions in hospital use for patients with cancer related to an observation unit in a comprehensive cancer center. Adoption of this approach for this patient population has the potential to reduce hospital use, which is of interest to hospitals, payers, and patients.
Introduction
For patients with cancer, the impact of observation status on hospital and patient outcomes is not well understood. “Observation status” refers to an alternative to hospital admission for patients who do not meet admission criteria at initial evaluation but require additional monitoring or short-term treatment. It is intended to be used to inform the decision regarding whether a patient will require a hospital admission or can be discharged.1,2 Approximately one third of emergency departments in the United States have an observation unit or clinical decision unit.3 There is increasing interest from hospitals in this approach given Medicare reimbursement policies that encourage a reduction in unnecessary hospital admissions and readmissions.4,5
Patients with cancer experience many of the same clinical concerns for which observation care has been established as a safe and cost-effective alternative to hospital admission. These include chest pain, new atrial fibrillation, asthma exacerbation, syncope, and transient ischemic attack.1,4,6,7 Some cancer-specific emergencies require only short-term interventions, such as intravenous hydration, antibiotics, analgesia, and antiemetics. Reducing avoidable hospital admissions can reduce patients' exposure to hospital-acquired conditions, maximize the use of limited societal resources, and optimize hospital resources for patients in need of high-level care.5,8 A hospital admission may be deemed a failure, or interfere with planned future therapy. Unnecessary hospitalization of patients with advanced GI malignancies has been associated with increased 90-day mortality.9 Patients with cancer generally do not want to be in the hospital.
Memorial Sloan Kettering Cancer Center (MSK) introduced an urgent care observation unit (OU) in July 2013. The Urgent Care Center (UCC), the MSK emergency department, is the central entry point for hospital admissions for nonsurgical patients. The OU was intended to provide an alternative to hospital admission for patients with a high likelihood of discharge after fewer than 24 hours of hospital-level care, or for patients who require further monitoring and diagnostic testing before safe discharge. The implementation of the OU represented a change in patient management. From the OU, UCC physicians determine whether patients should be admitted, sent home, or sent to another destination outside the hospital.
Our objective was to assess the impact that the OU had on hospital use for patients with cancer presenting to the UCC. We hypothesized that OU implementation would lead to a decrease in hospital use. We were also interested in examining the pattern of subsequent hospital admissions for patients in the OU in order to identify subgroups of patients for whom the OU provided the most benefit in this regard.
Methods
We conducted a retrospective study using data from the MSK institutional database to assess the impact of observation status on hospital use for patients with cancer.
Intervention: OU at MSK
The MSK OU is a “virtual unit” composed of 11 inpatient beds and staffed by midlevel providers and supervising attending physicians from the UCC. A nine-bed designated unit adjacent to the UCC is scheduled to open at the end of 2014. In the OU, there is an emphasis on frequent reassessment, continuity of care, and discharge within 24 hours when possible. Patients are seen throughout the day by the same clinical team that evaluated them in the UCC. This model allows for more continuity of care. The OU team tends to have smaller caseloads with higher turnover rates than inpatient teams.
Although secondary issues are addressed, the focus of care in the OU remains on specific acute problems. Diagnostic studies and consults ordered by the OU team are accorded a high priority by the institution and are expedited whenever possible. The OU also provides an alternative to hospital admission for patients who require an urgent procedure. Examples include interventional radiology placement or revision of pleural, biliary, and ureteral catheters in patients without evidence of an active infection; interventional radiology placement of inferior vena cava filters; revision of enteral feeding/drainage tubes; and biliary obstruction amenable to endoscopic or interventional radiology management.
Study Sample and Time Period
We included data from all nonsurgical patients > 18 years old who presented to the UCC at MSK for two 6-month intervals: pre-OU implementation (July 9, 2012–December 31, 2012) and post (July 9, 2013–December 31, 2013). Pediatric patients and those seen for scheduled nursing visits such as drug administration or chemotherapy disconnection were excluded. Each UCC patient visit was considered unique.
Analysis
We used χ2 tests to compare chief complaints and patients' age, sex, race, and ethnicity for those who presented to the UCC between study intervals. Then, we compared the proportion of UCC visits that resulted in an admission to the hospital pre- and post-OU implementation using χ2 tests. We also assessed patients' duration of stay, accounting for both hospital time and OU time. We included both in order to assess whether any observed differences in length of stay reflected differences in total bed time or solely reflected shifts in location of stay between an inpatient bed and an OU bed. We also evaluated the impact of the OU on readmissions to MSK within 72 hours of hospital discharge and on return to the UCC within 72 hours of UCC discharge.
To better understand the impact of the OU on hospital use for different patient subgroups, we stratified the data by UCC presenting complaint. We also followed the discharge patterns of these subgroups from the OU.
Differences were considered significant at the P < .05 level. This study was considered exempt research by the MSK Institutional Review Board.
Results
During each 6-month study interval, there were more than 10,000 patient visits to the UCC, representing approximately 6,000 unique patients. The patient demographic characteristics associated with the visits were similar during both intervals. Of the total visits, the mean age of patients was 60 years (median: 62), 46% were male, 7% were of Hispanic ethnicity, and 75% were white. The most common presenting chief complaints for UCC visits were fever (11%), abdominal pain (8%), uncontrolled back or limb pain (8%), dyspnea (6%), and neurologic abnormalities (6%). The proportions were similar between the pre and post periods. (Table 1).
Table 1.
Demographic and Clinical Characteristics of Patient Visits to the UCC, Before and After Implementation of the OU*
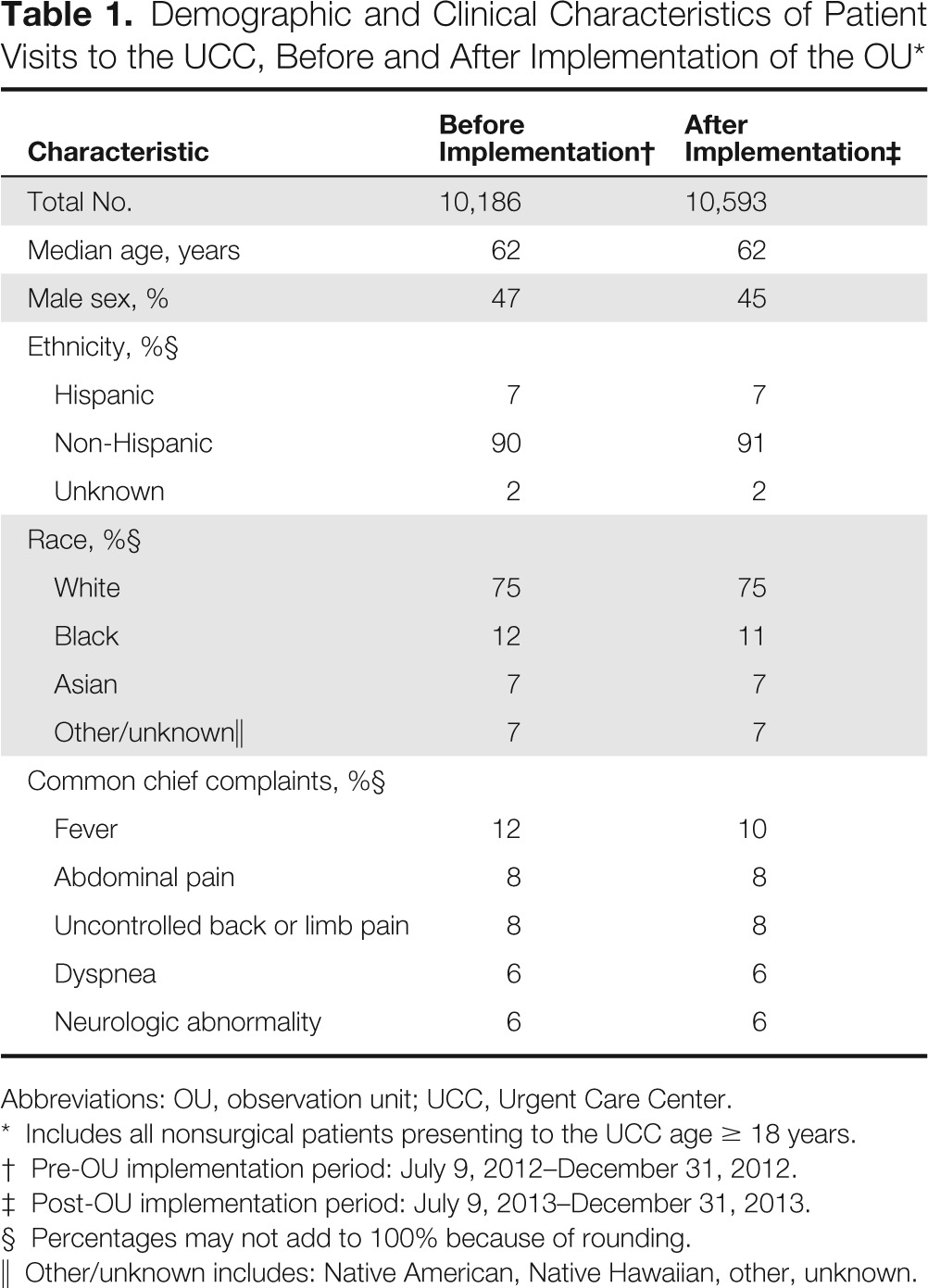
| Characteristic | Before Implementation† | After Implementation‡ |
|---|---|---|
| Total No. | 10,186 | 10,593 |
| Median age, years | 62 | 62 |
| Male sex, % | 47 | 45 |
| Ethnicity, %§ | ||
| Hispanic | 7 | 7 |
| Non-Hispanic | 90 | 91 |
| Unknown | 2 | 2 |
| Race, %§ | ||
| White | 75 | 75 |
| Black | 12 | 11 |
| Asian | 7 | 7 |
| Other/unknown∥ | 7 | 7 |
| Common chief complaints, %§ | ||
| Fever | 12 | 10 |
| Abdominal pain | 8 | 8 |
| Uncontrolled back or limb pain | 8 | 8 |
| Dyspnea | 6 | 6 |
| Neurologic abnormality | 6 | 6 |
Abbreviations: OU, observation unit; UCC, Urgent Care Center.
Includes all nonsurgical patients presenting to the UCC age ≥ 18 years.
Pre-OU implementation period: July 9, 2012–December 31, 2012.
Post-OU implementation period: July 9, 2013–December 31, 2013.
Percentages may not add to 100% because of rounding.
Other/unknown includes: Native American, Native Hawaiian, other, unknown.
Fewer UCC visits resulted in an inpatient admission after OU implementation (47%) compared with before implementation (50%; P < .001). The duration of hospital stay for admitted patients was higher in the post period (median 108 hours) than in the pre period (median 96 hours; P < .001). The proportion of hospital admissions with a length of stay less than 24 hours was lower in the post period (pre-OU: 7%; post-OU: 5%; P < .001). When we combined inpatient time and OU time, the total duration of stay for patients was lower post-OU implementation (median 93 hours) than pre (median 96 hours; P < .001; Figure 1). There was no significant difference in readmissions to MSK within 72 hours of discharge for the visits associated with a hospital admission (pre-OU: 0.37% of visits; post-OU: 0.34% of visits). There was also no difference in the proportion of UCC visits for which the patients returned to the UCC within 72 hours (3.5% of visits for both pre- and post-OU).
Figure 1.
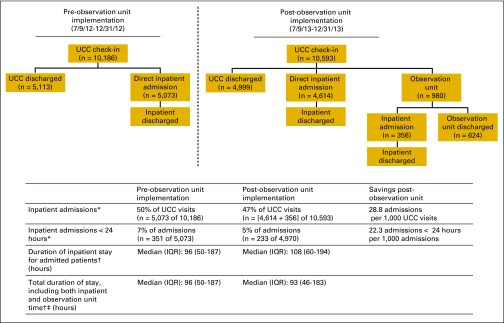
Patient flow from Urgent Care Center (UCC) check-in; includes all nonsurgical patients age ≥ 18 years who presented to the UCC. This figure maps the flow of patients from the Urgent Care Center (UCC), starting at patient check-in. Pre- and postobservation unit study periods are presented. * Statistically significant differences based on χ2 tests, pre versus post; P < .001. † Statistically significant differences based on Wilcoxon tests, pre versus post; P < .001. ‡ Accounts for patients presenting to the UCC who were admitted or seen in the observation unit.
In the study interval after OU implementation, 4,614 UCC visits (44%) resulted in a direct hospital admission, and 980 (9%) led to placement in the OU. The most common reasons for OU placement were fluid and electrolyte disorder, pain control, dyspnea, nausea and vomiting, and neurologic abnormality. Of the 980 patients placed in the OU, 36% required subsequent admission to the hospital. (Figure 1). Of the 624 patients sent home from the OU, 5% returned to the UCC within 72 hours or were subsequently admitted to the hospital. The mean length of hospital stay for the admitted group (n = 13) was 5 days.
The proportion of UCC visits resulting in an admission to the hospital was significantly lower during the post-OU implementation period compared with the pre-OU period for patients who presented with fluid and electrolyte disorders, nausea and vomiting, syncope (not statistically significant), and chest pain. Median total length of stay, including OU and inpatient time, was also lower for these subgroups in the post-OU period. (Table 2).
Table 2.
Hospital Admission and LOS Before and After Implementation of the OU for Selected Complaints
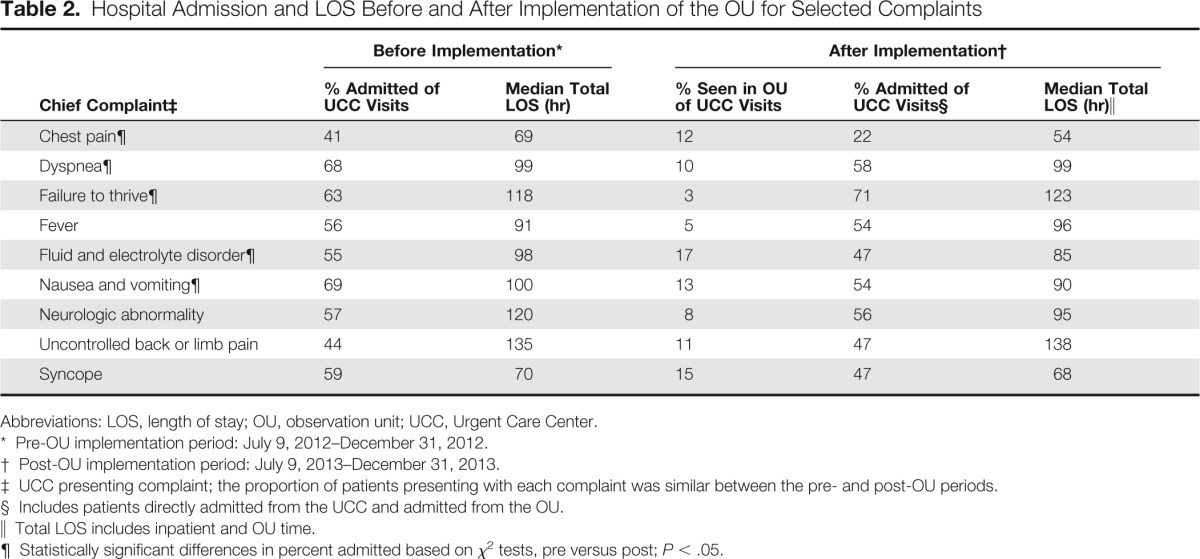
| Chief Complaint‡ | Before Implementation* |
After Implementation† |
|||
|---|---|---|---|---|---|
| % Admitted of UCC Visits | Median Total LOS (hr) | % Seen in OU of UCC Visits | % Admitted of UCC Visits§ | Median Total LOS (hr)∥ | |
| Chest pain¶ | 41 | 69 | 12 | 22 | 54 |
| Dyspnea¶ | 68 | 99 | 10 | 58 | 99 |
| Failure to thrive¶ | 63 | 118 | 3 | 71 | 123 |
| Fever | 56 | 91 | 5 | 54 | 96 |
| Fluid and electrolyte disorder¶ | 55 | 98 | 17 | 47 | 85 |
| Nausea and vomiting¶ | 69 | 100 | 13 | 54 | 90 |
| Neurologic abnormality | 57 | 120 | 8 | 56 | 95 |
| Uncontrolled back or limb pain | 44 | 135 | 11 | 47 | 138 |
| Syncope | 59 | 70 | 15 | 47 | 68 |
Abbreviations: LOS, length of stay; OU, observation unit; UCC, Urgent Care Center.
Pre-OU implementation period: July 9, 2012–December 31, 2012.
Post-OU implementation period: July 9, 2013–December 31, 2013.
UCC presenting complaint; the proportion of patients presenting with each complaint was similar between the pre- and post-OU periods.
Includes patients directly admitted from the UCC and admitted from the OU.
Total LOS includes inpatient and OU time.
Statistically significant differences in percent admitted based on χ2 tests, pre versus post; P < .05.
The proportion of admissions was higher for patients who presented with uncontrolled pain (not statistically significant) and failure to thrive. (Table 2). The subset of these patients with acute pain syndromes from readily identifiable proximate causes, such as postprocedural pain, had a higher likelihood of being discharged home from the OU.
Specific clinical scenarios with at least 75% of patient visits resulting in a successful discharge from the OU included nausea and vomiting after adjuvant or neoadjuvant chemotherapy for solid tumors, constipation refractory to outpatient treatment, hypercalcemia, and severe drug reactions.
Discussion
Findings from our evaluation of the OU impact on hospital use at a comprehensive cancer center support our hypothesis: implementation of the OU was associated with a reduction in overall hospital use for patients with cancer. They also support the notion that managing patients in the OU can be an effective alternative to inpatient care.
Compared with the pre period, during the post period we observed fewer inpatient admissions, fewer inpatient stays less than 24 hours, and shorter median total duration of stay. We observed longer duration of stays after OU implementation when we looked only at time spent in a designated inpatient bed. This finding suggests that after OU implementation, inpatient admissions were likely reserved for the sickest patients, who required lengthy stays. Of note, we observed that the implementation of the OU was not associated with prolonged hospitalization and did not lead to increases in return to the UCC. These findings temper concerns that care delivered in the OU was inferior to inpatient care. Differences in median length of stay of 3 to 12 hours in absolute terms are relatively small. However, an accumulation of savings can be meaningful to patients, staff, and hospital administrators. In particular, expediting bed turnover at times of peak hospital census is a priority for most institutions, particularly because overstressed hospitals may be at increased risk for harming patients.10
We observed different implications of the OU on hospital use for different patient subgroups. Patients with single-issue, short-term complications of cancer treatment such as dehydration and chemotherapy-induced nausea and vomiting had fewer hospital admissions post-OU implementation compared with pre-OU. Patients who presented with complaints that required further diagnostic testing before safe discharge also had fewer hospital admissions and spent less total time at the medical center post-OU implementation compared with pre-OU. This finding may reflect effective patient management in the OU. For example, individuals with neurologic complaints were placed in the OU for neurologic consultation, expedited neuro-imaging, serial examination, and evaluation for a response to therapy. Similarly, patients with chest pain, new atrial fibrillation, and hypertension were monitored in telemetered OU beds while they underwent expedited diagnostic work-up, cardiology consultation, and assessment for response to treatment.
Alternatively, patients who required management of chronic conditions such as pain control and failure to thrive had a higher proportion of hospital admissions post-OU implementation. These patients often had multiple medical and social issues that necessitated ongoing care, which frequently resulted in admission.
Similar positive impacts of observation status on hospital use have been noted in other settings and for other patient populations.1,7,11 However, to date, our understanding of the potential implications of this change in care delivery model for patients with cancer has been limited. A recent publication based on Medicare claims data noted that 2.8% of observation stays were followed immediately by a hospital admission.12 In our population, the proportion was 36%, highlighting the vast difference between patients in our study compared with those in the general population. Findings from this study demonstrate potential reductions in hospital use as a result of observation care for patients with cancer.
There were no other known changes between these time intervals that are likely to explain the differences observed. Overall, characteristics of presenting patients were similar between groups. However, we did not account for other characteristics that may have influenced our findings, such as severity of illness and patient preferences. Whether the observed changes in hospital use translate to positive health outcomes for patients and improvements in other important hospital outcomes remains unknown. There may be additional implications for patient and hospital outcomes of interest as we learn more about how to optimize the use of OUs to deliver high-quality and appropriate care for patients with cancer.
This assessment was conducted at a single institution. However, findings can provide insight into clinical scenarios in cancer care that can be effectively managed in the OU and potential implications of OU use on hospital use. This information can be useful to other institutions using or considering using observation care as an option for patients with cancer.
We observed reductions in hospital use for patients with cancer related to an OU in a comprehensive cancer center. Findings from this study support the notion that complications of cancer and cancer treatment can be successfully managed in an OU. Adoption of this approach for this patient population has the potential to reduce hospital use, which is meaningful for hospitals, payers, and patients.
Acknowledgment
Supported by Cancer Center Support Grant No. P30 CA 008748 to Memorial Sloan Kettering Cancer Center. Previously presented in part as an online abstract at the American Society of Clinical Oncology Annual Meeting, Chicago, IL, October 30-November 1, 2014.
Authors' Disclosures of Potential Conflicts of Interest
Disclosures provided by the authors are available with this article at jop.ascopubs.org.
Author Contributions
Conception and design: Allison Lipitz-Snyderman, Adam Klotz, Steven Martin, Jeffrey Groeger
Collection and assembly of data: Allison Lipitz-Snyderman, Adam Klotz, Coral L. Atoria
Data analysis and interpretation: Allison Lipitz-Snyderman, Adam Klotz, Coral L. Atoria
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Impact of Observation Status on Hospital Use for Patients With Cancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jop.ascopubs.org/site/misc/ifc.xhtml.
Allison Lipitz-Snyderman
No relationship to disclose
Adam Klotz
No relationship to disclose
Coral L. Atoria
No relationship to disclose
Steven Martin
No relationship to disclose
Jeffrey Groeger
Consulting or Advisory Role: T2 Biosystems
References
- 1.Daly S, Campbell DA, Cameron PA. Short-stay units and observation medicine: A systematic review. Med J Aust. 2003;178:559–563. doi: 10.5694/j.1326-5377.2003.tb05359.x. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Medicare & Medicaid Services. Part B hospital (including inpatient hospital Part B and OPPS). Chap. 4 in: Medicare claims processing manual [Internet], 2011. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads//clm104c04.pdf.
- 3.Wiler JL, Ross MA, Ginde AA. National study of emergency department observation services. Acad Emerg Med. 2011;18:959–965. doi: 10.1111/j.1553-2712.2011.01151.x. [DOI] [PubMed] [Google Scholar]
- 4.Baugh CW, Schuur JD. Observation care–high-value care or a cost-shifting loophole? N Engl J Med. 2013;369:302–305. doi: 10.1056/NEJMp1304493. [DOI] [PubMed] [Google Scholar]
- 5.Feng Z, Wright B, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood) 2012;31:1251–1259. doi: 10.1377/hlthaff.2012.0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sheehy AM, Graf B, Gangireddy S, et al. Hospitalized but not admitted: Characteristics of patients with “observation status” at an academic medical center. JAMA Intern Med. 2013;173:1991–1998. doi: 10.1001/jamainternmed.2013.8185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cooke MW, Higgins J, Kidd P. Use of emergency observation and assessment wards: A systematic literature review. Emerg Med J. 2003;20:138–142. doi: 10.1136/emj.20.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romero A, Brown C, Richards F, 3rd, et al. Reducing unnecessary medicare admissions: A six-state project. Prof Case Manag. 2009;14:143–150. doi: 10.1097/NCM.0b013e3181a340c4. [DOI] [PubMed] [Google Scholar]
- 9.Brooks GA, Abrams TA, Meyerhardt JA, et al. Identification of potentially avoidable hospitalizations in patients with GI cancer. J Clin Oncol. 2014;32:496–503. doi: 10.1200/JCO.2013.52.4330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pedroja AT, Blegen MA, Abravanel R, et al. The relationship between hospital systems load and patient harm. J Patient Saf. 2014;10:168–175. doi: 10.1097/PTS.0b013e31829e4f82. [DOI] [PubMed] [Google Scholar]
- 11.Baugh CW, Venkatesh AK, Hilton JA, et al. Making greater use of dedicated hospital observation units for many short-stay patients could save $3.1 billion a year. Health Aff (Millwood) 2012;31:2314–2323. doi: 10.1377/hlthaff.2011.0926. [DOI] [PubMed] [Google Scholar]
- 12.Feng Z, Jung HY, Wright B, et al. The origin and disposition of Medicare observation stays. Med Care. 2014 doi: 10.1097/MLR.0000000000000179. [DOI] [PMC free article] [PubMed] [Google Scholar]


