Abstract
Introduction:
Resources for public health (PH) are scarce and policymakers face tough decisions in determining their funding priorities. The difficulty of making these decisions is compounded by current PH accounting systems, which are ill-equipped to link fiscal resources to PH outcomes. This paper examines the types of revenues and expenditures, health services, and health outcomes that are being tracked at the local and state PH levels. The authors provide recommendations for strengthening the ability of local and state governments to link expenditures to PH outcomes, both within and across jurisdictions.
Framework and Next Steps:
The source of revenue data for most local jurisdictions is the accounting systems used for the budgeting and auditing of fiscal activities, and these are primarily linked to specific PH programs. In contrast, expenditure data are mostly generic and typically span multiple PH programs with no link to specific PH activities. Many challenges exist to then link PH activities to health outcomes data, which are often collected through separate reporting systems at the local, state, and national levels. Policy change at the state level and implementation strategies that are standardized across local health departments are required to assess the costs and health outcomes of PH activities.
Conclusion:
Information linking PH expenditures to health outcomes of PH services could greatly inform the decision-making process. This information will allow investments in PH to be better understood and will provide a strong foundation for the PH services and systems research community to understand variation and drive improvement. Ultimately, these data could be used to improve accountability at the local and state PH department levels.
Keywords: population health, finance, value/cost
Introduction
Based on the 2011 Institute of Medicine (IOM) report For the Public’s Health: Investing in a Healthier Future,1 a logic model for linking costs to health outcomes for informing investment in public health (PH) is as follows:
Figure 1.
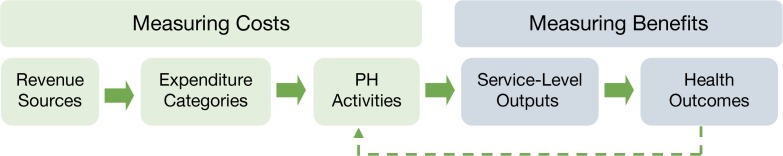
Logic Model for Linking Costs to Health Outcomes*
Note: *Adapted from the 2011 Institute of Medicine report: For the Public’s Health: Investing in a Healthier Future.1
The first three components of this logic model—Revenue Sources, Expenditure Categories, and PH Activities—are considered when measuring the costs of PH investments; the last two components—Service-level Outputs and Health Outcomes—are considered when measuring the benefits of PH investments.
The source of revenue data for most local jurisdictions is the accounting systems used for the budgeting and auditing of fiscal activities, and these are primarily linked to specific PH programs. In contrast, expenditure data are mostly generic and typically span multiple PH programs. Health outcomes data, on the other hand, are often collected through separate reporting systems at the local, state, and national levels. As a result, revenues, expenditures, and health outcomes lack a ”common language.” For example, from 1970 to 1995, state health department expenditure data were reported by revenue source and by major program areas (e.g., personal health, environmental health, laboratory, etc.) as part of a broader information collection system called the Association of State and Territorial Health Officials (ASTHO) Reporting System.2 The revenue sources included a uniform list of federal (Centers for Disease Control and Prevention, Health Resources and Services Administration, Medicare, Medicaid, etc.) and nonfederal (state general funds, fines, fees, etc.) entities. Program areas were solicited from each state health department on an annual basis, which created a comprehensive inventory of programs offering enough flexibility to accommodate the various organizational and reporting structures of health departments across different states. This flexibility was also its biggest downfall as it may not be accurate to directly compare financial data across states. For example, while some state health departments may report hypertension-screening clinics as a separate PH program, others may include hypertension-screening services within a broader chronic disease program. Such inconsistencies hinder a state-by-state comparison of revenues, expenditures, and PH activities. The federal government in 1995 eliminated funding for the ASTHO Reporting System and there has been no standardized replacement to report revenue sources and expenditures.2
Ideally, health outcomes should inform future PH activities, as shown in the IOM logic model. However, this feedback loop is complicated by the fact that a standardized nomenclature for PH activities may not exist among various local health departments (LHDs) within a state. For example, a 2002 survey of New York counties found a high level of variance in what counties defined as PH services.3 Such inconsistencies make it difficult to tie health outcomes to specific PH activities.
Policy change from above (e.g., regulations that mandate standardized reporting) and implementation strategies that are standardized from below (e.g., LHDs) are required to assess the costs of PH activities. In the following sections, we provide a detailed discussion of local data sources on costs and outcomes. The barriers inherent in the data and recommendations for linking costs to health outcomes in PH are addressed. Adopting a common language and understanding the form and content of data available at the local level for PH finance will make it easier for PH advocates to provide rigorous information to policymakers to drive efficient allocation of scarce PH resources.
Cost Data
Cost data for essential PH services and activities are typically derived from accounting systems, which provide information on revenue sources and expenditure categories. While appropriate for the budgeting and auditing of state and local fiscal activities, these systems are not designed to link costs to health outcomes or to make comparisons across time and jurisdiction. For example, accounting systems may not be uniform either across state lines or within state jurisdictions, the types of data being reported in the accounting systems may differ or the definitions of categories may vary.
Revenue Sources
LHDs receive revenue from a variety of local, state, and federal sources as outlined in Table 1. Standard definitions across and between jurisdictions are critical for comparability. Further, linking revenue source to expenditure category and PH activity may be challenging because many of these revenue sources have restrictions on how the funds can be used. For example, there may be some state funds that are restricted to maintaining infrastructure, such as facilities, and are not for the purchase of equipment. Alternatively, some federal funds are restricted to specific programs such as money received from the Medicaid program for perinatal services. Another barrier to tracking revenue sources is consideration of funds that are locally managed, such as reserve funds that may roll over from year to year. These funds are critical for LHDs that may experience shortfalls in revenue from state or federal sources. However, the funds may not be tracked in statewide systems—making it difficult to link to expenditures, activities, outputs, and health outcomes.
Table 1.
Example of Typical Revenue Sources in a Local PH Accounting System
| Local Revenue Sources | |
| County | Funds received from the county, including the local county match |
| Municipal | Funds received from city or other local government |
| Intra- and interagency | Funds received from other county health departments within the health district |
| Outpatient client fees | Client fees collected that do not fall into another specific category |
| Environmental fees | Current fees for environmental services |
| Vital records | Current fees collected for birth certificates, death certificates |
| Medicaid client co-pay | Payment amount collected form patients for Medicaid services requiring a co-pay |
| State Revenue Sources | |
| General grant-in-aid | Funding received from the state health department |
| Federal Revenue Sources | |
| Medicaid case management | Current Medicaid funds for case management |
| Medicaid perinatal services | Current Medicaid funds received under Medicaid Pregnancy Related Services |
| Outpatient Medicare | Current fees from Medicare |
| Nonqualifying contracts | Contracts with outside agencies not qualifying as match for administrative claiming |
Additionally, many PH services are delivered through partners such as community centers and hospitals. Often these services receive contributions from private entities, nonprofit foundations, and local charities, and are likely not in LHD accounting systems. For example, a survey of PH partners in New Hampshire collected information on expenditures for 10 PH service categories, where revenue data were categorized as direct federal funds, donations, foundations, non-PH state funds, and other revenue. The authors noted several limitations to this approach including the identification of PH partners that had an impact on PH services, the spillover of PH services between jurisdictions, adjusting for differences in fiscal year definitions, and a lack of validation of financial data obtained from PH partners. Survey results showed that in 2010, local PH partners spent $19.5 million on PH services out of which $10 million did not have “a discernible link to government money.”4
Expenditure Categories
In many PH accounting systems, data on PH expenditures are classified into a large number of individual categories that fall into three broad expenditure categories as shown in Table 2. For the decision maker to leverage appropriate funding sources, revenue sources must be linked to expenditure categories. For example, in the event of an epidemic, it would be useful to know how local fees collected for immunizations were tied to pharmaceutical purchases.
Table 2.
Examples of Typical Expenditure Categories in a PH Accounting System
| Personnel | Salaries Local salary supplement Hourly labor FICA |
Retirement Health insurance Personal liability insurance |
| Equipment | Motor vehicle equipment purchases Equipment <$5,000 Lease purchase |
Rental of equipment purchases Equipment ($5,000+) Computer equipment |
| Operating Expenses | Motor vehicle expenses Supplies and materials Pharmaceuticals Repairs and maintenance Utilities Travel Building rent Per diem and fees Contracts |
Printing Rents other than real estate Insurance and bonding Other operating expenses Computer software Telecommunication Postage Indirect costs |
However, most accounting systems only allow for aggregate revenue to be tied to aggregate expenditure within a single reporting period, and it is often not possible to tie a specific revenue source to a specific expenditure category. For example, an LHD’s accounting system may provide data on the expenditures for personnel within a specific period (e.g., annually) and show that a certain proportion of revenue is from federal sources. However, that accounting system may not allow the LHD to determine what proportion of federal revenue is tied specifically to personnel, equipment, or operating expenditures, which may be the most relevant source of data needed to make an accurate comparison.
A number of attempts have been made to standardize and condense expenditure categories and align them with revenue sources and PH activities. For example, in 2004 the Georgia Division of Public Health, motivated by a desire to negotiate cost-based reimbursements from Medicaid, made an effort to separate all major activities of PH services into ”cost centers” such as clinical, population-based, and environmental services; general administration; and all other activities.5 Current Procedural Terminology (CPT) codes were applied to clinical PH services regardless of whether or not they were billable, and codes were applied to common PH services offered at the county level. Expenditures were labeled by their respective cost centers. For example, any expense that supported clinical activities (e.g., paper for an exam table) was applied to the clinical cost center. A statewide implementation of this standardized costing methodology resulted in the generation of a credible cost report by county, which allowed for comparisons between program costs and revenue sources across LHDs.
In our own research, we have been prospectively evaluating a seven-year phased-in implementation of Georgia’s new formula for allocating state PH infrastructure funding to all LHDs (one in each county in Georgia), providing a natural experiment to evaluate the impact of revenues on expenditures, services, and health outcomes across the state. Prior to fiscal year (FY) 2012, General Grant-In-Aid (GGIA), which is funding from the state to counties, was based on population data from the 1970 census and a county’s percent share of the state’s tax base. The new GGIA funding formula includes poverty rates and county population estimates but no longer includes the share of the state’s tax base. GGIA is being phased in over a seven-year period (FY2012– FY2018) such that 15 percent of the change is included every year for six years, with the remaining 10 percent included in the final year. This phase-in period allows health departments that are losing funding based on the new formula to adjust their budgets gradually to this reduction.
To estimate the impact of changes in GGIA revenue at the county level, while controlling for changes in other revenue streams, a series of cross-sectional regression analyses were performed for the per capita change in revenues and expenditures for the first two years of formula funding change, from FY2011 to FY2012 and from FY2012 to FY2013, separately. Separate regressions were conducted with each per capita change in expenditure serving as the dependent variable and the per capita change in revenues as independent variables.
For the regression analysis of the change in FY2011 to FY2012 per capita revenues and expenditures reported in Table 3, GGIA revenue was positively and significantly associated with personnel, operating, and equipment expenses; but note that operating expenditures were not significantly associated with any other revenue category. These results indicate that for each additional dollar received through GGIA, on average $0.79 was spent on operating expenses and $0.25 on personnel expenses, with a small decrease in expenditures on equipment.
Table 3.
Results of Regressions of Revenue Sources on Each Expenditure Category for Change in Per Capita Revenue and Expenditures, FY2011 to FY2012 (N=157)
| Expenditures | Personnel | Operating Expenses | Equipment | |||
|---|---|---|---|---|---|---|
| Revenues | Coef | p-value | Coef | p-value | Coef | p-value |
| GGIA* | 0.25 | 0.046 | 0.79 | <0.001 | −0.06 | 0.007 |
| Local | 1.04 | <0.001 | −0.07 | 0.231 | 0.03 | 0.019 |
| Federal | 1.22 | <0.001 | −0.22 | 0.107 | 0.00 | 0.862 |
| Fees | 0.78 | <0.001 | 0.14 | 0.154 | 0.07 | <0.001 |
| Other | 1.08 | <0.001 | −0.05 | 0.737 | −0.03 | 0.364 |
Statistically significant coefficients for GGIA are in bold font.
The results of the regression analyses of the change in per capita revenues and expenditures for FY2012 to FY2013 are reported in Table 4. GGIA revenue was positively and significantly associated with personnel expenditures only; yet, the association was similarly found with all other revenue sources. These results indicate that on average for each additional dollar received through GGIA, nearly all were spent on personnel expenses. The next step in this research is to estimate the impact of expenditure changes on PH activities (and eventually to lagged effects in health outcomes).
Table 4.
Results of Regressions of Revenue Sources on Each Expenditure Category for Change in Per Capita Revenue and Expenditures, FY2012 to FY2013 (N=157)
| Expenditures | Personnel | Operating Expenses | Equipment | |||
|---|---|---|---|---|---|---|
| Revenues | Coef | p-value | Coef | p-value | Coef | p-value |
| GGIA* | 1.07 | <0.001 | −0.07 | 0.571 | 0.00 | 0.935 |
| Local | 0.64 | <0.001 | 0.33 | <0.001 | 0.03 | 0.076 |
| Federal | 0.98 | <0.001 | 0.05 | 0.754 | −0.03 | 0.477 |
| Fees | 0.72 | <0.001 | 0.24 | 0.008 | 0.04 | 0.059 |
| Other | −0.08 | 0.834 | 0.97 | 0.010 | 0.11 | 0.248 |
Statistically significant coefficients for GGIA are in bold font.
Expenditures: Public Health Activities
Despite the value of these data to understand the impact of cost on outcomes, linking expenditures to PH activities may not be that easy for many LHDs. For example, although an accounting system may report that 40 percent of an LHD’s budget is devoted to personnel expenditures, the accounting system may not show an allocation of these expenditures to PH programs or activities. PH agencies need effective management systems, not accounting systems, for tracking personnel time allocation by activity level and for those activities that are considered core capacity functions. For example, drawing from the IOM’s report,1 PH agencies need a chart of accounts to better track funding related to programmatic outputs and health outcomes (IOM report Recommendation 5). These accounts need to include information on how resources are allocated to key expenditures, which are then tied to PH activities.
Further, activities need to be separately defined as those that are programmatic (e.g., restaurant inspections) versus those that are core capacity functions (e.g., surveillance)—following Recommendation 3 of the IOM report. Activities may also be defined as the 10 essential services covered by PH.6 Activities need to be further defined as those that serve populations (e.g., restaurant inspections) and those that serve individuals (e.g., well-baby checkups), or both (e.g., immunizations). In other words, expenditures need to be tied to macro-level administrative and operational functions and to micro-level programs.
One purpose for moving from an accounting to a management system for tracking expenditures to activities is to develop a performance-based financial reporting framework. Reporting methodology developed by the National Association of State Budget Officers (NASBO) and the Reforming States Group (RSG) can be used as a template for the collation of PH expenditures around activities and populations.7,8 A slightly modified version of the NASBO and RSG template was field tested in two PH districts in Georgia.9 Each of the more than 400 program expenditure accounts were linked to the modified NASBO and RSG categories and were cross-coded by revenue source. Results from a five-year retrospective analysis of expenditure data indicated variations in PH investment patterns that were specific to each PH district. For example, one PH district showed a spike in PH infrastructure investment in FY2002 whereas the other district showed an increase in disaster-preparedness activities in FY2004. This experiment illustrates that it is indeed possible to connect PH expenditures to PH activities in ways that reflect programmatic priorities at the local level.
The Georgia local PH cost study5 provides further guidance on how to capture PH activities at the local level. For one week every quarter, PH staff designated their weekly PH activities to the respective cost centers described in the previous section. A different workweek was selected for each successive quarter. A task analysis was then performed to reveal which PH activities were conducted during a “typical” month. Although this method of connecting PH activities to expenditures was ultimately not adopted, it speaks to the potential of developing a standardized system for capturing PH activities at the LHD level.
There have also been several cohort studies that have assessed the correlation between revenue sources and expenditures for certain PH activities.3,10–15 For example, one study12 investigated the correlation between revenue source and local expenditures for the 10 essential services6 covered by local PH systems. While this study did not include the expenditure categories required to implement the services, it did provide some important information on the link between funding source and activity. Using data from 50 LHDs, the authors found that local revenue was significantly correlated to the development of policies, enforcement of laws, and training of the workforce. Taxes per capita were associated with 6 essential PH services including surveillance, disease investigation, development of policies, enforcement of laws, training the workforce, and research, while total expenditures were correlated with the development of policies and enforcement of laws. Expenditures per capita were not significantly correlated with any of the essential PH services. This suggests that the definition of the underlying population for assessing PH impact is critical to understanding the impact the local PH may have on the community, and that the population may need to be more narrowly defined (socioeconomic status, age, education, access to health care, etc.).
Outcome Data
Service-Level Output Data
Output data are frequently collected at the local level and include items such as the number of immunizations or the number of restaurant inspections. For many programmatic activities funded by federal sources, collection and reporting of these output data is required, yet the reporting may or may not be aggregated by the state. For the linkage of costs to health outcomes, costs by capacity and activity should be linked to process level variables or outputs. It is important to assess the costs per the unit of output under consideration, for example, the costs (by expenditure category) per person served, patient seen, restaurant inspected, or school visited. While the explicit linkage of expenditure category or activity-level costs to outputs at the person level is ideal, this information can be derived implicitly by comparing aggregate-level activity costs to aggregate output data to derive per unit costs.
There may also be exogenous factors that need to be accounted for when linking costs to outputs. For example, in the case of epidemics, like H1N1, the number of immunizations may rise dramatically during those periods, while the resources remain constant. A good management system that links expenditure categories to activities to outputs would allow a local jurisdiction to account for a shift in resources from one activity to another during an epidemic or other emergency.
Outcome Data
To provide information to policymakers on the most efficient allocation of scarce PH resources, output data need to be linked to short-, intermediate- and long-term health outcomes. Data on health outcomes, or health impacts, are frequently collected and aggregated at the state or federal levels, with some ability to estimate health outcomes at the local level. A logic model, which provides a graphic representation of complex linkages between resources and output data, can assist in showing the linkages from short- to intermediate- to long-term health outcomes that LHDs hope to achieve with programmatic and core activities.
However, there are a number of challenges in conducting research or finding data that informs those aforementioned linkages. First, health outcomes may be impacted years beyond the investment in PH. For example, a childhood immunization program may have demonstrable effects within a short time frame, while a prevention program targeting childhood obesity may have effects over a longer time horizon. Second, within the hierarchy of short- to long-term health outcomes, primary data may not be available on long-term health outcomes and additional epidemiologic efforts may be needed to develop models of activity effectiveness. In many cases, longitudinal data are not available to assess the long-term impact of PH interventions. Third, there should be some standardization of how rates of the outcomes are defined. For example, if the outcome is breast cancer screening rates, the denominator could include all women or all women over age 50 per the Guide to Clinical Preventive Services. Finally, when assessing PH impact it is important to consider the community-level variables that are known to influence the public’s health, such as poverty level, number of uninsured, educational attainment, percent of population ages 65 years and older, and access to health care due to recent state-level expansions of Medicaid.
Another consideration is defining the health outcomes that we, as a society, expect PH to have an impact on. For example, some studies that have tied local PH expenditures to health outcomes have reported mortality rates for the overall population and then specifically to cardiovascular disease (CVD), heart disease, unintentional injury, and years of potential life lost. Are these health outcomes that PH alone should be expected to have an impact on? If so, much of what is done in PH is part of a public-private partnership to improve population-level health. Then, either the cost to outcome link needs to include the non-PH costs in the logic model (from nonprofit health organizations, hospitals providing uncompensated care, and free health care clinics), or the health outcomes included in the model must be narrowly defined as under the purview of PH, and of PH alone.
Summary and Discussion
The way a state or local PH agency defines its system and role in the community—including related government agencies, employers, schools, the medical community, the philanthropic community, etc.—should be a fundamental driver of approaches to measuring costs and benefits, and in turn, these analyses should drive how scarce resources should be allocated. For example, one study16 assessed the impact of other community spending on spending by local PH agencies across the United States as a means for determining how the system overall works to tackle PH issues. The authors found that local PH spending was inversely associated with local-area medical spending, and that medical care resources varied inversely with the level of PH agency spending. The next natural step in this research is to assess the costs of local PH spending and local-area medical spending as it relates to local PH outputs and health outcomes.
As noted in this paper, local variation in data collection in PH programs requires policy change from above as well as implementation strategies that are standardized at the local level, like the chart of accounts as a first step. Honoré and others have made important recommendations for standardizing the PH financial management part of the logic model, such as uniform expense and revenue classifications, electronic reporting of standard data, standard financial analysis practices, and the PH chart of accounts.14,17–21
Standardized cost and financing data can be used for true comparisons of services and efficiency across PH departments, districts, states, and regions of the country, including historical trend analyses for assessment of financial status. In addition to the standardized financial management, uniform coding of PH activities and an ability to track PH expenditures to these activities through appropriate management systems are also critical. Combined, our investment in PH will be better understood and will provide a stronger base of data for the PH services and systems research community to use to understand variation and drive improvement. From there, we believe the priority should be moving toward valuing the health care system in general, of which PH is only one part. Ultimately, these data could be used to hold the system accountable for health outcomes, rather than focusing accountability on local and state PH departments. We want to know eventually how the unique public-private partnerships have an impact on important population-level health outcomes. For example, how do the resources provided by PH complement the health care resources provided by hospitals and other nongovernmental entities? This understanding will only begin when we have a better sense of cost and outcome data being tracked at the local and state PH levels that are both standardized and linked, both within and across jurisdictions.
Acknowledgments
We would like to acknowledge AcademyHealth and the Robert Wood Johnson Foundation for commissioning this paper.
Key Terms
- Benefits:
Improvements in health outcomes as a result of PH investments or activities.
- Benefit-cost analysis (BCA):
Analysis that quantitatively compares a program, policy, or system’s benefits in monetary terms to its costs in monetary terms, from a societal perspective and using an analytic horizon long enough to quantify all costs and benefits.
- Costs:
Monetary funds needed to deliver core PH services and programmatic activities.
- Expenditure categories:
Monetary funds, grouped by category (e.g., personnel, space, equipment, materials and supplies, etc.), that directly or indirectly support PH activities.
- Health outcomes:
Results of PH activities and investments that can be measured in terms of morbidity and mortality; for example, reduction in teenage pregnancies, obesity rates, etc.
- Public health (PH) activities:
Services provided by PH systems (e.g., monitoring health status, conducting surveillance, investigations or interventions of disease and injury, enforcing laws and regulations that protect health and ensure safety, etc.).
- Revenue data:
Monetary funds received by PH agencies at the local and state levels from governmental and nongovernmental sources.
References
- 1.Institute of Medicine. For the public’s health: investing in a healthier future. Washington, DC: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 2.Barry M, Bialek R. Tracking our investments in public health: what have we learned? J Public Health Manag Pract. 2004;10(5):383–392. doi: 10.1097/00124784-200409000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Leviss PS, Novick LF. Examining public health financing in New York state: a methodology for evaluating local and national public health data. J Public Health Manag Pract. 2004;10(5):393–399. doi: 10.1097/00124784-200409000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Bernet PM. Assessing the level of public health partner spending using the funding formula analysis tool. J Public Health Manag Pract. 2012;18(4):339–345. doi: 10.1097/PHH.0b013e31823f2703. [DOI] [PubMed] [Google Scholar]
- 5.Hadley CL, Feldman L, Toomey KE. Local public health cost study in Georgia. J Public Health Manag Pract. 2004;10(5):400–405. doi: 10.1097/00124784-200409000-00005. [DOI] [PubMed] [Google Scholar]
- 6.National Public Health Performance Standards. The public health system and the 10 essential public health services [Internet] Centers for Disease Control and Prevention; 2013. [Updated 2013 July 3; cited 2014 March 4]. Available from: http://www.cdc.gov/nphpsp/essentialservices.html. [Google Scholar]
- 7.2002–2003 State health expenditure report. New York: National Association of State Budget Officers, The Reforming States Group, and Milbank Memorial Fund; 2005. [Google Scholar]
- 8.2000–2001 State health care expenditure report. New York: National Association of State Budget Officers, The Reforming States Group, and Milbank Memorial Fund; 2003. [Google Scholar]
- 9.Hepburn VA, Eger R, Kim J, Slade C. Structuring a framework for public health performance-based budgeting: a Georgia case study. J Public Health Manag Pract. 2007;12(2):173–179. doi: 10.1097/00124784-200703000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Gordon RL, Gerzoff RB, Richards TB. Determinants of US local health department expenditures, 1992 through 1993. Am J Public Health. 1997;87(1):91–95. doi: 10.2105/ajph.87.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Honoré PA, Fos PJ, Wang X, Moonesinghe R. The effects on population health status of using dedicated property taxes to fund local public health agencies. BMC Public Health. 2011;11(1):471. doi: 10.1186/1471-2458-11-471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Honoré PA, Simoes EJ, Jones WJ, Moonesinghe R. Practices in public health finance: an investigation of jurisdiction funding patterns and performance. J Public Health Manag Pract. 2004;10(5):444–450. doi: 10.1097/00124784-200409000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Leider JP. The problem with estimating public health spending. J Public Health Manag Pract. 2013 doi: 10.1097/PHH.0b013e3182941a7b. [DOI] [PubMed] [Google Scholar]
- 14.Leider JP, Sellers K, Shah G, Pearsol J, Jarris PE. Public health spending in 2008: on the challenge of integrating PHSSR data sets and the need for harmonization. J Public Health Manag Pract. 2012;18(4):355–363. doi: 10.1097/PHH.0b013e31824c60d7. [DOI] [PubMed] [Google Scholar]
- 15.Santerre RE. Jurisdiction size and local public health spending. Health Serv Res. 2009;44(6):2148–2166. doi: 10.1111/j.1475-6773.2009.01006.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mays GP, Smith SA. Geographic variation in public health spending: correlates and consequences. Health Serv Res. 2009;44(5p2):1796–1817. doi: 10.1111/j.1475-6773.2009.01014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Costich JF, Honoré PA, Scutchfield FD. Public health financial management needs: report of a national survey. J Public Health Manag Pract. 2009;15(4):307–310. doi: 10.1097/PHH.0b013e31819b2c78. [DOI] [PubMed] [Google Scholar]
- 18.Getzen TE. Advancing public health finance. J Public Health Manag Pract. 2007;13(2):225–226. doi: 10.1097/00124784-200703000-00023. [DOI] [PubMed] [Google Scholar]
- 19.Gillespie KN, Kurz RS, McBride T, Schmitz HH. Competencies for public health finance: an initial assessment and recommendations. J Public Health Manag Pract. 2004;10(5):458–466. doi: 10.1097/00124784-200409000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Honoré PA, Clarke RL, Mead DM, Menditto SM. Creating financial transparency in public health: examining best practices of system partners. J Public Health Manag Pract. 2007;13(2):121–129. doi: 10.1097/00124784-200703000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Honoré PA, Costich JF. Public health financial management competencies. J Public Health Manag Pract. 2009;15(4):311–318. doi: 10.1097/PHH.0b013e31819c1308. [DOI] [PubMed] [Google Scholar]


