Abstract
Electronic health information systems can reshape the practice of public health including public health surveillance, disease and injury investigation and control, decision making, quality assurance, and policy development. While these opportunities are potentially transformative, and the federal program for the Meaningful Use (MU) of electronic health records (EHRs) has included important public health components, significant barriers remain. Unlike incentives in the clinical care system, scant funding is available to public health departments to develop the necessary information infrastructure and workforce capacity to capitalize on EHRs, personal health records, or Big Data. Current EHR systems are primarily built to serve clinical systems and practice rather than being structured for public health use. In addition, there are policy issues concerning how broadly the data can be used by public health officials. As these issues are resolved and workable solutions emerge, they should yield a more efficient and effective public health system.
Keywords: Informatics, EDM Forum, Public Health, Epidemiology, Surveillance, Quality Improvement, Quality Assurance, Policy, Electronic Medical Record, Electronic Health Record, Meaningful Use, Electronic Clinical Data, Electronic Lab Reporting
Introduction
Public health depends on a robust information base to carry out its primary tasks of assessment, policy development and assurance.1 Reliable, timely data are needed perhaps most evidently in response to infectious disease and other acute events. Historically, public health surveillance has relied on telephone and mail, and more recently online, completion of notifiable disease reports and access to electronic laboratory reporting (ELR). However, several new types of health information technology (HIT) may play an important role in support of public health in the near future, including: electronic health records (EHRs), personal health records (PHR), health information exchange (HIE), clinical decision support (CDS), and Big Data analytics. Each technology has potential benefits, as well as significant barriers to use.
This HIT is seen as central to achieving the “Triple Aim” of health-care reform: “improving the individual experience of care; improving the health of populations; and reducing the per capita costs of care for populations.”2 Ready access to data at the point of care supports clinical decision making that benefits the individual patient, and that same access to data is required to support agencies making decisions that have an impact on the health of populations. For example, public health could quickly assess the completeness of immunizations, understand which populations remain underimmunized, initiate action to understand the reasons, and take action targeted at clinical care systems, physicians, or patients as the need requires.3
Similarly, the availability of electronic clinical information on cases and their management will greatly enhance the ability to improve the quality of traditional public health services. While most communicable disease services are currently provided outside of public health clinics, public health remains responsible for investigation, contact tracing and management, relying on laboratory and passive physician reporting to assure cases are referred. More efficient and more rapid transmission of medical data can lead to more rapid identification of patients, simplify identification of clusters, facilitate contact tracing and patient or professional education and other initiatives. The data can be used to identify gaps in quality of care, such as failure to follow recommended guidelines or inadequate follow up and treatment.
The advent of widely available electronic health information and Big Data, the massive amount of data produced each day, also provides new opportunities to understand social interactions, environmental and social determinants of health and the impact of those environments on individuals. The powerful analytic tools that have been applied to marketing and other fields are not commonly present in public health departments, but implementing them has the potential to fundamentally change surveillance and other systems. By the same token, technology puts information into the hands of users who can use it to drive community change. Making data readily available – with appropriate protections, of course – can empower stakeholders in ways that one can now only imagine.
We are also at the cusp of major change as public health roles become more demanding and are being reshaped by the Affordable Care Act (ACA). As more people have insurance coverage, the need for public health to deliver clinical services will diminish substantially with a residual function for those who remain without access to the mainstream clinical care system. What will not diminish, however, is the public health responsibility to control certain clinical conditions.
This system transformation signals great opportunity for the integration of public health and health care through public health informatics. Indeed, public health informatics can support “the triple aim of achieving a public health goal faster, better, or at a lower cost by leveraging computer science, information science, or technology.”4 The Los Angeles County Department of Public Health has begun this journey and has a well-developed ELR system for notifiable diseases. However, it foresees the need to rapidly expand its capability to use emerging HIEs to access those data. Unlike the incentives available to the clinical care system for developing MU capabilities, public health has few resources to develop its information technology infrastructure and ability to analyze and use those data efficiently and effectively. This article provides some insights into the practical impacts of the burgeoning electronic systems on public health departments.
Current and Emerging Uses of Electronic Health Information
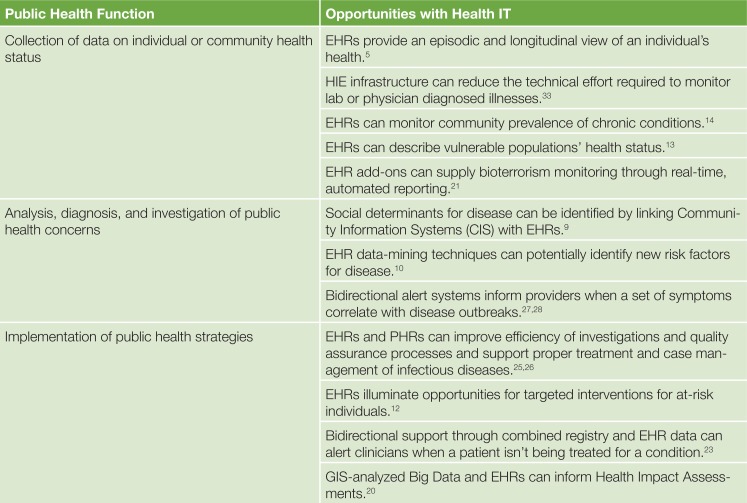
Electronic health information can potentially improve many of the core functions in public health (See Figure 1).
Figure 1:
Summary of Public Health Opportunities Utilizing HIT
Data Collection
Public health agencies monitor the health status of populations, collecting and analyzing data on morbidity, mortality and the predictors of health status, such as socioeconomic status and educational level. There is a particular focus on diseases of public health importance, the needs of vulnerable populations and health disparities. An EHR provides both episodic snapshots and a longitudinal view of a patient’s health related to clinical care. A PHR provides a powerful tool for gathering information about clinical visits, as providers and patients use the application to access, manage and share health information.5 A survey of PHR users identified a willingness to share their data for care improvement and public health purposes.6
The use of EHR data to support public health surveillance and epidemiology has been demonstrated for a wide range of conditions, including respiratory diseases, cancer, and even social determinants for disease.7,8,9 The use of data mining and analytic techniques on EHR data has the potential to identify new risk factors and target interventions at the individual level.10,11 For example, a health system’s EHR was used to identify smokers for tobacco dependence interventions.12
EHRs can provide data on subpopulations, geographic areas and health conditions that are typically underrepresented in public health surveillance and large-scale surveys, most often conducted at the federal or state level. For example EHR data from a county clinic serving children in foster care was used to describe the health status of this vulnerable population.13 The NYC Macroscope project launched “a population health surveillance system that uses electronic health records (EHRs) to track conditions managed by primary care practices that are important to public health,” whereby they monitor the community prevalence of “chronic conditions, such as obesity, diabetes and hypertension, as well as smoking rates and flu vaccine uptake.”14
The combination of EHR data and geographic information system (GIS) technology has the potential to provide for selective sampling of demographic groups or geographic communities and can be used to understand patterns of illness and delivery of care at the community level.15,16 Cancer epidemiology has prioritized the use of Big Data, and genomics has used it to identify genetic risk factors for common diseases and mutations that confer a high risk for rare conditions.17,18 Big Data facilitates more drilling down (viewing more detail), drilling up (viewing data in aggregate), and slicing-and-dicing (viewing specific combinations of data variables) than may be reasonable with traditional data collection and desktop-based analysis.19
Many public health departments are pursuing a health-in-all-policies approach to assure that health is a consideration in all major policy decisions. These might include developing new housing, factories, transportation systems, recreation facilities, or educational initiatives to increase graduation rates. Health impact assessments play a critical role in informing decision makers about how their decisions can be used to maximize health and mitigate harms.20 Using GIS to look at both Big Data and EHR data may support the detailed knowledge of risk groups, behaviors, social and physical environments needed for both epidemiology and comprehensive policy evaluation such as health impact assessments.
Analysis, Diagnosis, and Investigation of Public Health Concerns
Public health authorities are required to drill down for individual data and risk factors in order to diagnose, investigate and control disease and health hazards in the community, including disease that originates with social-, environmental-, occupational- and communicable-disease exposures. The community relies on public health to control exposure across jurisdictions and sectors, which may involve closing a school or business, isolating infectious individuals, or limiting exposures to health hazards. For example, a clinician or laboratory reports a case of active tuberculosis to the local health department. In response, public health staff performs chart reviews and patient interviews to identify exposed community members and immediately ensure appropriate precautions. For the next year they ensure that all affected patients receive appropriate care and case management. They may provide direct clinical services, expert consultation for drug-resistant and other challenging cases, or they may provide oversight of private sector care, to ensure an appropriate treatment regimen and patient adherence.
This process is resource intensive and time-consuming for both the public health department and clinicians, which can lead to a suboptimal response and public health control measures. Access to EHR data can improve the efficiency of both the investigation and quality assurance process, because health department staff no longer must travel to multiple sites, manually abstract data from multiple electronic medical records (EMRs), or reenter abstracted data into an electronic public health information system. EHR data may offer a more longitudinal, complete and accurate information than a onetime interview with a patient. Data obtained from a PHR may offer data that is different in content or time frame, and it might also offer information on patients that have not had a clinical visit.
Bioterrorism events and outbreaks such as bacterial meningitis and pandemic influenza demand a rapid public health response that only timely access to clinical data can guide. EHR add-on technologies have been developed specifically to support real-time, automated reporting of notifiable diseases, influenza-like illness, and diabetes prevalence to health departments.21 The efficiency of the public health response can also be improved when clinicians receive public health information in a timely way. Efforts to support bidirectional communication that integrates public health information and interventions at the point of care have been encouraged and might include information about patients followed by the public health agency (PHA), communicable disease outbreaks and control, environmental exposures, medication and product recalls.22
Implementation of Public Health Strategies
Several pilot studies have demonstrated the promise of bidirectional HIE to support efficient surveillance and public health interventions, including linking patients to care and assuring the quality of clinical care. The Louisiana State University Hospital System and the Louisiana Office of Public Health implemented a bidirectional data exchange to link HIV-positive patients not currently receiving HIV treatment to appropriate medical care.23 By matching hospital registration data with the local health department’s HIV/AIDS registry, the authors were able to alert physicians that a presenting patient was not currently receiving HIV treatment. The median time between the patient’s last medical visit and the alert was 20 months. More than 70% of alerts issued were followed by a documented action by the provider, helping to assure appropriate patient care.
This example of bidirectional communication provided person-specific, context-sensitive knowledge that supported both health-related decision making and action by healthcare providers, assuring high-quality clinical care and an effective and efficient public health intervention using CDS. More than merely providing information, CDS tools and processes can include automated reminders and alerts, condition-specific order sets, data reports and visualizations, clinical guidelines and evidence-based references.24 CDS is generally available as an embedded function of an EHR at the point of care; less commonly, CDS is provided through an EHR as an HIE service or to an individual via a PHR. CDS supports quality assurance efforts in that it facilitates high-quality clinical care that helps ensure a timely and effective public health response benefitting both the individual patient and the community.25,26
The Institute for Family Health in New York City used advisory statements from the local health department to create alerts within their EHR system, prompting appropriate laboratory testing during foodborne disease outbreaks and appropriate testing and treatment during a local Legionella outbreak.27,28 The alert was triggered by symptoms such as cough, chest pain, fever, chest congestion or cold symptoms, and the management guidance included information on diagnosis, testing and treatment. A prepared order set “included orders for sputum culture, Legionella urine antigen, chest x-ray, and complete blood count, as well as outpatient antibiotic prescriptions appropriate for community acquired pneumonia.”
Bidirectional communication via a PHR or a SMART (“Substitutable Medical Applications, Reusable Technologies”) application for a mobile device may also offer CDS to guide individual patient action or provide data for population surveillance and investigation via HIE services.29,30 PHR communications outside of clinical visits can link patients to appropriate care and exposure precautions. For example, perinatal Hepatitis B cases require lengthy oversight for to ensure that both patients receive appropriate care. Communications and oversight can be cumbersome, as mothers and their babies are often cared for in different health systems by different clinicians and covered by different health insurance plans. The combination of EHR and PHR technology could make this quality assurance activity much more efficient and timely for health departments.
Opportunities: Improvements in Infrastructure
The application of electronic health information in public health is supporting the increased adoption of EHRs by the medical community, the inclusion of required public health reporting within the Centers for Medicare and Medicaid Services (CMS) incentives for EHR adoption, and the national infrastructure for HIE.
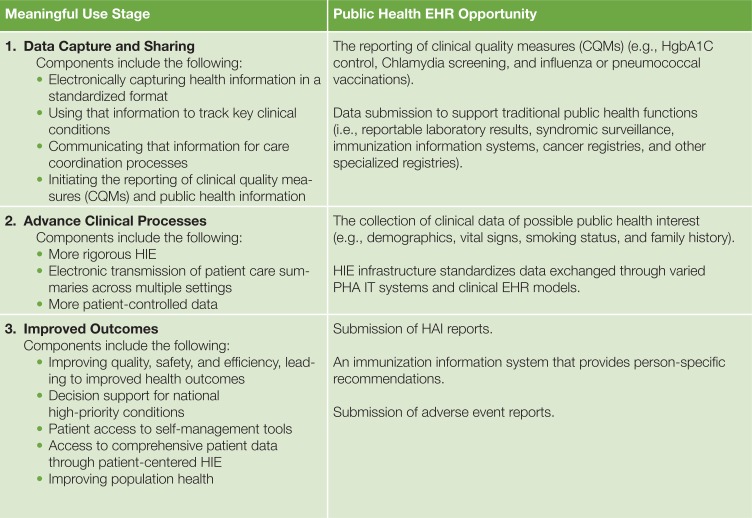
CMS incentives for demonstrating the MU of certified EHR technology have increased the adoption of EHRs by healthcare providers and hospitals.31 The first two stages of MU have both required and optional EHR functionality relevant to public health. The proposed third stage of MU recommends submission of Health-care Associated Infection (HAI) reports, adverse event reports, and the ability to receive person-specific recommendations from an immunization information system. (See Figure 2.)
Figure 2:
Public Health Functionality within MU
HIE refers to the electronic movement of health-related information, including MU data, among organizations according to nationally recognized standards.32 HIE may positively support public health data exchange with clinical health partners in a number of ways, including the following: reducing the number of system interfaces required to exchange data; providing automated routing of relevant electronic health information to public health; providing data standardization; providing record-linking services and supporting simultaneous queries across many care settings; supporting public health reminders and alerts; and, where agreed to, providing centralized data storage for efficient analysis.
HIE infrastructure serves as a hub, through which hospitals, ambulatory practices, laboratories, pharmacies, and other clinical entities exchange electronic data among their information systems. Connecting to an HIE may reduce the technical effort for a PHA versus attempting to connect and maintain direct interfaces with each clinical entity. HIE infrastructure can potentially monitor data transactions for specific laboratory or physician-based diagnoses, whether mandated or not mandated by statute, and can route appropriate health information to the PHA; this may preclude having the PHA work directly with each clinical entity or their technology vendor to achieve the same end.33 HIE infrastructure may provide services to standardize data exchanged across disparate IT systems, potentially reducing the data mapping effort of the PHA to create comparable population sets. A common feature of HIE service is the provision of a portal, which allows authorized users to search for health information about an individual across multiple healthcare settings, which could be used to support public health investigations. HIE infrastructure may serve as a mechanism for PHA communications back to clinical health; for example, in connecting to a provider’s EHR to identify individuals with notifiable diseases that have been lost to follow up, or to provide general information on epidemiologic trends in the community.33 Finally, HIE services may include the aggregation of data of public health interest into a centralized data warehouse to facilitate analysis.
Barriers and Limitations
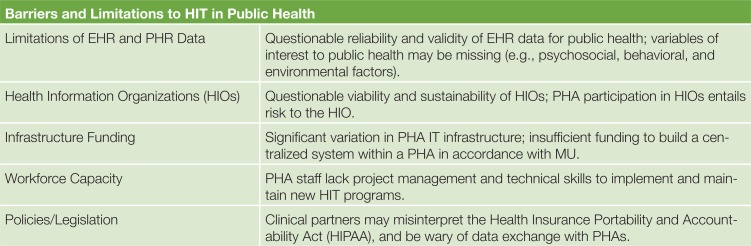
Barriers and limitations are detailed below, and illustrated in Figure 3.
Figure 3:
HIT Implementation Barriers and Limitations
Limitations of EHR and PHR Data
While EHRs have demonstrated potential to support public health practice, there are current limitations to more widespread public health use of EHR data. With respect to data availability, EHRs are generally designed around the provider-patient clinical encounter, and often do not include psychosocial, behavioral, and environmental variables of interest to public health. Some projects have attempted to capture such information within the clinical work-flow, but outside of the EHR context.34 Attempting to incorporate these variables into EHRs can require significant time and resource investment by PHAs to engage with EHR vendors and may also add additional burden to clinician workflow.35
With respect to data quality, the reliability and validity of EHR data for public health use may not be adequate, due to the use of different data models across EHRs, or to variation in data collection across practice settings, or to the use of free-text rather than structured data collection; however, there are demonstration projects currently underway to assess some of these issues.36 With respect to data exchange with EHRs, significant barriers include the following: the inconsistent use of available data and messaging standards, which may require ongoing encouragement of public health’s clinical partners; the establishment and ongoing monitoring of interfaces between clinical and public health; and policy or performance barriers to a PHA conducting direct queries or analyses.
Similarly, PHRs may also be difficult to use as a public health data source. Current evidence is limited with regard to the effectiveness of PHRs as a surveillance tool.37 In addition, there has been limited adoption of PHRs, their respective functionalities vary, uncertainty exists regarding market demand and who will support the cost of PHRs, in addition to lack of standards for data collection and biophysical measurements that may make PHRs prone to data quality issues.38,39
Health Information Organizations
While HIE shows promise as a service, there are significant concerns with regard to the financial viability and sustainability of the health information organizations (HIOs) that provide the oversight and governance for this service.40 In a survey to assess the state of HIE activity in the United States, only 75 of 197 potential HIOs were operational, 50 of those 75 HIOs did not meet criteria for financial viability, and only 13 of the HIOs surveyed met criteria for the first stage of MU.41 While information exchange with clinical care partners is conceptually attractive, PHA participation in an HIO entails significant risk where HIE is not already firmly entrenched as a sustainable, private community enterprise. Alternatively, where not supported by the market, HIE activity would have to be treated as a “public good,” with support provided by government and/or payers.42 If a PHA undertakes implementation of HIE activity, there are a number of prohibitive factors to consider: local PHA expertise in implementing these technologies should not be assumed; budgets must remain flexible to account for undiscovered work that is inevitably revealed during implementation; leadership should remain constant to ensure consistent vision; and contingencies must be in place to avoid delays that may undermine confidence, but delays should nevertheless be expected.43
Infrastructure Funding
The status of public-health information-technology infrastructure at health departments across the country is mixed. Baker and Koplan cited critical gaps in basic information technology services (such as fax, e-mail, and internet connectivity), although these gaps have been closing over the past decade.44 However, the software applications that are used to support core public health functions present a more variegated picture, as some PHAs have modern systems, while others maintain outdated legacy systems, and there are still others for whom these applications are “virtually nonexistent.”45 Seven percent of local health departments have implemented HIE and half have “no activity” in the area.46
Even within health departments, there is significant variation. Categorically funded public health programs have historically been prohibited from developing information systems that might also support the needs of other programs, leading to the development of information technology silos and information process silos (i.e., different programs in a PHA having parallel interactions with external data partners, such as hospitals and laboratories, leading to redundant coordination and resource investment).47,4 To support broad use of electronic health information across all programs in a public health department, shared infrastructure should be established for the receipt, processing, and analysis of data; development of such infrastructure will require separate dedicated funding and/or increased flexibility in the use of categorical funds.48
Although eligible hospitals and providers are receiving incentive funding for MU of certified EHR technology – including the submission of relevant data to PHAs, dedicated funding for public health to support ongoing receipt and management of MU data has been spare. Recently, traditional grant funding sources, including the CDC Cooperative Agreements for Epidemiology and Laboratory Capacity and Public Health Emergency Preparedness, have allowed PHAs more latitude to establish infrastructure that specifically supports MU engagement with hospitals and providers, although without providing specific guidance on specific, sustainable approaches.49,50,51 The National Association of County and City Health Officials have called for additional funds and The Joint Public Health Informatics Taskforce has called for alterations to cooperative agreements to fund necessary changes.52,53
Public health will need to advocate not only for building capacity to connect to clinical health, but to connect more efficiently through centralized HIE. While more than $547 million was initially awarded to states to support HIE activity through the State Health Information Exchange Cooperative Agreement Program, PHAs were generally not funded through these awards to connect into HIE infrastructure, nor was public health engagement of primary interest to some HIE efforts: in a survey of 27 of these cooperative programs, less than half supported public health use cases for HIE, such as the reporting of notifiable conditions or immunization data.54 It is critical for HIOs to be aware of PHAs as data exchange partners, and for both to pursue mutually beneficial funding opportunities that will sustain these relationships.
Workforce Capacity
Public health departments have variable information technology, and informatics and data analysis expertise, to receive, store, manage, and utilize new electronic health information sources. In an informatics needs assessment by the National Association of County and City Health Officials (NACCHO), barriers to implementing information systems (after insufficient funding and lack of time and resources) included lack of project management staff and lack of persons with technical skill to support systems.46 Even with information systems in place, local health departments may not have the appropriate staff to manipulate and understand the data: the percentage of local health departments that had epidemiologists, public health information specialists, and public health informatics specialists were 28%, 21%, and 13%, respectively.55 This is further compounded by a more general loss of approximately 15% of the local public health workforce from 2008 to 2011.56
For the moment, public health departments have not been mandated to receive MU data from hospitals and providers; however, if public health departments are compelled, or choose, to receive MU and other EHR data, they will likely need to add staff to conduct business analysis and project management to support the development of new systems and interfaces between public health and clinic health, as well as data analysts and epidemiology staff to prepare and analyze this new or augmented influx of data.
Policies and Legislation
In engagements between clinical and public health, the Health Insurance Portability and Accountability Act (HIPAA) is an oft-cited barrier to data exchange; in fact, according to the HIPAA Privacy Rule, covered entities may disclose protected health information for public health use, including reporting, surveillance, investigations, and interventions.57 Public health will need to continue to educate its clinical partners on permissibility of disclosures to public health, in order to support necessary and novel secondary uses of electronic health information.
State and local statutes have mandated the reporting of selected infectious and noncommunicable diseases. However, many other conditions of interest to public health, including indicators of chronic disease – or even negative results from tests for reportable diseases – do not enjoy the same sanctions. As new sources of electronic health data become available, corresponding legislation will be required to support their use for public health purposes. For example, in 2005, the New York City Board of Health mandated the laboratory reporting of hemoglobin A1C test results to track blood glucose levels in diabetes patients; while preliminary feedback has been positive, it has not been without controversy, and may provide important lessons for other health agencies.58
Conclusion
Ultimately, the broad vision is that electronic health information from EHRs and PHRs will be made available to PHAs through direct connections or via consolidated HIE. The latter will leverage Big Data science to conduct surveillance and make inferences about health determinants, implementing traditional population-level interventions and individual clinical interventions via CDS technologies. The potential of electronic HIE implies timely availability and improved access to data, compared to traditional paper-based manual processes. The availability of enhanced technology implies more timely analysis and opportunities for innovation.
In order to realize this vision, local health departments require additional funding and technical support from national bodies for infrastructure development. Additional personnel are needed for policy development and advocacy for the needs of public health departments in local HIE. Technical personnel must engage with both internal and external partners regarding MU reporting and must navigate the complex field of changing requirements and standards for health information technology. Appropriate business analysis and project management staff will be required to ensure that all systems are designed to help users work more efficiently, rather than simply automating and reinforcing redundant processes. Data analysis staff must then appropriately interpret these data and present the data in a way that makes decision making clear and actionable.
Public health leaders at the state and local levels need an increased commitment to public health informatics and the development of sustainable centralized HIE. They must develop their own strategic plan for sustainability that includes the public health workforce and technical expertise. Furthermore, leaders will need to offer ongoing education to all parties involved in HIE on the role of HIPAA for health departments. Surveillance laws must be addressed to include chronic diseases and other diseases of public health importance to protect access to electronic clinical data for the benefit of the public’s health.
Just as electronic health information will transform the day-today practice of medicine, it will transform the practice of public health. Together with the changes brought about by health reform, it will facilitate the development of PHAs into knowledge organizations. The transition will require investment in new technology, analytic and application techniques, hiring and retraining of staff, but – most importantly – creative leadership to capitalize on these new opportunities.
Acknowledgments
The authors sincerely thank the reviewers and editors for their insightful comments and assistance in preparing this article.
Endnotes
- 1.Institute of Medicine . The Future of Public Health. Washington, D.C.: National Academy Press; 1988. [Google Scholar]
- 2.Berwick DM, Nolan TW, Whittington J. The Triple Aim: Care, Health, and Cost. Health Affairs. 2008 May-Jun;27:759–69. doi: 10.1377/hlthaff.27.3.759. Available from http://content.healthaffairs.org/content/27/3/759.full.pdf+html. [DOI] [PubMed] [Google Scholar]
- 3.Schauer SL, Hopfensperger DJ, Verdon MJ, Maerz TR, Gabor GW, Davis JP. An immunization information system to meet evolving needs during the 2009–2010 Influenza A (H1N1) vaccination campaign. Disaster Med Public Health Prep. 2012;6(4):402–7. doi: 10.1001/dmp.2012.64. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention The Role of Public Health Informatics in Enhancing Public Health Surveillance. MMWR. 2012 Jul 27;61:20–24. [PubMed] [Google Scholar]
- 5.Markle Foundation Connecting for Health. 2003. The personal health working group final report.
- 6.Weitzman ER, Kelemen S, Kaci L, Mandl KD. Willingness to share personal health record data for care improvement and public health: a survey of experienced personal health record users. BMC Med Inform Decis Mak. 2012;12(39):1–10. doi: 10.1186/1472-6947-12-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Samarrai T, Wu W, Begier E, Lurio J, Tokarz R, Plagianos M, et al. Evaluation of a Pilot Respiratory Virus Surveillance System Linking Electronic Health Record and Diagnostic Data. J Public Health Manag Pract. 2013 Feb; doi: 10.1097/PHH.0b013e3182602ef6. (e pub ahead of print) [DOI] [PubMed] [Google Scholar]
- 8.Houser SH, Colquitt S, Clements K, Hart-Hester S. The impact of electronic health record usage on cancer registry systems in Alabama. Perspect Health Inf Manag. 2012 Spring;9 Epub. [PMC free article] [PubMed] [Google Scholar]
- 9.Comer KF, Grannis S, Dixon BE, Bodenhammer DJ, Wiehe SE. Incorporating geospatial capacity within clinical data systems to address social determinants of health. Public Health Rep. 2011;126(Suppl 3):54–61. doi: 10.1177/00333549111260S310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sun J, Hu J, Luo D, Markatou M, Wang F, Edabollahi S, et al. Combining Knowledge and Data Driven Insights for Identifying Risk Factors using Electronic Health Records. n.d. [Cited Oct 3, 2013] Available from: http://www.research.ibm.com/healthcare/papers/AMIA2012CHF.pdf. [PMC free article] [PubMed]
- 11.Solberg LI, Flottemesch TJ, Foldes SS, Molitor BA, Walker PF, Crain AL. Tobacco-use prevalence in special populations: Taking advantage of electronic medical records. Am J Prevent Med. 2008;35(6):S501–7. doi: 10.1016/j.amepre.2008.08.033. [DOI] [PubMed] [Google Scholar]
- 12.Lindholm C, Adsit R, Bain P, Reber PM, Brein T, Redmond L, et al. A demonstration project for using the electronic health record to identify and treat tobacco users. Wisc Med J. 2010;109(6):335–40. [PMC free article] [PubMed] [Google Scholar]
- 13.Schneiderman JU, Smith C, Arnold-Clark JS, Fuentes J, Duan L. Weight changes in children in foster care for 1 year. Child Abuse Negl. 2013 Mar 14; doi: 10.1016/j.chiabu.2013.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.New York City Department of Health and Mental Hygeine The New York City Macroscope: Developing an Electronic Health Record-Based Population Health Surveillance System. [Cited Aug 18, 2013] Available from http://www.nyc.gov/html/doh/downloads/pdf/data/nyc-macro-summary.pdf.
- 15.VanWormer JJ. Methods of using electronic health records for population-level surveillance of coronary heart disease risk in the Heart of New Ulm Project. Diabetes Spectrum. 2010;23(3):161–165. [Google Scholar]
- 16.Guilbert TW, Arndt B, Temte J, Adams A, Buckingham W, Tandias A. The theory and application of UW ehealth-PHINEX, a clinical electronic health record-public health information exchange. Wisc Med J. 2012;111(3):124–33. [PubMed] [Google Scholar]
- 17.Khoury MJ, Lam TK, Ioannidis JP, Hartge P, Spitz MR, Buring JE. Transforming epidemiology for 21st century medicine and public health. Cancer Epidemiol Biomarkers Prev. 2013;22(4):508–16. doi: 10.1158/1055-9965.EPI-13-0146. Epub 2013 Mar 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Evans JP, Berg JS, Olshan AF, Magnuson T, Rimer BK. We screen newborns, don’t we? Realizing the promise of public health genomics. Genet Med. 2013. (published online March 7) [DOI] [PMC free article] [PubMed]
- 19.Scotch M, Parmanto B, Monaco V. Evaluation of SOVAT: an OLAP-GIS decision support system for community health assessment data analysis. BMC Med Inform Decis Mak. 2008 Jun 9;8:22. doi: 10.1186/1472-6947-8-22. epublication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Research Council . Improving Health in the United States: The Role of Health Impact Assessment. National Academies Press; Washington, DC: 2011. [PubMed] [Google Scholar]
- 21.Klompas M, McVetta J, Lazarus R, Eggleston E, Haney G, Kruskal BA. Integrating clinical practice and public health surveillance using electronic medical record systems. Am J Public Health. 2012;102(Suppl):S325–32. doi: 10.2105/AJPH.2012.300811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dixon BE, Gamache RE, Grannis SJ. Towards public health decision support: a systematic review of bidirectional communication approaches. J Am Med Inform Assoc. 2013;20(3):577–83. doi: 10.1136/amiajnl-2012-001514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herwehe J, Wilbright W, Abrams A, Bergson S, Foxhood J, Kaiser M. Implementation of an innovative, integrated electronic medical record (EMR) and public health information exchange for HIV/AIDS. J Am Med Inform Assoc. 2012;19(3):448–52. doi: 10.1136/amiajnl-2011-000412. Epub 2011 Oct 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Office of the National Coordinator for Health IT Clinical Decision Support. 2012. Apr 5, [Cited Apr 5, 2013] Available from: http://www.healthit.gov/policy-researchers-implementers/clinical-decision-support-cds.
- 25.Bright T, Wong A, Dhurjati R, Bristow E, Bastian L, Coeytaux R, et al. Effect of clinical decision-support systems: a systematic review. Ann Intern Med. 2012;157(1):29–43. doi: 10.7326/0003-4819-157-1-201207030-00450. [DOI] [PubMed] [Google Scholar]
- 26.Jaspers MW, Smeulers M, Vermeulen H, Peute LW. Effects of clinical decision-support systems on practitioner performance and patient outcomes: a synthesis of high-quality systematic review findings. J Am Med Inform Assoc. 2011;18(3):327–34. doi: 10.1136/amiajnl-2011-000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu WY, Hripcsak G, Lurio J, Pichardo M, Berg R, Buck M, et al. Impact of integrating public health clinical decision support alerts into electronic health records on testing for gastrointestinal illness. J Public Health Manag Pract. 2012;18(3):24–7. doi: 10.1097/PHH.0b013e318241555d. [DOI] [PubMed] [Google Scholar]
- 28.Lurio J, Morrison FP, Pichardo M, Berg R, Buck MD, Wu W, et al. Using electronic health record alerts to provide public health situational awareness to clinicians. J Am Med Inform Assoc. 2010;17(2):217–9. doi: 10.1136/jamia.2009.000539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mandl KD, Mandel JC, Murphy SN, Berstam EV, Ramoni RL, Kreda DA, et al. The SMART Platform: early experience enabling substitutable applications for electronic health records. J Am Med Inform Assoc. 2012;19(4):597–603. doi: 10.1136/amiajnl-2011-000622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mandl KD, Simons WW, Crawford W, Abbett JM. Indivo: a personally controlled health record for health information exchange and communication. BMC Med Inform Decis Mak. 2007;7:25. doi: 10.1186/1472-6947-7-25. epublication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xierali IM, Hsiao CJ, Puffer JC, Green LA, Rinaldo JC, Baze-more AW, et al. The rise of electronic health record adoption among family physicians. Ann Fam Med. 2013;1(1):14–9. doi: 10.1370/afm.1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Alliance for Health Information Technology The National Alliance for Health Information Technology report to the Office of the National Coordinator for Health Information Technology on defining key health information technology terms. 2008.
- 33.Shapiro JS, Mostashari F, Hripcsak G, Soulakis N, Kuperman G. Using health information exchange to improve public health. Am J Public Health. 2011;101(4):616–23. doi: 10.2105/AJPH.2008.158980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Orlando LA, Hauser ER, Christianson C, Powell KP, Buchanan AH, Chesnut B, et al. Protocol for implementation of family health history collection and decision support into primary care using a computerized family health history system. BMC Health Serv Res. 2011;11:264. doi: 10.1186/1472-6963-11-264. epublication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kukafka R, Ancker JS, Chan C, Chelico J, Khan S, Mortoti S, et al. Redesigning electronic health record systems to support public health. J Biomed Inform. 2007;40(4):398–409. doi: 10.1016/j.jbi.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention CDC-BRFSS-Connecting with Clinical Medicine. 2013. Mar 19, [cited March 19, 2013] Available from http://www.cdc.gov/brfss/rd/connect_with_medicine.htm.
- 37.Paton C, Hansen M, Fernandez-Lugue L, Lau AY. Self-tracking, social media and personal health records for patient empowered self-care. Contribution of the IMIA Social Media Working Group. Yearb Med Inform. 2012;7(1):16–24. [PubMed] [Google Scholar]
- 38.Detmer D, Bloomrose M, Raymond B, Tang P. Integrated Personal health records: transformative tools for consumer-centric care. BMC Med Inform Decis Mak. 2008;45 doi: 10.1186/1472-6947-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stryker T, Wilson M, Wilson TW. Accuracy of home blood pressure readings: monitors and operators. Blood Press Monit. 2004;9(3):143–7. doi: 10.1097/01.mbp.0000130224.18777.ce. [DOI] [PubMed] [Google Scholar]
- 40.Hess J. The brave, new world of HIEs. Healthc Financ Manage. 2011;65(2):44–8. [PubMed] [Google Scholar]
- 41.Adler-Milstein J, Bates DW, Jha AK. A survey of health information exchange organizations in the United States: implications for meaningful use. Ann Intern Med. 2011;154(10):666–71. doi: 10.7326/0003-4819-154-10-201105170-00006. [DOI] [PubMed] [Google Scholar]
- 42.Vest JR, Gamm LD. Health information exchange: persistent challenges and new strategies. J Am Med Inform Assoc. 2010;17(3):288–294. doi: 10.1136/jamia.2010.003673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Merrill JA, Deegan M, Wilson RV, Kaushal R, Fredericks K. A system dynamics evaluation model: implementation of health information exchange for public health reporting. J Am Med Inform Assoc. 2013 Jun;20(e1):e131–8. doi: 10.1136/amiajnl-2012-001289. [epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baker EL, Koplan JP. Strengthening The Nation’s Public Health Infrastructure: Historic Challenge, Unprecedented Opportunity. Health Affairs. 2002;21(6):15–27. doi: 10.1377/hlthaff.21.6.15. [DOI] [PubMed] [Google Scholar]
- 45.Baker EL, Potter MA, Jones DL, Mercer SL, Cioffi JP, Green LW, et al. The Public Health Infrastructure and Our Nation’s Health. Annual Review of Public Health. 2005;2005;26:303–318. doi: 10.1146/annurev.publhealth.26.021304.144647. [DOI] [PubMed] [Google Scholar]
- 46.National Association of County and City Health Officials . The Status of Local Health Department Informatics: Results from the 2010 NACCHO Informatics Needs Assessment. Washington, DC: National Association of County and City Health Officials; 2010. [Google Scholar]
- 47.Lumpkin JR, Richards MS. Transforming the public health information infrastructure. Health Affairs. 2002;21(6):45–56. doi: 10.1377/hlthaff.21.6.45. [DOI] [PubMed] [Google Scholar]
- 48.Association of State and Territorial Health Officials Public Health Meaningful Use - Position Statement. 2010. [cited Aug 18, 2013] Available from http://www.astho.org/Policy-and-Position-Statements/Position-Statement-on-Meaningful-Use/
- 49.Buntin BM, Jain SH, Blumenthal D. Health Information Technology: Laying the infrastructure for national health reform. Health Affairs. 2010;29(6):1214–1219. doi: 10.1377/hlthaff.2010.0503. [DOI] [PubMed] [Google Scholar]
- 50.Department of Health and Human Services, Catalog for Federal Domestic Assistance The Affordable Care Act: Building Epidemiology, Laboratory, and Health Information Systems Capacity in the Epidemiology and Laboratory Capacity for Infectious Disease (ELC) and Emerging Infections Program (EIP) Cooperative Agreements; PPHF, No. 93.521. [Cited Aug 18, 2013] Available from https://www.cfda.gov/index?s=program&mode=form&tab=step1&id=d85e7ebd9a95b0bdfdd1d82a2b47c591.
- 51.Department of Health and Human Services, Catalog for Federal Domestic Assistance Public Health and Emergency Preparedness, No. 93069. [Cited Aug 18, 2013] Available from: https://www.cfda.gov/index?s=program&mode=form&tab=-step1&id=76ed45c029b6bffc156973a5b672a224.
- 52.National Association of County and City Health Officials . Statement of Policy: Electronic Health Records, Health Information Exchange, and Interoperability for Local Health Departments. Washington, DC: National Association of County and City Health Officials; 2012. [Cited Aug 18, 2013] Available from: http://www.naccho.org/advocacy/positions/upload/07-05_EHR-HIE-Interoperability-6-12.pdf. [Google Scholar]
- 53.Joint Public Health Informatics Taskforce Joint Meaningful Use Action Plan. 2010. [Cited Aug 18, 2013] Available from : http://www.astho.org/Display/AssetDisplay.aspx?id=5140.
- 54.National Opinion Research Center (NORC) at the University of Chicago . Evaluation of the State Health Information Exchange Cooperative Agreement Program: Early Findings from a Review of Twenty-Seven States. Bethesda, MD: NORC at the University of Chicago; 2012. [Google Scholar]
- 55.National Association of County and City Health Officials . 2010 National Profile of Local Health Departments. Washington, DC: National Association of County and City Health Officials; 2011. [Google Scholar]
- 56.Levi J, Segal LM, St Laurent R. Investing in America’s Health: A state-by-state look at public health funding and key health facts. Washington, DC: Trust for America’s Health; 2011. [Google Scholar]
- 57.Office for Civil Rights Title 45 of the Code of Federal Regulations, Part 164. 2003. Oct 1, [Cited Apr 5, 2013] Available from http://www.gpo.gov/fdsys/pkg/CFR-2003-title45-vol1/content-detail.html.
- 58.Chamany S, Silver LD, Bassett MT, Driver CR, Berger DK, Neuhaus CE, et al. Tracking diabetes: New York City’s A1C Registry. Milbank Q. 2009;87(3):547–70. doi: 10.1111/j.1468-0009.2009.00568.x. [DOI] [PMC free article] [PubMed] [Google Scholar]