Abstract
Introduction:
In the aftermath of Hurricane Katrina, much of New Orleans’ healthcare infrastructure was destroyed. Initial federal funding after the storm expanded primary care services and helped set up medical homes for New Orleans’ large uninsured and underinsured population. Following that, the Beacon Community in New Orleans, charged with improving health care through the use of technology, decided the best way to accomplish those goals was to build community partnerships and introduce technology improvements based on their input and on their terms. The purpose of this paper is to describe how those partnerships were wrought, including the innovative use of a conceptual framework, and how they are being sustained; how different technologies were and are being introduced; and what the results have been so far.
Methods:
Past successful community experiences, as well as a proven conceptual framework, were used to help establish community partnerships and governance structures, as well as to demonstrate their linkages. This paper represents a compilation of reports and information from key Beacon leaders, staff and providers and their firsthand experiences in setting up those structures, as well as their conclusions.
Results:
The community partnerships proved extremely successful in not only devising successful ways to introduce new technology into healthcare settings, but in sustaining those changes by creating a governance structure that has enough fluidity to adapt to changing circumstances.
Conclusions:
Building and developing community partnerships takes time and effort; however, these relationships are necessary and essential to introducing and sustaining new technologies in a healthcare setting and should be a first step for any organization looking to accomplish such goals.
Keywords: Health Information Technology, Sustainability, Governance, Beacon Community, Partnership Building, System of care
Background
The Greater New Orleans (GNO) area healthcare system (which includes four parishes, i.e., counties: Orleans, Jefferson, St. Bernard and Plaquemines) has undergone a major transformation over the past eight years. Prior to August 29, 2005, uninsured and underinsured GNO residents relied on a fractured, inefficient health system where the usual source of care often centered on the emergency department of Charity Hospital. At that time, the public Medical Center of Louisiana, comprising Charity and University Hospitals, both located in downtown New Orleans, received 50% of all ambulatory and hospital visits in GNO. Its patient population was 75% African American with incomes of $20,000 or less, with 83% of inpatient care and 88% of outpatient care uncompensated.1,2
While Hurricane Katrina devastated much of the area’s infrastructure, including its healthcare system, it also provided an opportunity to rebuild a better healthcare system, particularly for the safety net population.3 Starting in 2007, two federal funding opportunities supported improved access to coordinated care for poor residents in GNO. The first, the $100 million Primary Care Access and Stabilization Grant (PCASG), was successful in helping New Orleans expand primary care access services throughout GNO by setting up medical homes and moving away from a centralized public hospital system to a community primary care clinic model over a three-year period (2007–2010).4,5
Secondly, in 2010 New Orleans was awarded a three-year, $13.5 million Beacon grant from the Department of Health and Human Services Office of the National Coordinator for Health Information Technology (ONC). One of only 17 communities in the United Sates to be selected as a “Beacon,” this cooperative endeavor between ONC and the New Orleans community was designed to fulfill ONC’s mission of building and strengthening local health information technology systems as well as testing approaches to improve population health and lower health care costs.6
The Crescent City Beacon Community (CCBC) directly involved over 150,000 patients and 160 providers, including five hospitals, 16 community health center and federally qualified health center (FQHC) practice sites, and one health plan. Its goal was to demonstrate population health improvement through the use of health information technology (HIT) by lowering the burden of chronic disease, primarily diabetes and cardiovascular disease.7
The CCBC experience is a unique case study of a community with a fractured healthcare system using a cooperative opportunity with the ONC to chart a path for a data-driven, evidence-based health system transformation enabled by HIT. The purpose of this paper is to describe how the CCBC built partnerships to bring about such a transformation, how HIT interventions were selected by a community to improve the continuity of care and ultimately health outcomes, and what the challenges were in implementation and initial results.
As background for the case study, we describe two fundamental and related components of the CCBC efforts in New Orleans. The first is a conceptual framework that was originally developed by one of the authors and was critical to developing a common vision and understanding among CCBC partners for improving the community’s healthcare delivery system. The second is a description of the CCBC’s governance approach, which was so important in translating the vision into reality through a trusted and effective community collaboration. Based on this strong foundation and shared vision, CCBC partners successfully implemented three categories of complex interventions related to chronic care management, transitions of care, and consumer engagement through innovative use of information technologies.
Conceptual Framework
The CCBC interventions were developed using the Dynamic Framework for a Coordinated System of Care (DFCSC), a systemic approach which simplifies the complex relationships among different subsystems in a community healthcare setting by depicting how policies and actions in one part of the system affect the other. Developed at the Integrated Care Collaboration (ICC), a consortium of safety net providers in Austin, Texas, the DFCSC was successful in providing a model for community healthcare collaboration and showing the meaningful use of shared information through the adoption of information technology. However, neither the details nor the application of the DFCSC have been published before.
While different frameworks have been developed to explain healthcare delivery systems, few provide practical guidance on how health services may be better coordinated at a community level to improve service delivery for vulnerable populations.8 Also, there is a dearth of evidence regarding governance of shared healthcare data in such settings.9 A framework for explaining a real-world delivery system has to be dynamic in nature so it may be adapted to changing demographic, legal, and practice environments. It should also include feedback loops between patients and providers in a system.
The ICC partners in Austin, Texas, helped develop the DFCSC framework based on their practical understanding of the linkages in the system, particularly for safety net populations. This framework emphasized the community-level role of the health system and highlighted the importance of electronic, real-time linkages among different settings through a health information exchange that ICC had managed for over ten years.10 It would be hard to establish these linkages without the effective use of HIT infrastructure to allow for information sharing.
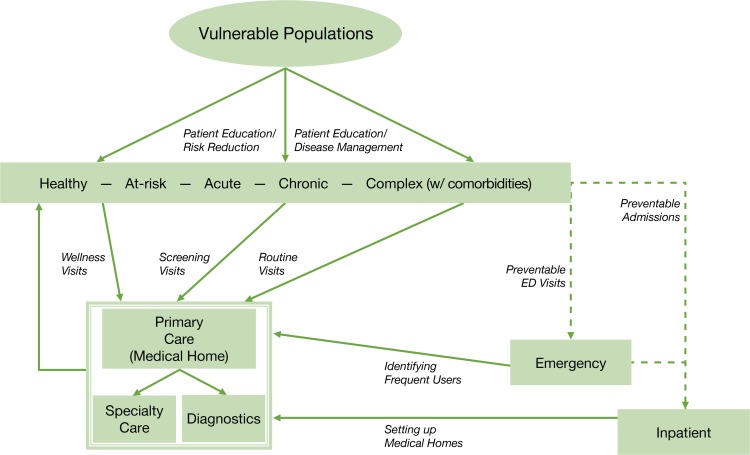
The DFCSC framework, as shown in Figure 1, assumes a population comprising people at different levels of health, ranging from those who are healthy and at low risk to those with comorbidities and at high risk for frequent visits and high costs. Depending on where people are on the health spectrum, they access primary care for routine check-ups, preventive services, screening, diagnosis, referrals, or treatment. Persons in the high-risk category place the largest demand on the system through frequent visits to emergency department and frequent inpatient admissions. Many of these visits can be prevented and avoided if these patients have a regular source of care, such as a medical home, and if better information about them is available through shared networks.11,12
Figure 1.
DFCSC Framework
Source: Based on information collected by author (AK) using key informants on the Board of ICC
The DFCSC also incorporates systems theory.13 The healthcare system as a whole is part of the community system that includes social services systems and educational systems influencing, and being influenced by, the healthcare system. If primary care clinics fail to provide quality care to their patients as medical homes, or if there is a shortage of specialty services for the seriously ill patients, then the link between high-risk patients and the primary care clinics will be weakened and the flow of patients to the emergency or inpatient facilities will increase.
HIT is key to developing a feedback loop among different parts of the healthcare system to ensure optimal continuity of care. The absence of such HIT linkages leads to the fragmented healthcare delivery that is often associated with increased cost and medical errors in the system.14
Interoperable and connected electronic medical record systems allow for the feedback loops in the DFCSC so emergency departments can see how patients using emergency services for non-urgent, preventable conditions can be helped by referring them to a primary care clinic for continuity of care. At the same time, this allows primary care clinics to understand the importance of follow-up and relationship-building in helping improve these patients’ care and preventing visits to emergency departments.15,16
The feedback loop can be in the form of real-time notifications, ADT (Admit, Discharge, Transfer) messages, or regular utilization reports available to the providers of healthcare services. The framework also emphasizes the need to adopt patient-centered approaches that help patients through a combination of appropriate care and behavior change.17,18 The DFCSC, therefore, lays the foundation for an evidence-based healthcare system built on the principles of prevention, coordination and information exchange, and enabled by system integration through health information technology.
Establishing Governance
Trust, engagement, ownership and accountability are essential for successful and sustainable intervention implementation among unaffiliated members of the healthcare delivery system. Lessons learned from other communities underscored the critical importance of establishing active governance bodies led by invested community stakeholders.7,19
The CCBC decided to base its governance structure on existing relationships with healthcare delivery partners, particularly its safety net providers. The CCBC partnership included 16 health operators serving the GNO safety net population that had a history of working together as well as with the Louisiana Public Health Institute (LPHI). Pre-Katrina the partnership focused on quality improvement initiatives. Post-Katrina the partnership worked more intensively to rebuild the health system through the PCASG grant.4
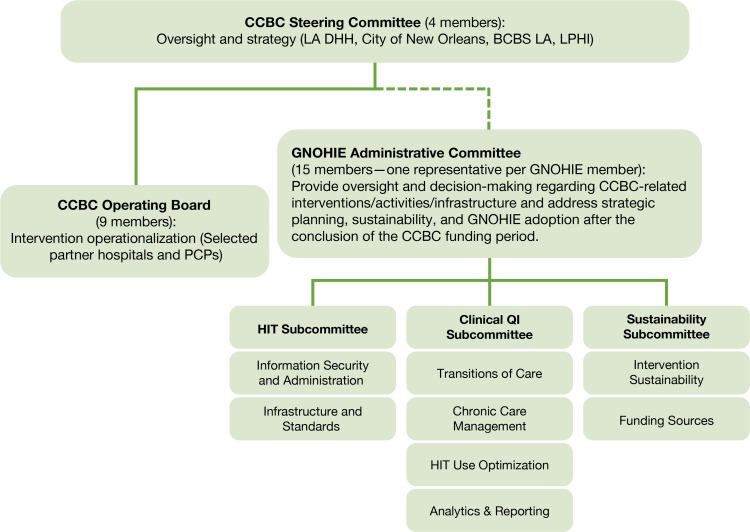
At the inception of the program, the CCBC decided its governance structure needed to include a Steering Committee, which comprised the Secretary of the Louisiana Department of Health & Hospitals (DHH), a senior executive of Blue Cross Blue Shield of Louisiana (BCBSLA), the Health Commissioner of City of New Orleans Health Department (NOHD), and the CEO of LPHI. The committee was charged with providing oversight and strategic direction to the CCBC beyond its specific project deliverables and helping ensure alignment with other federal, state, and local efforts to improve health in Louisiana.
More specifically, the state and local health officers (Secretary DHH and Commissioner NOHD) provided their perspectives on how CCBC efforts could integrate with other programs and policies, while the BCBSLA executive helped represent the view of payers on the value of these population health improvements. An Operating Board, with partner representation from the CCBC implementing partners, was then established to propose and monitor the interventions.
Clinical Quality Improvement (CQI), Health Information Technology (HIT), and Sustainability subcommittees were subsequently formed to address specific program areas, such as chronic care management, transitions of care and financial models for sustaining the HIT infrastructure. These committees had written charters that described their roles and responsibilities and how decisions would be made by the members. The relationship of these committees and their membership is shown in Figure 2.
Figure 2.
CCBC Governance Infrastructure
The subcommittees met regularly to identify appropriate intervention strategies, monitor progress, disseminate lessons and adjust direction as needed as well as make recommendations to the Operating Board and Steering Committee. These groups also worked closely with the Office of National Coordinator for HIT and other Beacon communities across the country to inform and share best practices for population health improvement strategies.20
The CCBC governance structure evolved over the course of the program as new partners joined, community needs changed, and the focus on sustainability increased to ensure CCBC maintenance.
The Greater New Orleans Health Information Exchange (GNOHIE) was established to manage the information technology infrastructure of CCBC after the completion of the grant and led to the establishment of a second governance component. The GNOHIE Administrative Committee was formed in the first quarter of 2012—approximately halfway through the CCBC grant period—as the first step in creating a permanent governance structure to provide oversight and decision-making to ensure CCBC sustainability through community-partner ownership.
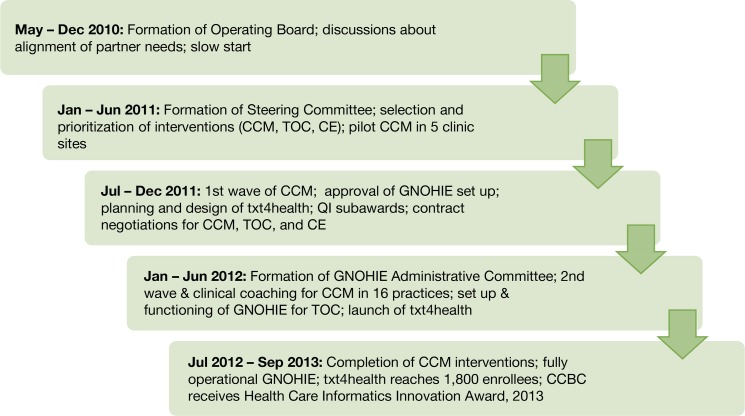
The key milestones of the CCBC project are shown in Figure 3. There was a significant planning period in year 1, followed by quick implementation and operationalization in years 2 and 3.
Figure 3.
Timeline of key CCBC milestones
The Administrative Committee also monitored CCBC-related interventions, activities, infrastructure, strategic planning, and GNOHIE adoption after the conclusion of the CCBC funding period. The Administrative Committee was composed of representatives of partners that were contributing data and otherwise participating in the GNOHIE interventions. The subcommittees (Clinical Quality Improvement, Health Information Technology, Sustainability) created under the original Operating Board were re-established under the new structure to ensure the sustainability of the governance structure.
Strategies to Meet the Goals of the CCBC Initiative
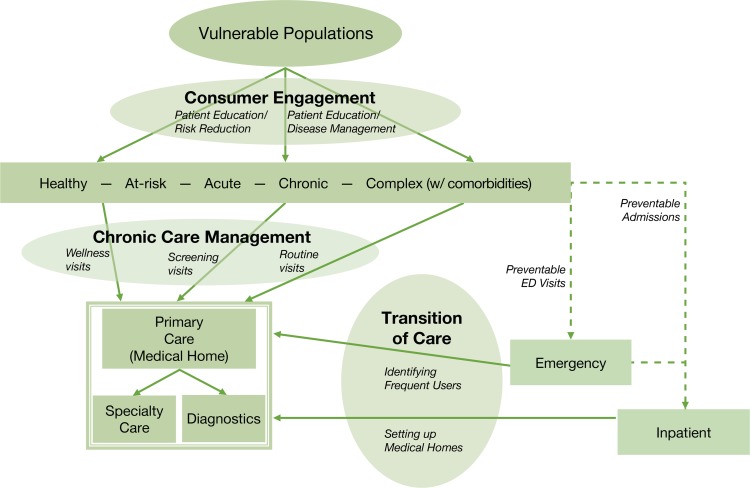
The DFCSC model was critical in guiding early discussions with GNO community providers, as it allowed them to visualize the impact of CCBC interventions in improving the healthcare delivery system. The model aligns with the triple aim of better care for patients, improved health of the population and reduced healthcare expenditures. The DFCSC not only provided a model for community collaboration in healthcare delivery but also a framework that showed the meaningful use of shared information through adoption of information technology. The CCBC partners, through the governance structure, were then able to identify the following ongoing strategic, community-wide interventions to meet the CCBC goals:
Chronic Care Management (CCM). This core set of HIT enabled evidence-based interventions focused on strengthening patient-centered medical homes in primary care practices that serve the safety net population suffering from diabetes and cardiovascular disease. The interventions included risk stratification, population-based registries, care team approaches, and clinical decision support systems in electronic medical records.
Transitions of Care (TOC). These interventions focused on improving care coordination to help ensure seamless transition of patients between primary care, specialty care and hospital-based settings, including electronic notification of emergency department visits to primary care physicians and specialty e-referral systems using a health information exchange.
Consumer Engagement. An innovative text messaging program, called txt4health, was developed to provide the public with personalized education, diabetes risk assessments and follow-up messages to increase the public’s awareness about diabetes and connect them to the healthcare system for screening, diagnosis and treatment.
The impact of each of these interventions was understood in the context of DFCSC as shown in Figure 4. The following describes how the governance structure facilitated the implementation of the interventions through the partner organizations.
Figure 4.
DFCSC Framework with Integrated Goals
Source: Modified version, based on information collected by author (AK) using key informants on the Board of CCBC
Methods
Using a descriptive case study approach, this paper examines how the New Orleans Beacon Community helped to create a better healthcare system by building and developing the community partnerships that were essential to introducing and sustaining new technologies. The case study approach uses a variety of data sources to develop an in-depth empirical inquiry about a contemporary phenomenon set within its real-world context. Data used to inform this case study include interviews with key Beacon leaders, clinic staff and healthcare providers as well as reports and other program documentation. Although traditionally associated with process evaluations, case studies have been used successfully to document and analyze the outcomes of interventions.23 This case study describes the processes and subsequent outcomes of establishing a complex and robust governance structure for the Beacon Community Program in New Orleans.
Results
The following explains the implementation of each intervention under the CCBC program and how the governance structure provided direction throughout the process. Recommendations based on our experiences related to each intervention are also included.
Chronic Care Management (CCM)
As shown in the DFCSC, improving chronic care management at the population level requires a central role for a quality primary care system that is patient-centered, efficient and accountable for patient health outcomes. Five clinics volunteered to pilot test four related interventions under CCM: (1) risk stratification of patients on evidence-based criteria; (2) using chronic disease registries in EHRs; (3) adopting clinical decision support systems in clinical workflow; and (4) introducing care team protocols in clinical settings. Most clinics found it overwhelming to try to implement new interventions that required changes in workflow. Therefore it was essential to pilot interventions with clinics that were willing to pilot the interventions.
Not surprisingly, these pilot clinics represented those whose medical directors were on the CCBC Operating Board, which highlights the importance of community involvement in governance.
The interventions were then expanded to 13 sites in the second wave and another six sites in the third wave, at approximately six-month intervals. The CQI subcommittee of clinic representatives monitored the implementation challenges and facilitated the diffusion of experiences from the first-wave clinics to the second-and third-wave clinics. Regular calls among all CCBC clinic representatives were held to discuss and share strategies. An online library was created using Sharepoint to allow for easy access and direct contribution of those involved in developing protocols and guidelines for CCM. Establishing a learning community among partners was critical to achieving the goals of CCM because it helped to build peer pressure among clinic operators to join the quality improvement efforts and provided a stage to recognize the work of the early adopters.
Although the CCBC program strongly encouraged all primary care clinics to implement the CCM interventions in a form that was similar across all partners, it also recognized that some adaptation was necessary to fit existing quality improvement programs and clinic operations. This flexible approach minimized the impact on, and potential resistance from, the staff in clinics that took on the daunting task of improving their internal systems while still fulfilling their routine responsibilities. These adaptations were reviewed through the CQI Subcommittee to ensure shared accountability to the goals of the CCBC program.
Provide Quality Improvement Incentives
During the implementation of CCM interventions, partners had difficulty allocating significant time to integrate new protocols, develop staff skills, and participate in the CCBC community meetings. To offset some of these additional costs and to incentivize the CCBC interventions, the CCBC governance launched the Quality Improvement Initiative in January 2012.
Each primary care clinic, including hospital-based clinics that demonstrated its ability to implement quality improvement programs encompassing the CCM and TOC interventions for patients with diabetes or cardiovascular disease was awarded up to $100,000. In total, 12 subawards were given out on a non-competitive basis depending on the clinic’s ability to regularly report data so that CCBC quality improvements could be evaluated within each organization. This strategy relied on encouraging quality improvement efforts already underway in partner institutions. This approach helped create more ownership of CCBC quality improvement goals as partners were asked to improve or expand existing efforts rather than look upon CCBC interventions as yet another workflow disruption.
The above strategy yielded positive results and much enthusiasm from staff, many of whom needed additional resources and wanted recognition for their quality improvements from within their own organizations. Not only did the subawards program help in implementation of already defined CCBC interventions (CCM and TOC) but it also resulted in related innovations that were tested and diffused through this partnership including:
– A Boot Camp to increase patient participation in diabetes education programs: A novel two-hour intensive education program, led by a multidisciplinary team of clinicians, proved effective among the newly diagnosed with HbA1c (blood glucose indicator) above 9.0 and the “recaptured” diabetic who had been lost to follow-up for various reasons. The boot camp concept involved a patient navigation system to streamline the patient’s interaction with each clinician in the care team. The system started with a medical office administrator triaging the patient at check-in and was followed by: a nurse practitioner performing the exam, prescribing medications and reviewing HbA1c, blood pressure and cholesterol levels; a pharmacist engaging in diet and medication-intensive diet education, and smoking cessation education; and a health educator reinforcing clinicians’ recommendations and scheduling education classes for the patient. As the details of this program were shared with other community clinics through the CCBC community collaborative, at least two other CCBC partners adopted the program in their own clinics within a few months.
– Operationalizing shared medical appointments to improve access and quality of care through enhanced patient education and support for those with chronic illness, especially diabetes. CCBC funding supported the operationalization of these shared medical appointments, where a multidisciplinary team (MD/NP, dietitian, health educator, and pharmacist) saw a group of patients (usually between 8–10 patients in 1.5- to 2-hour appointments) referred through the Emergency Department by the Diabetes Care Coordinator. This program also showed patient improvements in several process and outcome measures.
– A Clinical Seminar Series and a Learning Community of Practice was created to exchange ideas on diabetes and cardiovascular best practices and evidence-based guidelines; adopt, diffuse and replicate the quality improvements by operationalizing those best practices and evidence-based guidelines among at-risk patients; and develop strategies and innovations centered on building durable skills among providers for systemic improvement throughout the community. The audiences for this series were clinicians in the community, who received continuing medical education credits for participation in addition to getting chance to share ideas with other community partners.
Recommendations
Based on CCBC’s experience in implementing chronic care management interventions in primary care practices, the key strategies for progress were building trust relationships with partners and allowing flexibility in the implementation to adapt to the circumstances of each partner. Healthcare providers are responding to so many changes simultaneously that it is hard to lay down strict rules about participation without taking into account the timing and nature of the challenge posed by implementers. Also, while we were able to provide some financial incentives for increased commitment from community partners, we recognize that peer pressure and community recognition were also strong motivators that promoted collaborative behavior among providers.
Transitions of Care
Interventions to improve transitions of care in the delivery system were more challenging to implement due to the legal, technical, business, and ideological barriers among the partners. Facilitating any transitions of care requires sharing data across different organizations and providers as well as transforming providers’ practices and workflows on either side of the exchange. When dealing with numerous bilateral relationships, establishing a shared infrastructure and mechanism for this information exchange to take place in a secure and effective manner is essential. Although the community providers had, in principle, agreed on the concept of sharing information as joint applicants to the Beacon Community program and agreement on the DFCSC framework, there were many differences of opinion when it came to the architecture, scope, ownership, and business case for such data sharing among the partners.
The different components of the governance structure were critical to providing direction and making decisions. For example, when efforts to develop a consensus among all providers in the community to share health information centrally was not progressing, the Steering Committee, led by the DHH Secretary, approved the modified strategy of moving forward with a subset of partners (represented in the Operating Board of community providers) who were willing and able to participate in establishing the shared infrastructure.
This decision was made due to the reluctance of some of the large competing health systems to agree on the scope of data sharing. Discussions had stalled progress on the HIT infrastructure development for almost a year in the 3-year project and a modified strategy was critical to proceeding. The HIT subcommittee played a critical role in reviewing different data sharing options and making recommendations to the Operating Board and Steering Committee, and later to the GNOHIE Administrative Committee. The IT solution proposed by the HIT subcommittee to promote transitions of care interventions also garnered community support and was unanimously approved by the governance structure.
The community primary care clinics and the public hospital agreed to work together to demonstrate the use of information technology to improve transitions of care. As a result of this collaboration, the New Orleans community today has a care coordination system that links a network of primary care practice sites with two hospitals. If a patient previously seen at one of these primary care clinics (and who consented to share information) later appears in a hospital emergency department or inpatient setting, a real-time automatic notification goes to the primary care physician (and/or care manager nurse) of record for that patient. This notification is followed by a clinical summary of the encounter so the physician or care manager can plan the continuity of care for that patient after discharge.
Today more than a quarter million patients, mostly uninsured and underinsured, benefit from this system of care coordination. The GNOHIE, which is a community-owned HIE, provides the information technology platform for these transitions of care and can now facilitate other use cases related to specialty referrals, behavioral health integration with primary care, and public health surveillance.
Recommendations
Building a shared technology infrastructure to allow for seamless care coordination across different healthcare organizations is essential for effective transitions of care in the community. The specific architecture and functionalities of the HIT infrastructure should be determined by active involvement of the users early in the process and throughout the implementation of the system. These technologies are then integrated within the day-to-day working of the providers and end-users.
Consumer Engagement through Mobile Health
To reach those at risk of diabetes and cardiovascular disease in the general community, the CCBC program sought to engage consumers, change behavior and encourage early screening. CCBC partnered with a mobile health technology company, the American Diabetes Association, the Centers for Disease Control and Prevention, the ONC and local community organizations to develop the txt4health program that used texting to enroll people possibly at risk for diabetes.
The program provided free assessment to enrollees through an interactive risk assessment text survey. Over a period of 14 weeks customized messages and information were sent to help participants set behavior change goals and identify nearby locations for screening and treatment, and to inform them about healthy activities taking place in their neighborhoods. Txt4health allowed the CCBC to engage non-traditional partners, such as churches, sororities, retailers and health plans, through in-kind support and participation. A consumer advisory group helped in developing messages, strategies and social campaigns for publicizing the txt4health program. Over 1000 people were enrolled in the txt4health program in the first 12 months and it showed high uptake among minorities, obese or overweight populations, and those aged 45 years or less.21
Recommendations
Txt4health initiative helped our community understand the value of using social networks and consumer advisory groups to inform population health efforts that engage the public directly. It also emphasized the potential of new mobile technologies for sending customized, interactive messages to help individuals make healthy behavioral choices.
Lessons Learned / Policy Implications
Community leadership and a strong governance structure made up of community representatives were critical to ensuring smooth and timely implementation of interventions in many Beacon communities.22 Although the CCBC team focused on engaging partners from the beginning, it was critical to adjust the structure and membership during the course of the program to ensure initial intervention testing and implementation as well future sustainability. Specifically, establishing the GNOHIE governance structure as a community-owned entity was critical for sustaining the HIE and other CCBC interventions. The structure is still in operation today.
Providing the DFCSC framework to help guide the partners gave the partnership an important conceptual foundation. The framework helped community representatives understand how policies and actions in one part of the healthcare system affect the others and why it was logical for those representatives to get involved and coordinate among themselves. It also demonstrated the need for connectivity and interoperability among different electronic medical record systems for improved population health management and the meaningful use of HIT in fulfilling those needs.
When it came to designing and implementing its CCM objectives, the CCBC found that developing a community CQI Subcommittee early on and implementing its key clinic interventions in waves proved to be highly effective. With implementation staggered at approximate six-month intervals, first-wave clinics were able to work through challenges and inform other members of the CQI Subcommittee, who then were able to learn and participate in subsequent waves. This method allowed all partners to remain engaged and learn from the early adopters, while also giving the less prepared clinics the flexibility to join when they felt they were ready.
To improve TOC a shared infrastructure and mechanism was deemed absolutely necessary. However, dealing with the legal, technical, and business aspects of all the partner organizations was a Herculean task. The CCBC governance structure was essential to getting agreement on the shared infrastructure. Also critical was the cooperation of the community primary care clinics and the public hospital, who agreed to work together and demonstrate the use of information technology to improve transitions of care. The system worked smoothly because of CCBC’s strategy to focus on primary care practice end users to design and drive the implementation and adoption of the TOC interventions, which established a functional and effective care coordination system enabled by the community health information exchange.
And, finally, the CCBC’s objective of engaging consumers through mobile technology has provided the LPHI and CCBC partners with the opportunity to not only engage directly with consumers but also to collaborate with non-traditional partners, such as churches, retailers and health plans, in improving the health of residents in New Orleans and to benefit from their in-kind support. Initial enrollment in the program was promising and the enthusiasm of non-traditional partners was such that LPHI and the GNOHIE partnership plan to build on it in the future.
The CCBC and its health information technology approach to setting up GNOHIE provided important lessons for the GNO community and health systems implementing various aspects of healthcare reform, particularly those related to population health management and health information technology. Creating a true system of accountable, affordable, and accessible healthcare that includes the most vulnerable populations requires a systems approach that engages and involves the community and always keeps the patient at the center of its intervention design and implementation. While health reform law may have been passed at the federal level and new programs are being announced at the state level, real reform will occur through community partnerships and the joint efforts of providers, payers, government agencies and, most importantly, patients.
Sustainability of CCBC
The Beacon Community Program helped CCBC demonstrate an important lesson for community-wide health information technology programs. First, HIT investments have to be made in a user-defined manner where clinicians and end-users lead the design, scope, and implementation of HIT projects with support of IT professionals. Second, HIT investments are usually expensive and compete for resources with the provision of direct clinical services. It is therefore important that these investments are made with a view to not only current problems but also future opportunities. Third, the governance infrastructure, partnership building, and creation of a learning community have to be given high priority in any HIT effort, as these factors determine the success and sustainability of subsequent implementation and adoption.
Sustainability of the CCBC collaboration, its population health interventions, and the HIT infrastructure built through federal investments were a major challenge to the New Orleans community. The federal funding for CCBC officially ended in September 2013. Since then, several developments have validated the approach of the community partners in building an effective health information technology and community partnership infrastructure.
In October 2013 the CCBC Administrative Committee voted to form a separate nonprofit organization called Partnership for Achieving Total Health (PATH) to manage the GNOHIE. PATH received funding from a local grant through LPHI to provide essential HIE operational funds and the new entity has collaborated with a private company to launch a Medicare Shared Savings Accountable Care Organization (ACO) in New Orleans, which was approved in December 2013.
LPHI also partnered with the Louisiana Primary Care Association to form a Health Center Controlled Network funded by the Health Resources and Services Administration (HRSA) to help approximately 16 FQHCs in Louisiana improve their clinical data quality and ability to report quality measures in a standardized manner. The CCBC infrastructure was then used to collaborate with clinical research entities in Louisiana to apply for a Patient-Centered Outcomes Research Institute (PCORI) grant to form the Louisiana Clinical Data Research Network (LACDRN). In December 2013, PCORI announced a $6.9 million award for LACDRN, which will help use the CCBC and PATH infrastructure for patient-centered clinical research in partnership with other academic research centers in Louisiana.
The partnership built during the CCBC efforts provided transformational improvements in New Orleans’ healthcare delivery system and established an electronic data platform for better population management. That relationship is now expanding beyond its original partners to spread the impact of the CCBC both in scale and scope, not only helping prove the success of the CCBC’s relationship-first approach in introducing technology but also in providing post-Katrina New Orleans with a better coordinated and efficient healthcare system that is benefiting all its regional residents.
Acknowledgments
The authors would like to acknowledge the Office of the National Coordinator for Health Information Technology and its Beacon Community Program team for their financial and technical assistance on the project; the CCBC community partners who participated in the selection and implementation of the interventions and success of the program in New Orleans; colleagues from ICC, Austin Texas who helped develop the DFCSC framework and collaborated with the CCBC team; and Louisiana Public Health Institute’s staff that helped accomplish the many challenging tasks in this project.
Appendix A. Glossary of Abbreviations
| ACO | Accountable Care Organization |
| ADT | Admit, Discharge, Transfer |
| BCBSLA | Blue Cross Blue Shield of Louisiana |
| CCBC | Crescent City Beacon Community |
| CCM | Chronic Care Management |
| CQI | Clinical Quality Improvement |
| DFCSC | Dynamic Framework for a Coordinated System of Care |
| FQHC | Federally-Qualified Health Center |
| ICC | Integrated Care Collaboration |
| HIT | Health Information Technology |
| HRSA | Health Resources and Services Administration |
| GNO | Greater New Orleans |
| GNOHIE | Greater New Orleans Health Information Exchange |
| LACDRN | Louisiana Clinical Data Research Network |
| LA DHH | Louisiana Department of Health and Hospitals |
| LPHI | Louisiana Public Health Institute |
| NOHD | New Orleans Health Department |
| ONC | Office of the National Coordinator for Health Information Technology |
| PATH | Partnership for Achieving Total Health |
| PCASG | Primary Care Access and Stabilization Grant |
| TOC | Transition of Care |
References
- 1.Rudowitz R, Rowland D, Shartzer A. Health care in New Orleans before and after Hurricane Katrina. Health Aff (Millwood) 2006;25(5):w393–406. doi: 10.1377/hlthaff.25.w393. DOI: 10.1377/hlthaff.25.w393. [DOI] [PubMed] [Google Scholar]
- 2.Gillam M, Fischbach S, Wolf L, Azikiwe N, Tegeler P, editors. After Katrina: rebuilding a healthy New Orleans: final conference report of the New Orleans Health Disparities Initiative [Internet] Washington, D.C: Poverty and Race Research Action Council; 2007. May, [Cited 2007 Jul 24]. Available from: www.prrac.org/pdf/rebuild_healthy_nola.pdf. [Google Scholar]
- 3.DeSalvo K, Muntner P, Fox C. Community-based health care for ‘the City that Care Forgot’. J Urban Health. 2005;82(4):520–03. doi: 10.1093/jurban/jti129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rittenhouse D, Schmidt L, Wu K, James W. The post-Katrina conversion of clinics in New Orleans to medical homes shows change is possible, but hard to sustain. Health Aff (Millwood) 2012;31(8):1729–1738. doi: 10.1377/hlthaff.2012.0402. DOI: 10.1377/hlthaff.2012.0402. [DOI] [PubMed] [Google Scholar]
- 5.DeSalvo K, Kertesz S. Creating a more resilient safety net for persons with chronic disease: beyond the “Medical Home.”. J Gen Internal Med. 2007;22:1377–1379. doi: 10.1007/s11606-007-0312-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United States Department of Health and Human Services Office of the National Coordinator for Health Information Technology . Beacon Community Program. {Internet} Washington, D.C.: {Cited 2013 July 21, 2013}. Available at: http://www.healthit.gov/policy-researchers-implementers/beacon-community-program. [Google Scholar]
- 7.United States Department of Health and Human Services Office of the National Coordinator for Health Information Technology . Beacon-Factsheet-CC-NOLA.pdf. {Internet} Washington, D.C.: {Cited 2013 Jul 21}. Available at: http://www.healthit.gov/policy-researchers-implementersbeacon-community-program. [Google Scholar]
- 8.Ricketts T, Goldsmith L. Access in health services research: The battle of the frameworks. Nursing Outlook. 2005;53:274–280. doi: 10.1016/j.outlook.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 9.Elliott TE, Holmes JH, Davidson AJ, La Chance Pierre-Andre N, Andrew F, Steiner JF. Data Warehouse Governance Programs in Healthcare Settings: A Literature Review and a Call to Action. eGEMs (Generating Evidence & Methods to improve patient outcomes) 2013;1(1) doi: 10.13063/2327-9214.1010. Article 15. Available at: http://repository.academyhealth.org/egems/vol1/iss1/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khurshid A. Applying PM [Predictive Modeling] to transform access to healthcare in communities. Predictive Modeling News. 2009;1(9):1–7. [Google Scholar]
- 11.Starfield B, Shi L. The medical home, access to care, and insurance: A review of evidence. Pediatrics. 2004;113:1493–1498. [PubMed] [Google Scholar]
- 12.Hansagi H. Is information sharing between the emergency department and primary care useful to the care of frequent emergency department users? Eur J Emerg Med. 2008;15(1):34–9. doi: 10.1097/MEJ.0b013e3282aa4115. [DOI] [PubMed] [Google Scholar]
- 13.Easton D. A Systems Analysis of Political Life. New York: Wiley; 1965. [Google Scholar]
- 14.Cebul R, Rebitzer J, Taylor L, Votruba M. Organizational fragmentation and care quality in the US health care system. National Bureau of Economic Research; Cambridge: MA: 2008. Working Paper 14212. [DOI] [PubMed] [Google Scholar]
- 15.American College of Emergency Physicians The patient-centered medical home model. Annals Emerg Med. 2009;53:289–291. doi: 10.1016/j.annemergmed.2008.10.020. [DOI] [PubMed] [Google Scholar]
- 16.Oster A, Bindman A. Emergency department visits for ambulatory care sensitive conditions: Insights into preventable hospitalizations. Medical Care. 2003;41:198–207. doi: 10.1097/01.MLR.0000045021.70297.9F. [DOI] [PubMed] [Google Scholar]
- 17.Sidorov JE. The patient-centered medical home for chronic illness: Is it ready for prime time? Health Aff (Millwood) 2008;27:1231–1234. doi: 10.1377/hlthaff.27.5.1231. [DOI] [PubMed] [Google Scholar]
- 18.Davis K, Schoenbaum SC, Audet AM. A 2020 vision of patient-centered primary care. J Gen Internal Med. 2008;20:953–957. doi: 10.1111/j.1525-1497.2005.0178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beacon Community Program BeaconNation Learning Guide. 2013 May; Hawaii Island Beacon Community. [Google Scholar]
- 20.Louisiana Public Health Institute . Crescent City Beacon Community Initiative. {Internet} New Orleans, La.: {Cited 2013, Jul 21}. Available at http://lphi.org/home2/section/3-351/crescent-city-beacon-community-initiative. [Google Scholar]
- 21.Abebe NA, Capozza KL, Des Jardins, Kulick D, Rein A, Schacter A, Turske S. Considerations for community-based mHealth initiatives: insights from three Beacon Communities. J Med Internet Res. 2013;15(10):e221. doi: 10.2196/jmir.2803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rein A. Washington, D.C.: 2012. Beacon Policy Brief 1.0: The Beacon Community Program: Three Pillars of Pursuit. {Internet} {Cited 2013, Dec 3}.Available at: http://www.healthit.gov/sites/default/files/beacon-brief-061912_1.pdf. [Google Scholar]
- 23.Yin RK. Applications of Case Study Research. Thousand Oaks: Sage Publications, Inc; 2012. [Google Scholar]