Abstract
Introduction:
Secure exchange of clinical data among providers has the potential to improve quality, safety, efficiency, and reduce duplication. Many communities are experiencing challenges in building effective health information exchanges (HIEs). Previous studies have focused on financial and technical issues regarding HIE development. This paper describes the Western New York (WNY) HIE growth and lessons learned about accelerating progress to become a highly connected community.
Methods:
HEALTHeLINK, with funding from the Office of the National Coordinator for Health Information Technology (ONC) under the Beacon Community Program, expanded HIE usage in eight counties. The communitywide transformation process used three main drivers: (1) a communitywide Electronic Health Record (EHR) adoption program; (2) clinical transformation partners; and (3) HIE outreach and infrastructure development.
Results:
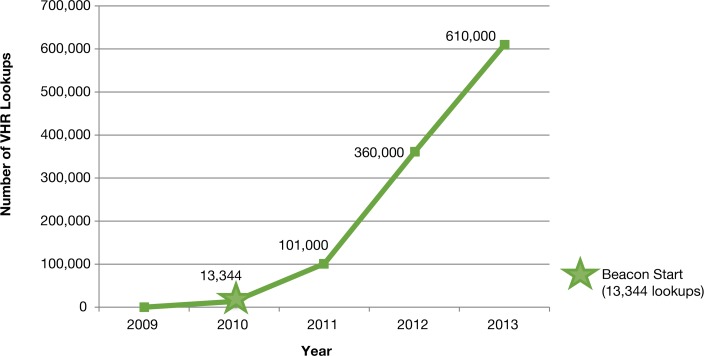
ONC Beacon Community funding allowed WNY to achieve a new level in the use of interoperable HIE. Electronic delivery of results into the EHR expanded from 23 practices in 2010 to 222 practices in 2013, a tenfold increase. There were more than 12.5 million results delivered electronically (HL7 messages) to 222 practices’ EHRs via the HIE in 2013. Use of a secure portal and Virtual Health Record (VHR) to access reports (those not delivered directly to the EHR) also increased significantly, from 13,344 report views in 2010 to over 600,000 in 2013.
Discussion and Conclusion:
The WNY Beacon successfully expanded the sharing of clinical information among different sources of data and providers, creating a highly connected community to improve the quality and continuity of care. Technical, organizational, and community lessons described in this paper should prove beneficial to others as they pursue efforts to create connected communities.
Keywords: Health Information Technology, Platforms, Standardized Data Collection
Introduction
Establishing effective means of health information exchange (HIE) has been cited as critical to the success of the Health Information Technology for Economic and Clinical Health (HITECH) Act’s Meaningful Use program.1 “HIE” refers to the act of electronically transmitting health-related data between organizations, following recognized data and communication standards. HIE refers to a trusted organization that allows a patient’s clinical information to follow when the patient seeks treatment, linking multiple health care entities that are involved in the patient’s care. Secure exchange of clinical data among providers via an HIE has the potential to improve quality, safety, and efficiency.2,3,4,5 However, many communities are experiencing challenges and barriers to building an effective HIE infrastructure. A recent study found that only 30 percent of hospitals and 10 percent of ambulatory practices participate in one of 119 operational HIEs across the United States.6
A literature review published in 2010 documented the barriers to HIE creation.7 The predominant barriers identified were the need for standards, concerns about security, and possible economic loss to competitors. The authors concluded that more research was needed to fully understand interoperability, to overcome the barriers, and to better facilitate HIE.
This paper describes the evolution of the Western New York (WNY) HIE, focusing on WNY’s progress in becoming a highly connected health care community. WNY’s experiences add to the body of knowledge about how to reach a tipping point in achieving successful expansion of electronic HIE. Key lessons learned from the WNY Beacon Community Program are presented, with the goal of documenting the experiences promoting widespread use of a regional HIE, which has potential to inform HIE infrastructure development in other communities.
Background
Effective HIE usage is particularly challenging in health care communities, such as WNY, that are not highly integrated. WNY includes urban, suburban, and rural areas, and there is no single dominant health system. Multiple EHR products are in use by the 27 hospitals in the region. Most primary care practices (309 of 360, 86 percent) are independently owned and operated, and more than 20 ambulatory EHR systems are in use.
In 2001 the four major hospital systems and the three major health insurance plans in the region took the first step toward developing an HIE by creating an administrative data exchange service (HEALTHeNET) that provides a common platform for insurance verification. This communitywide collaborative effort laid the foundation for the creation of the WNY HIE (known as HEALTHeLINK) for clinical information exchange in 2006.
Structure of the HEALTHeLINK HIE
The HEALTHeLINK HIE receives clinical data from hospitals, laboratories, and other organizations, collectively known as “data sources.” Hospitals and other data sources can each potentially provide various types of clinical data including laboratory results; radiology reports and images; other transcribed reports; and admission, discharge, and transfer notifications (ADTs). These data typically reside in different systems within each organization (e.g., a hospital may have separate systems for laboratory data, radiology data, transcribed reports, etc.), which therefore necessitates the creation of multiple different interfaces. Thus, there may be one or more data feeds for each data source.
Organizations that access the HEALTHeLINK HIE clinical data are referred to as “data users” and can access the data in two ways. The preferred means of access is by direct electronic feed into provider EHRs—a process known as “Results Delivery.” By creating an interface between the HIE and the EHR, HEALTHeLINK is able to deliver various forms of data—including laboratory and radiology results; and clinical reports—and view notifications into the provider’s EHR. The data are delivered as computable data files when possible; otherwise they are imported as portable document files (PDFs). Delivery requires the receiving provider to be appropriately indicated at the time of ordering.
For providers without Results Delivery capability, or in situations where the provider is not named and therefore does not receive the results (for example, a specialist orders laboratory tests but the primary care provider is not named in the order), an alternative system is required. In this system, known as the “Virtual Health Record” (VHR), authorized users can log in to a secure online portal from which they can view all available records for their patients and import results into each respective patient’s EHR. These records can only be accessed across the HEALTHeLINK HIE for patients who provide written consent.
New York State has an “opt-in” model of patient consent.8 Under this model, health information for a patient is available through the VHR only if the patient has consented to make the health information available. HEALTHeLINK developed a regionwide process, as opposed to requiring a separate consent for each provider. A single signed “YES” consent allows all health care entities who are providing care for that patient in the network to access that patients’ data via the VHR.
Data Sources
Initial clinical data came into the HEALTHeLINK HIE system in 2008. By early 2010, with the help of funding for New York State’s Health Care Efficiency and Affordability Law (HEAL) program, Phases 1 and 5,9 16 of 27 hospitals in the region, and 1 stand-alone laboratory were connected to and contributing data to the HIE. These data sources were mostly urban. Multiple untapped data sources were identified in the community including rural hospitals, standalone laboratory and radiology facilities, long-term care institutions, home health agencies, and pharmacies. Even among those organizations that were established as data sources, the range of data feeds was limited. Progress in connecting additional data sources and feeds was slow due to limited resources. Barriers included the time and effort required to reach out and establish relationships with new sources. Creation of new interfaces required vendor cooperation, and finding EHR vendors willing to work with the HIE was also a major challenge.
Use of the data at the point of care was also in an early stage of development. Only 23 ambulatory practices initially had the capability for Results Delivery. Although hospitals were by far the biggest data sources, there was very little use of the VHR in these settings. Across the community, 41,553 patients had given consent for VHR access as of Dec. 31, 2009, but there were only 13,344 VHR lookups across all users during 2010.
In summary, at the beginning of 2010, the HEALTHeLINK HIE had reached a modest level of development; however, WNY had built the foundation for expansion.
Creation of the WNY Beacon
In 2010, the Office of the National Coordinator for Health Information Technology (ONC) established the Beacon Community Program to accelerate promising health information technology (HIT) implementation.10 Based on these early efforts by HEALTHeLINK, WNY was selected as one of the nation’s 17 Beacon communities.
The mission of the WNY Beacon Community was to improve clinical outcomes and patient safety through the use of HIT and HIE, focusing on diabetes care management in the eight WNY counties. This aligned with one of the key “Pillars of Pursuit” defined by ONC, namely: “Building and Strengthening HIT Infrastructure.” The main infrastructure goals for the WNY Beacon were to connect all hospitals in WNY to the HEALTHeLINK HIE, and to expand the range of data sources to include long-term care, home health agencies, stand-alone laboratories and radiology facilities, and pharmacies. An additional goal was to expand the range of data shared from these data sources via new data feeds for radiology images, telemonitoring results, medication history, emergency room reports, and physical therapy reports. Furthermore, to make the data in the HIE more readily available to providers, HEALTHeLINK sought to rapidly expand the Results Delivery capability, to obtain consent for VHR lookup from the majority of patients, and to encourage VHR lookup by providers.
Transformation Process
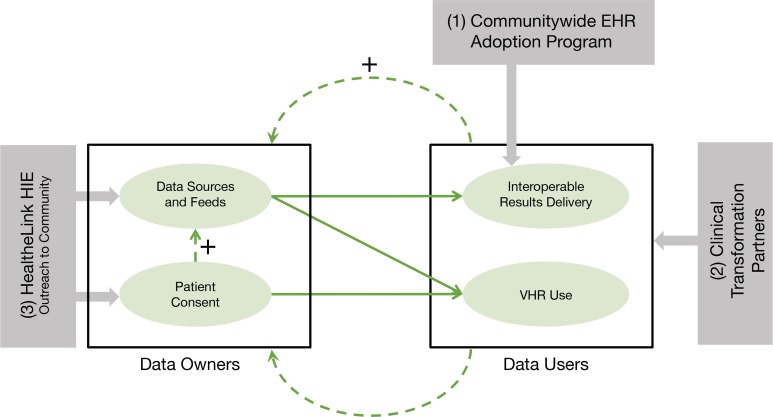
The WNY Beacon Community Model (see Figure 1) was designed to accelerate the growth in development and use of electronic HIE. The communitywide transformation process had three main drivers, shown in Figure 1: (1) a communitywide EHR adoption program; (2) clinical transformation partners; and (3) HIE out-reach and infrastructure development.
Figure 1.
Connected Community: Transformation Process
Communitywide EHR Adoption Program
Prior to the Beacon Community award, a communitywide EHR adoption program for physicians was funded by a New York State Phase 10 HEAL grant9 and by incentive payments from the three major insurers. The availability of funding coupled with HEALTHeLINK technical expertise was instrumental in helping primary care practices in the region to attain EHR capabilities. The EHR adoption program remained in place throughout the WNY Beacon Community grant term.
Through the EHR adoption program, HEALTHeLINK worked with practices for approximately nine months before the ONC Beacon grant began. During this time, HEALTHeLINK established relationships with practices and understood the status of practices in terms of EHR adoption, referral patterns, and connectivity needs. The WNY Beacon leveraged the EHR adoption program resources and experiences. This allowed early identification of practices that had successfully implemented their EHR and were ready to commence use of the HIE. Further, the EHR adoption teams understood practice needs and priorities with respect to accessing data from specific hospitals and laboratories, and the types of data that were most important. This critical knowledge informed decisions about the HEALTHeLINK HIE expansion, as discussed below under HIE outreach and infrastructure development.
Clinical Transformation Partners
The WNY Beacon Community Program was rolled out by the HEALTHeLINK, in collaboration with two clinical transformation partners. The Catholic Medical Partners has a practice network of more than 900 physicians. Their focus is on improving safety, effectiveness, and coordination of medical care. Services to their practices include educational programs, information technology (IT) support, quality improvement initiatives, and health plan advocacy. The P2 Collaborative of Western New York is a Robert Wood Johnson Foundation Aligning Forces for Quality grantee. This not-for-profit corporation was started by two local health plans in WNY and three large practices. This regional collaborative was formed to help improve health care in WNY through a variety of strategies, including setting common quality guidelines and providing reports on the quality of care in the WNY community.
As shown in Figure 1, these two clinical transformation partners focused their efforts on the data users, that is, the organizations that accessed health information from the HIE. Clinical transformation partners had existing and often long-standing relationships with these organizations, especially primary care practices. These relationships were instrumental in launching and engaging primary care practices in the WNY Beacon Program.
Specifically, clinical transformation partners worked with practices to develop workflows and processes to incorporate use of the HEALTHeLINK HIE in clinical practice. This included both Results Delivery and VHR use. Formal Statements of Work were developed to discuss all of the benefits available to the clinical practices, as well as to identify the priorities for each practice. These benefits were described to the practices, and—once prioritized—the clinical transformation partners worked with the practices to assure HIE integration into practice workflow. In addition, the clinical transformation partners worked with primary care providers to support Meaningful Use requirements such as registries, electronic guidelines (EHR prompts and alerts), medication lists and alerts, and practice-level quality improvement projects to improve the care of patients with diabetes mellitus.
HIE Outreach and Infrastructure Development
As indicated in Figure 1, HEALTHeLINK led the HIE outreach and infrastructure development process that focused on Data Owners. For the purpose of this paper, the term “Data Owners” refers to both the data sources that generate clinical data and the corresponding patients. A multipronged approach was used, including adding data sources, creating additional data feeds, expanding the number of data users, and promoting patient consent to access data in the communitywide VHR. This effort was synergistic with the efforts of the Community Transformation Partners.
The WNY Beacon Community grant supported the interface development with EHR vendors to increase the number of data sources and data users. However, funding of the interfaces by itself was not sufficient to get new data sources and engage users. A “value proposition” was created to support these efforts that included the following benefits:
More clinical information available electronically at point of service and able to be used for quality reporting and analysis;
Faster and more efficient transfer of clinical information;
Improved clinical workflow at the provider and practice level;
Improved accuracy of coded data by providing feedback on data quality; and
New opportunities to enhance care management (e.g., medication therapy management).
This value proposition was presented to WNY hospitals that were not already connected to the HIE, as well as to multiple long-term care facilities, home health agencies, stand-alone laboratories and radiology facilities, and pharmacies. The recruitment process involved letter notification, follow-up phone calls, personal visits by project staff, presentations, and ongoing communication at all levels, from clinical staff to senior management. Legal agreements were needed to protect the data and its usage, often necessitating lengthy negotiations.
Prioritization of interfaces for new data sources and new clinical data feeds (e.g., radiology images and hospital discharge medications) was informed by knowledge of users’ needs from the EHR adoption team and the clinical transformation partners. These efforts were leveraged to increase adoption of Results Delivery and VHR usage.
As described earlier, patient consent is needed to access data in the communitywide VHR system supported by the HEALTHeLINK HIE. HEALTHeLINK worked one on one with practices, encouraging providers and their staff to obtain consent at the time of a patient visit. In addition, HEALTHeLINK conducted a broad marketing campaign, using radio, television, and print advertising to inform health care consumers of the benefits of the HIE. The advertisements reinforced the message that patients were getting from their physicians about signing a consent form to participate in the exchange. This effort also increased pressure on physicians who were not yet participating in the HIE.
Toward the end of the Beacon grant term, HEALTHeLINK also began working with practices and EHR vendors to introduce transfer of Continuity of Care Documents (CCDs) at the close of a patient encounter and DIRECT (secure email) in addition to Results Delivery (HL 7 version 2).3,11,12 Results Delivery is the “push” of patient clinical results to their providers. The CCD HL 7 version 3 protocols support these push-based transactions but also support a “pull” of data, that is, the retrieval of data from multiple sources. DIRECT is a push model of HIEs that can be used by providers such as social service agencies who do not have EHRs. HIE deployment of CCD upload and DIRECT capabilities will facilitate transitions of care.
Synergy Among the Three Drivers
One of the most important features of the WNY Beacon Transformation Model (Figure 1) and the three drivers described above is the synergy that exists among the components. The EHR-adoption program prepared practices to participate in HIE. The work of the clinical transformation partners helped to incorporate the HEALTHeLINK HIE into practices. Increasing data usage through Results Delivery and VHR access demonstrated the value of the HIE, spurring the growth in data sources and feeds. As more providers participated as data users, they recruited more patients to participate in the HIE by signing consent. Increased patient and physician participation was used to encourage additional data sources to participate, building further momentum in a virtual cycle.
Results
We present below the results of the WNY Beacon infrastructure expansion efforts, including expansion of the HIE’s data sources and feeds, interoperable results delivery, patient consent, and use of the VHR.
HIE Data Sources and Data Feeds
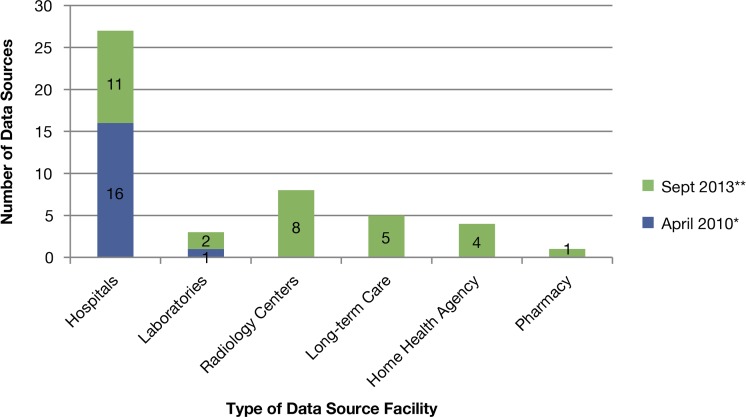
At the start of the ONC Beacon Community grant (April 2010) there were 16 hospitals and 1 laboratory connected to the HEALTHeLINK HIE, as shown by the yellow bars in Figure 2. Over the following three years—as shown by the turquoise bars in Figure 2—11 more hospitals, 2 more labs, 8 stand-alone imaging centers, 5 long-term care facilities, and 4 home care agencies were added. All 11 of the added hospitals were rural hospitals, and the HEALTHeLINK HIE now has 100 percent of the WNY hospitals participating in the network.
Figure 2.
Expansion of Data Sources, by number of facilities, April 2010 to September 2013
Notes: *Blue bars indicate the number of data sources in each category before the Beacon project, in April 2010. **Green bars indicate additional data sources connected during the course of the Beacon project, by September 2013. The total height of each bar shows the total number of data sources in place as of September 2013.
The WNY Beacon project also supported care transitions by creating interfaces for HIE with long-term care organizations and home care agencies. The long-term care and home care agency HL 7 interfaces established in 2012 and 2013 were among the first in the nation to submit and exchange data via an HIE. In addition, a large pharmacy specializing in long-term care, adult care, and infusion service began submitting medication data in 2013.
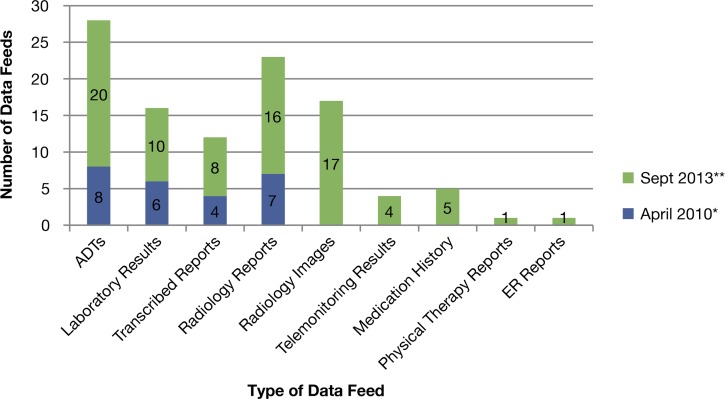
There were four types of data feeds at the start of the grant: Hospital Admission Discharge Transfer notifications (ADTs), laboratory results, transcribed reports, and radiology reports. By the end of the project, as of September 2013, five new types of data feeds had been added: radiology images, telemonitoring results, discrete medication history, physical therapy reports, and emergency room (ER) reports. From 2010 through 2013, the number of ADT feeds increased from 8 to 28, lab feeds increased from 6 to 16, hospital transcription feeds increased from 4 to 12, radiology feeds increased from 7 to 23, and 17 new imaging feeds were created (Figure 3).
Figure 3.
Expansion of Data Feeds, April 2010 to September 2013
Notes: ADTS=Admission, Discharge, and Transfer notifications; ER = Emergency Room.
*Blue bars indicate the number of data feeds of each type before the Beacon project, in April 2010. **Green bars indicate additional feeds created during the course of the Beacon project, by September 2013. The total height of each bar shows the total number of data feeds in place as of September 2013.
Monthly inflow of HIE data has increased as a result of these new data sources and data feeds. In 2013, 20 percent more ADTs flowed into the HIE per month compared to 2010, as well as 12 percent more laboratory results, 66 percent more radiology reports, and 45 percent more transcribed reports. In addition, telemonitoring, ER reports, radiology images, physical therapy, and medication data are now being fed into the HIE.
Interoperable Results Delivery
Six major EHR vendors partnered with HEALTHeLINK to promote adoption and interoperability. The data exchanged started with the ability to send test results via the HIE from the testing facility (laboratories or radiology centers) into the ordering provider’s EHR as discrete data (Results Delivery).
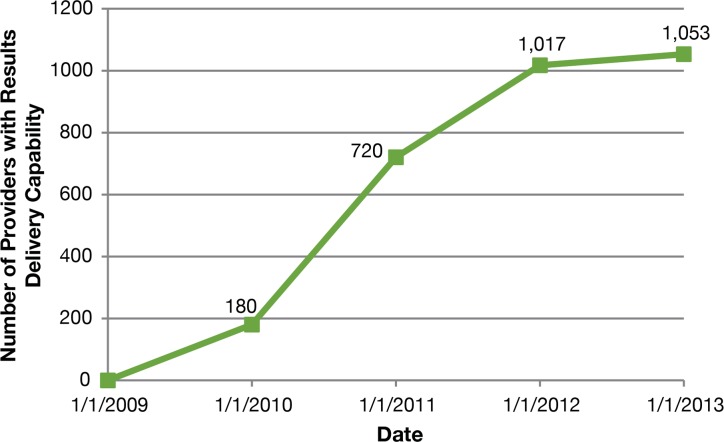
By 2010, 23 practices (with a total of 180 providers) had Results Delivery capability. This was expanded to a total of 222 practices by 2013, corresponding to a total of 1053 providers. Figure 4 shows the growth in the numbers of providers with Results Delivery from 2009 to 2013. During 2013, the last year of the WNY Beacon Community Program, there were more than 12.5 million results delivered electronically (using HL7 messages) to these 1,053 providers.
Figure 4.
WNY Providers with HIE Results Delivery, 2009–2013
Patient Consent
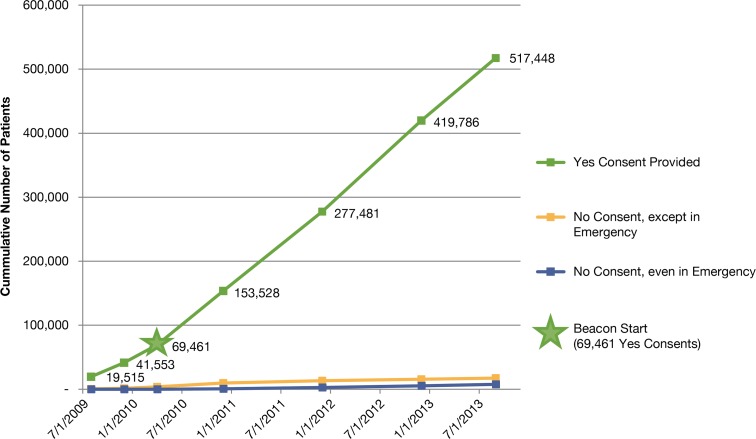
The number of patients who had given consent, allowing their health care providers full access to their clinical data in the HIE (lab, radiology results, medications, test results, discharge summaries, etc.), increased from fewer than 70,000 patients at the start of the Beacon project in April 2010 to over a half million by late 2013 (Figure 5). At the end of 2013, HEALTHeLINK had consent from over a third of the entire WNY population and over 40 percent of adults. More than 58 percent of the population ages 60 years and older had consented. Over the same period, a total of 17,383 of patients had elected to allow access only in an emergency (see the red line in Figure 5) while an additional 7,710 chose to refuse access even in an emergency (see the green line in Figure 5).
Figure 5.
WNY HIE Patient Consents
VHR lookup
Use of the VHR over the course of the Beacon project increased from 13,344 health care data lookups in 2010 to over 600,000 lookups in 2013, as shown in Figure 6. A “VHR lookup” is defined as a user viewing one section of the VHR—for example, laboratory results, or radiology results—regardless of how many discrete results were viewed in each section.
Figure 6.
Patient Virtual Health Record Annual Lookup Totals, 2009–2013
Discussion and Lessons Learned
The ONC Beacon Community grant facilitated HIE expansion and acceleration of both adoption and usage of electronic clinical information exchange to improve patient care. Expected benefits of HIE usage, such as improved continuity of care, reduced duplication of tests, and improved regional analytics, have been reported by the ONC13 and in several recent publications.1–6
However, HIE development is not an easy journey. A variety of challenges have been faced in WNY. Communities need to understand the HIE limitations up front during the planning stage. Electronic data exchange depends on HL7 capabilities that differed dramatically in WNY since there were more than 20 ambulatory care EHR vendors. Challenges, such as variations in code sets, had to be negotiated with each vendor simultaneously. HIE standardization had not been developed in some EHR products and is not fully embraced by all vendors.7,14 Even with EHR vendors using national HL7 specifications, the lack of true standardization generates conversion and mapping issues that take significant time and effort to resolve before HIEs can be established. HIEs will continue to face interoperability challenges until national standards are consolidated and are utilized uniformly by all vendors.
The following three tables summarize the lessons learned in WNY during the three-year grant period and are organized by technical, organizational, and community adoption lessons. Technical lessons are summarized in Table 1, which is organized by data owners. Table 2 presents organizational lessons arranged by themes. Table 3 contains community HIE adoption lessons organized by theme.
Table 1.
Technical Lessons
| Data Owners | Barriers | Solutions | Implications |
|---|---|---|---|
| Hospitals | Age and complexity of software and hardware can create problems. | The HIE needs to analyze current software and hardware to optimize interoperability. | Older, and especially small, rural hospitals need additional resources to participate in the HIE. |
| Hospitals | Hospital systems are not fully integrated and often act as separate entities (pharmacy, ER, etc.). | The HIE needs to plan on having multiple data feeds. | This adds up front costs and ongoing maintenance complexity, since each software product upgrade may require HIE changes. |
| Ambulatory Care Practices and other Data Owners | EHR vendors often have competing priorities (e.g., Meaningful Use, ICD-10) that do not always align with HIE needs; specific barriers include cost of initial development, scarce resources, and competing projects. | A new HIE should consider beginning with vendors that already have interfaces. The HIE needs to work with national partners so that vendors see a wider market rather than developing an interface for just one project. |
Nationwide collaborative efforts such as the Standards and Interoperability (S&I) Framework are critically important for expanding regional HIEs. |
| Long-term Care and Home Care Organizations | Products were developed for in-house use and not for data exchange. | Interface development can be accomplished by working with vendors. | Cost can be prohibitive unless the vendor realizes the benefit of HIE in marketing the product to other customers. |
| Long-term Care and Home Care Organizations | Although these entities recognize the value of interoperability, there are no Meaningful Use incentives to drive adoption. | The HIE needs to provide staff education and assistance with workflow changes. | Even if HIE capability is set up, it will not be used unless staff understand the benefits and workflows are changed. |
Table 2.
Organizational Lessons
| Themes | Barriers | Solutions | Implications |
|---|---|---|---|
| Trust | Organizations are protective of their data and are often reluctant to exchange data electronically. | Utilizing community-based clinical transformation partners is an effective tool to build trust. | HIEs need to build trust before tackling the technical issues. |
| Complexity | Interface development is a slow and tedious process with many vendors. | HIEs need to carefully explain that the process takes time and effort. | Overpromising the benefits to get organizations to participate leads to frustrations. |
| Workflow | Staff members are typically more comfortable continuing their existing routines rather than using new technology. | New workflows need to be developed to integrate HIE into patient care. Utilizing community-based clinical transformation partners is an effective tool in dissemination of successful workflow solutions. |
The workflow redesign cannot be underestimated when promoting HIE usage. It is important to share lessons across the community in order to help other practices adopt and use HIE. |
| Resources | Each organization has its unique own set of circumstances including resource limitations, availability of expertise, priorities, and time limitations. | Expansion of HIEs requires flexibility in scheduling and resource allocation—one practice may need more help with technical issues while another may need more time on workflow. | HIEs need to analyze resources in each organization and establish scopes of work based on the practice capabilities. Establishing rigid deadlines at the start of a communitywide roll out is likely to fail. |
Table 3.
Community Lessons
| Themes | Barriers | Solutions | Implications |
|---|---|---|---|
| Stakeholder Participation | The pressure of competition and fear of violating antitrust laws often keep health care organizations apart. Rural organizations typically are hesitant about collaborating with larger urban organizations. |
HEALTHeLINK was able to convene stakeholders while assuring no areas of competition would be impacted by the HIE process. Key community partners recruited additional organizations. |
The HIE can serve as the neutral playing field when there is not a large dominant health care system. Community partners that everyone trusts can facilitate collaboration and connection to the HIE. |
| Communication Channels | Individuals with the technical expertise to understand HIT and HIE do not “speak” the language of the medical community and do not understand its culture. | HEALTHeLINK created a team with diverse expertise including technical, clinical, and business expertise. Team members had worked for hospitals, practices, and payers, and were familiar with the challenges and priorities of these organizations. |
Technical expertise alone is not enough to successfully expand HIE usage. A combination of expertise and experience is needed to effectively increase HIE usage. Experts with knowledge of both clinical and technical domains are the most effective in communicating to practices. |
| Consent Process | New York is an “Opt-In” state, meaning that patients must sign the required consent form. | Using a communitywide consent form given to patients by their physicians was found to be effective. | The communitywide consent process allows multiple providers to access patient information without the need for duplicate consents. |
| Expansion | HIEs often focus on hospitals and primary care practices. | Reaching out to organizations and provider types (i.e., Transplant Services, dentists, social workers, emergency medical technicians, behavioral health providers, etc.) can add data sources and data users. | Increasing the number of data feeds and data users adds value to the HIE and accelerates usage. |
| Costs and Outcomes | It is difficult to quantify cost savings and outcomes during the rollout. Practice use of the HIE ranged from less than 6 months to more than 3 years. |
Classifying the practices into groups based on the start of HIE was attempted,but about 20% of the providers changed practices during the 3 years and these changes made it difficult to attribute hospitalization data to length of use of HIE. | Additional studies are needed to determine cost savings. |
The ONC Beacon Community funding allowed WNY to achieve the next level in the use of interoperable HIE. Meaningful Use Stage 2 criteria mandate some HIE use. Many hospitals and physician practices throughout the region now qualify for Meaningful Use payments—in part, due to the HIE expansion enabled during this grant.
HEALTHeLINK was also selected by ONC to participate in the “Virtual Lifetime Electronic Record (VLER) Health Communities Program” with the Veterans Administration (VA) for exchange of data over the e-Health Exchange (formerly the Nationwide Health Information Network [NwHIN] gateway). This now allows access to a veteran’s records nationwide, so that access is no longer limited to a geographic area. Expanding HIEs on the regional level will build the platform needed for nationwide data exchange.
Conclusions
Successful expansion and acceleration of HIE in a community such as WNY, with a diverse set of stakeholders in a large geographic area, requires significant financial resources. However, funding is not all that is required. We have described multiple lessons learned during the WNY HIE expansion efforts in technical, organizational, and community adoption domains. Perhaps the most important lesson is that creating the HIE infrastructure requires cooperation and collaboration across the community, trust and engagement of relevant stakeholders, effective communication, and effective technology. Individuals with the technical expertise to understand hardware and software and to create the interfaces typically do not “speak” the language of the medical community and do not understand its culture. Most members of the medical community do not “speak” the technical language and can become frustrated by EHR vendors’ perceived lack of understanding of medical community needs for usability. Lessons from the HEALTHeLINK HIE experience suggest that HIEs should bring in “translators” who understand both cultures.
As a result of the WNY Beacon project, the number of data sources and data users increased rapidly as barriers to HIE implementation were identified and solutions were developed in cooperation with stakeholders. The broad number of feeds now in the HEALTHeLINK HIE (including every hospital in WNY) facilitates better and more efficient care coordination and care transitions. Increased HIE usage has created opportunities to improve the continuity of care by providing increased access to clinical data.
There was not sufficient time during the Beacon grant term to evaluate cost savings. We are confident that significant benefits from HIE usage will occur over the next several years; and additional work is needed for a summative evaluation. The formative evaluation described in this paper can guide HIE development by taking context into consideration. The lessons learned in the process of HIE expansion in WNY can be beneficial to others who are pursuing efforts to create connected communities.
Acknowledgments
The Western New York Beacon Community comprised over 40 community partners. None of the accomplishments would have been possible without the diligent efforts of the staff at HEALTHeLINK, the Catholic Medical Partners, and P2 Collaborative of Western New York. This project was funded by the Office of the National Coordinator for Health Information Technology (ONC).
References
- 1.Gold MR, McLaughlin CG, Berenson RA, Bovbjerg RR. Obtaining providers “buy-in” and establishing effective means of information exchange will be critical to HITECH’s success. Health Aff (Millwood) 2012 Mar;31(3):514–26. doi: 10.1377/hlthaff.2011.0753. [DOI] [PubMed] [Google Scholar]
- 2.Frisse ME, Johnson KB, Nian H, Davison CL, Gadd CS, Unertl KM, et al. The financial impact of health information exchange on emergency department care. J Am Med Inform. Assoc. 2011 Nov 4;19:328–33. doi: 10.1136/amiajnl-2011-000394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shapiro JS, Mostashari F, Hripcsak G, Soulakis N, Kuperman G. Using health information exchange to improve public health. Am J Public Health. 2011 Apr;101(4):616–23. doi: 10.2105/AJPH.2008.158980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuperman GJ. Health-information exchange: why are we doing it, and what are we doing? J Am Med Inform Assoc. 2011 Sep-Oct;18(5):678–682. doi: 10.1136/amiajnl-2010-000021. Published online 2011 June 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hincapie AL, Warholak TL, Murcko AC, Slack M, Malone DC. Physicians’ opinions of a health information exchange. J Am Med Inform Assoc. 2011 Jan-Feb;18(1):60–5. doi: 10.1136/jamia.2010006502. Published online 2010 November 24. Epub 2010 Nov 24. PMID: 21106994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adler-Milstein J, Bates DW, Jha AK. Operational health information exchanges show substantial growth, but long-term funding remains a concern. Health Aff (Millwood) 2013 Aug;32(8):1486–92. doi: 10.1377/hlthaff.2013.0124. [DOI] [PubMed] [Google Scholar]
- 7.Edwards A1, Hollin I, Barry J, Kachnowski S. Barriers to cross-institutional health information exchange: a literature review. J Healthc Inf Manag. 2010 Summer;24(3):22–34. [PubMed] [Google Scholar]
- 8.Consent management for health information exchanges–Optum Insight White Paper [Internet] 2012. Feb 12, [cited 2014 Apr 10]. Available from: https://www.optuminsight.com/∼/media/Ingenix/Resources/White%20Papers/Consent_mgmt_for_hie_wp_09_2012.pdf.
- 9. New York State Department of Health - Health Care Efficiency and Affordability Law (HEAL) for New Yorkers Capital Grant Program [Internet][cited 2014 July 28]. https://www.health.ny.gov/technology/efficiency_and_affordability_law/
- 10.Health IT adoption programs: Beacon community program [Internet] [cited 2014 Apr 11]. Available from: http://www.healthit.gov/policy-researchers-implementers/beacon-community-program.
- 11.D’Amore JD1, Sittig DF, Wright A, Iyengar MS, Ness RB. The promise of the CCD: challenges and opportunity for quality improvement and population health. AMIA Annu Symp Proc. 2011;2011:285–94. Epub 2011 Oct 22. [PMC free article] [PubMed] [Google Scholar]
- 12. The Direct Project Overview. http://www.wiki.directproject.org/file/view/DirectProjectOverview.pdf [Internet] 2014 [cited 2014 Aug 4].
- 13.HIE Benefits [Internet] 2014. [cited 2014 Aug 4]. Available from http://www.healthit.gov/providers-professionals/health-information-exchange/hie-benefits.
- 14.Why is HL7 not plug and play? INTERFACEWARE [Internet] 2014. [cited 2014 Apr 11]. Available from: http://www.inter-faceware.com/why_is_hl7_not_plug_and_play_.html.