Abstract
Background and Introduction:
Disease registries, as part of electronic health records (EHRs), have shown promise in improving care and outcomes. However, little is known about how best to implement them across communities, especially in communities that are not highly integrated. The Western New York (WNY) primary care community consists largely of independent practices using at least 20 different EHR products. This paper discusses the processes undertaken to develop a communitywide EHR disease registry in WNY, improvements it engendered, barriers overcome, and the lessons learned.
Methods:
HEALTHeLINK, under the Office of the National Coordinator for Health Information Technology Beacon Community Initiative, reached out to 98 primary care practices in the WNY region to establish EHR-based diabetes registries. Working with practices, community partners, and vendors, registry specifications were created. The registry was piloted with practices using one local vendor’s EHR product and then rolled out to other practices, including five other EHR products. Using identified and de-identified registry datasets, quality benchmarking within and between practices and population health management were undertaken.
Findings:
From 2011 to 2013, the WNY Beacon Community assisted 98 practices (344 providers) serving over 50,000 adult diabetic patients. A major focus was on EHR registry development across diverse systems, and overcoming the challenges this presented. The Beacon diabetes registry was implemented at 85 of the 98 targeted practices. Of these registries, 65 met the criteria described in a later section for quality benchmarking and population health management purposes. Practices received quarterly benchmark reports summarizing their performance on key diabetes quality metrics and were compared to community practice averages. Practices used their registries for population health management by identifying and targeting patients in need of follow-up or specific diabetes-related care.
Discussion and Conclusion:
The creation of the registry infrastructure required unified registry technical specifications as well as close collaboration between all parties involved. The WNY experience showed that a useful disease registry can be established in a community largely consisting of numerous disparate primary care practices. This laid the groundwork for the future use of EHR data for a variety of purposes in the community. The methods used and lessons learned through this endeavor may benefit other communities in a similar position, with several disconnected EHRs, to establish unified registries.
Keywords: Health Information Technology, Platforms, Quality Improvement
Background
The Western New York (WNY) region is an open model of health care. The majority of physician practices are small and independently owned—there is no dominant health system. A consequence of this open model is that there are many different electronic health records (EHRs) in use in WNY.
The Office of the National Coordinator for Health Information Technology established the Beacon Community Initiative in 2010 to accelerate promising health information technology (HIT) implementation.1,2 WNY was selected as one of the 17 Beacon communities. HEALTHeLINK, the local Regional Health Information Organization (RHIO) was the lead agency for the WNY Beacon program. The overarching goal of the WNY Beacon program was to improve diabetes care in primary care settings across WNY. This effort builds on other community health care system and Health Information Exchange initiatives including Aligning Forces for Quality (AF4Q),3 the New York State Healthcare Efficiency and Affordability Law (HEAL NY),4 and EHR adoption programs from the three largest health plans in the community.
Health information exchange (HIE) has the ability of supporting interoperability of automated health data and can facilitate important improvements in health care quality.5 To date, HIEs have focused on integrating data from hospitals, laboratories, and radiology facilities. Integrating data from private primary care practices has proven much more difficult.6
Critical to the management of chronic diseases, such as diabetes, is the ability to run reports or “registries.” A registry is a list of patients meeting certain criteria (e.g., diagnosis of diabetes mellitus) and can include relevant clinical data such as laboratory values, vital signs, and dates of office visits and vaccinations. Registries can be used to identify patients who are in need of specific interventions, such as lab tests, follow-up, and vaccinations. In addition, they can be used to generate quality measures at the physician or practice level, such as the percentage of eligible patients achieving disease control. Electronic disease registries are viewed as important clinical information systems within the Chronic Care Model (CCM),7,8 and there is evidence that they can contribute to improved care (e.g., increased rates of testing for HbA1c) and intermediate outcomes (e.g., lower HbA1c, and lower blood pressure) in diabetes.9–11 Communitywide registries provide information on populations, not just individual patients and practices. This information can be very valuable to address disparities, quality, and value. While there have been reports of such efforts in integrated health care systems,12 the difficulties in other settings have been highlighted.6,13
In this paper we describe the development of a communitywide WNY registry from 2011 to 2013. This endeavor required several key strategies focusing on individual practices, EHR vendors, and community consensus. The WNY Beacon program made significant advances in establishing a communitywide EHR disease registry in WNY, overcoming many barriers and learning many lessons that may be of help to other communities looking to establish communitywide disease registries.
Methods
The Strategy
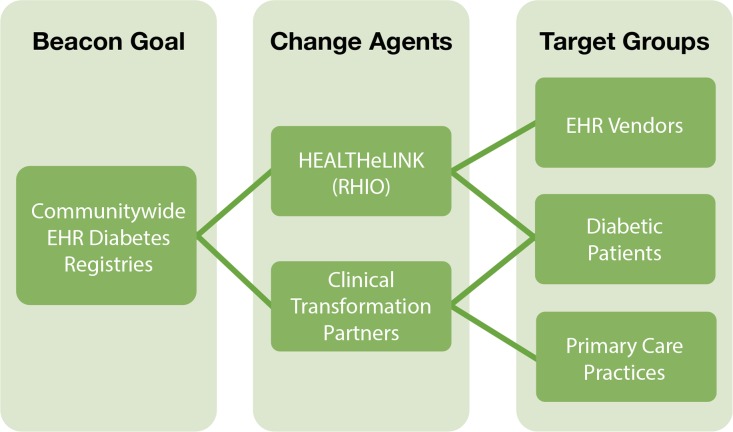
HEALTHeLINK, the lead agency for the WNY Beacon Community Initiative, established the goal of creating a communitywide diabetes registry that could be widely adopted and supported by the community. Three target groups were identified as necessary to accomplishing this goal: primary care practices, EHR vendors, and diabetic patients. Change agents were deployed to move each group toward the goal of a communitywide diabetes registry and address the barriers that were encountered in the process. This strategy is illustrated in Figure 1. As shown, HEALTHeLINK interfaced most closely with the EHR vendors. Two Clinical Transformation Partners (CTPs) were engaged to work with primary care practices. Table 1 summarizes the characteristics of the CTPs: Catholic Medical Partners—an Independent Practice Association (IPA); and the P2 Collaborative of WNY—a not-for-profit corporation with membership from all eight WNY counties.
Figure 1.
Strategy
Table 1.
Clinical Transformation Partners
| Clinical Transformation Partner: | Catholic Medical Partners (CMP) | P2 Collaborative of Western New York |
| Organizational Structure: | Independent Practice Association | Informal Collection of Providers |
| Number of Practices Enrolled in WNY Beacon: | 65 | 33 |
| Number of Physicians: | 152 | 192 |
Communitywide Registry
The purpose of the community diabetes registry was to improve care for patients with diabetes: (1) by providing primary care practices with a population health management capability of generating a list of their patients with diabetes and tracking preventive and recommended care for this population (such as follow-up, vaccination, laboratory testing, etc.); and (2) to drive quality improvement by providing practices with feedback regarding their performance on diabetes quality of care metrics over time, benchmarked in comparison with their peers. The clinical goals for diabetes control were prespecified as: Hemoglobin A1c (HbA1c) <9.0, Low Density Lipoprotein (LDL) <100mg/dL (both within the past year), urine microalbumin/creatinine ratio resulted within the past year, most recent blood pressure with systolic <140 and diastolic <90; documented influenza immunization within the past year, and pneumonia immunization within the past 10 years.
The first step in developing this communitywide registry was to reach agreement on a uniform data structure and registry format to be utilized across practices. To develop these specifications, HEALTHeLINK reached out to practices, CTPs, (see Table 1), and EHR vendors to identify the information that these stakeholders believed was most important for quality benchmarking for diabetic patients and for a meaningful communitywide registry. In addition, HEALTHeLINK has a long-standing Physician Executive Committee (PEC) for obtaining physician input. This group consists of influential and well-known members of the physician community. The PEC provided oversight and approved the final specifications for the registry. These stakeholders also established consensus regarding how and what information would be shared across practices in benchmark reports.
Developing Registries with EHR Vendors
In WNY, the participating practices used several different EHRs, each EHR having varying capabilities for generating reports and registries. The first step was to determine registry capability for each EHR product being used by the participating practices. This involved partnering with both practices and vendors.
The effort started with the dominant local EHR vendor (Medent), to create the customized registry report based on the registry specifications agreed upon by the community. The project team worked closely with each practice to appropriately map the data from the practice EHR to the community registry because the practices used different field labels and data types to collect the targeted information (e.g., smoking, smoking cessation as a procedure, part of social history, problem list, patient history, etc.).
After the development of the registry in Medent, which took several months, WNY Beacon began working with other EHR vendors. Registries were developed with five additional EHR products by the end of the grant period; two worked with WNY Beacon to create registries (eClinicalWorks and NextGen). Three were flexible enough to allow workarounds (Allscripts Enterprise, Allscripts Professional, and Sage). Some practices used a third-party data-collection intermediary (Extract Transform Load, ETL) tool or developed their own report template based on business intelligence software that was part of the EHR.
HEALTHeLINK communicated the local vendor’s specifications to the other vendors, but data mapping had to be tailored to each vendor. Registry rollout in each practice included HEALTHeLINK as an intermediary between practice and vendor to adapt the registry mapping for each practice for that vendor. In some cases, internal practice information technology (IT) staff assisted with the development of the reports.
Even with the defined registry specifications, and the efforts described above, data extracts were inconsistent. For example, some data were provided as text rather than in numeric form, and date formats varied. Rather than spending additional time working with the vendors to perfect the registries, normalization was done after extraction in order to permit combination of data sets across practices. Examples of normalization include the following: converting text to numeric formats; coding nonstandardized free text data such as race, ethnicity, language, and smoking status; stripping off extraneous text; and recoding laboratory values reported as “less than” (or “<”) to a standardized code. To the extent possible, this was accomplished using automated algorithms in the form of macros. Nevertheless, it still involved considerable manual effort.
Data Quality Assurance
Before data could be used for quality benchmarking and population health, it was necessary to determine the quality of the data. To characterize data quality, each of the participating practices was provided with a quarterly report containing a series of graphs that summarized the proportion of missing and invalid data in the clinical registry. This data quality report was used to improve data mapping and work with the EHR vendors to improve data collection. In addition, missing or invalid data elements were reviewed with practice staff to improve data capture at the practice level. The CTPs were sometimes able to assist practices in addressing these issues with the EHR vendors and, when this was not effective, would share this information with HEALTHeLINK, who would then follow up with the vendor. Once practices felt comfortable using the data (based on the quality of the registry), they began using it for quality benchmarking and population health management.
Using the Registries for Quality Improvement in Primary Care Practices
The CTPs worked closely with each practice, assisting them in setting up and maintaining their diabetes patient registries for both population health and benchmarking purposes. In addition to simply accessing the registries, the CTPs helped practices use this information to improve patient care, including working with practices in establishing workflows to provide appropriate follow-up and to track patient adherence with lab testing and preventive services.
Results
Registry Setup
By the end of the project, 85 of the 98 (87 percent) practices had developed a Beacon diabetes registry and submitted at least one extract to the HIE (HEALTHeLINK). These registries were developed to support organized care management of approximately 47,000 patients with diabetes in WNY. Of the remaining 13 practices who were unable to develop the Beacon registry, most were solo practitioners. They were able to run simple registry reports from their EHRs, but could not develop the more complex Beacon registry (see Table 2). Barriers included lack of dedicated IT staff in these practices who could work closely with the EHR vendor and HEALTHeLINK to implement the required data mappings and extraction needed to create the registry. Identifying comorbidities by ICD-9 codes in the problem list proved to be the most difficult challenge. Furthermore, most of these 13 practices used EHRs with low penetration in the WNY Beacon Community. These EHR vendors typically had little interest in partnering to create a customized registry—likely because their effort would benefit only a small number of practices.
Table 2.
WNY Beacon Diabetes Registry Elements
|
Registry Data Quality
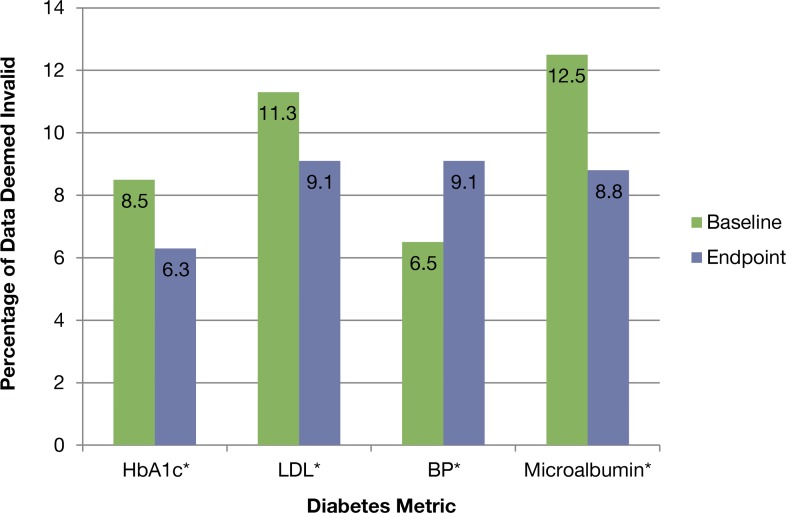
Figure 2 shows the change in the percentage of reported data that were deemed invalid, for each of four diabetes metrics, from March 2012 to June 2013—data across all 85 practices with registries. All differences are statistically significant (p<.001). As shown, the rate of invalid BPs increased from 6.5 percent at baseline (first quarter of 2012) to 9.1 percent at endpoint (second quarter of 2013). Invalid BPs included text such as “sitting” or “right arm” or numbers outside the acceptable range (ranges given in Footnote to Figure 2). It is not clear why this increased from baseline to endpoint.
Figure 2.
Percentage of Registry Data Deemed Invalid: Baseline (Q1 2012) to Endpoint (Q2 2013)
Notes: *Difference (baseline to endpoint) is significantly different at p<.001. Values represent the percentage of reported data that were deemed invalid (value or date not within an acceptable range). Acceptable ranges for laboratory values were: HbA1c 1 – 100%; LDL 1 – 300 mg/dL; Systolic BP 50–300 mmHg; Diastolic BP 35–200 mmHg; microalbumin/creatinine ratio 0–5000. Valid dates were within 12 months prior to the registry run date.
Among the 85 practices that set up a Beacon diabetes registry, 65 (76 percent) successfully generated registries each quarter that were deemed acceptable for quality benchmarking and population health management purposes. The other 20 practices had significant variances with completeness or consistency of their registry. Problems included excessive amounts of missing data due to failure to maintain data mappings, inconsistent use of data fields, or wide fluctuations in the numbers of patients reported due to changes in numbers of providers in the practice. HEALTHeLINK and the CTP reviewed these registries with the practice and came to a mutual agreement that the data lacked credibility for quality benchmarking.
Quality Benchmarking for Diabetic Patients
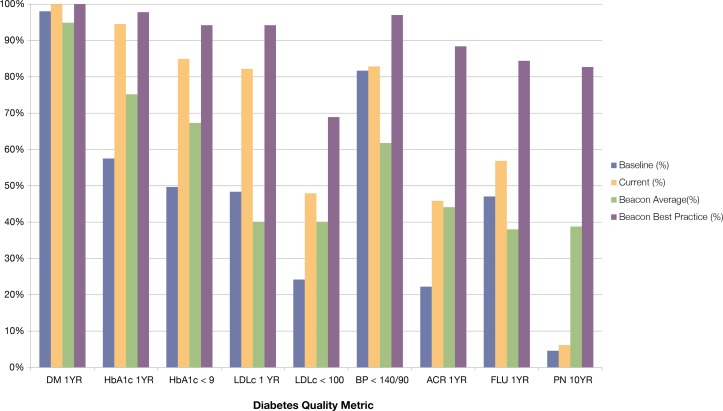
Each quarter, practices that submitted registry data received a benchmark report summarizing their performance on key diabetes quality metrics. In an effort that will be published separately, each practice, with guidance from its CTP, conducted Plan, Do, Study, Act (PDSA) cycles aimed at improving diabetes care quality. In brief, each practice worked with its CTP, reviewing the previous assessments and benchmark reports, to identify areas for improvements and corresponding goals. Improvement plans were developed and implemented, including workflow changes as needed. Reports from subsequent quarters were used to measure progress toward goals and adjust plans as needed.
Figure 3 is an example of a benchmarking report for one practice. This practice began the Beacon project with baseline performance (blue bars) that was below the mean for Beacon practices (green bars, labeled “Average” in the benchmark report) on several metrics. This information helped the practice to focus its improvement efforts, and by the second quarter of 2013 (red bars) the practice was exceeding the Beacon mean and approaching the “Beacon Best Practice” level (purple bars in Figure 3, indicating the highest level achieved for that measure by a Beacon practice with registries).
Figure 3.
Example of Practice Benchmark Report
Notes: DM 1YR = type of Diabetes Mellitus (1 or 2) was specified; HbA1c 1YR = Hemoglobin A1c was recorded within the last year; HbA1c<9 = HbA1c result <9.0 within lastyear; LDLc 1YR = Low Density Lipoprotein (LDL) recorded in last year; LDLc<100 = LDL result <100mg/dLwithin last year; BP<140/90 = Most recent blood pressure systolic <140 and diastolic <90; ACR 1YR = microalbumin/creatinine ratio (ACR) recorded within lastyear; FLU 1YR = Influenza immunization recorded within lastyear; and PN 10YR = Pneumonia immunization recorded within last 10 years.
Population Health Management for Diabetic Patients
As explained earlier, the goal of implementing the registries in primary care practices was twofold. The main focus was on quality benchmarking, as described above. The second purpose for was population health management. Specifically, practices were encouraged to focus on patients with uncontrolled diabetes. The 65 practices that were able to consistently generate an acceptable registry had a total of 12,789 out of 37,918 patients (33.7 percent) that were classified as uncontrolled (HbA1c> 9) in the third quarter of 2012. CTPs helped practice staff to target these patients for follow-up, and for additional interventions, as necessary. Results of this effort will be reported elsewhere.
Lessons Learned
Technical Lessons
Establish clear technical specifications for the registry
HEALTHeLINK, as the RHIO, understood what was needed to implement the communitywide registry based on technical specifications from each vendor. HEALTHeLINK acted as liaison between practices and EHR vendors. HEALTHeLINK needed to engage vendors up front to create buy-in for registries before the technical specifications could be presented. This required HEALTHeLINK to convert the clinical requirements into technical specifications that the vendors could understand.
Invest effort in data mapping
Documenting data mapping capabilities up front is a key step. Mapping involves identifying how and where each required data element is stored in each specific EHR system and extracting it to the correct data field in the registry. Mapping capabilities are dependent upon product capabilities, practice staff capabilities, and the willingness of EHR vendors to collaborate in the process of mapping data elements across multiple data sources, while handling complexities such as differing units. The ability of CTPs in the WNY Beacon practices to facilitate this process was also important to understand at the beginning of the project. Mapping efforts may be simplified by working with data sources. For example, the authors recommend that communities consider working with laboratories to create a communitywide compendium of laboratory test codes.
Anticipate the need for data normalization
Investing greater time and effort in perfecting data mapping and extraction procedures can lessen the need for post hoc normalization. The WNY Beacon Community chose to move ahead with imperfect extracts and had to expend considerable effort in data normalization. Over time, as practices improved their procedures, less effort was required, but some amount of effort will likely be needed until such time as complete interoperability between systems is achieved. Therefore, the challenge is to strike the right balance. Based on the WNY experience, the authors recommend working with EHR user groups to create communitywide consistent practices—especially regarding consistent coding—with the goal of improving the uniformity of data, entering the community registry, and minimizing the effort required to normalize the data.
Develop clear protocols to support practice staff
Practices needed clear protocols to support practice staff understanding how to run registries. Registry creation and file transfer issues had to be resolved by project staff. Multiple steps were often required to run and upload the registries. Practices only had to run registries quarterly, so step-by-step instructions were needed to remind practice staff about the process.
Understand that practices and vendors are both overwhelmed and don’t speak the same language
HEALTHeLINK acted as an intermediary, with technical, clinical, and business expertise. CTPs needed to translate clinical goals into technical specifications, allowing HEALTHeLINK to create standardized specifications for vendors. As practices were able to resolve the issues, lessons learned were shared across practices.
Anticipate that vendors have competing priorities
The local vendor was more willing to work closely with HEALTHeLINK to develop and refine the registry functionality. National vendors were more difficult to work with due to competing demands. Development of a customized, disease-focused registry was not attractive to national vendors. Vendors felt that investing in a small region of the country or developing a specific disease-focused registry had limited value. This was especially problematic due to time pressure to meet Meaningful Use (MU) Stage 1 and Patient-Centered Medical Home (PCMH) requirements. Some vendors did not cooperate at all while some offered to work via third-party ETL products.
Learn how to work with vendors
Vendors recommended providing one point of contact from the WNY Beacon Community to avoid overburdening vendors’ staff. It was necessary to work closely with vendors to develop data extraction methodology. Conducting a pilot test with one major vendor helped the project gain momentum. The pilot allowed the team to iron out technical issues and identified gaps in the design and workflow. Starting small with a local vendor gave the project a greater opportunity for success. HEALTHeLINK rolled out the registry to more vendors as expertise was gained.
Implementation Lessons
Learn how to work with practices
While creating communitywide registries looked straightforward on paper, rollout was slow and took over a year for 98 practices that each had unique characteristics. What worked in one practice might not work in another. Project staff needed to understand each practice’s resource limitations, priorities, and existing timelines. Changes could only be made in small increments. A critical step was to identify and nurture an information technology champion. Leveraging existing community resources also helped get the registry development started. Practice expertise was used where available and homegrown solutions, e.g., mappings and workarounds, were shared among practices.
Address data sharing concerns up front
Several providers expressed concern about sharing EHR data outside of the practice, resistance to allowing an outside party into the practice (especially with regard to HIPAA), and trepidation about being compared to other practices. In addition, some practices felt overwhelmed with other priorities and incentive programs, quality improvement-and research studies, including MU and PCMH.
The following strategies appeared to be the most important in helping to overcome this resistance.
Use peer group to provide legitimacy
As described earlier, HEALTHeLINK’s PEC consists of influential and well-known members of the physician community who provided oversight of the specifications for the registry. This committee’s approval of the communitywide registry was reassuring to many providers. Knowing that trusted colleagues were part of this project helped assuage concerns about data sharing and the burden on the practice.
Leverage existing relationships to gain momentum
All practices in the WNY Beacon were affiliated with one of the community partner organizations. The CTPs had built and established relationships by working with practices, often over a prolonged period, on quality improvement and other activities, frequently involving protected health information (PHI). Leveraging these pre-existing relationships was instrumental in achieving a high degree of participation in the WNY Beacon Community.
Gain buy-in by showing value to practices
The two goals of the registry, quality benchmarking and population health management, both met important practice needs. Requirements for MU and PCMH certification fueled practice interest in both quality benchmarking and population health management. The positive experience with both of these functions among the early adopters had a positive influence on others, via professional and social networks. Giving practices feedback about the quality of their registry and benchmarking helped to create buy-in and to sustain registry use.
Discussion
Developing a communitywide EHR disease registry in primary care practices requires significant commitment and close collaboration with vendors. Engagement of practices requires effective communication to overcome resistance to sharing data.
Setting up the registries was technically challenging. Many individuals with the technical expertise to understand vendors do not “speak” the language of the medical community and do not understand its culture. Members of the medical community typically do not speak the technical language and may become frustrated by EHR vendors’ perceived lack of understanding of their needs for usability.
Feedback on the quality of their own data was important to practices. Practices felt an ownership of the data, since it came from their own EHRs and not from claims or other external sources. The fact that the proportion of invalid data declined over time (with the exception of blood pressure data) suggests that the feedback was helpful to practices and helped them to focus their efforts to improve registry data quality. The improvements shown in Figure 2 are modest. Their significance lies in: (1) the demonstration that practices succeeded in improving their registry mapping and extraction processes; and (2) the greater credibility that comes from improved data quality. Maintaining invalid data rates at 10 percent or less was considered a success.
Mechanisms to sustain the population health collaborations are being explored. This project has spawned an additional pilot, using registries to collect Healthcare Effectiveness Data and Information Set (HEDIS) measures from the practices to provide to the health plans. The three largest health plans in the region are funding this project.
While development of registries was the immediate goal, another important result of the communitywide registry initiative was that it created a precedent and a roadmap for future efforts using EHR data. Leveraging the collaborative partnerships that were forged by this project may be the most lasting and impactful outcome.
It is hoped that the lessons learned through this endeavor may benefit other communities, especially those with multiple, disconnected EHRs, to establish unified registries to leverage EHR data for improved care and improved population health (see Tables 3 and 4).
Table 3.
Findings
| Findings |
|---|
|
Table 4.
Lessons Learned
| Lessons Learned |
|---|
Technical Lessons
|
Implementation Lessons
|
Acknowledgments
The Western New York Beacon Community was comprised of over 40 different community partners. None of the accomplishments would have been possible without the diligent efforts of the staff at HEALTHeLINK, the Catholic Medical Partners and P2 Collaborative of Western New York. This project was funded by the Office of the National Coordinator for Health Information Technology (ONC).
Footnotes
Disciplines
Health Services Research
References
- 1. Beacon Community program [Internet][cited 2014 Apr 11]. Available from: http://www.healthit.gov/policy-researchers-implementers/beacon-community-program.
- 2.McKethan A, Brammer C, Fatemi P, Kim M, Kirtane J, Kunzman J, Rao S, Jain SH. An early status report on the Beacon Communities’ plans for transformation via health information technology. Health Aff (Millwood) 2011 Apr;30(4):782–8. doi: 10.1377/hlthaff.2011.0166. [DOI] [PubMed] [Google Scholar]
- 3. Aligning forces for quality: Improving health & health care in communities across America [Internet] 2014 [cited 2014 Apr 11]. Available from: http://www.forces4quality.org.
- 4. Health Care Efficiency and Affordability Law for New Yorkers Capital Grant Program [Internet][revised 2010 Jul; cited 2014 Apr 11]. Available from: http://www.health.ny.gov/technology/efficiency_and_affordability_law.
- 5.Kuperman GJ. Health-information exchange: why are we doing it, and what are we doing? J Am Med Inform Assoc. 2011 Sep-Oct;18(5):678–682. doi: 10.1136/amiajnl-2010-000021. Published online 2011 June 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fairbrother G, Trudnak T, Christopher R, Mansour M, Mandel K. Cincinnati Beacon Community Program highlights challenges and opportunities on the path to care transformation. Health Aff (Millwood) 2014 May;33(5):871–7. doi: 10.1377/hlthaff.2012.1298. [DOI] [PubMed] [Google Scholar]
- 7.Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH. Improving the quality of health care for chronic conditions. Qual Saf Health Care. 2004 May 22;13:299–305. doi: 10.1136/qshc.2004.010744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. The Milbank Quarterly. 1996;74(4):511–44. [PubMed] [Google Scholar]
- 9.O’Connor PJ, Desai J, Solberg LI, Reger LA, Lauren-Crain A, Asche SE, et al. Randomized trial of quality improvement intervention to improve diabetes care in primary care settings. Diabetes Care. 2005 Aug;28(8):1890–7. doi: 10.2337/diacare.28.8.1890. [DOI] [PubMed] [Google Scholar]
- 10.Peterson KA, Radosevich DM, O’Connor PJ, Nyman JA, Prineas RJ, Smith SA, et al. Improving diabetes care in practice: Findings from the TRANSLATE trial. Diabetes Care. 2008 Dec;31(12):2238–43. doi: 10.2337/dc08-2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weber V, Bloom F, Pierdon S, Wood C. Employing the electronic health record to improve diabetes care: a multifaceted intervention in an integrated delivery system. J Gen Intern Med. 2008 Mar 29;23(4):379–82. doi: 10.1007/s11606-007-0439-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DeVoe JE, Sears A. The OCHIN community information network: bringing together community health centers, information technology, and data to support a patient-centered medical village. J Am Board Fam Med. 2013 May-Jun;26(3):271–8. doi: 10.3122/jabfm.2013.03.120234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eggleston EM, Klompas M. Rational use of electronic health records for diabetes population management. Curr Diab Rep. 2014 Apr;14(4):479. doi: 10.1007/s11892-014-0479-z. [DOI] [PubMed] [Google Scholar]