Abstract
Context:
Electronic health records (EHRs) have been promoted as a key driver of improved patient care and outcomes and as an essential component of learning health systems. However, to date, many EHRs are not optimized to support delivery of quality and safety initiatives, particularly in Intensive Care Units (ICUs). Delirium is a common and severe problem for ICU patients that may be prevented or mitigated through the use of evidence-based care processes (daily awakening and breathing trials, formal delirium screening, and early mobility—collectively known as the “ABCDE bundle”). This case study describes how an integrated health care delivery system modified its inpatient EHR to accelerate the implementation and evaluation of ABCDE bundle deployment as a safety and quality initiative.
Case Description:
In order to facilitate uptake of the ABCDE bundle and measure delivery of the care processes within the bundle, we worked with clinical and technical experts to create structured data fields for documentation of bundle elements and to identify where these fields should be placed within the EHR to streamline staff workflow. We created an “ABCDE” tab in the existing patient viewer that allowed providers to easily identify which components of the bundle the patient had and had not received. We examined the percentage of ABCDE bundle elements captured in these structured data fields over time to track compliance with data entry procedures and to improve documentation of care processes.
Major Themes:
Modifying the EHR to support ABCDE bundle deployment was a complex and time-consuming process. We found that it was critical to gain buy-in from senior leadership on the importance of the ABCDE bundle to secure information technology (IT) resources, understand the different workflows of members of multidisciplinary care teams, and obtain continuous feedback from staff on the EHR revisions during the development cycle. We also observed that it was essential to provide ongoing training to staff on proper use of the new EHR documentation fields. Lastly, timely reporting on ABCDE bundle performance may be essential to improved practice adoption and documentation of care processes.
Conclusion:
The creation of learning health systems is contingent on an ability to modify EHRs to meet emerging care delivery and quality improvement needs. Although this study focuses on the prevention and mitigation of delirium in ICUs, our process for identifying key data elements and making modifications to the EHR, as well as the lessons learned from the IT components of this program, are generalizable to other health care settings and conditions.
Keywords: 2014 EDM Forum Symposium, Learning Health System, Health Information Technology, Quality Improvement, Standardized Data Collection
Context
Electronic health records (EHRs) have been promoted as a key driver of improved patient care and outcomes and as an essential component of learning health systems. However, many current EHRs are not optimized to support delivery of quality and safety initiatives—particularly in Intensive Care Units (ICUs)—and do not facilitate efficient clinical workflow, adequate data capture, or real-time performance feedback necessary to achieve improvements in care. EHR customization can be a driver for health care systems to improve the adoption of quality improvement and patient safety initiatives, including evaluation of the impact these initiatives have on patient care and outcomes. This case study describes how an integrated health care delivery system modified its inpatient EHR to facilitate the implementation and evaluation of a safety and quality initiative (deployment of the ABCDE bundle), for the prevention and mitigation of delirium in ICU patients. The ABCDE bundle consists of the following five elements: awakening trials with reduction in the use of sedating medications, breathing trials to wean patients off mechanical ventilation faster, coordination of awakening and breathing trials to maximize their benefits, delirium screening and management, and early progressive mobility to prevent muscle weakness (Table 1).
Table 1.
ABCDE Bundle Elements and Main Safety Criteria
| Element | Description | Safety Criteria | |
|---|---|---|---|
| A | Spontaneous Awakening Trial (SAT) | Awaken patients daily with cessation of sedating medications. | No active seizures No alcohol withdrawal No agitation No paralytics No myocardial ischemia Normal intracranial pressure |
| B | Spontaneous Breathing Trial (SBT) | Daily assessment of patients’ readiness to discontinue mechanical ventilation | No agitation Oxygen saturation ≥ 88% FiO2 ≤ 50% PEEP ≤ 7.5 cm H2O No myocardial ischemia No vasopressor use Inspiratory efforts |
| C | Coordination | SAT conducted prior to SBT; Coordination between physicians, nursing, and therapy service lines | Meets SAT and SBT Criteria |
| D | Delirium Assessment (CAM-ICU) and Management | Objective delirium screening with the Confusion Assessment Method for the ICU (CAM-ICU). 33 Systematic evaluation for causation of delirium with appropriate interventions. | None |
| E | Early Mobility (EM) | Patients meeting criteria receive mobility evaluation and therapy as indicated. | No myocardial ischemia Stable heart rate & cardiac rhythm FiO2 ≤ 0.6 PEEP ≤ 10 cm H2O Minimal vasopressor Response to verbal stimulation |
According to the Office of the National Coordinator (ONC) for Health Information Technology (IT), the main goal of health IT is to improve the quality and safety of patient care.1 Health care quality has been defined as “getting the right care to the right patient at the right time.”2 EHRs can help patients receive optimal care by improving communication among providers, promoting timely access to information at the point of care, standardizing care processes, and providing clinical decision support.3–10 The benefit of EHRs may be magnified for patients with chronic diseases or complicated acute illnesses who require coordination of multiple care processes or care bundles. For instance, in the primary care setting, use of EHRs has been associated with improvements in the delivery of care processes designated as “best practices” for diabetes care and in outcome measures for patients with diabetes.11–13 In the inpatient setting, EHR documentation and electronic checklists in ICUs have been associated with increased compliance with evidence-based catheter care and a decrease in central-line associated bloodstream infections.3,14
Despite the potential benefits of EHR technologies, many certified EHRs are not user friendly and are not directly geared toward improving the quality and efficiency of patient care.15,16 Often EHRs do not contain structured data fields to capture performance of key process measures for specific conditions and do not facilitate real-time performance feedback or easy electronic extraction of data elements to evaluate performance.17 As a result, most quality and safety data must be derived from retrospective and labor-intensive sampling of patient populations via manual chart review and are shared months after the care processes of interest have been performed. Although many EHRs do contain large volumes of patient-level data, poor organization of data fields across multiple windows creates information overload for some clinicians and hinders the usability of these data.18 Unorganized data or lack of real-time data within the EHR make it difficult for providers to recognize gaps in care delivery that may lead to suboptimal care and patient harm.18,19 In fast-paced clinical environments such as ICUs, the provider’s ability to quickly assess multiple patient data points is key to preventing delays in diagnosis and care delivery that can have devastating consequences for critically ill patients.18
Delirium, or acute brain dysfunction, is a common complication of critical care and a significant patient safety problem, occurring in up to two-thirds of ICU patients.20,21 ICU delirium is independently associated with increases in mortality, morbidity, and health care costs.22–26 Delirium may be prevented or mitigated through the timely use of evidence-based care processes such as those included in the ABCDE bundle.21,27–31 Delivery of each ABCDE bundle care process on a daily basis is triggered by patients fulfilling specific safety criteria (e.g., breathing trials are held if a patient is exhibiting hemodynamic instability) and requires the coordination of care among physicians, nurses, and respiratory, physical, and occupational therapists. Despite supporting evidence of their effectiveness, widespread implementation of these practices has been challenging, limiting the potential reduction in iatrogenic harm if they were applied consistently.21,32
Case Description
This case study examines an integrated health care delivery system’s approach for tailoring the EHR to facilitate the implementation of the ABCDE bundle in multiple ICUs across three hospitals and to enable a future evaluation of the impact of bundle adoption on clinician adherence to delirium care processes and on patient outcomes. Although a few studies have been published describing ABCDE bundle implementation,27,28,34 none have focused on the process of modifying the EHR to document and track bundle adherence. We have outlined the steps we took to establish infrastructure within the EHR that support the implementation and evaluation of this quality improvement initiative. First, we describe our process for identifying key data needs for ABCDE bundle implementation and evaluation and for modifying the EHR to optimize delivery of ABCDE processes of care. Next, we examine changes in the documentation of bundle elements over time to assess adherence to the new documentation processes and bundle element data capture. Finally, we discuss lessons learned and the next steps in our implementation and evaluation process.
Setting
Baylor Scott & White Health (BSWH) is the largest not-for-profit health care system in Texas and one of the largest systems in the United States. BSWH comprises Baylor Health Care System (BHCS) and Scott & White Healthcare, who merged in 2013 to create a new model system to meet the demands of health care reform, the changing needs of patients, and the recent advances in clinical care. BSWH includes 43 hospitals with 5,410 licensed beds. In 2012, the BHCS Center for Clinical Effectiveness received funding from the Agency for Healthcare Research and Quality (AHRQ) to test the implementation of the ABCDE bundle in the ICUs of 3 BHCS hospitals, with a primary focus on identifying generalizable best practices in how to deploy the bundle expeditiously. The intervention hospitals included a large, urban tertiary care facility; a midsize community hospital; and a small rural hospital. Although, the study team selected these 3 hospitals to participate in ABCDE bundle implementation, the EHR modifications were rolled out to all BHCS hospitals, as the inpatient EHR (AllScripts) is standard across facilities. This project was designated as a quality improvement initiative. We received approval from the Baylor Research Institute Institutional Review Board (IRB) for the use of patient data, including process and outcomes measures collected as part of routine care, and were granted a waiver of informed consent.
Patient Population
Patients admitted to the ICUs of intervention hospitals were eligible to receive the ABCDE bundle if they were 18 years of age or older, had an ICU admission lasting more than 24 hours, and were on the ventilator for more than 24 hours and less than 14 days. Patients were excluded if they were on comfort care; pending a transfer order to a non-ICU bed; were never on the ventilator; had a primary diagnosis of brain tumor, mental disorder, stroke, or intracranial injury; or were poisoned by drugs, medicinal, or biologic substances based on ICD-9 classification.
Identification of Required Data Elements and EHR Modifications
To facilitate uptake of ABCDE practices and measure their adoption, we needed to capture EHR data that would allow us to measure and report performance of ABCDE care processes and related outcome measures. Key ABCDE process measures are fully described in Table 1. The number of ABCDE care processes that a patient was eligible for depended on how long the patient was ventilated and the patient’s ICU length of stay (LOS). Patients were potentially eligible (provided they met specific safety criteria—see Table 1) to receive all five bundle elements every day they remained in the ICU and were on the ventilator. When patients were weaned off the ventilator they were eligible to receive relevant bundle elements (generally delirium assessment and management, and early exercise) every day they remained in the ICU and were not on a ventilator. Related outcome measures include incidence of delirium, days on the ventilator, ICU- and hospital LOS, inpatient mortality, and discharge status.
Formation of Clinical Design Team
In August 2012, we formed an interdisciplinary team of nurses, physicians, and physical, occupational, and respiratory therapists from the three BHCS implementation hospitals, as well as IT personnel from the system EHR clinical documentation group, to determine what EHR modifications and decision support tools were necessary to streamline the delivery and capture of ABCDE bundle processes. This team had a series of meetings over a four-month period, which resulted in a set of EHR change requests including modifications to documentation templates, creation of new viewing fields, and revision of order sets that were submitted to the System IT Governance Committee. The Clinical Design Team continued to meet monthly throughout the duration of the project to provide ongoing input pertaining to optimization of the ABCDE tools within the EHR.
Prioritization of EHR Modification by System Leadership and Assignment of IT Resources
As basic EHR installation was still in progress at some BHCS facilities during the project period, system IT bandwidth for customized projects like the ABCDE bundle deployment was limited. In this context, a subgroup of the System IT Governance Committee (“Workgroup 1”) had responsibility for prioritizing EHR projects in the IT production queue. In November 2012, the change requests associated with ABCDE bundle implementation were reviewed by Workgroup 1 and assigned a high priority, based on the following rationales: (1) this program addressed a pressing patient safety and quality issue; (2) building the documentation and EHR reporting capabilities for the ABCDE bundle would replace unreliable (and inefficient) paper-based processes; and (3) this was a shared interest that overlapped with other change requests from the system Critical Care Council. With this prioritization (effectively a green light for developing the change requests for the EHR production environment), designated IT resources from the Clinical Documentation Group, Nursing and Physician Informatics, and other programming personnel were assigned to work with the project team.
Development and Implementation of EHR Modifications
Between November 2012 and June 2013, the change requests moved through the development cycle. This was an iterative, collaborative process between the project team and IT personnel. For example, IT would create a draft of an EHR documentation template, clinical personnel would provide feedback, and the template would subsequently be revised. Following rigorous quality testing of the final content, these changes were implemented in the EHR production environment for use by frontline staff in July 2013. As EHR fields are standardized across BHCS (isolating documentation changes to selected hospitals is not feasible), these changes were rolled out to all BHCS hospitals. The IT team sent an electronic notification to all hospitals immediately prior to implementation of the changes, highlighting all EHR modifications per their standardized protocol.
Additional Training for Intervention Hospitals
The intervention hospitals received ABCDE bundle training and implementation tools, including posters and pocket cards detailing bundle components prior to the EHR modifications, and had designated bundle champions. This initial training included education on the bundle elements and their benefits and strategies for incorporating the bundle into routine clinical care. Following the implementation of the EHR modifications, the intervention hospitals received supplemental in-person training on proper documentation of the bundle processes within the EHR. This training was included as part of a four-hour training for frontline staff on the ABCDE bundle. Clinical champions provided workshop attendees with an overview of the new bundle documentation fields within the EHR and demonstrated how to properly document ABCDE processes of care. A refresher training on EHR documentation was conducted approximately four months later.
Evaluation of Proper Documentation of Bundle Elements
We examined the percentage of ABCDE bundle elements captured over time in the ICUs of the intervention hospitals in order to track compliance with data entry procedures and to improve documentation of care processes. Data were abstracted from the EHR data mart and summarized using SAS version 9.3 (SAS Institute, Inc., Cary, North Carolina).
Existing Data Infrastructure
Prior to the ABCDE bundle deployment project, the EHR contained a critical care flowsheet for documentation of ICU care processes. However, the only ABCDE data element that was captured within that flowsheet was performance of the CAMICU. After a review of other EHR forms and data fields, we found that some data related to the performance of the bundle elements were captured elsewhere in the EHR. Unfortunately, these data were recorded in disparate sections of the EHR, making it difficult for clinicians to quickly assess if the processes of care had been performed for particular patients. In addition, some of the bundle elements were not captured by structured data fields, and it was difficult or impossible to perform an automated abstraction of these data to assess performance of bundle elements. Thus, members of the study team had to conduct manual chart audits to retrieve baseline data related to the performance of some of these measures.
A structured documentation field did not exist to record the performance of Spontaneous Awakening Trials (SATs) or Spontaneous Breathing Trials (SBTs) or reasons why a patient may not have received these processes. Auditors had to examine the respiratory ventilator records or the 24-hour ventilator flowsheet to determine if there was evidence that sedatives had been titrated down or if the ventilator had been turned down to provide minimal pressure support. The physical and occupational therapy (PT/OT) structured note within the EHR already included fields for physical and occupational therapists to document performance of early mobility assessments and the level of mobility achieved. However, early mobility exercises are often performed by nurses before patients meet the criteria for a physical therapy consult, and there were no structured fields for nurses to document early mobility. Outcome measures such as incidence of delirium, days on the ventilator, and ICU- and hospital LOS were already captured within the EHR. Inpatient mortality and discharge status were documented in the BHCS administrative database and could be extracted from the enterprise data warehouse (EDW).
EHR Modifications
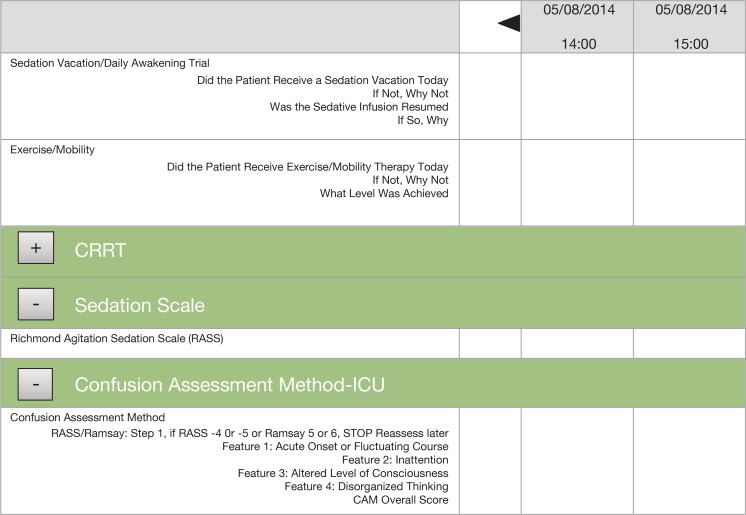
The project team agreed that structured data fields for the documentation of ABCDE bundle eligibility and delivery of bundle processes should be added to the EHR. These data fields were added to the existing nursing critical-care flowsheet or the respiratory therapist structured note, depending on who was responsible for providing the care process. “Sedation Vacation/Daily Awakening Trial” and “Exercise/ Mobility” sections were added to the nursing critical-care flowsheet under the ventilator bundle section. The fields in the “Sedation Vacation/Daily Awakening Trial” section prompted nurses to document if the patient had received a SAT that day or why the patient had failed to receive a SAT, if the sedative infusion was resumed, and why the sedation was resumed. The “Exercise/Mobility” section prompted nurses to document if the patient received an early mobility assessment that day, or why the patient did not receive an early mobility assessment, and what level of mobility the patient achieved (Figure 1).
Figure 1.
Adding Spontaneous Awakening Trial (SAT) to the Nursing Critical Care Flowsheet
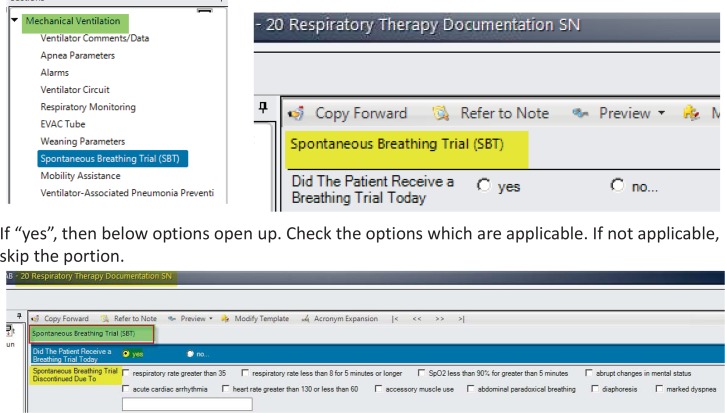
A line was added to the respiratory therapist structured note for “Spontaneous Breathing Trial” with a pull down box indicating whether or not a SBT was performed, and if not, why not (Figure 2).
Figure 2.
Documenting Spontaneous Breathing Trial (SBT) in Respiratory Therapy Structured Notes
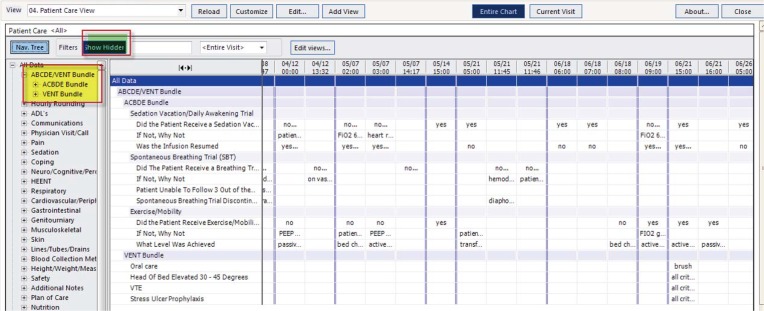
The PT/OT structured note already included fields for documentation of early mobility. In addition the design team created an “ABCDE” tab in the existing Patient Care Viewer that provided a summary of SAT, SBT, delirium (CAM-ICU), and early mobility assessments, to promote quick viewing of the bundle elements received by individual patients and enhance interdisciplinary communication (Figure 3).
Figure 3.
Creation of the Patient Viewer for the ABCDE Bundle
Tracking and Reporting of Bundle Elements
The design team planned to create a business intelligence (BI) dashboarding tool to allow ICU managers to pull bundle compliance data in real time, monitor key performance indicators, and provide feedback to frontline staff. However, the creation of this tool was not feasible at the time due to resource constraints. As a temporary solution, we created monthly ICU reports (Figure 4) with graphs displaying the percent of missing data elements; performance of SATs, SBTs, delirium assessment (CAM-ICU), and early mobility over time; and reasons why patients did not receive these assessments. A BSWH data analyst generated these reports by extracting data from the EHR data mart using SAS, and the reports were emailed to the nurse managers in each ICU.
Figure 4.
Example of Monthly Bundle Performance Report for a Study ICU
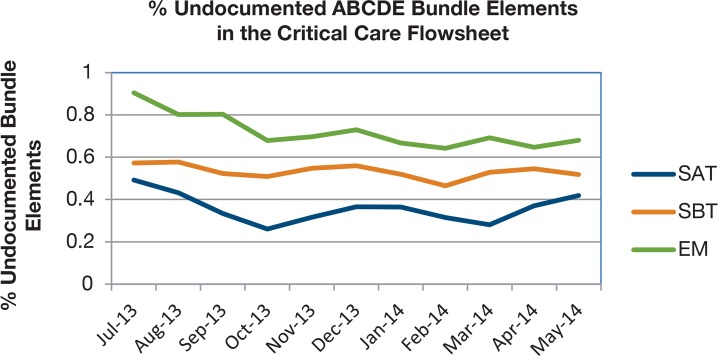
ABCDE Bundle Element Documentation Following EHR Modifications
We tracked the percent of ABCDE bundle elements captured in the critical care flowsheet and structured notes for the 11 months following the EHR modifications to assess adherence to the new documentation processes and bundle element data capture (Figure 5). From July 2013 to May 2014, the percent of undocumented SATs (n= 3018) decreased from 49 percent to 41 percent. The percent of undocumented SBTs (n= 2775) decreased from 57 percent to 52 percent, and the percent of undocumented early mobility assessments (n = 4315) decreased from 91 percent to 68 percent.
Figure 5.
Percentage of Undocumented ABCDE Bundle Elements in the Critical Care Flowsheet
Major Themes
The Clinical Design Team indicated that the EHR was not structured in a manner that facilitated interdisciplinary care coordination among the range of providers in the ICU including nurses, physicians, and respiratory, physical, and occupational therapists. In addition, the EHR did not allow for adequate documentation of patient eligibility for certain processes of care in the ICU, such as those contained in the ABCDE bundle, or delivery of these care processes. These shortcomings prevented the delivery of efficient care and our ability to assess the potential benefits of this quality improvement initiative. Our particular EHR allowed flexibility to customize documentation fields in support of ABCDE bundle deployment. We capitalized on that flexibility by assembling a collaborative team of IT personnel and clinical experts to identify the bundle data elements to be added to the EHR, to streamline EHR documentation in support of staff workflow, and to make these data easily accessible to providers. Structured data fields to capture performance of bundle elements were added to the existing nursing critical-care flowsheet and the respiratory therapist structured notes. A tab in the EHR Patient Viewer was created to allow clinicians to view in one place the performance of bundle elements for individual patients.
Documentation of bundle elements improved over time; however, the percentage of missing data elements is still relatively high. We believe that current efforts to report missing data and ABCDE bundle compliance rates to nurse managers on a monthly basis and the eventual establishment of real-time feedback on these measures for use in daily rounds will drive improved documentation and bundle adherence.
Lessons Learned
Tailoring the EHR to accelerate adoption of the ABCDE bundle was a challenging, time-consuming, and resource-intensive process, but we learned many valuable lessons that can facilitate the implementation of future quality improvement projects involving EHR modifications. Gaining buy-in from senior leadership at the beginning of the project is crucial to ensuring that EHR modifications can be prioritized and resourced accordingly. Our health IT partners had a number of other competing EHR optimization projects during the study period, and even with designation as a high-priority project, the development and testing cycle for the ABCDE bundle EHR change requests required nearly seven months before all components were ready for frontline use. Health systems need to set timeline expectations accordingly for similar projects requiring EHR modifications.
As we worked through the redesign process, we found that it was critical to understand the varying workflows of the multidisciplinary care teams and to involve them in the EHR front end redesign. We wanted to improve the documentation and uptake of ABCDE bundle elements by clinical staff, which necessitated obtaining buy-in from the staff and streamlining the documentation process to fit their current workflow. One crucial aspect of this was architecting the documentation fields in a structured format so that it created a net efficiency for providers by eliminating double documentation, meaningfully synthesizing disparate data, and allowing paper-based tools to be retired.
We also observed that improving EHR interfaces will not improve capture of bundle performance if clinical staff are not trained on how to properly document specific care processes in the EHR. Frequent retraining and communication on the importance of this documentation (and how to record data in a way that facilitates extraction) are also important. We found that documentation of care processes improved for the period immediately following the implementation and initial training. However, the amount of missing data for SAT, SBT, and early mobility assessments started to increase four months into the project. After we conducted another round of training, the percent of missing data decreased—until approximately four months later when it began to increase. Staff turnover, changes in nursing management, and task saturation among staff may have contributed to observed increases.
Ongoing performance feedback has been associated with improvements in adoption of quality improvement initiatives.35 Our inability to provide staff with real-time data about documentation practices and performances as planned may have also prevented sustained reductions in the percentage of missing data. In an era of increasing reliance on reports and quality metrics directly derived from EHRs, clinical staff should be continually reminded that their failure to document care processes is interpreted as failure to perform these processes, and that poor documentation affects the system’s ability to determine what practices translate to improved patient outcomes.
Next Steps
Our next step is to create a BI dashboarding tool that allows ICU managers to pull bundle compliance data in real time, monitor key performance indicators, and provide feedback to frontline staff. We will then abstract patient outcomes data from the EHR to determine bundle adherence rates and the effect of bundle implementation on patient outcomes including incidence and duration of delirium, ventilator days, coma days, LOS, nursing home utilization, and mortality.
Conclusions
The creation of learning health systems is contingent on the ability to modify EHRs to meet emerging health care delivery and quality improvement needs. Stage three of the Centers for Medicare and Medicaid Services (CMS)’s Meaningful Use of Certified EHRs criteria will focus on the use of EHRs to improve quality, safety, and efficiency as well as health outcomes. However, many out-of-the-box EHRs are poorly designed for the delivery of clinical care and often do not include good documentation templates and decision-support tools for specific conditions.36,37 Continual modification and optimization of these systems is needed to meet the needs of providers and, more importantly, of the patients.36 In order to provide high quality care across conditions, health care systems will need to expeditiously make modifications to EHRs. New interfaces and structured data fields will need to be created to track performance of specific care processes and to collect data for evaluation of quality improvement initiatives.
Health care systems are currently challenged to find efficient ways to modify the EHR. Use of standardized disease or condition-specific forms embedded within the EHR and use of real-time reporting tools may help providers quickly identify gaps in care and address these problems before they result in patient harm. This case study provides an example of how health delivery organizations can make meaningful improvements to EHRs and move toward becoming a learning health system. Although this program focuses on the prevention and mitigation of delirium in ICUs, our EHR change process, governance methods for modifying the EHR, and lessons learned from our experience with ABCDE bundle deployment are broadly generalizable to other health care settings and conditions.
Acknowledgments
This submission is based on work presented at the 2014 EDM Forum Symposium. This project was supported by a grant (R18HS021459) from the Agency for Healthcare Research and Quality (AHRQ). The findings and conclusions in this document are those of the authors, who are responsible for its content, and do not necessarily represent the views of AHRQ.
References
- 1.Health IT and Health Care Quality. 2014. (Accessed July 28, 2014. at http://www.healthit.gov/patients-families/health-it-and-health-care-quality.)
- 2.Clancy Carolyn M., MD . Committee on Finance, Subcommittee on Health Care. Washington D.C.: 2009. What is Health Care Quality and Who Decides? [Google Scholar]
- 3.Pageler NM, Longhurst CA, Wood M, et al. Use of electronic medical record-enhanced checklist and electronic dashboard to decrease CLABSIs. Pediatrics. 2014;133:e738–46. doi: 10.1542/peds.2013-2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144:742–52. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 5.Jones SS, Rudin RS, Perry T, Shekelle PG. Health information technology: an updated systematic review with a focus on meaningful use. Ann Intern Med. 2014;160:48–54. doi: 10.7326/M13-1531. [DOI] [PubMed] [Google Scholar]
- 6.Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005;330:765. doi: 10.1136/bmj.38398.500764.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kern LM, Barron Y, Dhopeshwarkar RV, Edwards A, Kaushal R. Electronic health records and ambulatory quality of care. J Gen Intern Med. 2013;28:496–503. doi: 10.1007/s11606-012-2237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nuckols TK, Smith-Spangler C, Morton SC, et al. The effectiveness of computerized order entry at reducing preventable adverse drug events and medication errors in hospital settings: a systematic review and meta-analysis. Syst Rev. 2014;3:56. doi: 10.1186/2046-4053-3-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poon EG, Wright A, Simon SR, et al. Relationship between use of electronic health record features and health care quality: results of a statewide survey. Med Care. 2010;48:203–9. doi: 10.1097/MLR.0b013e3181c16203. [DOI] [PubMed] [Google Scholar]
- 10.Roumia M, Steinhubl S. Improving cardiovascular outcomes using electronic health records. Curr Cardiol Rep. 2014;16:451. doi: 10.1007/s11886-013-0451-6. [DOI] [PubMed] [Google Scholar]
- 11.Cebul RD, Love TE, Jain AK, Hebert CJ. Electronic health records and quality of diabetes care. N Engl J Med. 2011;365:825–33. doi: 10.1056/NEJMsa1102519. [DOI] [PubMed] [Google Scholar]
- 12.Herrin J, da Graca B, Nicewander D, et al. The effectiveness of implementing an electronic health record on diabetes care and outcomes. Health Serv Res. 2012;47:1522–40. doi: 10.1111/j.1475-6773.2011.01370.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weber V, Bloom F, Pierdon S, Wood C. Employing the electronic health record to improve diabetes care: a multifaceted intervention in an integrated delivery system. J Gen Intern Med. 2008;23:379–82. doi: 10.1007/s11606-007-0439-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allen GB, Miller V, Nicholas C, et al. A multitiered strategy of simulation training, kit consolidation, and electronic documentation is associated with a reduction in central line-associated bloodstream infections. Am J Infect Control. 2014;42:643–8. doi: 10.1016/j.ajic.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 15.Blumenthal D. Stimulating the Adoption of Health Information Technology. New England Journal of Medicine. 2009;360:1477–9. doi: 10.1056/NEJMp0901592. [DOI] [PubMed] [Google Scholar]
- 16.Fihn SD, Francis J, Clancy C, et al. Insights From Advanced Analytics At The Veterans Health Administration. Health Affairs. 2014;33:1203–11. doi: 10.1377/hlthaff.2014.0054. [DOI] [PubMed] [Google Scholar]
- 17.Capurro D, Yetisgen M, van Eaton E, Black R, Tarczy-Hornoch P. Availability of Structured and Unstructured Clinical Data for Comparative Effectiveness Research and Quality Improvement: A Multi-Site Assessment. eGEMs (Generating Evidence & Methods to improve patient outcomes) 2014:2. doi: 10.13063/2327-9214.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pickering BW, Herasevich V, Ahmed A, Gajic O. Novel Representation of Clinical Information in the ICU: Developing User Interfaces which Reduce Information Overload. Appl Clin Inform. 2010;1:116–31. doi: 10.4338/ACI-2009-12-CR-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahmed A, Chandra S, Herasevich V, Gajic O, Pickering BW. The effect of two different electronic health record user interfaces on intensive care provider task load, errors of cognition, and performance. Crit Care Med. 2011;39:1626–34. doi: 10.1097/CCM.0b013e31821858a0. [DOI] [PubMed] [Google Scholar]
- 20.Flinn DR, Diehl KM, Seyfried LS, Malani PN. Prevention, diagnosis, and management of postoperative delirium in older adults. J Am Coll Surg. 2009;209:261–8. doi: 10.1016/j.jamcollsurg.2009.03.008. quiz 94. [DOI] [PubMed] [Google Scholar]
- 21.Vasilevskis EE, Ely EW, Speroff T, Pun BT, Boehm L, Dittus RS. Reducing iatrogenic risks: ICU-acquired delirium and weakness--crossing the quality chasm. Chest. 2010;138:1224–33. doi: 10.1378/chest.10-0466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lundstrom M, Edlund A, Karlsson S, Brannstrom B, Bucht G, Gustafson Y. A multifactorial intervention program reduces the duration of delirium, length of hospitalization, and mortality in delirious patients. J Am Geriatr Soc. 2005;53:622–8. doi: 10.1111/j.1532-5415.2005.53210.x. [DOI] [PubMed] [Google Scholar]
- 23.Inouye SK, Schlesinger MJ, Lydon TJ. Delirium: a symptom of how hospital care is failing older persons and a window to improve quality of hospital care. Am J Med. 1999;106:565–73. doi: 10.1016/s0002-9343(99)00070-4. [DOI] [PubMed] [Google Scholar]
- 24.Vidan MT, Sanchez E, Alonso M, Montero B, Ortiz J, Serra JA. An intervention integrated into daily clinical practice reduces the incidence of delirium during hospitalization in elderly patients. J Am Geriatr Soc. 2009;57:2029–36. doi: 10.1111/j.1532-5415.2009.02485.x. [DOI] [PubMed] [Google Scholar]
- 25.Pisani MA, Murphy TE, Van Ness PH, Araujo KL, Inouye SK. Characteristics associated with delirium in older patients in a medical intensive care unit. Arch Intern Med. 2007;167:1629–34. doi: 10.1001/archinte.167.15.1629. [DOI] [PubMed] [Google Scholar]
- 26.Inouye SK. Delirium in older persons. N Engl J Med. 2006;354:1157–65. doi: 10.1056/NEJMra052321. [DOI] [PubMed] [Google Scholar]
- 27.Balas MC, Burke WJ, Gannon D, et al. Implementing the awakening and breathing coordination, delirium monitoring/ management, and early exercise/mobility bundle into everyday care: opportunities, challenges, and lessons learned for implementing the ICU Pain, Agitation, and Delirium Guidelines. Crit Care Med. 2013;41:S116–27. doi: 10.1097/CCM.0b013e3182a17064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Balas MC, Vasilevskis EE, Burke WJ, et al. Critical care nurses’ role in implementing the “ABCDE bundle” into practice. Crit Care Nurse. 2012;32:35–8. 40–7. doi: 10.4037/ccn2012229. quiz 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Girard TD, Pandharipande PP, Ely EW. Delirium in the intensive care unit. Crit Care. 2008;12(Suppl 3):S3. doi: 10.1186/cc6149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hipp DM, Ely EW, Dittus RS. Delirium and Long-Term Cognitive Impairment in Intensive Care Unit Survivors—Has Your Team Practiced Its ABCDEs Today? Federal Practitioner. 2013;30:14–8. [Google Scholar]
- 31.Vasilevskis EE, Pandharipande PP, Girard TD, Ely EW. A screening, prevention, and restoration model for saving the injured brain in intensive care unit survivors. Crit Care Med. 2010;38:S683–91. doi: 10.1097/CCM.0b013e3181f245d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Young J, Leentjens AF, George J, Olofsson B, Gustafson Y. Systematic approaches to the prevention and management of patients with delirium. J Psychosom Res. 2008;65:267–72. doi: 10.1016/j.jpsychores.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 33.Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAMICU) JAMA. 2001;286:2703–10. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 34.Carrothers KM, Barr J, Spurlock B, Ridgely MS, Damberg CL, Ely EW. Contextual issues influencing implementation and outcomes associated with an integrated approach to managing pain, agitation, and delirium in adult ICUs. Crit Care Med. 2013;41:S128–35. doi: 10.1097/CCM.0b013e3182a2c2b1. [DOI] [PubMed] [Google Scholar]
- 35.Hughes RG, editor. Patient safety and quality: An evidence-based handbook for nurses (Prepared with support from the Robert Wood Johnson Foundation). Rockville, MD: Agency for Healthcare Research and Quality; Mar, 2008. AHRQ Publication No. 08-0043. [PubMed] [Google Scholar]
- 36.Urban Institute Lessons from the Literature on Electronic Health Record Implementation. 2013 [Google Scholar]
- 37.Miller RH, West CE. In: Increasing EHR Use for Quality Improvement in Community Health Centers: The Role of Networks. Fund C, editor. 2011. Issue Brief. [Google Scholar]