Abstract
Purpose:
Given the extensive data stored in healthcare data warehouses, data warehouse governance policies are needed to ensure data integrity and privacy. This review examines the current state of the data warehouse governance literature as it applies to healthcare data warehouses, identifies knowledge gaps, provides recommendations, and suggests approaches for further research.
Methods:
A comprehensive literature search using five data bases, journal article title-search, and citation searches was conducted between 1997 and 2012. Data warehouse governance documents from two healthcare systems in the USA were also reviewed. A modified version of nine components from the Data Governance Institute Framework for data warehouse governance guided the qualitative analysis.
Results:
Fifteen articles were retrieved. Only three were related to healthcare settings, each of which addressed only one of the nine framework components. Of the remaining 12 articles, 10 addressed between one and seven framework components and the remainder addressed none. Each of the two data warehouse governance plans obtained from healthcare systems in the USA addressed a subset of the framework components, and between them they covered all nine.
Conclusions:
While published data warehouse governance policies are rare, the 15 articles and two healthcare organizational documents reviewed in this study may provide guidance to creating such policies. Additional research is needed in this area to ensure that data warehouse governance polices are feasible and effective. The gap between the development of data warehouses in healthcare settings and formal governance policies is substantial, as evidenced by the sparse literature in this domain.
Keywords: Governance, Health Information Technology, SPAN
Introduction
Use of electronic clinical and administrative data has increased significantly across the healthcare enterprise over the last two decades. Some healthcare organizations with electronic health record systems are building data warehouses to meet many needs. Inmon created the accepted definition of a data warehouse as “a subject-oriented, nonvolatile, integrated, and time variant collection of data in support of management’s decisions.”1 For most of the last 3 decades, data warehouse use has been mainly in commercial, non-healthcare settings. Recently some healthcare organizations have built data warehouses that may have uses similar to those in the non-healthcare setting, but may also be quite dissimilar. In healthcare organizations these data warehouses collect data from patient care, population-based databases, financial, claims, and administrative transactional systems, and then organize these data elements to support information retrieval, business intelligence, research, and decision making. Information management is critical to many customers within healthcare delivery systems, especially providers, management, and clinical operations. Such data warehouses have become the central information management platform for decision support in many organizations. Compared to data warehouses in non-healthcare settings, those in healthcare settings may focus more on privacy and security of protected health information, as well as compliance with federal and state regulations and organizational policies.
The United States healthcare delivery system’s IHI Triple Aim Initiative of improving the care experience and population health, while reducing costs, relies heavily on data sharing.2 Successful achievement of the Triple Aim requires electronic databases or data warehouses that have effective and well-articulated governance programs. Good data warehouse governance requires ensuring security, privacy, and regulatory compliance, as well as effective and efficient procedures. To achieve these key trust elements for information sharing and management, a critical need for effective data warehouse governance (DWG) has arisen.
James Walker defined data warehouse governance as “the model the organization will use to ensure optimal use and re-use of the data warehouse and enforcement of corporate policies and ultimately derive value for the money.”3 Wright suggests that data warehouse governance consists of the formal leadership structure, governing bodies and institutional policies related to the development and operation of a data warehouse.4 Data warehouse governance provides standards, policies and procedures to ensure benefit, utility, and value, as well as manage risks. Ideally, a primary focus of data warehouse governance should be strategic decision making and oversight, while secondary goals may focus on resource allocation, investment value and risk mitigation. However, in healthcare settings, DWG may be more concerned about privacy and security, compliance, and risk mitigation due to the sensitivity of protected health information. However, data warehouse governance may vary widely depending on the type, size, and complexity of the organization.
This study was undertaken to summarize current knowledge and assist in understanding the governance issues faced by healthcare organizations that implement data warehouses. We had several questions about DWG programs in healthcare settings to be addressed by this literature search: 1) How robust is the literature about DWG programs in healthcare settings? 2) Are there any published conceptual frameworks for DWG programs in health-care settings? 3) Can these conceptual frameworks be used to analyze existing DWG programs as well as perform gap analysis? And 4) are there any models of DWG programs in healthcare settings that can be used as a model for new or existing DWG programs? We did not study data or information governance, information technology/information services governance, or knowledge management governance, but focused exclusively on data warehouse governance.
Purpose of the Review
This work is part of a larger project called Scalable PArtnering Network for Comparative Effectiveness Research (SPAN), which was funded by the Agency for Healthcare Research and Quality to conduct comparative effectiveness research through a distributed research network of 11 healthcare delivery systems’ virtual data warehouses. In the process of developing a data warehouse governance model for SPAN, we recognized the gap in well-articulated governance strategies for a data warehouse within a healthcare setting. We were particularly interested in studying data warehouse governance programs in healthcare organizations published in the scientific, public domain literature.
Approach
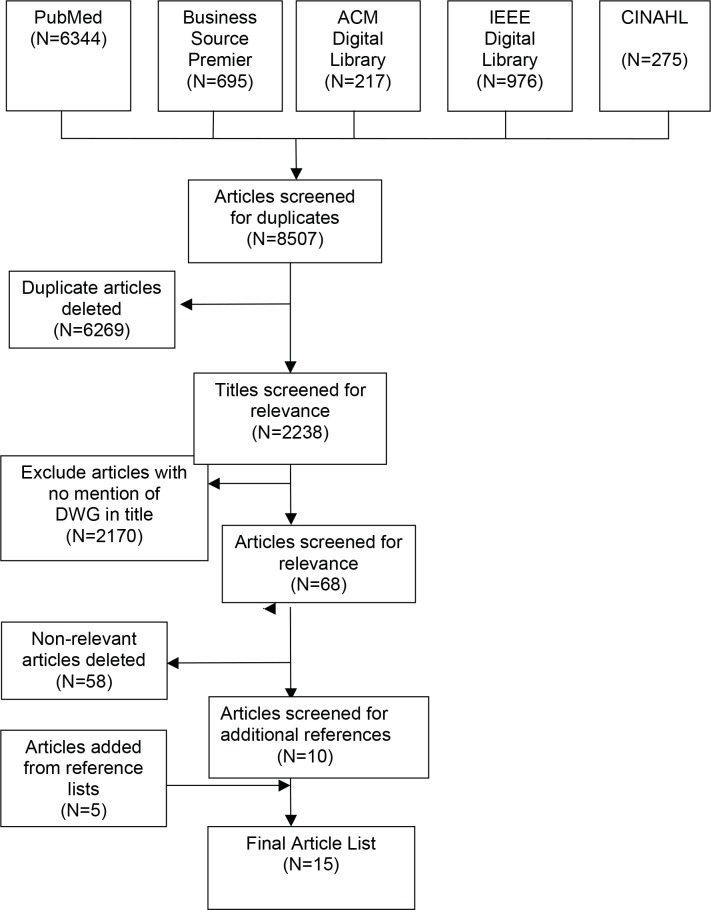
We conducted a literature search to determine what has previously been published about DWG programs in healthcare settings. Because healthcare data warehouses are a relatively recent technological development, we searched via PubMed, Business Source Premier, ACM Digital Library, CINAHL, and IEEE Computer Society Digital Library for English-language literature published since 1997 using these terms: data warehouse governance, data warehouse, healthcare data warehouse, medical data warehouse, clinical data warehouse, information technology governance, and information service governance. We also searched journals published over the last 15 years for relevant titles in their table of contents, including Journal of American Medical Informatics Association, International Journal of Medical Informatics, Decision Support Systems, Journal of Data Warehousing, Data Management Review, Health Informatics Journal, and Information Management. Also we reviewed the citations in found articles to find additional relevant publications. Our literature search excluded books, conference proceedings, letters, and abstracts. We focused entirely on data warehouse governance and excluded articles about data or information governance, information technology/information services governance, and knowledge management governance. Figure 1 depicts the flow of the article search.
Figure 1.
Flow of Article Search
Conceptual Framework of Data Warehouse Governance
We based our study on a conceptual framework derived from several sources that primarily included the DGI Data Governance Framework from The Data Governance Institute.5 We found several other data governance conceptual frameworks, such as Anne Marie Smith’s Data Governance as Part of a Data Warehouse Initiative, Jill Dyche’s Data Governance Next Practices: The 5+2 Model, and Winston Chen’s Simple Data Governance Framework.6–8 These conceptual frameworks were in the grey literature, blogs, or websites, but were not peer-reviewed or easily accessible by scientific search methods. The International Organization for Standardization (ISO) published a technical report on implementing a clinical data warehouse, but did not include a conceptual framework for a DWG program.9 These frameworks focused on data governance and not DWG. None of these offered the elements of a DWG conceptual framework to analyze the literature on DWG, due to their focus on business functions, responsibilities, and deliverables for data governance.
We created a conceptual framework to focus specifically on DWG in healthcare settings. This framework has nine components:
Mission, vision, purpose
Strategy, goals, and objectives with metrics for each objective
Guiding principles
DWG organizational structure and position within the greater organization
Policies and processes for governing the data warehouse
Users’ training, support and engagement
Technical operations (data model, definitions, and quality; metadata)
Security, access, privacy, risk and compliance
Communication plan for stakeholders, users and leadership
Our framework was derived mainly from the DGI Data Governance Framework from The Data Governance Institute.5 The following table shows the similarities and differences between the two frameworks:
We are uncertain that our conceptual framework has validity, reliability, or utility, and testing for these attributes was beyond the scope of this work. This proposed conceptual framework simply serves as a starting point to analyze our findings.
Published studies about data warehouse governance (DWG) in healthcare and non-healthcare settings were analyzed using this conceptual framework with these nine components. We used an iterative process to define a component’s domain. Publications that had robust presentations of a component were used to define a component’s potential, full content. Study components that covered the majority of the component’s full domain were assigned the notation “Yes.” Those study components that partially covered the full domain were assigned the notation “Partial.” Lastly, those study components not mentioned in the published study were assigned the notation “Not reported.”
Supporting Literature and Interviews
Literature Search
Our literature search identified 15 studies about DWG in health-care and non-healthcare settings.3,10–23 Of these 15 studies only three were about DWG programs in healthcare settings.10–12 Chute et al described the Enterprise Data Trust at Mayo Clinic, but presented minimal information about one of the nine components of a DWG program (organizational structure).10 Newcomb provided a compelling rationale for a DWG program in healthcare settings, but addressed only one component (strategy, objectives).11 Wylie et al presented privacy models for biomedical databases, but did not mention the other components of a DWG program.12
Although Watson described many of the components of a DWG program, the paper addressed best practices at a health insurance company, not a healthcare delivery organization.13 Of the 12 studies about DWG programs from commercial settings outside healthcare,3,13–23 five did not address any of the DWG program components, but did provide very useful lists of “do’s and don’ts” or “steps to take” to implement a DWG program.19–23 Examples of recommendations to ensure success in a DWG program include establishing a top-down, model-driven architecture for managing data; clearly defining rules and relationships between data elements; using comprehensive metadata management and reference data management controls; implementing rules and policy; and providing for audit records and security.23 Other recommendations are: designing a DWG program with policies and procedures that support sharing and exchange of knowledge; establishing a single version of the “truth” for information; enforcing security, accountability and regulatory compliance; and supporting efficiency and cost-effectiveness.20–22Several studies suggest that threats to the DWG program include: weak executive sponsorship, inadequate funding, organizational politics, poor collaboration of information technology staff with users, and suboptimal user engagement, support and training.19–22 In summary, the literature is very scant about DWG programs in healthcare settings and silent about research uses. Only 3 of the 15 studies were peer-reviewed (Chute et al, 2010, Wylie et al, 2003, Watson et al, 2004).10,12–13
Data Warehouse Governance Components
Table 2 shows how well each study addressed the nine components of our DWG conceptual framework for the 10 studies that included at least one of the nine components.3,10–18
Table 2.
Data Warehouse Governance Components in Included Studies
| Authors, Year | Mission, Vision, Purpose | Strategy, Objective | Guiding Principles | Organizational Structure | Policies, Procedures | Training, Support | Technical Operations | Security, Risk | Communication Plan |
|---|---|---|---|---|---|---|---|---|---|
| Chute et al, 2010 | Partial | ||||||||
| Dyche, 2011 | Yes | Partial | |||||||
| Imhoff, 2011 | Yes | Partial | |||||||
| Leonard, 2007 | Yes | Yes | Yes | Yes | |||||
| McHugh, 2007 | Partial | ||||||||
| Newcomb, 2009 | Yes | ||||||||
| O’Neal, 2011 | Partial | Partial | |||||||
| Walker, 2007 | Partial | Partial | Partial | Partial | Partial | Yes | |||
| Watson et al, 2004 | Partial | Partial | Yes | Yes | Partial | Yes | Partial | ||
| Wylie et al, 2003 | Partial |
Blank space indicates DWG program documents lacked these components
Yes indicates robust description of these components
Partial indicates minimal description of these components
Mission, vision and purpose. Mission statements describe why a DWG program exists and its specific purpose. Vision statements portray a future desired state to be achieved by a DWG program. Only the study by Watson et al, 2003, partially addressed this component.13
Strategy, goals, objectives and metrics. Strategy articulates how the DWG program will get to the desired future state and achieve its vision. Goals are broad, overarching objectives that the DWG program will achieve, such as overseeing the use and usability of data as a research asset. In contrast, specific aims or objectives are more narrowly focused on considerations such as instituting data quality processes in order to formalize data correction and enrichment. Metrics should be formulated for each strategic objective to determine if a specific objective has been achieved. As healthcare organizations change, their DWG program will change, as will its specific objectives over time. Only the study by Newcomb, 2008, addressed this component.11
Guiding principles. Guiding principles are strategic initiatives that articulate desired states or objectives to be achieved. These principles should fit the culture, information needs and technological capabilities of the healthcare organization. Guiding principles are derivatives of the mission, vision and strategy of a DWG program. Studies by Imhoff, 2011, and Leonard, 2007, provided examples of guiding principles for a DWG program.15,16
-
Organizational structure. DWG organizational structure describes the DWG committee, its membership, charter and leadership; other related DWG committees, their duties and responsibilities, authorities, relationships to other groups; positions in the greater organization; and executive sponsorship. Also, the structure shows how the DWG process provides oversight for data owners, data stewards, data custodians, and data users that are the common positions in a data warehouse. Although definitions for these positions vary considerably depending on the source, data owners typically decide who can have access to enterprise data. Data stewards maintain data elements, ensure compliance with data element definitions, resolve data conflict, remove unused data, ensure appropriate data use, document data sources, and are responsible for data content and context. Data custodians, also called database administrators, data modelers, or ETL developers, are responsible for safe custody, transport and storage of data; technical environment; and database structure. Often this component (organizational structure) makes the distinction between data warehouse governance and data warehouse management. Studies by Watson et al, 2003, Dyche’, 2011, and Leonard, 2007, provided abundant information about DWG organizational structure.13,14,16 Studies by Walker, 2007, Chute et al, 2010, and O’Neal, 2011, presented some information about this component.3,10,18
Fernandes et al, 2009, described three data warehouse governance and stewardship model structures as central, decentralized, and hybrid.20 The central model has a dedicated team with corporate-wide structure and responsibilities. These authors suggest that the centralized DWG model may be appropriate for the large integrated healthcare systems with an electronic health record system. In the decentralized model, each organizational function or department handles its own data quality issues and DWG program, which may be best for small organizations with several distinct, autonomous functions. These authors described a hybrid model that enables smaller departments to work with a larger integrated system with cross-source teams to coordinate DWG program functions, which may be useful for a hospital linked to several physician offices.20
Policies and procedures. DWG policies and procedures describe the processes for governing a data warehouse. Within this component, critical processes include: accountability, authority, roles, rules of engagement (how people work together), management of cross-functional conflicts, decision making and rights, stewardship, management of change, resolution of issues, making and enforcing rules, management of cost and complexity and creating value. Studies by Watson, 2004, and Leonard, 2007, had extensive descriptions of this component.13,16 In addition, studies by Walker, 2007, and Dyche’, 2011, had some coverage of this component.3,14
User training and support. Training, support and engagement of data warehouse users may be an important component of DWG, but received little attention in these studies. Both Walker, 2007, and Watson, 2004, briefly mentioned the need to train, educate and support data warehouse users as well as members of the DWG committee.3,13
Technical operations. DWG program technical operations include oversight and governance of the data model, architecture, definitions, dictionaries, and quality. Other domains usually included in this component are metadata, data life cycle, data integration and flow, mitigating data disasters and providing for maintenance, upgrades, auditing and monitoring of the data warehouse. Studies by Walker, 2007, Watson, 2004, and Imhoff, 2011, provided some content on DWG technical operations.3,13,15
Security and risk. DWG security and risk component covered security, access, privacy, risk mitigation, regulatory and contractual compliance, as well as monitoring and enforcement. Studies by Walker, 2007, Wylie et al, 2003, and Watson, 2004, partially described the DWG security and risk component.3,12,13
Communication plan. The communication plan of a DWG program reports its processes, decisions and activities to ensure data warehouse user engagement, organizational leadership and executive support, and value to the data warehouse and its DWG program. Studies by Walker, 2007, and Leonard, 2007, provided models of this component.3,16
Implications for Policy, Practice, and Research
Based on our literature search and analysis, we constructed a nine-component conceptual framework for DWG, derived partially from the DGI Data Governance Framework (The Data Governance Institute), that may be useful for healthcare organizations designing and implementing DWG programs.5 This conceptual framework needs to be empirically tested and refined among a large number of healthcare organizations with DWG programs. In the meantime, this conceptual framework could be used as a gap analysis tool for existing and future DWG programs in healthcare organizations. Testing this conceptual framework for validity, reliability, and utility could be done in the future, after sufficient DWG program models have been published to allow this analysis.
In the United States, ongoing legislation to promote adoption and use of electronic health records and other healthcare system reforms will require healthcare organizations with data warehouses to develop DWG programs that ensure benefit, utility and value, as well as manage risk.2,24,25 In addition, healthcare organizations need DWG programs to effectively support business intelligence, research, and clinical and administrative decision making. Our study has offered a potentially useful, but preliminary, conceptual framework for DWG. However, there is very limited guidance in the published, peer-reviewed literature to help healthcare organizations develop DWG programs.
Main Findings
Our search for peer-reviewed articles published over the last 15 years in scientific journals about data warehouse governance in healthcare organizations revealed very few relevant articles. Most of the literature about data warehouse governance focused on commercial settings outside of healthcare and was published in the grey literature. Furthermore, our study found no published DWG conceptual framework, but found five conceptual frameworks for data governance. Through a literature search, we found 10 published studies about DWG programs, nearly all of which were from non-healthcare, commercial organizations. Our analysis revealed that no organization’s DWG program embraced all nine components of our conceptual framework, but all had at least one component with a range of 1 to 7, and median of 2. However, all nine components were addressed at least partially by the 10 studies in aggregate.
Answers to Our 4 Questions
- How robust is the literature about DWG programs in health-care settings?
- Minimal: only 3 articles were found in peer-reviewed, scientific literature
- Are there any published conceptual frameworks for DWG programs in healthcare settings?
- None existed
- Can these conceptual frameworks be used to analyze existing DWG programs as well as perform gap analysis?
- None existed
- Are there any models of DWG programs in healthcare settings that can be used as a model for new or existing DWG programs?
- None that were sufficient
Limitations and Future Work
Our study has several limitations, which suggests opportunities for future work. First, we found very little published data, which limits the generalizeability of our findings and proposed conceptual framework. While it is possible that some organizations have “implicit” DWG governance plans and processes, the failure to articulate those processes in a formal plan may be a barrier to communication and coordination among the multiple entities that contribute data to, or use data from, the warehouse, and among those charged with maintaining the privacy and security of that data. Second, our methods were limited to finding and analyzing titles and key words of articles. Therefore, articles describing DWG but where our search terms were not in the title or appeared as key words may have been missed. Third, exploration of more DWG programs in healthcare organizations would contribute to better understanding of DWG practices and better inform our proposed conceptual framework. Ideally, this DWG conceptual framework should be studied further through a combination of observational case studies in order to more rigorously verify the conceptual framework and ultimately quantify the value of DWG programs. In the future, it would be valuable to assess the comparative effectiveness of different DWG models across multiple healthcare organizations.
Several questions remain: Which of the nine components are really needed? What are the metrics for measuring success in DWG programs? Which models (centralized, decentralized, hybrid) work best in healthcare settings, with and without research centers? And, what is the cost effectiveness and return on investment for various DWG program models? DWG programs will likely vary widely depending on the type, size and complexity of the healthcare organization. We would hypothesize that there is no universal DWG program model, but the best model for a healthcare organization depends on its organizational context and culture. Lastly, which internal DWG program model is best for healthcare organizations when involved in cross-institutional efforts, such as comparative effectiveness research, is unknown.
The literature and evidence base about DWG programs for health-care settings is sparse. Healthcare organizations planning to implement or improve existing DWG programs need better guidance from the literature based on rigorous evaluations and validated conceptual frameworks. Future studies need to test the validity of this DWG conceptual framework for healthcare organizations and gain understanding of how internal DWG models influence readiness and capabilities when working collaboratively with outside healthcare organizations in multi-site research projects. We invite discussion about current conceptual frameworks for DWG programs in healthcare settings, but which were not specifically created for these applications. An opportunity exists for testing current conceptual frameworks, such as the DGI model, and creating future conceptual frameworks for healthcare settings. The learning healthcare system depends on digital collaboration and infrastructure to support meaningful comparative effectiveness research.26 Other studies are needed to test the effectiveness of various DWG models in reducing waste, duplication, rework, invalid results, and costs, as well as ensuring high- value decision support and research. Finally, DWG programs should be evaluated by the value they provide in conducting clinical and population-level research and clinical and population-based interventions.
We encourage healthcare organizations with data warehouses, especially those with research centers, to publish information about their DWG programs and be willing to share their DWG program documents for future studies. More comparative data would assist in testing and improving our proposed conceptual framework and discovering which of the already identified components of an effective DWG program are truly needed or yet to be defined. We call others to action to improve knowledge about effective DWG programs for healthcare settings.
Table 1.
Data Warehouse Governance and Data Governance Frameworks
| Our DWG Program Framework | DGI Data Governance Framework5 |
|---|---|
| Mission, vision, purpose | Mission and vision |
| Strategy, goals, and objectives with metrics for each objective | Goals, governance metrics & success measures, funding strategies |
| Guiding principles | Data rules & definitions |
| DWG organizational structure & position within the greater organization | Decision rights |
| Policies & processes for governing the data warehouse | Accountabilities |
| Users’ training, support & engagement | Controls |
| Technical operations (data model, definitions & quality, metadata) | Data stakeholders |
| Security, access, privacy, risk & compliance | Data governance office |
| Communication plan for stakeholders, users & leadership | Data stewards |
| Proactive, reactive, & ongoing data governance processes |
Acknowledgments
This work was supported by grant number R01HS019912 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Footnotes
Disciplines
Health Services Research
References
- 1.Inmon WH. Building the Data Warehouse. 4th Edition. John Wiley and Sons; Oct, 2005. [Google Scholar]
- 2.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Affairs. 2008;27(3):759–69. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 3.Walker DM. Data warehouse governance. 2007. Version 1.1.Data management and warehousing. www.datamgmt.com/ (accessed 11 April 2013)
- 4.Wright A, Sittig DF, Ash JS, et al. Governance for clinical decision support: case studies and recommended practices from leading institutions. J Am Med Inform Assoc. 2011;18:187–94. doi: 10.1136/jamia.2009.002030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Data Governance Institute. The DGI data governance framework 2005–2006. www.datagovernance.com/ (accessed 11 April 2013)
- 6.Smith AM. Data governance: as part of a data warehouse initiative. www.eiminstitute.org/library/eimi-archives/volume-3-issue-4-april-2009-edition (accessed 11 April 2013)
- 7.Dyche J. Data governance next practices: The 5+2 Model. http://www.b-eye-network.com/view/14782 (accessed 25 May 2013)
- 8.Chen W. A simple data governance framework. http://blog.kalido.com/a-simple-framework-for-data-governance/ (accessed 25 May 2013)
- 9.OSI. Health Informatics-deployment of a clinical data warehouse. www.iso.org/iso/ts29585:2101(en) (accessed 11 April 2013)
- 10.Chute CG, Beck SA, Fisk TB, et al. The enterprise data trust at Mayo Clinic: a semantically integrated warehouse of biomedical data. J Am Med Inform Assoc. 2010;17:131–35. doi: 10.1136/jamia.2009.002691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Newcomb C. Health care data governance. Information Management. 2009;19(7):26. [Google Scholar]
- 12.Wylie JE, Mineau GP. Biomedical databases: protecting privacy and promoting research. Trends in Biotechnology. 2003;21(3):113–16. doi: 10.1016/S0167-7799(02)00039-2. [DOI] [PubMed] [Google Scholar]
- 13.Watson HJ, Fuller C, Ariyachandra T. Data warehouse governance: best practices at Blue Cross and Blue Shield of North Carolina. Decision Support Systems. 2004;38:435–50. [Google Scholar]
- 14.Dyche’ J. Governance from the ground up: launching your data governance initiative. Baseline Consulting Group 2011. www.virtualtechtour.com (accessed 11 April 2013)
- 15.Imhoff C. Maximizing the data warehouse through information integration and governance. Intelligent Solutions 2011. www.tdwi.org (accessed 11 April 2013)
- 16.Leonard B. Governance: a business intelligence best practice. Baseline Consulting Group 2007. www.baseline-consulting.com/ (accessed 11 April 2013)
- 17.McHugh L. Getting a grip on data governance and data management. Baseline Consulting Group 2007. www.baseline-consulting.com/ (accessed 11 April 2013)
- 18.O’Neal K. The role of business in data governance. Beye NETWORK 2011. www.b-eye-network.com/view/15381 (accessed 11 April 2013)
- 19.Dyche’ J, Nevala K. Governance White Paper. Ten mistakes to avoid when launching your data governance program. Baseline Consulting Group 2009. www.baseline-consulting.com (accessed 11 April 2013)
- 20.Fernandes L, O’Connor M. Governance should lead the healthcare data dance. Beye NETWORK 2009. www.b-eye-network.com/view/10067 (accessed 11 April 2013)
- 21.Newcomb C. Implementing data governance in complex healthcare organizations: challenges and strategies. Baseline Consulting Group 2008. www.baseline-consulting.com/ (accessed 11 April 2013)
- 22.Nunn S. Data governance: make it a priority. For The Record. 2008;20:19. [Google Scholar]
- 23.Kalido White Paper. Data governance for data warehousing: top five critical success factors. Kalido. 2009. www.kalido.com/ (accessed April 11 2013)
- 24.Berwick DM. Launching Accountable Care Organizations – The proposed rule for the Medicare Shared Savings Program. N Engl J Med. 2011;364:32. doi: 10.1056/NEJMp1103602. [DOI] [PubMed] [Google Scholar]
- 25.Blumenthal D. The “Meaningful Use” regulation for electronic health records. N Engl J Med. 2010;363:501–40. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 26.Institute of Medicine (US); Grossman C, Powers B, McGinnis JM, editors. Digital infrastructure for the Learning Health System: The Foundation for Continuous Improvement in Health and Health Care: Workshop Series Summary. Washington (DC): The National Academies Press (US); 2011. pp. 53–67.pp. 167–80.pp. 239–45. [PubMed] [Google Scholar]