Abstract
The current study is a randomized clinical trial evaluating the efficacy of Focused Playtime Intervention (FPI) in a sample of 70 children with Autism Spectrum Disorder. This parent-mediated intervention has previously been shown to significantly increase responsive parental communication (Siller et al. in J Autism Dev Disord 43:540–555, 2013a). The current analyses focus on children’s attachment related outcomes. Results revealed that children who were randomly assigned to FPI showed bigger increases in attachment-related behaviors, compared to children assigned to the control condition. Significant treatment effects of FPI were found for both an observational measure of attachment-related behaviors elicited during a brief separation-reunion episode and a questionnaire measure evaluating parental perceptions of child attachment. The theoretical and clinical implications of these findings are discussed.
Keywords: Autism, Randomized clinical trial, Parent child communication, Attachment, Intervention
Introduction
From early in development, typically developing children form expectations about how caregivers will respond to bids for comfort. These expectations guide how children seek proximity to or contact with their caregiver under conditions of stress (e.g., during and after a short separation from their caregiver). The specific pattern of attachment behavior elicited is often seen as a reflection of the affectional bond that young children form with their caregiver (Ainsworth et al. 1978; Bowlby 1969/1982; Cassidy and Shaver 1999; Rutgers et al. 2004). Despite pervasive deficits in social, affective, and communicative behaviors, the attachment behaviors of children with Autism Spectrum Disorder (ASD) show striking similarities to those of typically developing children. More often than not, children with ASD show distress or searching for their mother during separation and a preference for their mother over a stranger after reunion (Bernabei et al. 1998; Sigman and Mundy 1989). Moreover, Rutgers et al. (2004) conducted a meta-analytic review of studies that evaluated not only on the absence or presence of specific attachment behaviors, but also on the quality of children’s attachment relations. Results from this meta-analytic review showed that about 50 % of children with ASD form secure attachment relationships with their caregivers, suggesting that many children with ASD are capable of forming secure attachment relations. However, Rutgers et al. (2004) also revealed that, when compared to groups of typically developing children, secure attachments are significantly underrepresented (medium effect size) in ASD. High levels of ASD symptoms and the presence of intellectual disability seem to significantly reduce the likelihood that a child with ASD will develop secure attachment relations (Rutgers et al. 2004; Naber et al. 2007b). One interpretation of these findings is that it may take children with ASD more time to form coherent expectations about how caregivers will respond to bids for comfort. That is, difficulties interpreting the emotional cues and intentional states of others may cause delays in their ability to construct a working model of parent and self (Rogers et al. 1991).
According to developmental theory, the organization of children’s attachment relations is the cumulative outcome of early interactive experiences with their caregiver (Ainsworth 1979). Specifically, a mother who is aware of her child’s signals, who accurately interprets these signals, and who responds in a prompt, appropriate and empathetic manner (i.e., a mother who is optimally sensitive) is expected to promote the formation of a secure attachment relationship (Ainsworth et al. 1978). Empirically, this association between maternal sensitivity and attachment security has been shown across a range of non-clinical samples (De Wolff and van Ijzendoorn 1997). Moreover, in a recent cross-sectional study of 45 preschool-age boys with ASD, Koren-Karie et al. (2009) showed that mothers of securely attached children with autism were more sensitive to their children than mothers of children classified as either insecure/organized or insecure/disorganized. Importantly, this association between maternal sensitivity and attachment security remained significant when the severity of children’s autism symptoms and children’s level of cognitive functioning were statistically controlled. Investigating this association between maternal sensitivity and attachment security in atypical populations such as children with autism (Capps et al. 1994; van IJzendoorn et al. 2007) or children with Down syndrome (Atkinson et al. 1999) strengthens the validity of the evaluated constructs and illuminates the processes that underlie the development of attachment relations.
The cross-sectional and longitudinal research reviewed above does not allow us to draw firm conclusions about underlying causal mechanisms. Experimental research designs are necessary to evaluate the causal link between children’s interactive experiences and subsequent gains in attachment behaviors more directly. The current study presents analyses from a randomized clinical trial evaluating the efficacy of Focused Playtime Intervention (FPI), a parent-mediated intervention that has previously been shown to increase responsive parental communication in young children with ASD (Siller et al. 2013a). To investigate the effects of FPI on children’s attachment behaviors, we administered an observational measure where attachment-related behaviors were elicited in the context of a brief separation-reunion episode, as well as a parent-report measure evaluating parental perceptions of child attachment. Attachment-related outcomes were assessed both before and after the 12-week intervention period. Given that FPI has previously been shown to effectively increase responsive parental behaviors, we predict that children who are randomly assigned to FPI will show bigger gains in attachment-related behaviors, compared to children assigned to the control condition.
Methods
This study reports on attachment-related outcomes of children and parents who participated in a randomized controlled experimental intervention study between 2004 and 2007. Brief descriptions of the research design, participant characteristics, intervention procedures, and measures are included, but for details please see Siller et al. (2013a). This randomized clinical trial involved three waves of data collection, scheduled immediately before (i.e., baseline), immediately after (i.e., exit), and 12 months after (i.e., follow up) the 12-week intervention period. Measures of attachment behaviors were collected as part of the baseline and exit assessments, which will be the focus of the current manuscript. Baseline assessments occurred during three individual sessions. Two assessment sessions were held at our research lab and one session was scheduled in the families’ home. Assessments included two measures to confirm children’s ASD diagnoses (Autism Diagnostic Interview-Revised, ADI-R, Lord et al. 1994; Autism Diagnostic Observation Schedule, ADOS, Lord et al. 2000), the Mullen Scales of Early Learning (Mullen 1995), the Early Social Communication Scale (Seibert et al. 1982), and a separation-reunion episode. In addition, children’s mothers were interviewed using a survey of non-project services (Bono et al. 2004) and asked to complete the Maternal Perception of Child Attachment (MPCA) questionnaire (Hoppes and Harris 1990). Once the baseline assessments were completed, families were randomly assigned to either the experimental or control condition. Throughout the study, staff and students involved in administering assessments or coding observations were kept blind to the participants’ group assignment. Across both intervention conditions, parents were invited to participate in a parent education program that aimed to help parents effectively advocate for their young child with ASD (Parent Advocacy Coaching, PAC). Families assigned to the experimental condition were also invited to participate in FPI. After the last intervention session, families completed a series of exit assessments. Since families required different amounts of time to complete the intervention sessions, the time lag between baseline and exit assessments varied substantially between families, but was well matched between the experimental (M = 147 days, SD = 41, range 91–279) and control group (M = 141 days, SD = 43, range 78–255). Assessments administered at exit included some, but not all the measures administered at baseline. Information on subjects’ completion of the allocated intervention, measures and attrition is displayed in Fig. 1 (CONSORT flow diagram).
Fig. 1.
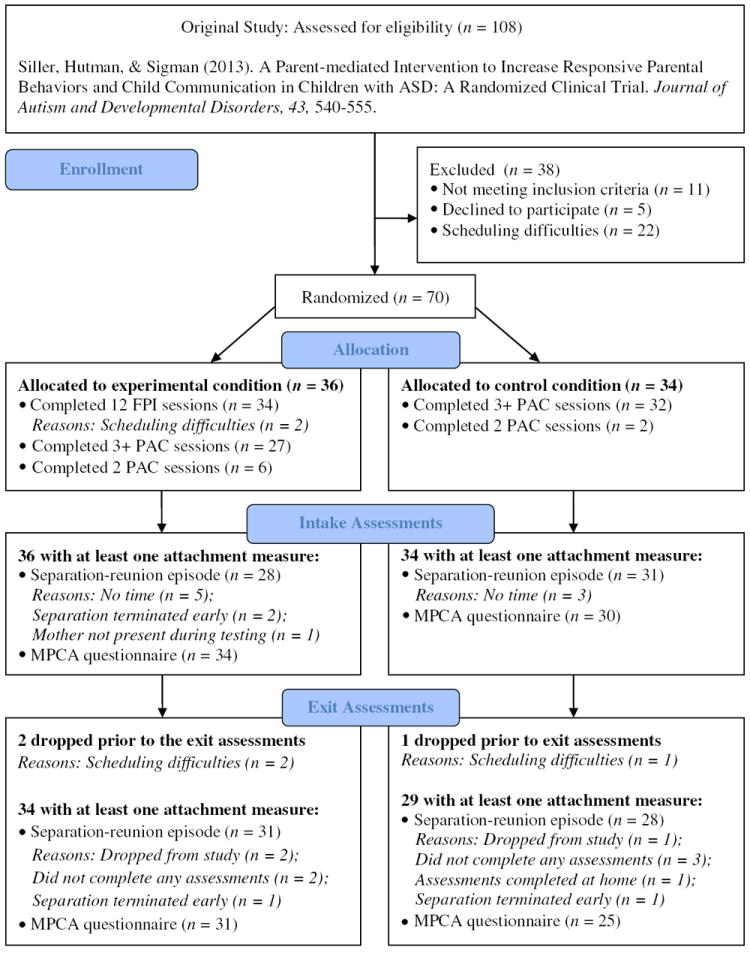
Participant recruitment, enrollment, randomization, and retention
Participants
Seventy children (64 boys and 6 girls) between 2 and 6 years of age participated in this research. Children met the following inclusion criteria: (1) the child was 6 years or younger when entering the study, (2) the child had previously been diagnosed with ASD, (3) the child showed limited or no use of spoken language (generally fewer than 25 words and no phrases based on parent report), (4) the child’s mother was fluent in English and willing/available to participate in all assessment and intervention sessions, and (5) the family lived within a reasonable travel distance from the research lab (generally less than 90 min). Children’s ASD diagnoses were confirmed using the Autism Diagnostic Interview-Revised (ADI-R; Lord et al. 1994) and the Autism Diagnostic Observation Schedule (ADOS; Lord et al. 2000). Sixty-four children (91 %) met diagnostic criteria for Autistic Disorder on both measures. The sample was diverse in terms of children’s ethnic/racial background (44 % were Hispanic/Latino, 20 % were White, 19 % were Asian, 7 % were Black, and 10 % were of mixed ethnic/racial origin), the mothers’ educational attainment (49 % of mothers were college graduates), and the families’ annual income (the median annual household income was $65,000). In addition, 36 mothers (51 %) were born outside the US. Sample characteristics are presented in Table 1.
Table 1.
Descriptive information on child characteristics, family characteristics, and non-project services reported separately for the experimental and control group
| Experimental group | Control group | Effect size | |||
|---|---|---|---|---|---|
|
|
|
|
|||
| M ± SD | n (range) | M ± SD | n (range) | Hedge’s G | |
| Child age (months) | 58.3 ± 12.7 | 36 (33–82) | 55.9 ± 11.9 | 34 (32–76) | .19 |
| Mullen Scales of Early Learning | |||||
| Fine motor age (months) | 28.6 ± 10.4 | 36 (12–55) | 28.3 ± 11.8 | 34 (10–59) | .03 |
| Visual reception age (months) | 26.6 ± 9.4 | 36 (11–50) | 24.6 ± 11.2 | 33 (1–11) | .19 |
| Receptive language age (months) | 17.5 ± 8.0 | 36 (5–36) | 16.5 ± 8.0 | 34 (1–33) | .13 |
| Expressive language age (months) | 16.5 ± 9.8 | 36 (4–36) | 15.1 ± 8.2 | 34 (4–37) | .15 |
| Autism Diagnostic Observation Schedule | |||||
| Social affect total | 14.7 ± 3.3 | 36 (6–20) | 14.8 ± 3.4 | 33 (4–20) | -.03 |
| Restricted and repetitive behavior total | 4.9 ± 2.0 | 36 (0–8) | 5.2 ± 2.2 | 33 (0–8) | -.14 |
| Total | 19.6 ± 4.1 | 36 (9–26) | 20.0 ± 4.2 | 33 (7–26) | -.10 |
| Early Social Communication Scale | |||||
| Response to joint attention | 47.0 ± 24.1 | 36 (8–100) | 39.6 ± 24.1 | 34 (5–88) | .31 |
| Mother characteristics | |||||
| Chronological age (years) | 36.2 ± 5.3 | 36 (26–45) | 35.7 ± 6.1 | 34 (23–48) | .09 |
| Education (years) | 14.9 ± 2.6 | 36 (10–20) | 15.8 ± 2.5 | 34 (12–22) | −.35 |
| Non-project services | |||||
| Autism specific individual services | |||||
| Twelve months prior to intake | 8.8 ± 10.4 | 36 (0–44) | 8.8 ± 10.9 | 32 (0–46) | .00 |
| Between intake and exit | 12.4 ± 11.0 | 34 (0–40) | 12.1 ± 10.2 | 30 (0–44) | .03 |
| School programs | |||||
| Twelve months prior to intake | 11.5 ± 6.6 | 36 (0–29) | 12.6 ± 7.1 | 32 (0–25) | −.16 |
| Between intake and exit | 14.6 ± 8.8 | 34 (0–30) | 14.8 ± 5.5 | 30 (1–28) | −.03 |
Intervention Procedures
Focused Playtime Intervention (FPI)
FPI is a parent education program that involves 12 in-home training sessions (one session per week for 12 weeks, 90 min per session) and follows a standardized intervention manual. The intervention manual and an illustrated workbook for parents are available as an online resource to Siller et al. (2013a).
Structure
FPI was delivered by trained graduate and postdoctoral students in developmental psychology and counseling. All intervention sessions were video-recorded and at least two sessions per child were chosen at random and coded using a fidelity checklist (n = 77). Results revealed a mean fidelity score of 89.6 % (SD = 9.0), demonstrating that overall, the intervention was implemented as described in the intervention manual. Only two of the reviewed sessions revealed fidelity scores below 70 %; interestingly both sessions involved families who eventually failed to complete the experimental intervention. Each intervention session consisted of two parts. The first part (30–60 min) involved both parent and child and provided ample opportunities for parent and interventionist to take turns interacting with the child. In the context of these interactions, the interventionist demonstrated strategies that related to the sessions’ topic, provided specific and concise feedback on the parent’s play (accentuating her positive contributions), and commented on the child’s responses. All interactions between parent, child and interventionist were videotaped and captured live using a laptop computer. The second part of each session (30–60 min) involved only the parent (an intervention assistant was available to supervise the child and possibly his or her siblings). During this time, each intervention topic was elaborated using a range of adult learning strategies, including an illustrated workbook for parents, video feedback, conventional teaching, and the review of weekly homework assignments.
Content
FPI was initially developed as an experimental intervention to test the causal mechanisms that underlie longitudinal associations between early responsive parental behaviors and children’s subsequent gains in spoken communication (Siller and Sigman 2002, 2008). The FPI intervention manual outlines an ordered sequence of eight topics. During the early sessions, parent and interventionist developed a detailed understanding of the child’s communication skills (Topic 1: When and how does my child communicate?), evaluated and reframed the parent’s goals (Topic 2: What do I hope to accomplish during play?), and developed strategies to arrange the play environment in ways that are conducive to play (Topic 3: How do I develop a special play time routine?). One specific product developed as part of Topic 3 was a playtime routine that could feasibly be incorporated into the family’s daily schedule. After these three initial topics, parent and interventionist developed a shared understanding of the goal of this intervention (i.e., parent and child will learn to coordinate their attention and collaborate to accomplish shared goals during toy play), as well as three specific sub-goals: coordinating attention, coordinating actions, and sharing control (Topic 4: How to tackle play one step at a time?). These three sub-goals were addressed in more detail as part of Topics 5–8: parent and interventionist discussed and practiced strategies to support coordinated attention (Topic 5: Who gets to pick the toys?), ensured that parent and child found a shared way of using the toys (Topic 6: Who decides the ‘correct’ way of using the toys? Topic 7: How do I speak to my child during play?), and gradually shifted increasing amounts of responsibility for initiating and maintaining the shared encounter to the child (Topic 8: How do I make play more balanced between me and my child?).
Approach
FPI aims to enhance the capacity of families to meet the needs of their children. Important principles of such a family-centered approach were outlined by Woods and Brown (2011), including the importance of (1) addressing the families’ informational needs (e.g., to accommodate different learning styles, material and practices were presented in multiple formats), (2) using their natural environments as the intervention context (e.g., all intervention sessions were held in the families’ homes and focused on play as a preferred everyday activity), (3) engaging parents to be active participants in the intervention process (e.g., parent and child engaged in weekly practice while the interventionist observed, guided, modeled, and provided feedback in the form of comments, suggestions, reflective questions, and encouragement), and (4) supporting the caregivers’ reflection and self-evaluation (e.g., FPI used video-feedback and play journals to teach parents the observational tools necessary to evaluate the consequences of specific parental choices and strategies).
Parent Advocacy Coaching (PAC)
PAC is a structured education program that aims to promote the parents’ ability to actively participate in the planning of their children’s intervention and educational programs. A more detailed description of this educational program is published elsewhere (Siller et al. 2013b). Most families of children with autism in California have access to two kinds of annual planning meetings; one meeting involves a representative from the families’ local California Regional Center (i.e., Individual Program Plan); the second meeting involves the child’s teacher and/or representative from the child’s school district (i.e., Individualized Education Program). Because of significant overlap in content between the first sessions of FPI and PAC, families randomized to the experimental condition were invited to participate in three PAC sessions; families assigned to the control condition were offered a total of four PAC sessions (one session per month, 90 min per session). In the context of these sessions, parents learned about the structure of the individualized planning process and how to access available resources. They also participated in a structured conversation that aimed to identify developmental needs in the areas of health, daily-living skills, challenging behaviors, social integration, education and family supports. In addition to a detailed report about the results from our developmental assessments, parents were provided with a written summary of the needs identified during this parent interview.
Measures
Assessment of Observed Attachment-Related Child Behaviors
The current study used a brief separation-reunion episode to elicit attachment-related child behaviors. After videotaping a 10-minute episode of parent–child play interaction, a stranger entered the assessment room and mothers were asked to step outside and watch the child through a live video-feed in an adjacent room. Throughout the separation episode, the stranger remained with the child, engaging him or her in play. After about 2 min of separation, mothers re-entered the room, following a specific protocol that involved: (1) calling the child’s name loudly from outside the door, (2) pausing momentarily after opening the door, and (3) greeting the child naturally thereafter. Children’s behaviors during the reunion episode were videotaped and coded for attachment-related behaviors. Coding began after the mother called her child’s name from outside the door, ended 1 min later, and consisted of two observational 7-point rating scales that were adapted from Ainsworth et al. (1978). The Proximity and Contact Seeking Behaviors (PCSB) Scale evaluates the intensity of a child’s effort to regain contact with, or proximity to, their mother. Higher PCSB scores indicate that the child took initiative in achieving contact, where lower scores indicate the child made no effort to make contact with their mother. The Avoidant Behaviors (AB) Scale evaluates the intensity and duration of the child’s avoidance toward their mother. Lowest AB scores indicate that the child did not greet his/her mother upon reunion despite the mother’s attempts at interaction, where higher scores indicate that the child did not display avoidant behaviors toward his/her mother. Please note that both measures were scored so that higher numbers represent stronger signs of attachment. The observational coding was completed by the second author and an undergraduate research assistant. Both coders were kept blind to the experimental condition and assessment time point (intake vs. exit). The coders overlapped on 20 % of the sample and reliability was estimated using single measure intra-class correlation coefficients (ICC). Excellent inter-observer reliability was established for both variables, ICC = .86 for the PCSB Scale and ICC = .89 for the AB Scale. Preliminary analysis using bivariate correlations revealed a strong association between children’s PCSB and AB scores, intake: r(59) = .75, p < .0001 and exit: r(59) = .67, p < .0001. Thus, we created a global measure of observed attachment behaviors, which was computed as the average of children’s PCSB and AB scores.
Assessment of Parent-Reported Attachment-Related Child Behaviors
Children’s mothers were asked to complete the Maternal Perceptions of Child Attachment questionnaire (MPCA; Hoppes and Harris 1990). This parent-report measure consists of 23 items rated on a 5-point rating scale, ranging from frequently (1) to never (5). High scores indicate maternal perceptions of strong child attachment. The items are intended to evaluate the extent to which the mother perceives the child as initiating physical, verbal, play, or eye contact and being capable of reciprocal intimacy (e.g., “My child comes to me when s(he) wants help with something” “When my child is hurt or in pain s(he) comes to me for comfort or help” “My child reacts with jealousy when I pay attention to other people;” “My child seeks my company and attention and actively seeks my attention on a regular basis;” “In general my child seems to show an awareness of my feelings”). Reliability analyses for the 23 items revealed excellent internal consistency at intake (Chronbach’s alpha = .88) and exit (Chronbach’s alpha = .92).
Assessment of Children’s Non-verbal Cognitive and Language Abilities
To evaluate nonverbal cognitive and language abilities, children were administered the Mullen Scales of Early Learning (MSEL, Mullen 1995). The MSEL includes four subscales measuring nonverbal cognitive abilities (Visual Reception and Fine Motor Subscale) as well as children’s receptive and expressive language abilities. All subscales provide age equivalent scores for children’s abilities. Even though the MSEL provides norm-referenced T-scores, most children in this study scored outside the range of differentiated scores. For this reason, all reported analysis were based on children’s age equivalent scores.
Assessment of Children’s Non-verbal Communication Abilities
Children’s responsiveness to others’ bids for joint attention was evaluated during each of the two lab visits, scheduled both before and after the intervention period. During each lab visit we administered four kinds of probes. (1) Response to name was evaluated during the warm up period of each assessment session. The child was provided with a set of toys, which were laid out on the floor (e.g., a colorful play mat, large colored blocks, music toys). Once the child was comfortable, the examiner positioned herself at a 90 degree angle to the child and called the child’s name (3 trials). The remaining prompts were administered in the context of the Early Social Communication Scale (ESCS, Seibert et al. 1982). In this procedure the child and examiner sat facing each other at a small table. A set of toys was in view but out of reach to the child. (2) Response to a head turn: After eliciting eye contact from the child, the examiner called the child’s name while turning his head/gaze towards posters displayed to the left, right, and behind the child (three trials). (3) Response to a head turn with pointing gesture: After eliciting eye contact from the child, the examiner called the child’s name while turning his head/gaze and pointing towards posters displayed to the left, right, and behind the child (three trials). (4) Response to pointing during book reading: While looking at a picture book with the child, the examiner pointed to pictures while calling the child’s name (nine trials). All probes were video-recorded and coded to determine children’s responses during each trial. For each kind of probe (across both assessment sessions), we calculated the percentage of instances where the child correctly responded to the examiner’s bid for attention. The final measure of RJA was the average percentage of successful responses across all four kinds of probes. Inter-observer reliability was evaluated based on more than 70 assessment sessions (above 25 %). Across the four different kinds of probes, intra-class correlation coefficients ranged from ICC = .85 to ICC = .93, demonstrating excellent agreement between two independent observers.
Assessment of Non-project Services
At baseline, parents were interviewed about services their child had received during the preceding 12-month period, using a structured questionnaire developed by Bono et al. (2004). As part of this interview, parents were asked whether children received a range of specialized services for children with ASD (e.g., occupational therapy, speech therapy, applied behavior analysis/ABA, floortime/DIR, social groups) or participated in an educational program (center based early intervention program, preschool, kindergarten, elementary school). If the parents indicated that the child received such services, we also inquired about the time period during which each service was received, the intensity of the service (number of hours per week), whether the service was delivered individually or in a group setting, and whether it was delivered at home or school. The interviews were re-administered after the intervention was completed. Data collected during these interviews were entered into a database, programmed in Microsoft® Access. Using this database, we extracted summary information for two time windows: (1) the 12-month period prior to the beginning of the intervention, and (2) the time period between the beginning and end of the intervention. For each time window, we computed (1) the average number of hours per week during which the child received specialized autism services that were delivered individually; and (2) the average number of hours per week during which the child attended a school program (including non-school services delivered in a group setting).
Data Analysis
Intent-to-Treat Approach
Analyses were performed on the intent-to-treat basis. Prior to performing the key analyses, we used multiple imputation to deal with the missing data. Briefly, multiple imputation uses a regression-based procedure to generate multiple copies of the data set, each of which contains different estimates of the missing values (Enders 2010). We used the data augmentation algorithm in the SAS MI procedure to generate 100 imputed data sets (Graham et al. 2007, recommend at least 20 for most situations). The imputation process included all variables that appeared in one or more of the subsequent regression analyses as well as eight auxiliary variables (see below). The methodological literature currently recommends an inclusive analysis strategy that incorporates auxiliary variables into the missing data handling procedures because this approach can make the missing at random assumption more plausible and can improve statistical power (Collins et al. 2001). To identify auxiliary variables that correlate with missingness, we computed a series of independent-samples t tests for continuous variables (e.g., non-verbal mental age) and Chi square tests for categorical variables (e.g., whether mothers were born inside/outside the US), comparing children with complete (n = 47) and incomplete (n = 23) attachment data. Mean comparisons revealed that dyads with missing attachment data took longer to complete the intervention period, t(63) = −2.1, p < .05, included children with lower nonverbal mental age scores, t(68) = 2.2, p < .05, and parents who were younger, t(68) = 2.6, p < .05, and less educated, t(68) = 2.4, p < .05. To correct for any systematic bias that might be related to these differences, all four variables were used as auxiliary variables in the missing data handling procedures. We also used baseline measures of children’s abilities (i.e., response to joint attention, language age, and ADOS scores) as well as whether children’s mothers were born inside/outside the US as auxiliary variables because of their correlation with incomplete outcome measures. After creating the complete data sets, we estimated the multiple regression models on each filled-in data set and subsequently used SAS MIANALYZE to combine the parameter estimates and standard errors into a single set of results. Note that methodologists currently regard multiple imputation as a “state of the art” missing data technique because it improves the accuracy and the power of the analysis relative to other missing data handling methods (Schafer and Graham 2002).
Primary Hypothesis Testing Approach
The main goal of this analysis was to evaluate the effect of FPI on gains in attachment from baseline to exit. Consistent with recommendations for clinical trials (Fitzmaurice et al. 2004; Carter et al. 2011), gains in attachment were quantified as residual gain scores. One advantage of this approach is that it can provide considerably more power to detect treatment effects than other statistical methods (see NICHD ECCRN and Duncan, 2003 for a comparison of different approaches). Residual gain scores were obtained by regressing the Time 1 measure of each variable onto the later measure of the same variable. The residual errors for each subject were then used as the criterion scores quantifying change. In the context of the current study, residual gain scores answer whether a participant randomized to FPI is expected to change more than a participant in the control condition, given that they have the same initial value. Linear regression analysis revealed that baseline MPCA scores reliably predicted exit MPCA scores, B = .94, SE B = .08, t(49) = 11.7, p < .001, indicating that seventy-two percent of variability in MPCA scores at exit were explained by baseline variation in that variable. For our observational measures, regression analyses revealed significant stability of individual differences for children’s PCSB scores, B = .46, SE B = .12, t(45) = 3.8, p < .001, but not children’s AB scores, B = .21, SE B = .13, t(50) = 1.6, ns. Twenty-three percent of variability in PCSB scores at exit, and five percent of variability in AB scores were accounted for by baseline variation in the respective variables.
Results
Preliminary Analyses
Prior to evaluating the primary hypotheses, potentially confounding variables were examined. To check that the experimental and control groups were not different at baseline, independent-samples t tests for continuous variables (e.g., nonverbal mental age) and Chi square tests for categorical variables (e.g., whether children’s mothers were born inside/outside the US) were performed as appropriate. Measures considered for this analysis included a range of baseline variables potentially associated with outcomes (e.g., maternal age, education and country of birth, as well as children’s chronological ages, Mullen Scores, ADOS scores, Response to Joint Attention scores, the intensity of children’s non-project services). Results from this analysis revealed no significant differences between the experimental and control groups on any of the evaluated measures (p > .15; see Table 1 for effect size estimates). Similar analyses comparing the two groups on a range of socioeconomic characteristics (e.g., family income, ethnicity/race, number of siblings, birth father living with family, home owned/rented) were also not significant and are reported elsewhere (Siller et al. 2013a). Finally, we specified a series of multiple regression models using SAS PROC REG to determine whether baseline measures of parent reported and observed attachment behaviors differed between the experimental and control groups. Results revealed no significant baseline differences on any outcome measure; effect size estimates are reported in Table 2.
Table 2.
Means and standard errors for parent reported and observed attachment behaviors (raw and residual gain scores)
| Time | Experimental group
|
Control group
|
Main effect for treatment group allocation
|
||
|---|---|---|---|---|---|
| Estimate (SE) | Estimate (SE) | B | SE B | Effect Size | |
| MPCA | |||||
| T1 | 3.06 (.12) | 2.93 (.13) | .13 | .17 | .01 (.00, .02) |
| T2 | 3.33 (.13) | 2.89 (.14) | .43* | .19 | .08 (.04, .12) |
| T1–T2 | .15 (.07) | −.16 (.07) | .31** | .10 | .15 (.05, .23) |
| Observed attachment behaviors (mean of PCSB and AB) | |||||
| T1 | 3.47 (.34) | 3.83 (.34) | −.35 | .48 | .01 (.00, .04) |
| T2 | 3.83 (.30) | 3.10 (.31) | .74 | .43 | .05 (.01, .10) |
| T1–T2 | .41 (.27) | −.43 (.28) | .84* | .41 | .07 (.01, .13) |
| PCSB | |||||
| T1 | 2.49 (.30) | 3.14 (.30) | −.64 | .42 | .04 (.01, .08) |
| T2 | 2.55 (.28) | 2.20 (.29) | .35 | .40 | .01 (.00, .04) |
| T1–T2 | .31 (.24) | −.33 (.25) | .64+ | .36 | .06 (.01, .12) |
| AB | |||||
| T1 | 4.46 (.42) | 4.52 (.43) | −.07 | .60 | .00 (.00, .02) |
| T2 | 5.11 (.37) | 4.00 (.39) | 1.13* | .53 | .07 (.01, .13) |
| T1–T2 | .55 (.35) | −.58 (.36) | 1.13* | .52 | .08 (.01, .14) |
Effect size is presented using Cohen’s f2 statistics. By convention, f2 effect sizes of 0.02, 0.15, and 0.35 are termed small, medium, and large, respectively (Cohen 1988).
MPCA = Maternal Perception of Child Attachment questionnaire; PCSB = Proximity/Contact Seeking Behavior Scale rated based on the separation-reunion episode; AB = Avoidant Behavior Scale rated based on the separation-reunion episode. T1 = baseline assessments; T2 = exit assessments; T1 to T2 = residual gain scores obtained by regressing the T1 measure of each variable onto the T2 measure of the same variable; The residual errors for each subject were then used as the criterion scores quantifying change
p < .08,
p < .05,
p < .01
Evaluating Treatment Effects on Observed and Parent Reported Attachment Behaviors
To test the main effect of treatment group allocation on our measures of observed and parent reported attachment behaviors, we specified a series of multiple regression models using SAS PROC REG. All models included a main effect for treatment group assignment. Detailed results from the regression analysis are reported in Table 2 and presented graphically in Fig. 2. Results revealed a significant main effect of treatment group allocation on gains in parent reported attachment behaviors (MPCA scores), t(48) = 3.0, p < .01. To evaluate whether this significant treatment effect can be attributed to treatment-related improvements in the experimental group or worsening in the control group, we computed simple difference scores (Time 2 – Time 1) and used SAS GENMOD to evaluate whether these difference scores differed significantly from zero. Results for the experimental group revealed that parental perceptions of child attachment increased significantly from 3.06 (.12) at Time 1 to 3.33 (.13) at Time 2, t(26) = 3.6, p < .01. In contrast, the parental perceptions of child attachment scores in the control group were 2.93 (.13) and 2.89 (.14) at Time 1 and Time 2, respectively, evidencing no significant change over time, t(23) = −.51, ns.
Fig. 2.
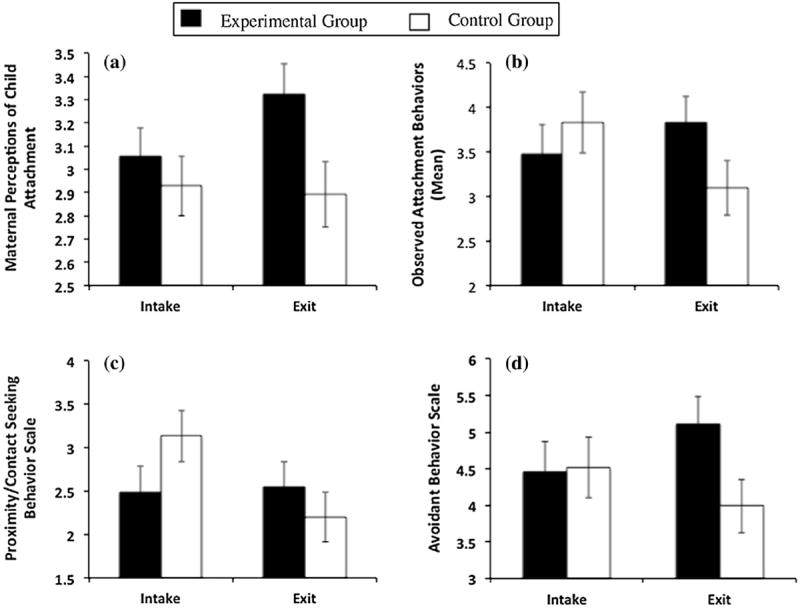
Graphs depicting change in four measures of attachment-related behaviors between intake and exit assessments, presented separately for the experimental and control groups: a maternal perceptions of child attachment, b observed attachment behaviors (mean), c observed proximity/contact seeking behavior, and d observed avoidant behavior
Results also revealed a significant main effect of treatment group allocation on gains in observed attachment behaviors (mean), t(54) = 2.0, p < .05. However, the nature of this treatment effect differed somewhat between the two types of observed attachment behaviors. For children’s Avoidant Behaviors, results revealed a significant main effect of treatment group allocation on improvements in Avoidant Behaviors from Time 1 to Time 2, t(54) = 2.2, p < .05. However, follow up analyses were inconclusive as to whether this treatment effect could be attributed to improvements in avoidant behaviors in the experimental group, t(24) = 1.4, p = .18, or worsening of avoidant behaviors in the control group, t(25) = −1.0, p = .34. In contrast, the treatment effect on children’s Proximity and Contact Seeking Behaviors was only marginally significant, t(54) = 1.8, p < .08. Subsequent analyses revealed that children assigned to the control group showed a significant decrease in Proximity and Contact Seeking behaviors, t(24) = −3.3, p < .01, while children assigned to the experimental group evidenced no significant change over time, t(24) = .2, p = .86.
Discussion
The current study presents analyses from a randomized clinical trial evaluating the efficacy of FPI. Previously published results have shown that FPI is associated with significant increases in responsive parental communication (Siller et al. 2013a). Results from the current analyses revealed that children who were randomly assigned to FPI also showed bigger increases in attachment-related behaviors, compared to children assigned to the control condition. Significant intervention effects of FPI were found for both an observational measure of attachment-related behaviors elicited in the context of a brief separation-reunion episode and a questionnaire measure evaluating parental perceptions of child attachment.
This is the first randomized clinical trial to investigate intervention effects on attachment-related outcomes in children with autism. Potentially, improvements in this area are of great clinical significance. Research on high-risk populations has linked early attachment relations to a broad range of long-term outcomes, including children’s language and cognitive development (van Ijzendoorn et al. 1995), self-esteem, independence, and school achievement (Sroufe et al. 2010). In addition, Claussen et al. (2002) hypothesized that the link between early attachment relations and children’s long-term outcomes (e.g., cognition, language) may at least in part be mediated by children’s early joint attention milestones. That is, parent–child relations that are secure and organized may provide an effective context for children to appreciate the social rewards associated with joint attention bids and responses. Consistent with this hypothesis, the authors present data that reveal a concurrent association between attachment classifications and joint attention behaviors in 56 high-risk infants prenatally exposed to cocaine. Only few studies involving children with ASD have investigated the association between quantitative (Siller and Sigman 2002) or qualitative aspects of caregiving (Naber et al. 2007a) and children’s emerging joint attention behaviors. Similarly, the long-term outcomes associated with early attachment security in autism are largely unknown. This lack of research activity is surprising, given that joint attention is commonly viewed as a core deficit in autism, and given the robust findings emphasizing the important role of early attachment relations in other populations.
The current study revealed a significant intervention effect of FPI on the degree to which parents perceived that their child was attached to them. This perception was evaluated using the Maternal Perception of Child Attachment Questionnaire (Hoppes and Harris 1990) which includes items such as “When my child is hurt or in pain, s(he) comes to me for comfort or help”. In a recent study, Goodman and Glenwick (2012) reported that parental perceptions of child attachment were significantly related to children’s functional impairments. Thus, a lean interpretation of the current results is that intervention effects on attachment-related outcomes were evident not only in the context of an experimental separation-reunion episode, but also in the context of (parent reported) every-day interactions. In addition, changes in parental perceptions of child attachment may reveal or be associated with underlying changes in parenting-related cognitions or emotions. For example, Hoppes and Harris (1990) reported a significant positive association between maternal perceptions of child attachment and maternal feelings of gratification. Similarly, Goodman and Glenwick (2012) reported an association between parental perceptions of child attachment and parenting related stress. Interestingly, this association was only significant for fathers, but not mothers, leading the authors to speculate that this relation may be moderated by parental attributions. For example, parents may experience greater stress or feel less competent if they attribute their child’s lower degree of attachment as a reflection of their own parenting.
FPI was initially developed as an experimental intervention to test the causal link between responsive parental communication and children’s subsequent gains in joint attention and language (Siller and Sigman 2002, 2008). In this program of research, responsive parental communication (i.e., parental synchronization) is defined as parental gestures or language that are responsive to the child’s focus of attention and ongoing engagement with toys. Previously published results have shown that FPI is associated with significant increases in responsive parental communication (Siller et al. 2013a). However, it is currently unknown whether FPI also improves global ratings of maternal sensitivity, which are commonly viewed as the developmental context of secure attachment relations. In a previous study, Siller and Sigman (2008) observed parent–child play interactions in a sample of 28 preschoolers with ASD. Unpublished results from this study (Siller et al. 2006) revealed a significant association between quantitative measures of maternal synchronization and global ratings of maternal sensitivity (Ainsworth et al. 1978), r(28) = .38, p < .05 (Siller et al. 2006). Results from the current study do not allow us to specify the active ingredient responsible for children’s increases in attachment-related behaviors. However, it seems likely that FPI causes changes in parenting that go beyond our original focus on parental synchronization. These changes may include a range of sensitive parenting behaviors. To effectively increase responsive gestures and language, FPI targets the parents’ ability to notice and interpret their child’s communicative signals (e.g., eye gaze, posture, emotions, gestures), and promotes interactive behaviors that are responsive to the child’s interest and developmental level (e.g., following the child’s lead, imitating, commenting, and elaborating on the child’s actions).
This research contributes to a growing body of research which demonstrates that sensitivity based interventions can enhance the attachment-related behaviors of various groups of high-risk children (van der Boom 1994, 1995; Heinicke et al. 1999, 2001; Powell et al. 2007; Juffer et al. 2008). In the context of parent-mediated interventions that aim to support the capacity of families to meet the needs of young children with ASD, attachment related outcomes seem particularly relevant. The parent–child relationship provides an important context for children’s early social, emotional, and communicative development. Even seemingly small changes in children’s attachment-related behaviors (e.g., a child who begins to seek his parents’ proximity after a short separation) may impact the parents’ affective attachment to their child, which may have lasting implications for the parents’ ability to support their child throughout the lifespan. Interestingly, results from the current study reveal that children assigned to the control condition showed a significant increase in avoidant behaviors between baseline and exit assessments. This finding suggests that, in the absence of appropriate parent support, the interactions between children with ASD and their parents may become increasingly strained as children get older. Consistent with this interpretation, findings reported by Siller et al. (2013a) revealed that responsive behaviors of some parents assigned to the control condition (i.e., parents who were classified as insightful at baseline) significantly decreased with time. Thus, one important outcome of effective parent education may be to prevent worsening in the quality of parent–child interaction over time.
The current study has several strengths, including random assignment, intent-to-treat analysis with “state of the art” missing data techniques, a relatively large sample size, and the use of mixed methods to evaluate attachment-related outcomes (i.e., observation, parent-report). Moreover, the current study raises several questions for further investigation. First, future research should investigate whether FPI increases not just the quantity of attachment-related behaviors, but also the quality of children’s attachment relations (Ainsworth et al. 1978). Second, both longitudinal and experimental research designs should be used to investigate the long-term outcomes associated with individual differences in the early attachment relations in ASD. Finally, to evaluate whether changes in maternal sensitivity mediate the relation between intervention group assignment and attachment-related outcomes, and to evaluate whether the severity of ASD symptoms or intellectual disability moderates intervention effects on attachment-related outcomes, clinical trials with larger samples sizes are necessary. By refining our understanding of active ingredients that explain intervention effects on attachment-related outcomes, and by increasing our ability to predict whose attachment-related outcomes are likely to increase during intervention, we would gain a greater understanding of the causal mechanisms that underlie the current intervention effects, and also be in a better position to guide families who are making decisions about their children’s intervention programs.
Acknowledgments
The authors extend a special thanks to the families that participated in this study. We also wish to thank the researchers who contributed to this project over the years, especially Amanda Chinchilla and Elia Jimenez. Special Thanks to David Oppenheim and Nina Koren-Karie for their invaluable support and feedback on drafts of this manuscript. Support from this research include: CPEA Grant HD-DCD35470 and the M.I.N.D. Institute Research Program.
Contributor Information
Michael Siller, Email: msiller@hunter.cuny.edu, Department of Psychiatry and Biobehavioral Sciences, University of California at Los Angeles, Los Angeles, CA 90024, USA; Psychology Department, Hunter College, The City University of New York, RM 611 HN, 695 Park Ave, New York, NY 10065-5024, USA.
Meghan Swanson, Psychology Department, Hunter College, The City University of New York, RM 611 HN, 695 Park Ave, New York, NY 10065-5024, USA.
Alan Gerber, Psychology Department, Hunter College, The City University of New York, RM 611 HN, 695 Park Ave, New York, NY 10065-5024, USA.
Ted Hutman, Department of Psychiatry and Biobehavioral Sciences, University of California at Los Angeles, Los Angeles, CA 90024, USA.
Marian Sigman, Department of Psychiatry and Biobehavioral Sciences, University of California at Los Angeles, Los Angeles, CA 90024, USA.
References
- Ainsworth MS. Infant–mother attachment. American Psychologist. 1979;34:932–937. doi: 10.1037//0003-066x.34.10.932. [DOI] [PubMed] [Google Scholar]
- Ainsworth MDS, Blehar MC, Waters E, Wall S. Patterns of attachment: A psychological study of the strange situation. Hillsdale, NJs: Lawrence Erlbaum Associates; 1978. [Google Scholar]
- Atkinson L, Chisholm VC, Scott B, Goldberg S, Vaughn BE, Blackwell J, et al. Maternal sensitivity, child functional level, and attachment in Down syndrome. In: Vondra J, Barnett D, editors. Atypical attachment in infancy and early childhood. Monographs of the Society for Research in Child Development. Serial No. 258. Vol. 64. 1999. pp. 45–66. [DOI] [PubMed] [Google Scholar]
- Bernabei P, Camaioni L, Levi G. An evaluation of early development in children with autism and pervasive developmental disorders from home movies: Preliminary findings. Autism. 1998;2:243–258. [Google Scholar]
- Bono MA, Daley T, Sigman M. Relations among joint attention, amount of intervention and language gain in autism. Journal of Autism and Developmental Disorders. 2004;34:495–505. doi: 10.1007/s10803-004-2545-x. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss: Attachment. Vol. 1. New York: Basic Books; 1969/1982. Original work published 1969. [Google Scholar]
- Capps L, Sigman M, Mundy P. Attachment security in children with autism. Development and Psychopathology. 1994;6:249–261. [Google Scholar]
- Carter AS, Messinger DS, Stone WL, Celimli S, Nahmias AS, Yoder P. A randomized controlled trial of Hanen’s ‘More Than Words’ in toddlers with early autism symptoms. Journal of Child Psychology and Psychiatry. 2011;52:741–752. doi: 10.1111/j.1469-7610.2011.02395.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy J, Shaver PH. Handbook of attachment: Theory, research, and clinical applications. New York: Guilford; 1999. [Google Scholar]
- Claussen AH, Mundy PC, Mallik SA, Willoughby JC. Joint attention and disorganized attachment status in infants at risk. Development and Psychopathology. 2002;14:279–292. doi: 10.1017/s0954579402002055. [DOI] [PubMed] [Google Scholar]
- Collins LM, Schafer JL, Kam CM. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychological Methods. 2001;6:330–351. [PubMed] [Google Scholar]
- De Wolff MS, van IJzendoorn MH. Sensitivity and attachment: A meta-analysis on parental antecedents of infant attachment. Child Development. 1997;68:571–591. [PubMed] [Google Scholar]
- Enders CK. Applied missing data analysis. New York: Guilford; 2010. [Google Scholar]
- Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. New York: Wiley; 2004. [Google Scholar]
- Goodman SJ, Glenwick DS. Correlates of attachment perceptions in parents of children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2012;42:2056–2066. doi: 10.1007/s10803-012-1453-8. [DOI] [PubMed] [Google Scholar]
- Graham JW, Olchowski AE, Gilreath TD. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Preventive Science. 2007;8:208–213. doi: 10.1007/s11121-007-0070-9. [DOI] [PubMed] [Google Scholar]
- Heinicke CM, Fineman NR, Ponce VA, Guthrie D. Relation-based intervention with at-risk mothers: Outcome in the second year of life. Infant and Mental Health Journal. 2001;22:431–462. [Google Scholar]
- Heinicke CM, Fineman NR, Ruth G, Recchia SL, Guthrie D, Rodning C. Relationship-based intervention with at-risk mothers: Outcome in the first year of life. Infant Mental Health Journal. 1999;20:349–374. [Google Scholar]
- Hoppes K, Harris SL. Perceptions of child attachment and maternal gratification in mothers of children with autism and Down syndrome. Journal of Clinical Child Psychology. 1990;19:365–370. [Google Scholar]
- Juffer F, Bakermans-Kranenburg MJ, van IJzendoorn MH. Promoting positive parenting: An attachment-based intervention. New York: Taylor & Francis; 2008. [Google Scholar]
- Koren-Karie N, Oppenheim D, Dolev S, Yirmiya N. Mothers of securely attached children with autism spectrum disorder are more sensitive than mothers of insecurely attached children. Journal of Child Psychology and Psychiatry. 2009;50:643–650. doi: 10.1111/j.1469-7610.2008.02043.x. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Jr, Leventhal BL, DiLavore PC, et al. The autism diagnostic observational schedule-generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Development Disorders. 2000;30:205–223. [PubMed] [Google Scholar]
- Lord C, Rutter M, Le Couteur A. Autism diagnostic interview-revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Development Disorders. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Mullen E. Mullen scales of early learning (AGS ed) Circle Pines, MN: American Guidance Service; 1995. [Google Scholar]
- Naber FB, Swinkels SHN, Buitelaar JK, Bakermans-Kranenburg MJ, van IJzendorn MH, Dietz C, et al. Attachment in toddlers with autism and other developmental disorders. Journal of Autism and Developmental Disorders. 2007a;37:1123–1138. doi: 10.1007/s10803-006-0255-2. [DOI] [PubMed] [Google Scholar]
- Naber FB, Swinkels SHN, Buitelaar JK, Dietz C, van Daalen E, Bakermans-Kranenburg MJ, et al. Joint attention and attachment in toddlers with autism. Journal of Abnormal Child Psychology. 2007b;35:899–911. doi: 10.1007/s10802-007-9142-3. [DOI] [PubMed] [Google Scholar]
- NICHD Early Child Care Research Network. Duncan GJ. Modeling the impacts of child care quality on children’s preschool cognitive development. Child Development. 2003;74:1454–1475. doi: 10.1111/1467-8624.00617. [DOI] [PubMed] [Google Scholar]
- Powell B, Cooper G, Hoffman K, Marvin R. The circle of security project: A case study—‘It’s hard to give that which you did not receive’. In: Oppenheim D, Goldsmith DF, editors. Attachment theory in clinical work with children. New York: Guilford Press; 2007. pp. 172–202. [Google Scholar]
- Rogers SJ, Ozonoff S, Maslin-Cole C. A comparative study of attachment behavior in young children with autism or other psychiatric disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30:483–488. doi: 10.1097/00004583-199105000-00021. [DOI] [PubMed] [Google Scholar]
- Rutgers AH, Bakermans-Kranenburg MJ, van IJzendoorn MH, Van Berckelaer-Onnes IA. Autism and attachment: A meta-analytic review. Journal of Child Psychology and Psychiatry. 2004;45:1123–1134. doi: 10.1111/j.1469-7610.2004.t01-1-00305.x. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Seibert JM, Hogan AE, Mundy PC. Assessing interactional competencies: The early social-communication scales. Infant Mental Health Journal. 1982;3:244–258. [Google Scholar]
- Sigman M, Mundy P. Social attachments in autistic-children. Journal of the Academy of Child and Adolescent Psychiatry. 1989;28:74–81. doi: 10.1097/00004583-198901000-00014. [DOI] [PubMed] [Google Scholar]
- Siller M, Hutman T, Sigman M. A Parent-mediated intervention to increase responsive parental behaviors and child communication in children with ASD: A randomized clinical trial. Journal of Autism and Developmental Disorders. 2013a;43:540–555. doi: 10.1007/s10803-012-1584-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siller M, Reyes N, Hotez E, Hutman T, Sigman M. Longitudinal change in the use of services in autism spectrum disorder: Understanding the role of child characteristics, family demographics, and parent cognitions. Autism. 2013b doi: 10.1177/1362361313476766. [DOI] [PubMed] [Google Scholar]
- Siller M, Rozga A, Sigman M. The nature of individual differences in the behaviors of mothers of young children with autism. University of California; Los Angeles: 2006. Unpublished manuscript. [Google Scholar]
- Siller M, Sigman M. The behaviors of parents of children with autism predict the subsequent development of their children’s communication. Journal of Autism and Developmental Disorders. 2002;32:77–89. doi: 10.1023/a:1014884404276. [DOI] [PubMed] [Google Scholar]
- Siller M, Sigman M. Modeling longitudinal change in the language abilities of children with autism: Parent behaviors and child characteristics as predictors of change. Developmental Psychology. 2008;44:1691–1704. doi: 10.1037/a0013771. [DOI] [PubMed] [Google Scholar]
- Sroufe LA, Coffino B, Carlson EA. Conceptualizing the role of early experience: Lessons from the Minnesota longitudinal study. Developmental Review. 2010;30:36–51. doi: 10.1016/j.dr.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Boom DC. The influence of temperament and mothering on attachment and exploration: An experimental manipulation of sensitive responsiveness among lower-class mother with irritable infants. Child Development. 1994;65:1457–1477. doi: 10.1111/j.1467-8624.1994.tb00829.x. [DOI] [PubMed] [Google Scholar]
- van der Boom DC. Do first-year intervention effects endure? Follow-up during toddlerhood of a sample of Dutch irritable infants. Child Development. 1995;66:1798–1816. [PubMed] [Google Scholar]
- van IJzendoorn MH, Dijkstra J, Bus AG. Attachment, intelligence, and language: A meta-analysis. Social Development. 1995;4:115–128. [Google Scholar]
- van IJzendoorn MH, Rutgers AH, Bakermans-Kranenburg MJ, Van Daalen E, Dietz C, Buitelaar JK, et al. Parental sensitivity and attachment in children with autism spectrum disorder: Comparison with children with mental retardation, with language delays, and with typical development. Child Development. 2007;78:597–608. doi: 10.1111/j.1467-8624.2007.01016.x. [DOI] [PubMed] [Google Scholar]
- Woods JJ, Brown JA. Integrating family capacity-building and child outcomes to support social communication development in young children with autism spectrum disorder. Topics in Language Disorders. 2011;31:235–246. [Google Scholar]


