Abstract
Among health behaviors, physical activity has the most extensive record of research using passive sensors. Control systems and other system dynamic approaches have long been considered applicable for understanding human behavior, but only recently has the technology provided the precise and intensive longitudinal data required for these analytic approaches. Although sensors provide intensive data on the patterns and variations of physical activity over time, the influences of these variations are often unmeasured. Health behavior theories provide an explanatory framework of the putative mediators of physical activity changes. Incorporating the intensive longitudinal measurement of these theoretical constructs is critical to improving the fit of control system model of physical activity and for advancing behavioral theory. Theory-based control models also provide guidance on the nature of the controllers which serve as the basis for just-in-time adaptive interventions based on these control system models.
I. INTRODUCTION
Smoking, poor diet, and inadequate physical activity are the leading causes morbidity and mortality [1]. Of these health risk behaviors, physical activity has made the greatest advances in measurement via wearable sensors. Accelerometer algorithms have become increasingly sophisticated and precise, providing detailed, moment-by-moment monitoring of energy expenditure and types of physical activity [2, 3]. These advances in wearable physical activity sensor have made physical activity a promising area for control systems and other system dynamic approaches.
Behavior has been considered amenable to a control systems approach for many years [4, 5], and Carver and Scheier have argued that dynamical regulatory systems are critical to understanding behavior [6]. Until recently, however, health behavior data has not been precise enough or longitudinally intensive enough to utilize computational modeling approaches. Wearable physical activity sensors now provide precise and temporally dense information on the activity of individuals throughout the day. Unfortunately, precise and temporally dense monitoring of the putative mediators that influence physical activity has not advanced as rapidly as the monitoring of the behavior itself.
II. THEORIES OF HEALTH BEHAVIOR
For nearly a century, health behavior theories have served as a guide for identifying potential influences of these behaviors and developing interventions that target these influences. Although a comprehensive review of health behavior theories is beyond the scope of this paper, a brief summary of the major theories seems warranted, particularly for those from outside the health behavior field who are applying computational modeling to health behavior problems. Regardless of scientific field, a theory is a systematic set of concepts, definitions, and propositions that specify the relationship among concepts for the purposes of explaining or predicting phenomena [7]. Theories are derived from observational data and hypotheses but also serve as the basis for determining what to observe and hypothesize. Therefore, for control systems modeling of physical activity, these theories offer guidance on the inputs of the system that influence physical activity.
In the 1950s, the U.S. Public Health Service began offering mobile tuberculosis (TB) screenings, and it was assumed that greater convenience and access would result in everyone getting screened, but screening rates did not increase appreciably [8]. Studies to understand why these screenings were not more effective led to the development of the Health Belief Model (HBM). HBM posits that an of the illness (e.g. TB) interact with the perceived benefits and barriers of engaging in the health behavior (e.g. chest x-ray screening) and with cues to action to increase or decrease the likelihood of engaging in the behavior [9]. Applied to physical activity, HBM posits that removing barriers to physical activity (e.g. improved access to places to walk and exercise) is a necessary but not sufficient condition to increase physical activity, and that individuals must also: a) believe that that there were benefits to regular physical activity that outweigh any remaining barriers, b) be cued or reminded to engage in physical activity, and c) believe that failing to engage in regular physical activity will result in serious consequences to their health and well-being. Many theories have been developed since HBM, and it is an incomplete model of behavior, but it continues to be the basis for many health behavior interventions.
The Theory of Reasoned Action and its subsequent revision as the Theory of Planned Behavior (TPB) incorporated some HBM concepts within its added social influences such as normative perceptions [10]. TPB also placed an intermediate conceptual step, behavioral intention (i.e. readiness to perform a given behavior), between these theoretical mechanisms and the actual behavior. Compared to HBM and applied to physical activity, TPB would posit that individuals are more likely to engage in physical activity if they a) care about the opinions of others, and b) believe that others are engaging in regular physical activity. Although both HBM and TPB have been useful for developing behavior change interventions, they have been criticized for their reliance on subjective cognitive influences that are difficult to measure [11].
Social Cognitive Theory (SCT) shares communalities with HBM and TPB but was developed from a different tradition more aligned with the behavioral learning principles of classical (or respondent or Pavlovian) and operant conditioning. Social Learning Theory expanded on the experiential learning of classical and operant conditioning to include observational or vicarious learning or modeling [12]. A subsequent reformulation to what is now known as Social Cognitive Theory included internal cognitive constructs such as self-efficacy and other perceived phenomena [13]. SCT also makes explicit the bidirectional relationship of behavior and the environment via the concept of reciprocal determinism [13]. Applied to physical activity, SCT posits that changes in physical activity are the result of self-efficacy (i.e., confidence in one’s ability to engage in physical activity), outcome expectancies (i.e., expectation of positive and negative outcomes from engaging in physical activity), self-management skills (i.e. the ability to set goals and monitor progress) and a range of environmental factors that facilitate or impede engaging in physical activity.
Although there are numerous theories of health behavior, HBM, TPB, and SCT have been among the most commonly used theories in the health behavior intervention literature [14]. While these theories are widely used for health behavior intervention development, they also have significant weaknesses. The application of these theories far exceeds the empirical support for these theories, and the lack of evidence for some of these constructs and their interrelationships is well-documented [14]. Moreover, these intrapersonal theories of behavior have been predominate the behavioral intervention literature while higher level factors (e.g. interpersonal, community, organizational, policy) and their related theories and models are underutilized in intervention development [15].
III. APPLICATIONS OF DYNAMICAL SYSTEMS MODELING TO HEALTH BEHAVIOR THEORY
These theories or health behavior can be viewed as dynamical systems in which various inputs (i.e., theoretical constructs) influence the output (i.e. behavior). As noted earlier, the concept that behavior could be understood as a dynamical system is not new, but only recently have dynamical system models been applied to existing health behavior theories. The first to do so was Navarro-Barrientos, Rivera, and Collins who developed a control system fluid analogy model for Theory of Planned Behavior (TPB) [16]. Orr and colleagues subsequently proposed a parallel constraint dynamical model of its precursor, the Theory of Reasoned Action [17]. Rivera and colleagues are developing a dynamical systems model of SCT [18].
Dynamical system modeling of health behavior theories has numerous advantages. Health behavior theories typically describe constructs that influence behavior and their interrelations but do not specify computational relationships among these constructs. Therefore, system identification efforts for health behavior theories improve the specificity and precision of the hypothesized relationships, making these theories more testable, and more refutable. Health behavior theories are based primarily on efforts to explain differences between individuals, not within individuals over time [19]. Dynamical system modeling facilitates the study of the interrelations of variables within individuals over time and provides a more comprehensive analytic technique for testing theories of human behavior [16, 19, 20, 21]. Since the process of behavior change is a within-person dynamic, an understanding of how behaviors change within a person over time based on the dynamical systems that influence the behavior has considerable potential to improve interventions, especially just-in-time adaptive interventions (JITAI) that adjust interventions based on ongoing inputs.
IV. MEASUREMENT OF THEORETICAL CONSTRUCTS TO UNDERSTAND THE INFLUENCES OF PHYSICAL ACTIVITY
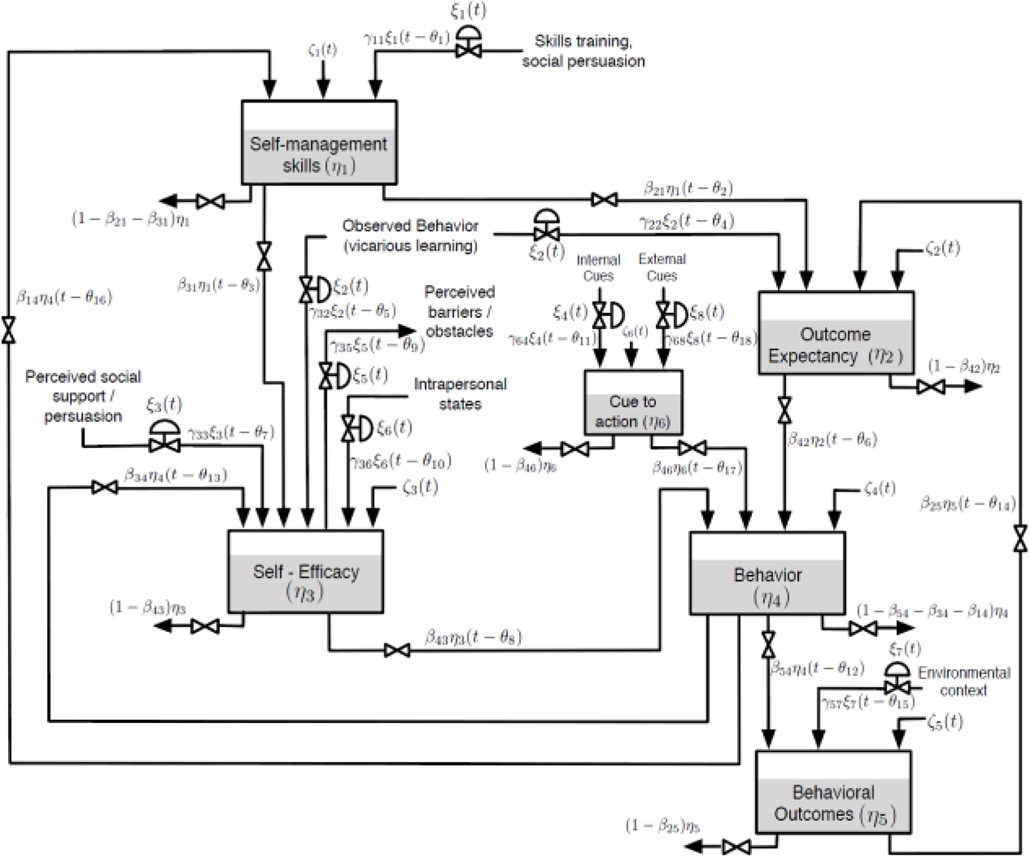
Figure 1 is a fluid analogy model of SCT, the details of which are described elsewhere [18]], which provides an example of the SCT variables that need to be considered to test such a model for understanding changes in physical activity over time in an individual or group of individuals. In this example, Behavior (η4) represents physical activity and is measured by wearable sensors (accelerometers).
Figure 1.
Fluid analogy of Social Cognitive Theory (SCT)
One of the proximate inputs to Behavior is Cue to Action (η6). In the context of physical activity, these are a combination of both internal cues (e.g., feeling bored) and external cues in the environment (e.g. friend asks if you want to go for a walk). Therefore, many of the external cues may be measurable via sensors that detect the context the individual is in (e.g. location) and/or the behavior in which they are engaged (e.g., working at the computer, watching TV, talking to someone). Although sensor technologies alone are unlikely to provide a comprehensive assessment of all of the external cues to action (or inaction), current sensor technologies are able to identify a wide array of possible cues. Via a combination of sensors for facial expressions and psychophysiology, it is also possible to detect some internal affective states [22], but until these technologies are field tested, validated, and unobtrusive, prompted self-reports of intrapersonal states are needed.
Two advances in self-report measurement are important to consider for testing theory via dynamic systems. One of these advances is the Computer Adaptive Testing (CAT) via Item Response Theory. Item Response Theory (IRT) has been used in the educational field for decades but has only recently been applied to health and health behavior constructs. The Patient-Reported Outcomes Measurement Information System (PROMIS) is perhaps the most well-known of these efforts [23]. IRT-developed item banks have the potential to precisely estimate the underlying latent trait efficiently. While computerized administration of self-report measures has been available for some time, the combination of computerized administration and IRT psychometric calibrations provides the basis for computerized adaptive testing (CAT) in which items are flexibly administered based on prior responses from items in the bank, resulting in maximum precision for minimum respondent burden [24].
Ecological Momentary Assessment (EMA) is the second advance in self-report measurement. A valid criticism of retrospective self-report is recall bias, but by prompting self-reports in real-time throughout the day, EMA or experience sampling minimizes recall bias, increases ecological validity, and allows for an intensive longitudinal analysis of the processes that influence behavior over time that are critical to dynamical system models of the influences of health behaviors [25]. EMA was initially implemented on PDA (Personal Digital Assistant) platforms, but the advent and rapid penetration of smartphone use, especially in the U.S., has provided a ubiquitous platform for EMA administration. The potential to combine EMA with CAT could allow for frequent and precise self-report while also minimizing habitual responding by varying the items administered [26]. When further integrated with the sensor technologies described above, event-based reporting can be performed without relying on the individual to identify the event.
Therefore, until sensor technologies develop that allow for the passive sensing or observing of these theoretical constructs, the combination of EMA and CAT provides researchers with frequent and precise measures of the other SCT variables described in Figure 1. For example, there are a number of well-accepted self-report measures of Self-report (η3) and Outcome Expectancy (η2) [27]. These measures, however, have been used predominantly in cross-sectional research and would need to be modified for intensive longitudinal, EMA administration.
Self-management Skills (η1) potentially could be assessed as a performance measure via a smartphone application in which the participant sets physical activity goals and monitors their progress toward those goals, with application use and the quality of the goal setting and monitoring techniques serving as indicators of self-management skills.
This example has focused on the measurement of the reservoir inputs to physical activity based on this SCT fluid analogy, but similarly, the various inputs to one of these reservoirs, e.g., self-efficacy, could be modeled and tested by measuring over time the various inputs to self-efficacy (i.e., perceived social support, observed behavior, intrapersonal states).
V. IMPLICATIONS FOR ADAPTIVE INTERVENTIONS
Beyond testing and refining theories of health behavior, the testing of dynamical systems based on theory also provide the basis for just-in-time adaptive interventions (JITAI) that can be delivered via mobile or wireless technologies and adapted based on prior inputs. Many of the initial efforts in JITAI have involved conditional logic algorithms, often with limited empirical support for the adaptations [19]. Dynamical systems, especially tested systems, would provide a rigorous empirical basis for JITAI that only reacts to inputs but also proactively anticipates the need for adaptive interventions. For example, Rivera and colleagues have shown how a control systems model can be used to optimize intervention intensity over the course of treatment [20]. The integration of intervention optimization with computational models of health behavior theories involves the addition of “controllers” to better regulate the system and “close the loop.” As illustrated by Rivera and colleagues, an intervention essentially shifts the variability from the behavioral outcome to the controller. Modifying the type and intensity of the intervention over time to maintain a desirable level of the outcome is very consistent with the adaptive potential of automated, technology-based interventions [19]. More importantly, these computational models can integrate theory testing and intervention testing, reducing the current disconnect between theory and practice.
VI. CONCLUSION
Wearable sensor technologies have produced precise measure, temporally dense measures of physical activity that can be used for dynamical system modeling. The challenge, however, is to identify the inputs that influence physical activity and health behavior theories provide a framework for such identification. While some of these theoretical constructs can be detected via sensor technologies, others are most efficiently measured via prospective and prompted self-reports throughout the day. The combination of CAT and EMA advances improve the precision while reducing the respondent burden of providing this information within an intensive longitudinal protocol. Utilizing current theory to guide system identification and modern measurement tools to assess these theoretical constructs in an intensive longitudinal manner provides a robust test of these theories and provides the basis for just-in-time adaptive interventions.
Contributor Information
William T. Riley, Email: wiriley@mail.nih.gov.
Cesar A. Martin, Email: cmartinm@asu.edu.
Daniel E. Rivera, Email: daniel.rivera@asu.edu.
REFERENCES
- 1.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 2.Plasqui G, Bonomi AG, Westerterp KR. Daily physical activity assessment with accelerometers: new insights and validation studies. Obesity Reviews. 2013;14:451–462. doi: 10.1111/obr.12021. [DOI] [PubMed] [Google Scholar]
- 3.Khusainov R, Azzi D, Achumba IE, Bersch SD. Real-time human ambulation, activity, and physiological monitoring: taxonomy of issues, techniques, applications, challenges and limitations. Sensors. 2013;13:12852–12902. doi: 10.3390/s131012852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wiener N. Cybernetics: On Communication and Control in Animals and Machines. Cambridge, MA: MIT Press; 1948. [Google Scholar]
- 5.Hanneman RA. Computer-assisted Theory Building: Modeling Dynamic Social Systems. Newbury Park, CA: Sage Publications; 1988. [Google Scholar]
- 6.Carver CS, Scheier MF. On the Self-Regulation of Behavior. Cambridge, MA: Cambridge University Press; 2001. [Google Scholar]
- 7.Kerlinger FM. Foundations of Behavioral Research. 3rd Ed. New York: Holt, Rinehart, and Winston; 1986. [Google Scholar]
- 8.Rosenstock IM. Historical origins of the Health Belief Model. Health Education Monographs. 1974;2:328–335. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- 9.Rosenstock IM. The Health Belief Model and preventive health behavior. Health Education Monographs. 1974;2:354–386. [Google Scholar]
- 10.Ajzen I. The Theory of Planned Behavior. Organizational Behavior and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- 11.Ogden J. Some problems with social cognition models: A pragmatic and conceptual analysis. Health Psychology. 2003;22:424–428. doi: 10.1037/0278-6133.22.4.424. [DOI] [PubMed] [Google Scholar]
- 12.Bandura A, Walters RH. Social Learning and Personality Development. New York: Holt, Rinehart & Winston; 1963. [Google Scholar]
- 13.Bandura A. Social Foundations of Thought and Action. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 14.Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annual Review of Public Health. 2010;31:399–418. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- 15.Stokol D. Translating social ecological theory into guidelines for community health promotion. American Journal of Health Promotion. 1996;10:282–296. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]
- 16.Navarro-Barrientos JE, Rivera DE, Collins LM. A dynamical model for describing behavioural interventions for weight loss and body composition change. Mathematical and Computer Modelling of Dynamical Systems. 2011;17:183–203. doi: 10.1080/13873954.2010.520409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Orr MG, Thrush R, Plaut DC. The Theory of Reasoned Action as parallel constraint satisfaction: Towards a dynamic computational model of health behavior. PLOS One. 2013;8:e62490. doi: 10.1371/journal.pone.0062490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martin CA, Rivera DE, Riley WT, Heckler EB, Bauman MP, Adams MA, King AC. Proceedings of the 2014 American Control Conference. Portland, OR: 2014. A dynamical systems model of Social Cognitive Theory. page in press. [Google Scholar]
- 19.Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: Are our theories up to the task? Translational Behavioral Medicine. 2011;1:53–71. doi: 10.1007/s13142-011-0021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rivera DE, Pew MD, Collins LM. Using engineering control principles to inform the design of adaptive interventions: a conceptual introduction. Drug and Alcohol Dependence. 2007;88:S31–S40. doi: 10.1016/j.drugalcdep.2006.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Deboeck PR, Bergeman CS. The reservoir model: A differential equation model of psychological regulation. Psychological Methods. 2013;18:237–256. doi: 10.1037/a0031603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.el Kaliouby R, Picard R, Baron-Cohen S. Affective computing and autism. Annals of the New York Academy of Science. 2006;1093:228–248. doi: 10.1196/annals.1382.016. [DOI] [PubMed] [Google Scholar]
- 23.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse DJ, Choi SW, Cook KF, DeVellis R, DeWalt D, Fries JF, Gershon R, Hahn E, Pilkonis P, Revicki D, Rose M, Weinfurt K, Hays RD on behalf of the PROMIS Cooperative Group. Initial item banks and first wave testing of the Patient–Reported Outcomes Measurement Information System (PROMIS) network: 2005–2008. Journal of Clinical Epidemiology. 2010;63:1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cook KF, O’Malley KJ, Roddey TS. Dynamic assessment of health outcomes: time to let the CAT out of the bag? Health Services Research. 2005;40:1694–1711. doi: 10.1111/j.1475-6773.2005.00446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stone AA, Turkkan JS, Bachrach CA, Jobe JB, Kurtzman HS, Cain VS. The Science of Self-Report. Implications for Research and Practice. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- 26.Shiffman S S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- 27.Frei A, Svarin A, Steurer-Stey C, Puhan MA. Self-efficacy instruments for patients with chronic diseases suffer from methodological limitations--a systematic review. Health Quality of Life Outcomes. 2009;7:86. doi: 10.1186/1477-7525-7-86. [DOI] [PMC free article] [PubMed] [Google Scholar]