Abstract
Kikuchi's disease is a benign, self-limiting disease, whose pathogenesis remains unknown. Patients most often present with cervical lymphadenopathy, sometimes associated with fever and leukopenia. It has been reported that up to 40% of patients with Kikuchi's disease have also cutaneous eruptions, but no specific skin changes have been described. Kikuchi's disease can be subclassified into three histologic subtypes: a proliferative type, a necrotizing type and a xantomathous type. Most patients with Kikuchi's disease require no specific treatment, because the disease regresses spontaneously, within a few weeks to months. We report a case of a 31-year-old woman with xanthomatous type of Kikuchi's disease, whose first manifestation was the onset of erythematous papules with central suppuration on her face and on her left hand.
Keywords: Fever of unknown origin, Leukopenia, Rare diseases
INTRODUCTION
Kikuchi's disease (KD), also known as histiocytic necrotizing lymphadenitis was first reported by Kikuchi and Fujimoto, in 1972.1 It has a worldwide distribution and affects predominantly young adults, especially young women of Asian descent.2 In most cases, the disease resolves spontaneously within several months. 2 Patients most often present with cervical lymphadenopathy, sometimes associated with fever and with leukopenia.2,3 It has been reported, that up to 40% of patients with KD have cutaneous eruptions, but no specific skin changes have been described.4-6 KD can be subclassified into three histologic types, which may represent different evolving stages in the evolution of the disease: a proliferative, a necrotizing type and a xanthomatous type.2 The necrotizing type of KD is the most common type of KD and the xanthomatous type is the least common.2
We present a case of a young woman with xanthomatous type of KD, whose first manifestation was appearing of papules and pustules with central crust on her face and on her left hand.
CASE REPORT
A previously healthy 31-year-old Caucasian woman came to our observation with multiple slowly growing, painless, non-pruritic, erythematous papules and pustules on the face and left hand. The lesions appeared progressively over 3 weeks. They were asymptomatic and there was no history of local trauma. She also had complaints of intermittent fever and tender swelling of both sides of her neck and right axilla, over the previous 2 weeks.
Physical examination revealed numerous erythematous papules and pustules with central crusts, on her face and on her left hand (Figure 1 and 2). She also had infracentimetric enlarged and tender bilaterally cervical and right axillary lymph nodes, confirmed by computed tomography. There wasn't splenomegaly and hepatomegaly. She was afebrile.
FIGURE 1.

Erythemato us papules with central suppuration on the face
FIGURE 2.

Erythemato us papules on left hand
Her past medical and family history was unremarkable. She was not taking any medication.
Laboratory examination demonstrated a hemoglobin level of 10,4 g/dL, a platelet count of 188 x103/uL and a leukopenia (white blood cell count: 2,2x103/uL). White blood cell differential revealed 44,4% neutrophils, 42,6% lymphocytes (without atypical forms), 12,5% of monocytes and 0,5% of eosinophils. An elevated erythrocyte sedimentation rate of 18 mm/h and a C-reactive protein of 24,70 mg/L were noted. The serum titers of Epstein-Barr virus and cytomegalovirus were negative.
Histopathological examination of a lesion taken from the left hand revealed that within the papillary dermis there was edema and a lymphohistiocytic infiltrate (Figure 3).
FIGURE 3.
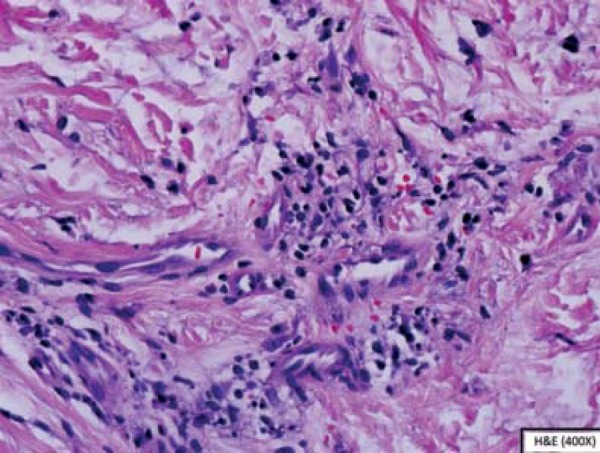
Edema of the papillary dermis, with a lymphohistiocytic infiltrate
Histopathological examination of an ultrasound guided fine-needle aspiration of lymph node on right axilla showed many foamy histiocytes, nuclear debris and lymphoid follicles with reactive germinal centers (Figure 4).
FIGURE 4.
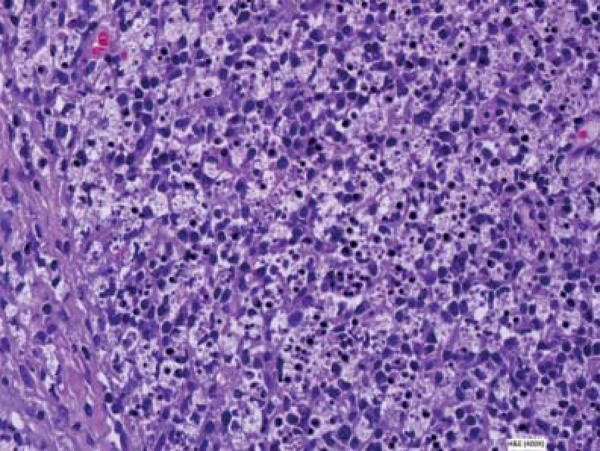
Lymphoid follicles with reactive germinal centers and many foamy histiocytes and nuclear debris
Taken together, clinical and pathological data suggested a diagnosis of xanthomatous type of KD.
The disease was self-limited with spontaneous resolution of the cutaneous lesions and lymphadenopathy, within 3 months.
DISCUSSION
KD is a benign disease, whose etiology and pathogenesis remains unknown, although the hypothesis that immune-mediated mechanisms might activate KD has been postulated.3,4,7 Some viral infections, such as human herpes virus-6, Epstein-Barr virus, cytomegalovirus, parvovirus B19 and human immunodeficiency virus have also been proposed as possible triggering factors for KD.1,3,7
Patients most often present with cervical lymphadenopathy, sometimes associated with fever and leukopenia.1,3,4 It has been reported that up to 40% of patients with KD have cutaneous eruptions, but no specific skin changes have been described.4,5,6 The most common skin manifestations are erythematous macules, papules, plaques, nodules and ulcers, localized on the face, on the upper and lower extremities and on the trunk.1,4,5,8 In our patient, the first symptom of KD was the appearing of papules and with central suppuration, on her face and on her left hand. Posteriorly, she also complained of fever and cervical lymphadenopathy and on laboratory examination there was leukopenia.
The cutaneous histopathological findings of KD are variable, and as a consequence, it has been difficult for pathologists to make a specific diagnosis, only based on skin biopsy specimens.4 Most of the histopathological findings of cutaneous lesions, described in the literature, were perivascular or interstitial infiltration of lymphohistiocytes and nuclear debris.4,5
The definitive diagnosis is only made histopathologically on lymph nodes.3,4 Histopathological examination of the involved lymph nodes is characterized by histiocytes, lymphocytes and a large amount of nuclear debris, with patchy necrosis and an absence of neutrophils or a granulomatous reaction.6,8
KD can be subclassified into three histologic subtypes, which may represent different evolving stages in the evolution of the disease: a proliferative type, a necrotizing type and a xanthomatous type.2 The proliferative type shows a mixture of histiocytes and lymphoid cells, with apoptosis, but without necrosis. In the necrotizing type, the lymph nodes show large areas of necrosis in addition to the changes characteristic of proliferative type. In the xantomathous type, the foamy histiocytes predominate and necrosis can be present or absent.2 The necrotizing type of KD disease is the most common and the xanthomatous type is the least common type. In our patient, the KD was of the xanthomathous type, because the biopsy of lymph node showed a collection of foamy histiocytes.2,9
KD disease is a self-limiting disease and an early and precise diagnosis may be helpful for avoiding unnecessary invasive procedures and treatment.
The differential diagnosis of KD with cutaneous manifestations includes viral exanthema, lupus erythematosus and leukemia or lymphoma cutis. Unlike the non-specific macular eruption in infectious mononucleosis, the skin lesions in KD may present as plaques, erosions or ulcers. Lupus erythematosus can be differentiated from KD histologically. Leukemia and lymphoma cutis can be difficult to differentiate from KD both clinically and histologically. However, leukemia and lymphoma rarely regress spontaneously and tend to be more monomorphous histologically.6,8
Most patients with KD require no specific treatment, because the disease resolves spontaneously, with a few weeks to months, without any serious complications and only rarely recur.1,2,8 Of the few cases described in the literature, which received oral steroids or antibiotics, there were no differences in the course of the disease.7,8
Footnotes
Conflict of Interests: None
Financial Support: None
How to cite this article: Resende C, Araújo C, Duarte ML, Vieira AP, Brito C. Kikuchi's disease of the xanthomathous type with cutaneous manifestations. An Bras Dermatol. 2015;90(2):245-7.
Work performed at the Hospital de Braga - Braga, Portugal.
References
- 1.Kim KJ, Jee MS, Chang SE, Choi JH, Sung KJ, Moon KC, et al. Kikuchi-Fujimoto disease with papulopustular skin manifestations. Clin Exp Dermatol. 2003;28:142–144. doi: 10.1046/j.1365-2230.2003.01160.x. [DOI] [PubMed] [Google Scholar]
- 2.Kuo TT. Kikuchi´s disease (histiocytic necrotizing lymphadenitis): A clinicopathologic study of 79 cases with an analysis of histologic subtypes, immunohistology and DNA ploidy. Am J Surg Pathol. 1995;19:798–809. doi: 10.1097/00000478-199507000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Kim SK, Kang MS, Yoon BY, Kim DY, Cho SK, Bae SC, et al. Histiocytic necrotizing lymphadenitis in the context of systemic lupus erythematosus (SLE): Is histiocytic necrotizing lymphadenitis in SLE associated with skin lesions? Lupus. 2011;20:809–819. doi: 10.1177/0961203310397684. [DOI] [PubMed] [Google Scholar]
- 4.Kim JH, Kim YB, In SI, Kim YC, Han JH. The cutaneous lesions of Kikuchi's disease: a comprehensive analysis of 16 cases based on the clinicopathologic, immunohistochemical, and immunofluorescence studies with an emphasis on the differential diagnosis. Hum Pathol. 2010;41:1245–1254. doi: 10.1016/j.humpath.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Yen HR, Lin PY, Chuang WY, Chang ML, Chiu CH. Skin manifestations of Kikuchi- Fujimoto disease: case report and review. Eur J Pediatr. 2004;163:210–213. doi: 10.1007/s00431-003-1364-y. [DOI] [PubMed] [Google Scholar]
- 6.Yasukawa K, Matsumura T, Sato-Matsumura KC, Takahashi T, Fujioka Y, Kobayashi H, et al. Kikuchi's disease and the skin: case report and review of the literature. Br J Dermatol. 2001;144:885–889. doi: 10.1046/j.1365-2133.2001.04151.x. [DOI] [PubMed] [Google Scholar]
- 7.Toll A, Gilaberte M, Matias-Guiu X, Camacho L, Alomar A, Gonzalez-Gay MA, et al. Kikuchi's disease with cutaneous involvement associated with subacute cutaneous lupus erythematosus. Clin Exp Dermatol. 2004;29:240–243. doi: 10.1111/j.1365-2230.2004.01454.x. [DOI] [PubMed] [Google Scholar]
- 8.Yen A, Fearneyhough P, Raimer SS, Hudnall SD. EBV-associated Kikuchi's histiocytic necrotizing lymphadenitis with cutaneous manifestations. J Am Acad Dermatol. 1997;36:342–346. doi: 10.1016/s0190-9622(97)80413-6. [DOI] [PubMed] [Google Scholar]
- 9.Hutchinson CB, Wang E. Kikuchi-Fujimoto disease, Arch Pathol Lab. Med. 2010;134:289–293. doi: 10.5858/134.2.289. [DOI] [PubMed] [Google Scholar]


