Abstract
Patient: Male, 40
Final Diagnosis: Mesenteric desmoid tumor
Symptoms: Abdominal mass
Medication: —
Clinical Procedure: Laparotomy exploratory
Specialty: Surgery
Objective:
Rare disease
Background:
Desmoid-type fibromatosis (DF) is a rare entity that predominantly involves the extremities, the trunk, and the abdominal cavity. It is a non-metastasizing, sporadic mesenchymal tumor with high tendency to recurrence and often is categorized as low-grade sarcoma.
Case Report:
We present here an extremely rare case of a mesenteric desmoid tumor (DT). A 40-year-old man presented to our clinic with a mass in the right-lower quadrant of the abdomen, which he incidentally palpated. A computerized tomography (CT) scan of the abdomen showed a mass between the loops of small intestine. The patient was treated successfully with wide excision of involved mesentery and adjacent small intestine. Histopathology of the mass revealed DT of the mesentery. No adjuvant treatment was applied and the patient was free of disease after a 6-month follow-up.
Conclusions:
Intra-abdominal DF is a rare pathology which should be differentiated while exploring abdominal tumors. Surgery, when dealing with operable masses, is the appropriate treatment.
MeSH Keywords: Abdominal Cavity, Fibromatosis Abdominal, Mesentery, Sarcoma
Background
DF, also known as aggressive fibromatosis, is a rare tumor characterized by proliferation of myofibroblasts [1] arising from the deep muscle fascia, aponeurosis, tendons, and scar tissue [2]. According to the WHO, desmoid tumors are defined as “clonal fibroblastic proliferations that arise in the deep soft tissue and are characterized by infiltrative growth and tendency toward local recurrence but inability to metastasize”. Their etiology is unknown, although often associated with endocrine factors, FAP, and trauma [3]. DTs are often categorized as low-grade sarcomas because of their high tendency to recur locally if excision margins are infiltrated. Two different types of DTs are described: sporadic ones and those associated with familial adenomatous polyposis (FAP). This manifestation accounts for 5–10% of DF [4]. There is no sex predilection and the average age at disease development is 30–40 years [5]. The extremities, trunk, and abdominal cavity are most frequently involved. Only 5% of sporadic desmoids tumors are intra-abdominal, but 80% of patients with FAP-associated DTs develop intra-abdominal disease [6]. In the abdominal cavity they are mostly found as mesenteric masses. The incidence of DT is <3% of all soft-tissue sarcomas and 0.03% of all malignancies [3].
The natural history of DF depends on several known and unknown factors. These factors influence the therapeutic approach to the disease and it has not yet been possible to establish an optimal therapy protocol. Nowadays, the treatment of desmoids tumors consists of surgery, radiation therapy, and/or antiproliferative treatment in various combinations. In the past, surgery (alone or in combination with radiotherapy [RT]), was the first line of treatment. The avoidance of excessive morbidity with preservation of function and improvement of the patient’s quality of life led to reassessment of overall management, giving priority to a “wait and see” approach. However, the surgical approach remains the first-line therapy for resectable tumors.
We report here a new case of DT of the mesentery.
Case Report
A 40-year-old Caucasian man presented to our surgical department with a mass in the right-lower quadrant of the abdomen, incidentally palpated by him and without any pathological signs such as abdominal pain, vomiting, or constipation. His past medical history was free of prior abdominal trauma, surgery, or any genetic disease. The performed physical examination disclosed a painlessness abdominal mass. The laboratory test results did not reveal any abnormalities. A computerized tomography (CT) scan of the abdomen showed an easily removable mass between the loops of the small intestine. Its size was 8×8.5 cm (Figure 1).
Figure 1.
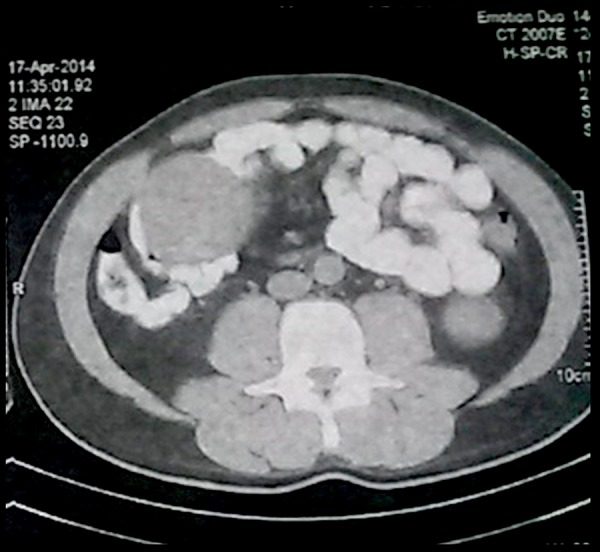
Intra-abdominal tumor (8×8.5 cm) between loops of the small intestine.
The patient underwent exploratory laparotomy, which disclosed a “tennis ball-shaped” tumor of the mesentery close to the small intestine, 40 cm from the ileocecal valve (Figure 2). No ascites or peritoneal or liver metastases were found. A wide excision of the involved mesentery and adjacent small intestine was performed with a side-to-side anastomosis between the proximal and the distal end of the small intestine using stapling technique. The surgical procedure was uneventful, without intraoperative blood loss and lasted approximately 45 min. A drain was placed in the abdominal cavity, near to the anastomosis. The patient resumed oral intake on postoperative day (POD) 3. On POD 5, the drainage catheter was removed because there was no significant drainage volume. Hospitalization was uneventful and the patient was discharged home on POD 7.
Figure 2.
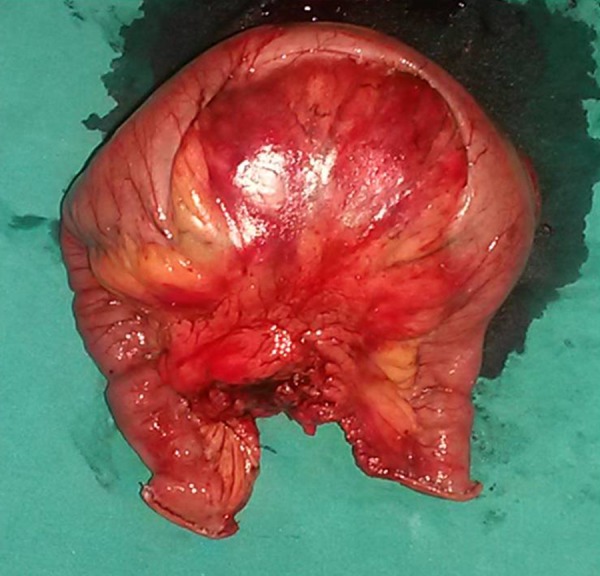
A “tennis ball-shaped” tumor of the mesentery and small intestine, which did not block the lumen.
Histopathology of the mass revealed DT of the mesentery, which infiltrated the muscularis propria of the small bowel, provoking ulceration of the mucosa. Immunohistochemical analysis showed diffuse cytoplasmic immunoreactivity for vimentin and nuclear expression of β-catenin (Figure 3). The lesion was 9.8 cm in diameter and was excised with clear margins.
Figure 3.
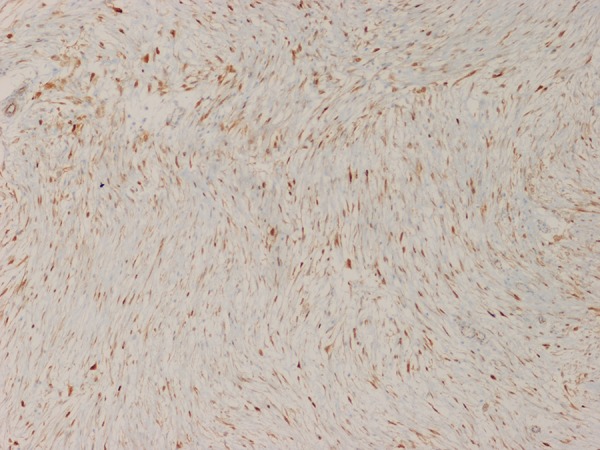
Immunostaining for β-catenin demonstrates nuclear expression (×100).
No adjuvant treatment was applied and no local recurrence or distant metastasis was found during 6-month follow-up.
Discussion
DTs are soft-tissue tumors, with poor data on their management and prognosis because of their infrequency [7]. In the USA the incidence is 2–4 out of 1 million people each year. Their etiology is unknown, although it they often associated with endocrine factors, FAP, and trauma [3]. The average age is 30–40 years regardless of sex, but they are predominantly found in young female patients of reproductive age [8]. Intra-abdominal DTs are often asymptomatic and the differential diagnosis includes GIST, lymphomas, carcinoids, fibrosarcomas, and inflammatory fibroid polyps [9]. Our patient did not mention any abdominal trauma or surgical intervention in his medical history and the colonoscopy 2 months after surgery did not reveal polyposis.
Surgery is the mainstay therapeutical approach for patients with resectable intra-abdominal DTs, but surgery may cause significant morbidity, especially because of excessive resection of the small intestine [6]. Excision of adherent structures and viscera, which may be close but not invaded, may be needed for tumors arising in the retroperitoneum or abdomen, with microscopic intralesional margins achieving local tumor control and possibly improving survival [10]. According to the NCCN guidelines (version 2.2014), after the performance of the biopsy, which confirms the diagnosis, a careful “watch and wait” approach can be followed if the tumors do not provoke functional limitations. DF has an unknown natural history and there is a possibility of aggressive progression during the observational period; therefore, patients with resectable tumors should be treated surgically when R0 excision is feasible. In our case, surgical intervention was chosen based on the CT scan findings and the patient’s preference; diagnostic laparoscopy and biopsy were therefore not required. Intraoperatively it was revealed that the lumen of the small intestine was infiltrated and could have become blocked (also confirmed by histopathology). During the operation we observed that wide excision for achieving negative margins was feasible, with no excessive morbidity produced.
When the tumor is unresectable, the margins of resection are unclear. In case of recurrence, adjuvant radiation or chemo-therapy [6,11] is indicated. Desmoids respond slowly to radiation but radiotherapy is not generally recommended for retroperitoneal or intra-abdominal DTs. Cytostatic or cytotoxic systemic therapy with tamoxifen, interferon-alpha, imatinib, and non-steroidal anti-inflammatory agents have been reported to reduce the progression of the disease.
The French and the Italian sarcoma groups have recently approved a treatment algorithm, based on a front-line “wait and see” approach and subsequent therapy in the case of progression [12]. However, the chosen approach depends on patient preference, the presence of pain, and the threatening of adjacent anatomical sites.
Disease-free survival (DFS) is limited by the following factors: tumor size larger than 5 cm, extra-abdominal tumor location, R1 resection status, and history of recurrence [7,13,14]. The growth pattern of these tumors is deeply infiltrating, and there is no tumor capsule. Because the boundaries of the tumors are difficult to distinguish intraoperatively from scars or connective tissue, R0 excision is not always possible and leads to recurrence. A specific mutation of β-catenin (45F) in patients treated surgically has been correlated with poor 5-year DFS. A potential value of β-catenin mutational analysis as a predictor of progression-free survival has not yet been proven, and the benefit from adjuvant therapy in that group of patients is still under investigation [15]. In our case, the tumour size was 9.8×8.5 cm, the excision margins were clear, and a mutational analysis of β-catenin had not yet been performed.
Management should include multidisciplinary consultation to determine optimal therapy.
Conclusions
Desmoid fibromatosis of the mesentery is a rare entity. The surgical resection of DTs using wide negative margins remains the first-line treatment of resectable intra-abdominal desmoid tumors. Adjuvant/neoadjuvant radiation therapy and chemo-therapy are contingent on an accurate histologic diagnosis and are used to shrink or to inhibit the progression of the tumor in cases of unresectable disease if the resection margins are not clear or if there is disease recurrence.
Acknowledgments
The authors thank pathologist Vladika Natalia MD for her valuable help by giving us the histological slides.
Abbreviations:
- DF
desmoid-type fibromatosis;
- CT
computerized tomography;
- POD
postoperative day;
- FAP
familial adenomatous polyposis;
- DFS
disease-free survival
Footnotes
Competing interests
The authors declare that they have no competing interests.
References:
- 1.Burke AP, Sobin LH, Shekitka KM, et al. Intra-abdominal fibromatosis. A pathologic analysis of 130 tumours with comparison of clinical subgroups. Am J Surg Pathol. 1990;14(4):335–41. [PubMed] [Google Scholar]
- 2.Kriz J, Eich HT, Haverkamp U, et al. Radiotherapy is effective for DTs (aggressive fibromatosis) – long-term results of a german multicenter study. Oncol Res Treat. 2014;37(5):255–60. doi: 10.1159/000362398. [DOI] [PubMed] [Google Scholar]
- 3.Reitamo JJ, Häyry P, Nykyri E, Saxén E. The DT. I. Incidence, sex-, age- and anatomical distribution in the Finnish population. Am J Clin Pathol. 1982;77(6):665–73. doi: 10.1093/ajcp/77.6.665. [DOI] [PubMed] [Google Scholar]
- 4.Calvert GT, Monument MJ, Burt RW, et al. Extra-Abdominal DTs Associated with Familial Adenomatous Polyposis. Sarcoma. 2012;2012:726537. doi: 10.1155/2012/726537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Plukker JT, van Oort I, Vermey A, et al. Aggressive fibromatosis (non-familial desmoids tumour): therapeutic problems and the role of adjuvant radiotherapy. Br J Surg. 1995;82(4):510–14. doi: 10.1002/bjs.1800820424. [DOI] [PubMed] [Google Scholar]
- 6.Kasper B, Ströbel P, Hohenberger P. DTs: Clinical Features and Treatment Options for Advanced Disease. Oncologist. 2011 May;16(5):682–693. doi: 10.1634/theoncologist.2010-0281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeng WG, Zhou ZX, Liang JW, et al. Prognostic factors for DT: a surgical series of 233 patients at a single institution. Tumour Biol. 2014;35:7513–21. doi: 10.1007/s13277-014-2002-1. [DOI] [PubMed] [Google Scholar]
- 8.Okamura A, Takahashi T, Saikawa Y, et al. Intra-abdominal DT mimicking gastric cancer recurrence: a case report. Int J RadiatOncolBiol Phys. 1990;19(1):225–27. [Google Scholar]
- 9.Bethune R, Amin A. Mesenteric fibromatosis: a rare cause of acute abdominal pain. Ann R CollSurg Engl. 2006;88(2):1–2. doi: 10.1308/003588406X83113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gronchi A, Colombo C, Raut CP. Surgical management of localized soft tissue tumours. Cancer. 2014;120(17):2638–48. doi: 10.1002/cncr.28715. [DOI] [PubMed] [Google Scholar]
- 11.Wood TJ, Quinn KM, Farrokhyar F, et al. Local control of extra-abdominal DTs: systematic review and meta-analysis. Rare Tumours. 2013;5(1):e2. doi: 10.4081/rt.2013.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gronchi A, Colombo C, Le Péchoux C, et al. Sporadic desmoid-type fibromatosis: a stepwise approach to a non-metastasising neoplasm – a position paper from the Italian and the French Sarcoma Group. Ann Oncol. 2014;25(3):578–83. doi: 10.1093/annonc/mdt485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stoeckle E, Coindre JM, Longy M, et al. A critical analysis of treatment strategies in DTs: a review of a series of 106 cases. Eur J Surg Oncol. 2009;35(2):129–34. doi: 10.1016/j.ejso.2008.06.1495. [DOI] [PubMed] [Google Scholar]
- 14.Huang K, Wang CM, Chen JG, et al. Prognostic factors influencing event-free survival and treatments in desmoid-type fibromatosis: analysis from a large institution. Am J Surg. 2014;207(6):847–54. doi: 10.1016/j.amjsurg.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 15.Lazar AJ, Tuvin D, Hajibashi S, et al. Specific mutations in the beta-catenin gene (CTNNB1) correlate with local recurrence in sporadic DTs. Am J Pathol. 2008;173(5):1518–27. doi: 10.2353/ajpath.2008.080475. [DOI] [PMC free article] [PubMed] [Google Scholar]


